CHAPTER 34 Transversus abdominis plane block
Clinical anatomy
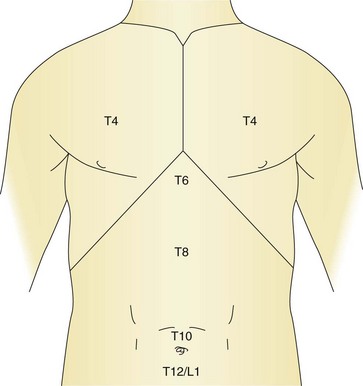
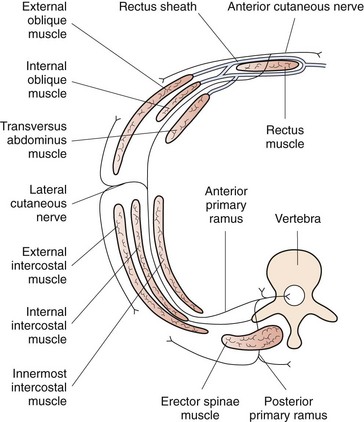
The sensory innervation of the abdominal wall is derived from the sixth thoracic nerve to the first lumbar nerve (Fig. 34.1). The nerves arise from the ventral rami of their respective nerve roots and travel anteriorly in a groove beneath the respective ribs to lie between the internal intercostal muscle and the innermost intercostal muscle. The intercostal nerve gives a sensory branch at the mid-axillary line, which provides variable innervation from the posterior axillary line anteriorly. The nerve continues forward as the anterior cutaneous branch, which enters the transversus abdominis plane of the anterior abdominal wall and supplies the skin, muscles and parietal peritoneum in the abdomen (Fig. 34.2). The transversus abdominis plane (TAP) lies between the internal oblique and transversus abdominis muscles, and forms a connective tissue conduit through which the ventral rami of T6 to L1 travel. Deposition of local anesthetic solution in the TAP permits abdominal wall sensory blockade.
Surface anatomy
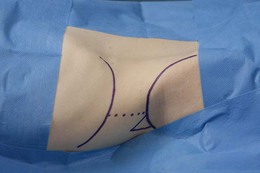
The surface anatomical landmarks for this block are: the iliac crest, the mid-axillary line and the costal margin. The needle insertion point is at the apex of the Lumbar Triangle of Petit, which is formed by the external oblique muscle anteriorly, the latissimus dorsi muscle posteriorly, and the iliac crest inferiorly (Fig. 34.3).
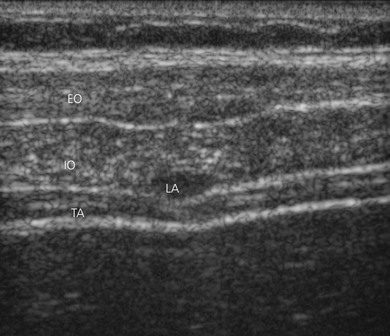
Sonoanatomy
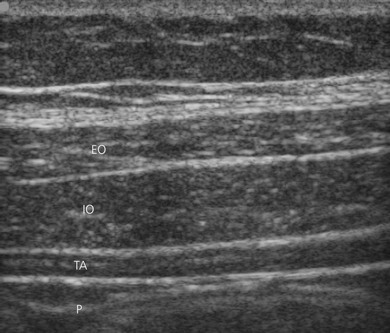
The muscles of the anterior abdominal wall are readily visible as three distinct layers (external oblique, internal oblique, transversus abdominis) (Fig. 34.4). The muscle layers are seen as marbled transverse structures surrounded by bright hyperechoic fascial coverings. The target for this block is the space between the internal oblique muscle and the transversus abdominis muscle at the level of the apex of the Lumbar Triangle of Petit.
Landmark-based approach
The block tray is set up with antibacterial solution and swabs, block needle and local anesthetic injectate. With the patient in a supine position, the operator stands opposite the side to be blocked and the iliac crest is palpated from anterior to posterior. The needle insertion point is at the apex of the Lumbar Triangle of Petit cephalad to the iliac crest, behind the mid-axillary line. The skin is disinfected with antiseptic solution and draped. The skin is pierced by the regional anesthesia needle (18-G Tuohy needle connected to sterile extension tubing). The needle is advanced at right angles to the skin, and a ’pop’ sensation is appreciated as the external oblique muscle is traversed (Fig. 34.5). Further advancement results in a second ‘pop,’ which signals entry to the transversus abdominis fascial plane. After aspiration to exclude vascular puncture, 0.3 mL/kg of local anesthetic (usually 0.25% levobupivacaine to a maximum dose of 2 mg/kg) is injected into the space (repeated on the other side, if indicated).
