225 Transport Medicine
Critically ill patients occasionally need to be moved within an institution or between hospitals. Transport of critically ill patients is a procedure with risks and benefits. Neither the nature and magnitude of risk and benefits nor the variables that might mitigate risks and maximize benefit (e.g., team training and composition, mode of transport) have been well studied. Referral patterns for many diseases, including critical illness, are evolving around centers of excellence. The structure of transport systems and the body of transport research need to keep pace. In order to realize the benefits of regionalization of critical care services, intensivists must take an active role in designing the transport systems and maintaining quality assurance. (Please note that transport issues important to the management of mass casualties in disasters are addressed in Chapter 226.)
 Risks of Transport
Risks of Transport
The transport environment, given its limited resources and multiple distractions, is bound to be error prone. In a population-based retrospective cohort study of nearly 20,000 air-medical transports, significant adverse events (defined as death, need for major resuscitative measures, hemodynamic deterioration, inadvertent extubation, or respiratory arrest) occurred in 1 in 20 transports. Baseline hemodynamic instability and assisted ventilation before transport and duration of transport were independent predictors of adverse events.1 A retrospective review of voluntarily reported adverse events, which is likely to underestimate the true incidence, reported 11.3 adverse events occurred per 1000 flights.2 The error rate of 1.13% seems low relative to the 2.9% to 16.6% reported incidence of adverse events per hospitalization, but given that the duration of transport is measured in hours, not days, the incidence of adverse events per unit time is quite high.3
The most frequent cause of transport-related adverse events with potential for patient harm is inadequate communication.2 Communication errors are widely recognized to be a major preventable cause of morbidity and mortality in medicine in general. Because interfacility transport involves handoffs between at least three care teams, special care must be taken to ensure that critical details are transmitted. Complete documentation of all patient care records must be sent from the referring facility. Referring physicians should directly communicate the following to both the transport team and the accepting physician: (1) patient identification and medical history, (2) interventions performed during initial stabilization and the patient’s response, (3) pertinent physical examination findings, (4) ongoing therapy, and (5) complications that might occur during transport. The transport team must relay this information to the accepting physician, nurse (RN) and respiratory therapist (RT) in addition to information about the patient’s physiology and interventions performed while en route.
The incidence of adverse events in children is somewhat higher, ranging from 1.5% to 2.8% in transports with a specialized pediatric team to 20% to 61% in high-risk patients transported by nonspecialized teams. Adverse events in pediatric transport tend to be more serious. Airway-related events (loss of endotracheal tube, multiple intubation attempts, malposition of endotracheal tube) are by far the most common adverse event in pediatric transport, followed by loss of critical intravenous (IV) access, sustained hypotension, and cardiac arrest.4–6
 Rapid Transfer, Goal-Directed Therapy, and the Golden Hour
Rapid Transfer, Goal-Directed Therapy, and the Golden Hour
Emergency medical services (EMS) and regional flight teams tend to work under the assumption that the time between the moment of injury and arrival at a center capable of delivering definitive care is among the most important determinants of survival. This notion has been taught for 3 decades but is based on little or no evidence and has recently been scrutinized. Time from scene departure to arrival at the hospital was not associated with survival in out-of-hospital cardiac arrest, and transport time including scene time was not associated with survival in trauma.7,8 At the time the “golden hour” was conceived, prehospital care consisted of providing supplemental oxygen, a fast-moving vehicle, and minimal resuscitation. Under these circumstances, a worse outcome could be expected as prehospital time increased.
In pediatric patients, respiratory failure and shock are the most common reasons for transport. A recent study identified shock in 37% of children transferred to tertiary centers, regardless of reason for referral.9 In adults and children, protocolized, aggressive, early therapy of septic shock has proven vastly more effective than any pharmacologic intervention at improving mortality.10–12
Pediatric protocols recommend aggressive fluid resuscitation, initiation of inotropes, and administration of antibiotics within the first hour after presentation.13 The recommended treatments are simple interventions that can be initiated in community emergency departments (EDs) and continued and refined in transport, provided the treating physician and transferring team appreciate the urgent need and are sensitive to the subtle signs of shock in children. Han et al. reported that when community physicians aggressively resuscitated and successfully reversed shock before a transport team arrived, patients had a ninefold increase in their odds of survival.11 These studies defy the popular notion that out-of-hospital stabilization wastes time and delays definitive therapy that should be rendered at the receiving facility.
