Trauma
Incidence and Etiology
Birth trauma related to cephalopelvic disproportion, large gestational weight, atypical presentation, and the use of forceps or vacuum extraction is discussed in Chapter 23.
Imaging in Pediatric Head Trauma
Limitations of CT include low contrast in the immature brain, which decreases its sensitivity in detecting edema in infants, and beam hardening artifact, which may partially obscure small extraaxial collection or subtle cortical contusions adjacent to bone, particularly in the posterior fossa and skull base. Although advances in CT scanners have improved their sensitivity in detecting TBI, CT is known to underestimate the degree and extent of traumatic parenchymal injuries when compared with MR imaging (MRI). Nonetheless, acute imaging findings on CT have been proposed as criteria for grading and predicting outcome in persons with TBI (the Marshall Classification and subsequent modifications by Maas et al.).1
CT has been used liberally in children with scalp contusions. Recently, the exposure of children’s brains to excessive radiation has become a concern after Pearce et al.2 demonstrated that children exposed to radiation to the head from CT scans have an increased risk of the development of brain tumors many years later. For patients with a minor head injury (Glasgow Coma Scale [GCS] score of 13 to 15), clinical guidelines are available regarding indications for obtaining a CT scan of the head, such as the New Orleans Criteria, the Canadian CT Head Rule, and guidelines from the Pediatric Emergency Care Applied Research Network, with high sensitivity for detecting injuries that require neurosurgical intervention.3 The American College of Radiology also publishes Appropriateness Criteria for imaging in the setting of head trauma, including a special section for children younger than 2 years in whom clinical assessment and criteria are less reliable than for older children.4
Adaptive statistical iterative reconstruction is a reconstruction technique that reduces image noise and improves low-contrast detectability and image quality. It provides higher diagnostic performance at a lower dose with no loss of image sharpness, noise, and artifacts.5
Magnetic Resonance Imaging
Because of its more limited availability and longer scanning times, MRI generally is a secondary modality in the evaluation of acute head trauma. MRI usually is performed in the subacute and chronic phases when the findings on CT do not correlate with the patient’s clinical condition, or when patients have unexpected neurologic deterioration or are not responding as expected. MRI offers the advantages of direct multiplanar imaging and greater overall sensitivity and specificity for the detection of TBI. It is particularly useful in the detection of small extraaxial hematomas, nonhemorrhagic intraaxial contusions, edema, brainstem injury, posterior fossa abnormalities, and DAI.6 Contraindications to MRI include incompatible vascular clips, metallic implants, ocular foreign bodies, and most pacemakers.
T2* gradient-echo sequence (GRE) uses a pair of bipolar gradient pulses instead of a refocusing 180-degree pulse to enhance magnetic susceptibility caused by magnetic field distortion. Susceptibility-weighted imaging (SWI) is a technique that uses the signal loss from out-of-phase protons with different magnetic susceptibilities. SWI is more sensitive than GRE for detection of blood products such as deoxyhemoglobin, methemoglobin, and hemosiderin.7
Diffusion-weighted imaging (DWI) assesses the diffusion of water protons with use of a bipolar gradient pulse. The normal diffusion of water protons along the gradient reduces the MR signal. Areas of restricted diffusion will retain the MR signal and represent acute cerebral injury in persons with ischemia/hypoxia, trauma, metabolic disorders, and infection. Reduced diffusion is present in lesions with a low nucleus-cytoplasm ratio. DWI is susceptible to the intrinsic T2* signal of the tissue because it is a gradient sequence, known as the T2 shine-through effect. To separate the DWI signal from T2 shine through, the apparent water diffusion coefficient (ADC) is calculated by acquiring images with different gradient duration and amplitude (b-values), thus eliminating the T1 and T2* values.8 Diffusion tensor imaging (DTI) assesses the anisotropy of the brain tissue by evaluating differences in the direction of diffusion of water molecules in normal and abnormal tissues and provides information about the orientation and integrity of the white matter tracts.
MR spectroscopy (MRS) assesses the distribution and quantification of naturally occurring molecules within the central nervous system (see Chapter 25). Various techniques are available. The most commonly used technique is the point-resolved spectroscopy sequence. Both short time to echo (TE) and long TE acquisitions can be obtained. All acquisitions provide sensitive, noninvasive analysis of brain metabolites and cellular biochemical changes. Decreased N-acetyl aspartate (NAA) has been reported to correlate with abnormal neuropsychological function tests in persons with TBI.9
Perfusion MRI of the brain can be assessed either through a dynamic T2/T2* acquisition during a bolus injection of intravenous contrast material or with unenhanced techniques such as arterial spin labeling and blood–oxygen level dependent sequences (see Chapters 27 and 28). Perfusion MRI provides the cerebral blood volume, cerebral blood flow, and mean transit time in targeted areas of the brain.