Ultrasound-guided approach
The operator stands on the side to be blocked with the patient in a supine position and the ultrasound machine located on the contralateral side (Fig. 34.6). If both sides are to be blocked, placing the ultrasound machine at the top of the table is optimal. The skin is disinfected with antiseptic solution and draped. A sterile sheath is applied over the ultrasound transducer with sterile ultrasound gel. Another layer of sterile gel is placed between the sterile sheath and the skin. The lateral abdominal wall is scanned in a transverse plane with a high frequency linear array transducer in the 10–13 MHz range. A low frequency transducer in the 2–5 MHz range is used in larger patients. The transducer is oriented transversely over the lateral abdominal wall between the iliac crest and the costal margin (Fig. 34.7). The ultrasound screen should be made to look like the scanning field. That is, the right side of the screen represents the right side of the field. Adjustable ultrasound variables such as scanning mode, depth of field, and gain are optimized.

Figure 34.6 Global view of the block field for the ultrasound-guided transversus abdominis plane block.
The image of the abdominal wall at this level reveals the three muscle layers with their surrounding connective tissue sheaths. The peritoneum and intestine are seen deep to the abdominal muscles (Fig. 34.4). The target is kept in the centre of the field of view, and the needle entry site is at the superior border of the linear transducer. An 18-G Tuohy needle is attached to sterile extension tubing, which is connected to a 20-mL syringe and flushed with local anesthetic solution to remove all air from the system. It is then introduced superior to the transducer and visualized along its entire path to the space between the internal oblique muscle and the transversus abdominis muscle (Fig. 34.8). It is important not to advance the needle without proper visualization; this may require ultrasound transducer adjustment.
Two distinct ‘pops’ are appreciated as the needle traverses the external oblique and internal oblique muscles. The second pop heralds entry to the transversus abdominis plane. Needle placement in the correct plane is indicated by fluid expansion in a space bounded by the hyperechoic fascial sheath of the internal oblique and transverse abdominis muscle layers (hydro dissect; Fig. 34.9). Incorrect needle placement will result in intramuscular fluid during hydrodissection. Following confirmation of correct needle placement, 2–30 mL of solution may then be injected and observed to fill the plane. For a surgical incision that does not involve the midline, a unilateral block on the side of the surgical incision will suffice. For a midline incision, the procedure must be repeated on the opposite side, as blockade of the contralateral sensory afferents is necessary to obtain midline analgesia.
Adverse effects
Armstrong O, Hamel A, Grignon B, et al. Lumbar hernia: anatomical basis and clinical aspects. Surg Radiol Anat. 2008;30:533-537.
Carney J, McDonnell JG, Ochana A, et al. The transversus abdominis plane block provides effective postoperative analgesia in patients undergoing total abdominal hysterectomy. Anesth Analg. 2008;107(6):2056-2060.
Farooq M, Carey M. A case of liver trauma with a blunt regional anesthesia needle while performing transversus abdominis plane block. Reg Anesth Pain Med. 2008;33(3):274-275.
Forastiere E, Sofra M, Giannarelli D, et al. Effectiveness of continuous wound infusion of 0.5% ropivacaine by On-Q pain relief system for postoperative pain management after open nephrectomy. Br J Anaesth. 2008;101(6):841-847.
Grady MV, Cummings KC3rd. The ‘flank bulge’ sign of a successful transversus abdominis plane block. Reg Anesth Pain Med. 2008;33(4):387.
Hebbard P. Transversalis fascia plane block, a novel ultrasound-guided abdominal wall nerve block. Can J Anesth. 2009;56(8):618-620.
McDonnell JG, O’Donnell BD, Heffernan A, et al. The analgesic efficacy of transversus abdominis plane block after abdominal surgery: a randomized controlled trial. Anesth Analg. 2007;104(1):193-197.
McDonnell JG, O’Donnell BD, Farrell T, et al. Transversus abdominis plane block: a cadaveric and radiological evaluation. Reg Anesth Pain Med. 2007;32(5):399-404.
Rosario DJ, Jacob S, Luntkey J, et al. Mechanism of femoral nerve palsy complicating percutaneous ilioinguinal field block. Br J Anaesth. 1997;78:314-316.