54 Transversus Abdominis Plane Block
Transversus abdominis plane (TAP) blocks can provide pain relief following surgeries that involve a lower abdominal incision. Examples include the Pfannenstiel (transverse) incision for cesarean delivery or hysterectomy, and surgeries that use a lower midline incision. Although somatic nerves of the abdominal wall are anesthetized, visceral pain following surgery is still an issue. These blocks therefore do not always provide definitive pain relief and multimodal analgesia is often necessary. TAP block reduces patient-controlled anesthesia (PCA) morphine requirements following surgery but does not appear to reduce opioid-related side effects.1 Another application for TAP blocks has been pain relief for anterior iliac crest bone grafts. TAP blocks also can be used as part of the diagnostic workup of chronic abdominal pain to distinguish visceral and somatic components as potential causes. Many variations of the TAP block exist, but most use a posterior or slightly modified approach.
Sonographic Landmarks
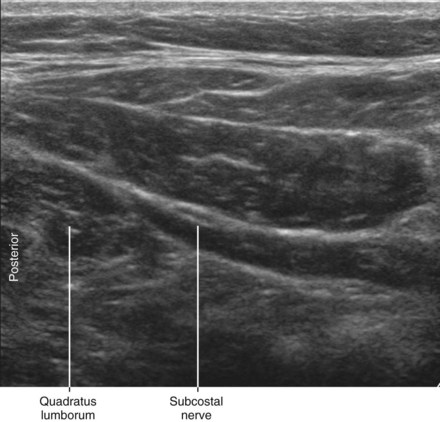
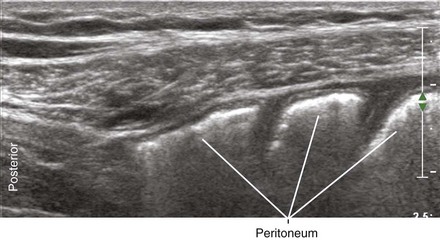
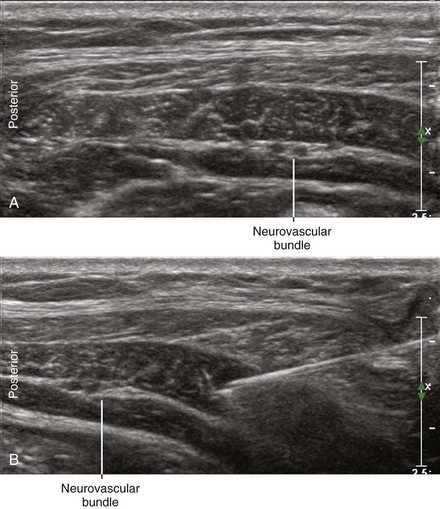
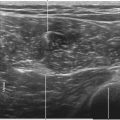
The first step in performing TAP blocks with ultrasound guidance is to identify the muscles of the anterolateral abdominal wall (Table 54-1). The external oblique is usually the most echogenic muscle of the anterolateral abdominal wall. The external oblique and internal oblique muscles typically extend farther posteriorly than the transversus abdominis muscle. Retroperitoneal fat (hypoechoic appearance on ultrasound scans) lies under the posterior aspect of the transversus abdominis muscle. The layers underneath the transversus abdominis muscle are (in order) the transversalis fascia, extraperitoneal fat, and peritoneum. The quadratus lumborum muscle is hypoechoic and therefore difficult to visualize on ultrasound scans (as is the retroperitoneal fat).
Table 54-1 Ultrasound Anatomy of the Anterolateral Abdominal Wall and Related Structures
| Structure | Sonography | Reference |
|---|---|---|
| Subcutaneous tissue | One or two layers | |
| External oblique | Often hyperechoic | |
| Internal oblique | Thickest muscle | Rankin et al |
| Transversus abdominis | Thinnest muscle | Rankin et al |
| Hypoechoic | Hebbard et al | |
| Retroperitoneal fat | Fibro-fatty echoes | Gore et al |
| Quadratus lumborum | Hypoechoic | Callen et al |
| Peritoneum | Very hyperechoic | Hanbidge et al |
| Comet-tail artifact | Thickman et al | |
| Gut sliding |
Rankin G, Stokes M, Newham DJ. Abdominal muscle size and symmetry in normal subjects. Muscle Nerve 2006;34:320–6; Hebbard PD, Barrington MJ, Vasey C. Ultrasound-guided continuous oblique subcostal transversus abdominis plane blockade: description of anatomy and clinical technique. Reg Anesth Pain Med 2010;35(5):436–41; Gore RM, Callen PW, Filly RA. Displaced retroperitoneal fat: sonographic guide to right upper quadrant mass localization. Radiology 1982;142(3):701–5; Callen PW, Filly RA, Marks WM. The quadratus lumborum muscle: a possible source of confusion in sonographic evaluation of the retroperitoneum. J Clin Ultrasound 1979;7(5):349–52; Hanbidge AE, Lynch D, Wilson SR. US of the peritoneum. Radiographics 2003;23:663–84; Thickman DI, Ziskin MC, Goldenberg NJ, et al. Clinical manifestations of the comet tail artifact. J Ultrasound Med 1983;2:225–30.