Magnetization transfer imaging (MTI) relies on the principle that protons bound in macromolecules of tissues exhibit T1 relaxation coupling with protons in the aqueous phase or water. When an off-resonance saturation pulse is applied, it selectively saturates the protons that are bound in macromolecules. These protons subsequently exchange longitudinal magnetization with free water protons, leading to a reduction in the detected signal intensity. The magnetization transfer ratio (MTR) may provide a quantitative index of the structural integrity of tissue. Animal models of rotational acceleration suggest that quantitative MTI offers increased sensitivity to detection of histopathologically proven damage, such as axonal swelling, compared with conventional MRI. Although the precise mechanism for MTR reduction is incompletely understood for mild head trauma, the extent of the abnormality usually increases as the MTR value decreases. Abnormal MTR also has been found in normal-appearing white matter on MRI and is an apparent predictor of poor outcome.10 Functional MRI has shown changes in regional brain activation in patients with TBI and has been used for assessment of clinical outcome of these patients.
Other Imaging Modalities
Magnetoencephalography (MEG) detects the magnetic waves that are created by the electric current along the axons. The advantage of MEG over electroencephalography is that the magnetic waves are less susceptible to distortion caused by the skull than the electric currents (see Chapter 28). This method of imaging has found that brain dysfunction is present in a significantly greater number of patients with minor head trauma and postconcussive syndrome than is shown by MRI or electroencephalography. This method shows excessive abnormal low-frequency magnetic activity, which provides objective evidence of brain injury in these patients that correlates with the degree of symptomatic recovery.
Positron emission tomography (PET) measures the cerebral metabolism of various substrates (see Chapter 25). Fluorodeoxyglucose is the primary substrate used in the measurement of glucose metabolism, which should correspond to neuronal viability. PET can be used in patients with DAI to determine the extent of damage and prognosis. PET also has been helpful in delineating the extent of reversibility of lesions. The major limitation of PET is the inability to distinguish functional abnormalities from structural damage.
Classification and Mechanisms of Head Injury
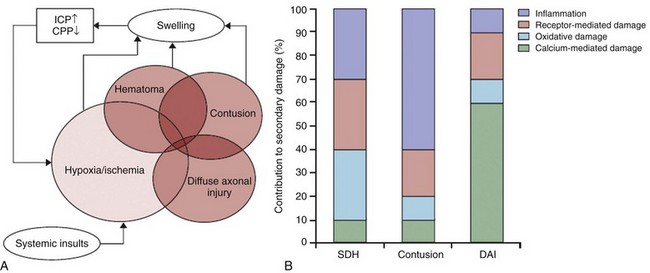
Based on different mechanisms of trauma and the associated injuries, the sequelae of head trauma can be classified into direct injury related to impact loading forces and indirect injury related to acceleration/deceleration and rotational forces. Direct injury may be subclassified into penetrating and nonpenetrating closed head injury (CHI). Moreover, brain injury in persons with a CHI may result directly from the impact (coup), or it may happen indirectly (contrecoup). The most common sequelae of direct head injury are scalp hematoma, skull fracture, direct brain contusion caused by a fracture and inward deformation of the skull, brain contusion caused by movement against the rough surface of the skull base, indirect (contrecoup) brain contusion diagonal to the site of impact, stretching and laceration of the brain parenchyma, subarachnoid hemorrhage (SAH) as a result of parenchymal injury, and epidural and subdural hematomas caused by direct vascular injury beneath the site of impact. Nonimpact, acceleration/deceleration injuries are the result of forces of translation (linear), acceleration/deceleration, and rotational and angular acceleration causing shear-strain forces on axons, neurons, and blood vessels. These injuries include contusions, DAI, deep gray matter injury, brainstem injuries, intraparenchymal hematomas as a result of vascular injury, and extraaxial hematomas. The axons are most vulnerable, and the blood vessels are the most resistant to injury from acceleration/deceleration forces (Fig. 39-1).11
Based on the GCS, head injuries are classified as mild (GCS score 13 to 15), moderate (GCS score 9 to 12), and severe (GCS score 3 to 8). Most head trauma results in mild injury; the risk of death from minor head injury in childhood approaches 0%. Moderate head injury in children has a similar rate of occurrence as in adults but a lower mortality rate. Severe head injury occurs less frequently in children compared with adults and has a significantly lower mortality rate. The exception is in infants younger than 2 years, who have a higher mortality rate from severe head injuries. This higher mortality rate is partially attributed to the occurrence of NAT in this age group.12
Skull Fractures
Linear calvarial fractures are more frequent in all age groups, followed by depressed or comminuted calvarial fractures and basilar fractures. Linear fractures usually heal without complication. Complex fractures in which the dura mater is torn may be complicated by herniation of the pia and arachnoid layers, creating a leptomeningeal cyst. The CSF pulsations lead to progressive erosion of skull around the fracture, known as a “growing fracture,” which appears as an angular or linear lytic lesion in the skull with scalloped margins (see Chapter 23). Underlying brain contusion is not uncommon.