Although adult guidelines are more relaxed, there are no data to suggest that it is safe to delay goal-directed therapy for transport. In fact, in adults with septic shock, a delay in antibiotic therapy is associated with worse survival, with mortality increasing by 7% for every 30 minutes that passes without delivery of appropriate antibiotic therapy. The golden hour in transport is the time from presentation to initiation of appropriate treatment, treatments that should be initiated at the referring facility and continued and refined by the transport team.14
 Regionalization of Critical Care
Regionalization of Critical Care
Significant advances in therapeutic and diagnostic interventions for critically ill patients have occurred, but often at great cost and limited availability, prompting the need for transport of these patients to tertiary care centers. A recent consensus conference on prioritizing the organization and management of intensive care services in the United States (PrOMIS) suggested that intensive care would be optimally delivered in a tiered regionalized system.15 Ideally, regionalization would reduce practice variation, improve adherence to best practices, and reduce costs by realizing economies of scale. Regionalization would necessarily result in an increased number of transfers of critically ill patients from lower-volume to higher-volume centers, so the PrOMIS conference proposed that regionalization must be coupled with a regionalized emergency transportation system.
 Out-of-Hospital Transport
Out-of-Hospital Transport
Prehospital Transport
Out-of-hospital tracheal intubation by paramedics has recently come under fire. Despite the fact that tracheal intubation is the standard of airway management in the hospital and that tracheal intubation has been practiced by paramedics for 25 years, few studies support a survival benefit of tracheal intubation over bag-valve mask ventilation in the prehospital setting. Tracheal intubation is a complex skill rarely performed by paramedics. Failure rates are high, and multiple attempts are common; both of these may be accompanied by hypoxemia and other physiologic deterioration.16 When intubation is successful, tracheal tube dislodgement during transport by EMS is common; tracheal tube misplacement or dislodgement rate at the time of arrival to ED varies from 5.8% to 12% for adults to 25% for pediatrics.16–18 Finally, uncontrolled hyperventilation during manual ventilation by the EMS crew may be deleterious in head-injured patients and during cardiopulmonary resuscitation (CPR).
Appropriate utilization of resources (air versus ground units) for the prehospital transport of injured patients has been a subject of study and debate since the inception of air medical transport. In general, air medical transport is associated with both shorter transport intervals and a greater medical capability of the transporting team. The decision to use air transport in the prehospital setting should be supported by on-line medical control or preapproved protocols based on the factors of time, distance, geography, patient stability, and local resources. The National Association of Emergency Medical Service Physicians (NAEMSP) and the American College of Emergency Physicians (ACEP) have each recommended triage guidelines for on-scene helicopter transport.19 Retrospective studies have shown improved outcomes in patients transported by air, particularly major trauma patients and patients with severe traumatic brain injury.20–24 Defining the types of specific injuries or medical conditions that benefit from air medical transport has been difficult. As specialized cardiac and stroke centers have developed, air transport has begun to be utilized for rapid transport of these patients directly from the scene.
Interfacility Transport
In most areas at the time of this writing, regional critical care teams are synonymous with air medical transport teams. However, the U.S. military has developed critical care transport teams with significantly greater capabilities that may serve as a model for critical care specialty civilian teams. In the mid 1990s, the U.S. Air Force began to develop what has come to be called the critical care aeromedical transport team (CCATT.) The team consists of a nurse, respiratory therapist, and physician, all with experience in critical care as well as specific training pertinent to functioning in the transport environment. The teams carry resources to create a mobile ICU, including ventilators, mobile ultrasound equipment, and point-of-care laboratory testing. They go far beyond resuscitation and are able to recognize and manage multiple organ failures. The composition of these teams and details on the equipment and pharmacology they carry are described in an excellent article by Grissom and Farmer.25 In the military, these resource-intensive teams are routinely used to manage up to three critically ill patients in a single transport. Although this model cannot be precisely duplicated in the civilian world, the experience of these teams must be considered when transport systems are designed to support regionalization of critical care.
Issues Specific to Air Medical Transport
The helicopter environment is noisy, so auscultation of blood pressure and breath sounds in flight is difficult if not impossible.26 To monitor patients in flight, transport teams must rely on methods that do not depend on audible sounds: noninvasive blood pressure monitoring, capnometry, and pulse oximetry, to name a few.
Rotorcraft rarely fly at altitudes more than 2000 feet above ground level. At these altitudes, pressure changes have only a minor impact on the volume of air-filled spaces. The relatively small volume of air in the tracheal tube cuff may be subject to clinically significant pressure changes at that altitude. A recent prospective study found that 98% of patients had tracheal tube cuff pressures above 30 mm Hg, and 72% had intracuff pressures above 50 mm Hg during helicopter transport at a mean of 2260 feet.27 Tracheal tube cuff pressures should be measured and adjusted during flight.