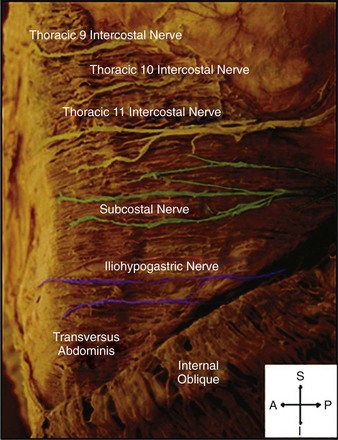
The nerves of the abdominal wall are most visible where they enter the TAP. In this location they are relatively large and shallow with the surrounding muscles providing contrast. The T11 and T12 (subcostal) nerves are often accompanied by intercostal arteries and can often be identified as they run within the TAP. The iliohypogastric and ilioinguinal nerves cross over the anterior surface of the quadratus lumborum muscle2 but are difficult to visualize in this anatomic location.
Suggested Technique
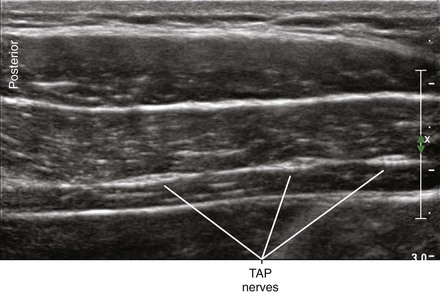
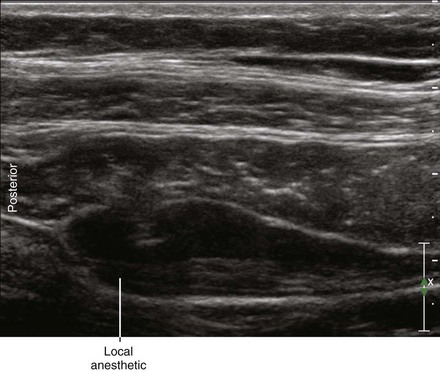
The nerves of the TAP are tacked down to the surface of the transversus abdominis muscle by fascia.3 Some therefore consider the optimal plane for infiltration of anesthetic to be between this fascial layer and the transversus abdominis muscle.3 Injections within the transversus abdominis muscle itself often result in successful block of nerves of the lower abdominal wall.4 The nerves of TAP are not solely confined to the plane between the internal oblique and transversus abdominis, but rather have a long-running (albeit limited) course within this plane.
Key Points
| Transversus Abdominis Plane Block | The Essentials |
|---|---|
| Anatomy | The nerves of the abdominal wall have a long-running course between IO and TA. |
| The subcostal nerve is often identified within the TAP. | |
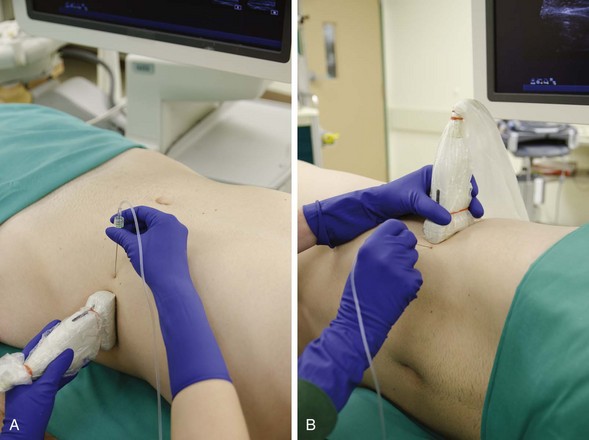
| Positioning | Supine or lateral |
| Operator | Standing at the side of the patient |
| Display transducer | Across the table |
| High- to medium-frequency linear, 38- to 50-mm footprint | |
| Initial depth setting | 35 to 40 mm |
| Needle | 21 gauge, 70 to 90 mm in length |
| Anatomic location | Begin by placing the transducer between the costal margin and iliac crest at the midaxillary line. |
| Identify the EO, IO, and TA muscle layers. | |
| Approach | Place the needle tip in the TA. |
| Advance through the posterior corner of the TA. | |
| Inject slowly as the needle is withdrawn. | |
| Sonographic assessment | The injection should layer between the TA and IO. |
| Anatomic variation | Anatomic variation in where nerves enter and exit the TAP is common. |
Clinical Pearls
• The characteristic distribution within the transversus abdominis plane is elliptical with well-defined margins.5 Side-to-side layering of the injection within the field of imaging is desired.
• TAP blocks are performed dorsal to the midaxillary line. The concern is that anteriorly placed injectates do not adequately distribute throughout the TAP.6
1 Petersen PL, Mathiesen O, Torup H, et al. The transversus abdominis plane block: a valuable option for postoperative analgesia? A topical review. Acta Anaesthesiol Scand. 2010;54(5):529–535. Epub 2010, Feb 17
2 Tubbs RS, Salter EG, Wellons JC, 3rd., et al. Anatomical landmarks for the lumbar plexus on the posterior abdominal wall. J Neurosurg Spine. 2005;2(3):335–338.
3 Rozen WM, Tran TM, Ashton MW, et al. Refining the course of the thoracolumbar nerves: a new understanding of the innervation of the anterior abdominal wall. Clin Anat. 2008;21(4):325–333. Review
4 Weintraud M, Marhofer P, Bösenberg A, et al. Ilioinguinal/iliohypogastric blocks in children: where do we administer the local anesthetic without direct visualization? Anesth Analg. 2008;106(1):89–93. Table of contents
5 Lee TH, Barrington MJ, Tran TM, et al. Comparison of extent of sensory block following posterior and subcostal approaches to ultrasound-guided transversus abdominis plane block. Anaesth Intensive Care. 2010;38(3):452–460.
6 Carney J, Finnerty O, Rauf J, et al. Ipsilateral transversus abdominis plane block provides effective analgesia after appendectomy in children: a randomized controlled trial. Anesth Analg. 2010;111(4):998–1003. Epub 2010 Aug 27