Depressed fractures are comminuted skull fractures in which broken bones are displaced inward by at least the thickness of the skull. Depressed skull fractures usually result from blunt force trauma to the head and may result in increased intracranial pressure (ICP), epidural hematoma, and parenchymal contusion or laceration. Depressed fractures usually are treated surgically to prevent complications and also for cosmetic reasons. Fractures displacing the dural sinuses often are treated conservatively because of the potential risk of fatal hemorrhage with intervention (e-Fig. 39-2). Depressed fractures are categorized as compound fractures when a laceration of the overlying scalp is present and as penetrating fractures when an underlying dural tear is present, allowing potential communication between the external environment and the brain. Fractures that communicate with the paranasal sinuses, middle ear, or the mastoid air cells within the intracranial compartment are considered compound fractures. Pneumocephalus indicates the presence of a compound fracture (e-Fig. 39-3). The most serious complications of compound skull fractures are CSF leak and infection. Increased risk factors for infection include visible contamination (hair, skin, fat, or bone), a meningeal tear, and delayed treatment for more than 8 hours after the initial injury. A rare type of compound skull fracture is the elevated skull fracture, which occurs when the fracture is elevated outward above the outer table of the skull.
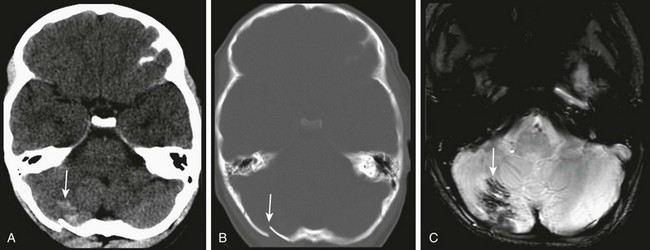
e-Figure 39-2 Occipital fracture and cerebellar contusion.
A, Unenhanced computed tomography shows an area of hyperdensity in the right cerebellum representing a hemorrhagic contusion (arrow). B, Bone reconstruction shows a depressed right occipital bone fracture (arrow). C, On the magnetic resonance imaging susceptibility-weighted imaging sequence, the blood products cause low signal susceptibility artifact (arrow). Depressed fractures adjacent to a venous sinus may not be suitable for surgical repair.
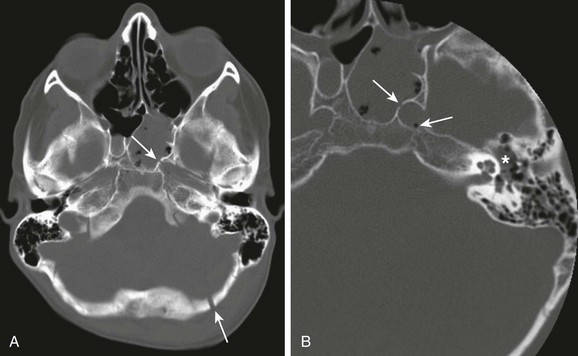
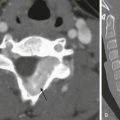
e-Figure 39-3 Skull base fracture.
A, A compound fracture through the left occipital bone and petrous apex extending into the sphenoid sinus (arrows). B, High-resolution reconstruction showing involvement of the left carotid canal (arrow) with the presence of a locule of air within the carotid canal (thin arrow) and partial opacification of the middle ear cavity (asterisks).
Extraaxial and Intraventricular Hemorrhage
Epidural hematoma is uncommon in infants and slowly increases in incidence with age, reaching a peak in adulthood. The etiology of epidural hematomas in children is different from that in adults. In younger children, venous epidural hematomas are more common than the arterial epidural hematomas. Tearing of a dural venous sinus, typically the transverse or sigmoid sinus, or an emissary or diploic vein are common causes of venous epidural hematomas. The typical locations of venous epidural hematomas are in the posterior fossa and occipital region from laceration of the transverse or sigmoid sinus, in the middle cranial fossa from injury of the sphenoparietal sinus or middle meningeal veins, and in the parasagittal area from a tear of the superior sagittal sinus. In older children and adolescents, arterial hematomas are more common. The vascular groove for the middle meningeal artery is relatively shallow, with the dura more adherent to the calvarium in children. Trauma to the calvarium causing inward deformity can separate the dura from the inner table and injure the meningeal artery, with hematoma accumulating over the temporal or parietal convexities (Fig. 39-4). The incidence of associated fractures with epidural hematomas is slightly less in children than in adults (83% vs. 93%).
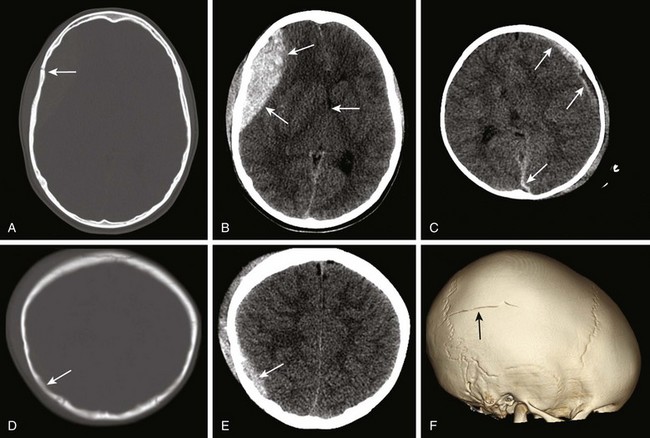
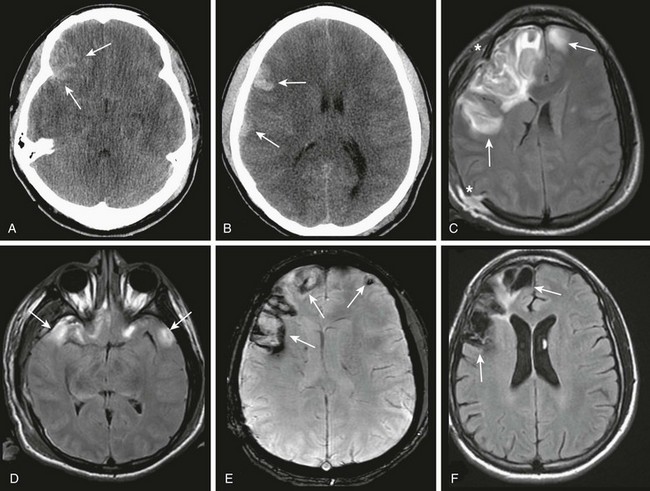
Figure 39-4 Skull fractures and extraaxial hematomas.
Unenhanced computed tomography images showing a pterional fracture (arrow) (A) and a large acute epidural hematoma with a contralateral midline shift (B). C, In contrast to the acute epidural hematoma, a hyperacute mixed attenuation left frontal subdural hematoma extending to the left occipital lobe is shown (arrows). D, A skull fracture parallel to the image plane appears as focal hypoattenuation (arrow). E, An acute epidural hematoma adjacent to the fracture (arrow) in the same patient as in part D. F, The fracture that is poorly visualized on axial images is well demonstrated on three-dimensional volume rendering (arrow).
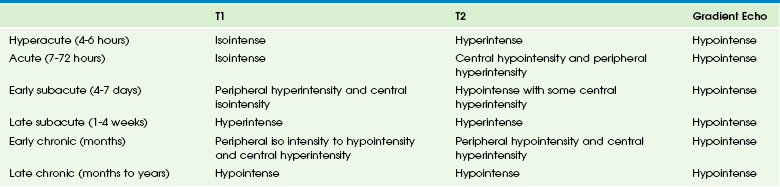
The aging of extraaxial hematomas based on signal characteristics in children has not been validated. The evolution of epidural and subdural hematomas follows a similar pattern (Table 39-1). In contrast to parenchymal hematomas, the hypointense rim on T1- and T2-weighted images representing hemosiderin is rarely seen in extraaxial hematomas because of the absence of a blood-brain barrier.
Subdural Hematoma
The CT imaging characteristics of subdural hematomas depend on the age of the hematoma. Hyperacute hematomas representing unclotted blood show attenuation similar to flowing blood in the dural sinuses. After a few hours, an acute subdural hematoma demonstrates increased attenuation related to clotted blood. The hyperattenuating acute blood clot may be mixed with blood from active bleeding, serum from clot retraction, or CSF resulting from a tear in the arachnoid (see Fig. 39-4). Typically within 1 to 3 weeks, the attenuation of a subacute hematoma decreases and becomes isodense to brain parenchyma. After 2 to 3 weeks, the attenuation of a chronic hematoma becomes similar to that of CSF. The hematoma may be difficult to see during the subacute and chronic phases, and associated signs of mass effect will indicate its presence, such as effacement of the adjacent sulci, displacement of the gray-white matter junction, compression of the ventricles, or herniation. If the presence of a hematoma is questionable, intravenous contrast material can be administered to show enhancing inner and outer membranes that are not seen in the acute phase. If the size of the collection increases or if the attenuation values appear greater than expected or are heterogeneous, rebleeding should be suspected. The development of a fluid-fluid level in the chronic phase also is suggestive of rebleeding. The membranes calcify in up to 3% of cases.
Subarachnoid and Intraventricular Hemorrhage
CT is the imaging modality of choice for acute SAH and intraventricular hemorrhage, showing increased attenuation blood within the sulci (Fig. 39-5), layering along the interhemispheric fissure and the tentorium, and in the ventricles. The most common location of traumatic SAH is in the posterior interhemispheric fissure and along the tentorium. Although the normal falx is relatively hyperdense on CT, hyperdense material insinuating into the cerebral sulci is indicative of SAH. Initially, SAH is detected adjacent to the source of bleeding. With time, SAH accumulates in the basal cisterns (particularly the interpeduncular cistern) and Sylvian fissures, over the convexities, and in the occipital horns of the lateral ventricles.
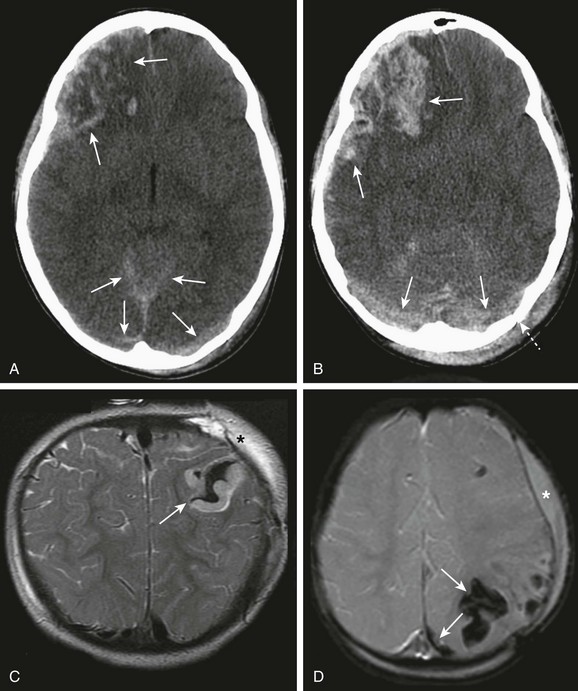
Figure 39-5 Parenchymal contusion, subarachnoid hemorrhage, and laceration.
Unenhanced computed tomography images (A and B) showing a contrecoup right frontal and temporal contusion with associated subarachnoid hemorrhage. In the occipital region, acute bilateral subdural hematomas are present, along with a left occipital fracture and a large scalp hematoma from the primary impact (broken arrow). A magnetic resonance imaging T2-weighted image (C) and susceptibility-weighted image (D) show a typical parenchymal laceration with a hematoma (arrows). Also note postcraniectomy findings (asterisks).
Traumatic Parenchymal Injury
CT shows hypoattenuation with loss of the gray-white matter differentiation and effacement of the sulci. Hemorrhagic foci appear as areas of increased attenuation involving the cortex (see Fig. 39-5). The attenuation of acute focal parenchymal hematomas increases during the first few days as the clot retracts and then decreases with subsequent proteolysis. Cortical enhancement may be seen for 1 to 2 weeks as a result of proliferation of immature capillaries that lack a blood-brain barrier.
MRI is the imaging modality of choice for parenchymal contusion. In the first hours after the injury when overt edema is not apparent, DWI is the most sensitive sequence for detecting parenchymal contusion, as well as shear injury. After 1 to 2 days, the contused areas appear hyperintense on FLAIR and T2-weighted images related to edema, and the microhemorrhages or focal confluent hemorrhages appear hypointense on T2 GRE or SWI images (e-Fig. 39-6). High signal intensity on T1-weighted images may be seen in the subacute phase, related to the presence of methemoglobin. FLAIR is insensitive to parenchymal contusion in neonates and infants because of the low contrast with the unmyelinated white matter. T2-weighted images are particularly useful in these cases showing loss of gray-matter differentiation and hyperintensity relative to the normal brain.
e-Figure 39-6 Evolution of a hemorrhagic parenchymal contusion.
A and B, Unenhanced computed tomography images demonstrate an acute right frontal contusion (arrows) with minimal midline shift. C and D, A few days later, magnetic resonance imaging fluid attenuated inversion recovery (FLAIR) demonstrates extensive edema, increasing midline shift, and additional areas of contusion in the left frontal lobe and bilateral temporal lobes (arrows). Postsurgical findings are related to a recent right hemispherical craniotomy (asterisks). E and F, A few months later, a peripheral rim of susceptibility related to chronic blood products (arrows) is seen on susceptibility-weighted imaging (E), and encephalomalacia and volume loss are seen on FLAIR (F).
Lacerations of brain parenchyma are the result of a greater mechanical force that causes tearing of tissue, extending from the cortex into the white matter. Although lacerations are characteristic of penetrating or perforating injury, they also occur in CHI or near a fracture. They are associated with a variable degree of hemorrhage (see Fig. 39-5). The hematoma may rapidly increase in size after the injury, and follow-up imaging in the first 24 to 48 hours is recommended. The most typical locations for parenchymal laceration are the inferior frontal and anterior temporal lobes. Lacerations also may occur in the corpus callosum and brainstem in association with DAI. Lacerations in the pontomedullary junction and cerebral peduncles presumably are related to hyperextension injury. Cerebellar contusions usually are associated with occipital fractures and most frequently involve the inferior cerebellar hemispheres and cerebellar tonsils.
Diffuse Axonal Injury
All imaging modalities underestimate the extent of DAI. As previously noted, diffuse brain damage may not be evident on CT. Reports have found that CT of acute CHI reveals abnormalities in only 20% to 50% of patients with axonal shear injuries, primarily because of their small size and frequent initial nonhemorrhagic nature. The typical CT findings of DAI include discrete foci of increased or decreased attenuation, which are usually bilateral, less than 1 cm in size, and are oriented in an axis that parallels the tracts. DAI is most commonly located in the subcortical white matter, near the gray-white matter junction of the frontal and temporal lobes, posterior corpus callosum (most commonly the posterior body and splenium), and brainstem (dorsolateral midbrain and upper pons). An important indirect sign of axonal injury involving the corpus callosum is the presence of intraventricular hemorrhage from shearing of the adjacent subependymal veins (Fig. 39-7). With increasing severity, involvement of the internal and external capsules, basal ganglia, thalami, cerebellum, and parietal and occipital lobes occurs. CT also demonstrates diffuse brain edema in infants with severe shear-strain injury. Within 2 to 3 weeks, encephalomalacia and volume loss develop.
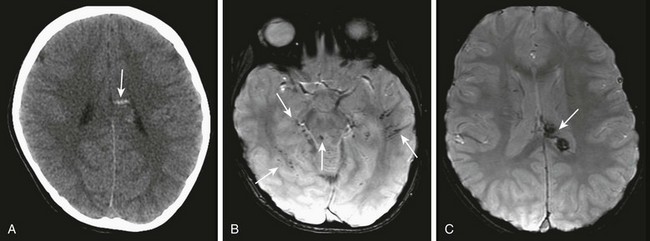
Figure 39-7 Diffuse axonal injury.
A, An unenhanced computed tomography image with hyperdense foci in the region of the corpus callosum compatible with a shear injury (arrow). B and C, A magnetic resonance susceptibility-weighted imaging sequence shows multiple susceptibility foci of hypointensity/blooming (arrows) consistent with parenchymal (B) and intraventricular (C) hemorrhage.
MRI using SWI and T2* sequences detects DAI in approximately 30% of patients with mild head injury and an initially normal CT scan. DAI is visualized as multiple small, round, ovoid, or elliptical areas of decreased T1 signal, increased T2 and FLAIR signal, and abnormal DWI signal. Hemorrhagic lesions cause susceptibility effect, with hypointensity on T2* and SWI (see Fig. 39-7). Initial nonhemorrhagic lesions may convert to hemorrhagic foci with time, showing typical evolution of signal characteristics of blood, with increasing size as a result of hemorrhage and edema. DWI depicts additional lesions that exhibit facilitated or, most commonly, restricted diffusion. ADC values decrease over a longer period, ~18 days, after injury, which is beyond the usual time frame for cytotoxic edema related to ischemia.13
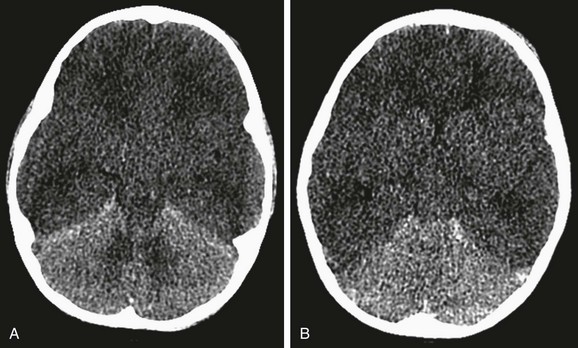
Diffuse Brain Swelling and Hypoperfusion Injury
The imaging findings in both conditions primarily affect the cerebrum with loss of the gray-white interface, diffuse homogeneously decreased attenuation, and effacement of the basal cisterns and ventricles on CT. The decreased attenuation can cause the circulating blood to appear hyperdense on CT and give a “pseudo-SAH” appearance, and the cerebellum may appear relatively hyperdense in contrast to the edematous cerebral hemispheres (“white cerebellar sign,” Fig. 39-8).
Sequelae of Trauma
Pediatric traumatic vascular injury is less common in children than in adults. Traumatic arterial dissection may result in infarction (Fig. 39-9). Vasospasm, vascular thrombosis, compression of a vessel from a hematoma, and hypoperfusion also can cause infarction. Intracranial carotid dissection, pseudoaneurysms after skull base fractures, and carotid cavernous fistula are less common sequelae following trauma. Intraoral trauma as a result of a fall with an object in the mouth is the most common cause of extracranial carotid artery injury in children.
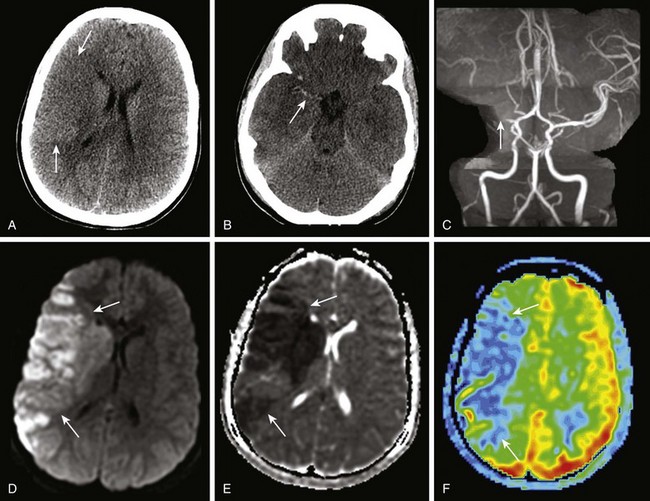
Figure 39-9 Traumatic dissection of the right middle cerebral artery (MCA).
A, An unenhanced computed tomography (CT) image of the brain at the level of the lateral ventricles demonstrates poor gray-white matter differentiation in the right frontal lobe (arrows). B, An unenhanced CT image at the level of the circle of Willis and midbrain demonstrates the “hyperdense MCA sign” (arrow). C, Occlusion of the right MCA (arrow) on three-dimensional time-of-flight magnetic resonance angiography. D and E, Restricted diffusion and low apparent diffusion coefficient values (arrows). F, An arterial spin label perfusion image showing decreased cerebral blood flow in the right MCA territory (arrows).
Nonaccidental Trauma
More than five children die each day in the United States as a result of abuse and neglect, with many cases likely unreported. Head injury after NAT is one of the leading causes of mortality and morbidity in infants and children. Radiologic findings are an integral part of the workup and diagnosis of NAT (see Chapter 144). Head injuries in these infants and children include skull fractures, intracranial and retinal hemorrhages, and parenchymal brain injury such as contusions, edema, ischemia, and infarction.
On MRI, the signal intensity of parenchymal injuries varies with time, and when correlated with other clinical findings, it can be helpful to clinicians and child advocacy services. However, the precise aging of parenchymal lesions and extraaxial hematomas should be undertaken with caution. CT hyperdensity is the only reliable indicator of age (Fig. 39-10). Subdural hematomas in infants younger than 2 years and subdural hematomas of different ages are highly suspicious for NAT. Retinal hemorrhages are a cardinal manifestation of NAT (Fig. 39-11). The severity of retinal hemorrhages and their extension to the periphery of the retina correlates with the likelihood of NAT and the severity of associated brain injury.
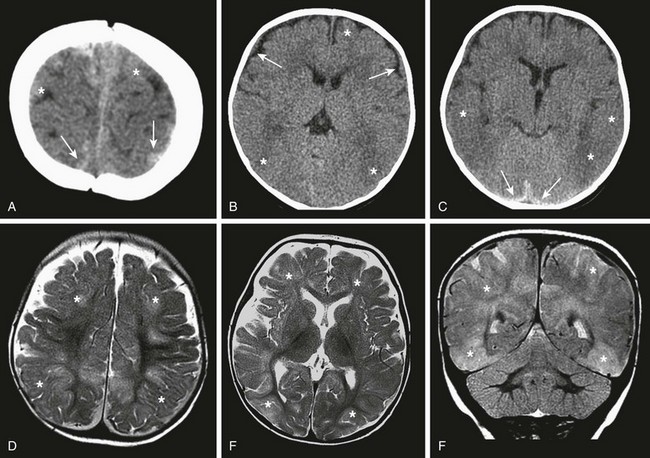
Figure 39-10 Nonaccidental trauma.
A, B, and C, An unenhanced computed tomography image demonstrates multiple areas of loss of gray-white matter differentiation (*) and bilateral acute and subacute subdural hematomas. D, E, and F, Magnetic resonance imaging T2-weighted images show the extent of the parenchymal injury with multifocal areas of cortical and subcortical injury (asterisks).
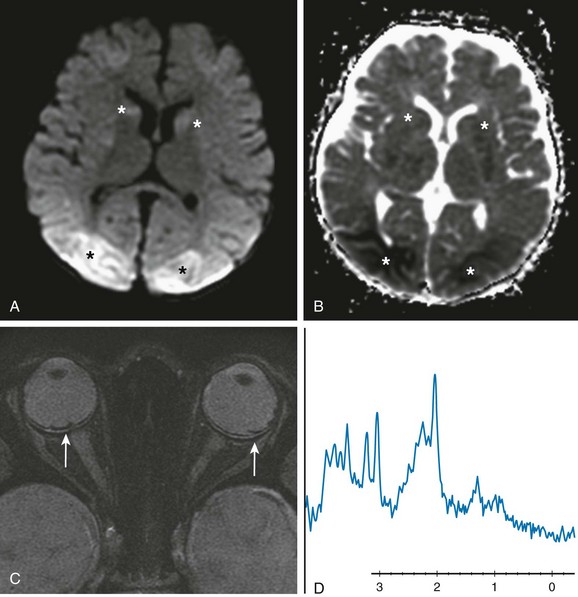
Figure 39-11 Nonaccidental trauma.
A and B, Magnetic resonance imaging (MRI) diffusion-weighted imaging (DWI) sequences show multiple areas of restricted diffusion that are more pronounced in the bilateral occipital lobes and the head of the caudate nuclei seen (asterisks) on DWI (A) and apparent diffusion coefficient (B). C, A high-resolution MRI susceptibility-weighted imaging sequence shows susceptibility related to retinal hemorrhages bilaterally (arrows). D, MR spectroscopy at level occipital lobes demonstrates a decreased N-acetylaspartate level (2.0 ppm) and elevated lactate and lipid (0.8 to 1.2 ppm) and glutamate/glutamine (2.2-2.4 ppm) levels.
Imaging findings show a diffuse loss of gray-white matter differentiation with sparing of the basal ganglia. Severe insults show more extensive brain edema, and the basal ganglia and the posterior fossa structures may be involved. Hypoxia resulting from strangulation involves the territory of the anterior circulation as a result of compression of the carotid vessels with relative sparing of the vertebral circulation. MRI and DWI are useful to delineate the full extent of ischemic injury, and MRS may demonstrate neuronal loss by demonstrating a decrease in the neuronal marker NAA and an increase in lactate, indicating anaerobic metabolism in the affected areas of the brain (see Fig. 39-11).
Barkovich, AJ. Pediatric neuroradiology, 5th ed. Philadelphia: Lippincott Williams & Wilkins; 2012.
Provenzale, JM. Imaging of traumatic brain injury: a review of the recent medical literature. AJR Am J Roentgenol. 2010;194(1):16–19.
Tortori-Donati, P, Rossi, A. Pediatric neuroradiology: brain, head, neck and spine. New York: Springer; 2005.
References
1. Maas, AI, et al. Prediction of outcome in traumatic brain injury with computed tomographic characteristics: a comparison between the computed tomographic classification and combinations of computed tomographic predictors. Neurosurgery. 2005;57(6):1173–1182.
2. Pearce, MS, Salotti, JA, Little, MP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet. 2012;380(9840):499–505.
3. Stiell, IG, et al. The Canadian CT Head Rule for patients with minor head injury. Lancet. 2001;357(9266):1391–1396.
4. Davis, PC, et al. Head trauma. American College of Radiology. ACR Appropriateness Criteria. Radiology. 2000;215(suppl):507–524.
5. Vorona, GA, et al. The use of adaptive statistical iterative reconstruction in pediatric head CT: a feasibility study. AJNR Am J Neuroradiol. 2012. [May 24 [Epub ahead of print]].
6. Lee, H, et al. Focal lesions in acute mild traumatic brain injury and neurocognitive outcome: CT versus 3T MRI. J Neurotrauma. 2008;25(9):1049–1056.
7. Sehgal, V, et al. Clinical applications of neuroimaging with susceptibility-weighted imaging. J Magn Reson Imaging. 2005;22(4):439–450.
8. Provenzale, JM. Imaging of traumatic brain injury: a review of the recent medical literature. AJR Am J Roentgenol. 2010;194(1):16–19.
9. Tollard, E, et al. Experience of diffusion tensor imaging and 1H spectroscopy for outcome prediction in severe traumatic brain injury: preliminary results. Crit Care Med. 2009;37(4):1448–1455.
10. Bagley, LJ, et al. Magnetization transfer imaging of traumatic brain injury. J Magn Reson Imaging. 2000;11(1):1–8.
11. Zhu, GW, Wang, F, Liu, WG. Classification and prediction of outcome in traumatic brain injury based on computed tomographic imaging. J Int Med Res. 2009;37(4):983–995.
12. Maas, AI, Stocchetti, N, Bullock, R. Moderate and severe traumatic brain injury in adults. Lancet Neurol. 2008;7(8):728–741.
13. Galloway, NR, et al. Diffusion-weighted imaging improves outcome prediction in pediatric traumatic brain injury. J Neurotrauma. 2008;25(10):1153–1162.