Ventilators are calibrated for performance at sea level. Most flights maintain a cabin pressure equivalent to 6000 to 8000 feet. In the United States, Federal Aviation Administration regulations mandate cabin altitude less than 8000 feet. Ventilators that recognize and compensate for changes in barometric pressure exist (Uni-Vent Eagle Model 754 [Impact Instrumentation Inc., West Caldwell, New Jersey]) but are not in common use outside the military. Tidal volumes delivered by the LTV 1000 (Pulmonetic Systems Inc., Minneapolis, Minnesota), a commonly used transport ventilator, may vary from 5% to 12% at a simulated altitude of 4000 and 8000 in volume control mode. At 15,000 feet, LTV-delivered tidal volumes may be 30% to 37% greater than set tidal volumes.28 Similar findings have been reported with the Drager Oxylog ventilators (Dragger, Telford, Pennsylvania). Ventilators that use pneumatic circuits for respiratory rate control may deliver lower rates and increased tidal volumes at high altitude.29
 Structure of Regional and Specialty Retrieval Systems
Structure of Regional and Specialty Retrieval Systems
Communications
The communications center for the retrieval system should be easily accessible to both the referring physician and the transport team.8,30 It should be staffed around the clock by full-time communication specialists who have no distracting duties. The communication specialist should notify the appropriate personnel and arrange all aspects of the transport so the referring physician can direct his or her attention to patient care. A detailed log of transport requests including time, demographic data, diagnosis, and vehicle availability is kept both for administrative review and medicolegal documentation. Equipment for direct communication with the center should be available in every transport vehicle.
Staffing a Retrieval System
The administrative staff of a retrieval system should include, at a minimum, a program director, medical director, transport coordinator, and medical command.31,32 The program director is responsible for the structure, activities, and organization of the transport system and assumes overall program responsibilities; acts as a liaison between the team and hospital administration; and develops and implements quality management.
The medical director should be a licensed physician specialist in critical care or emergency medicine and might also have training in a surgical subspecialty (trauma) or in pediatrics (neonatology). The medical director should be experienced in both air and ground transport (as appropriate), understand patient care capabilities, and be familiar with limitations and stressors of the transport environment. The medical director must be actively involved in quality management, administrative decisions affecting medical care, and the hiring, training, and continuing education of all transport personnel, including physicians who provide on-line medical direction in policies, procedures, and patient care protocols. The transport medical director may also act as a liaison to the referral community for teaching and outreach.9,30
Medical crew composition varies between regional retrieval teams. More than 70% of medical flight crews consist of a nurse-paramedic team. Approximately 20% of programs use two nurses, and only 3% of programs routinely use a flight physician. Respiratory therapists are teamed with nurses in a small percentage of programs and may be particularly appropriate in critical care transport teams.31 Flight nurses typically have extensive experience in the ED or ICU.
Flight physicians are usually emergency medicine residents. In a few programs, they may be attending physicians or medical directors of flight programs. The use of physicians in these services as flight crew members is indicated when the physician might contribute significantly to the care provided in flight. Studies suggest that specific physician judgment or skill may be required in approximately 25% of transports.20,33,34
 Responsibilities of the Referring Hospital
Responsibilities of the Referring Hospital
In the United States, the transfer of patients from one institution to another is regulated by federal statute. The Consolidated Omnibus Budget Reconciliation Act of 1986 (COBRA) and its amendment, the Omnibus Reconciliation Act of 1989, set the current legal standard for patient stabilization and transfer.35,36 In an attempt to guarantee equal access to emergency treatment regardless of a patient’s ability to pay, COBRA attributes responsibility for the patient’s transfer to the referring hospital and physician. Violations can result in a number of penalties, including termination of Medicare privileges for the physician and hospital. The Emergency Medical Treatment and Labor Act established by the COBRA legislation governs how patients may be transferred from one hospital to another. Hospitals cannot transfer patients unless the transfer is “appropriate,” the patient consents to transfer after being informed of the risks of transfer, and the referring physician certifies that the medical benefits expected from the transfer outweigh the risks. Appropriate transfers meet the following criteria: (1) the transferring hospital must provide care and stabilization within its ability, (2) copies of medical records and imaging studies must accompany the patient, (3) the receiving facility must have available space and qualified personnel and agree to accept the transfer, and (4) the interfacility transport must be made by qualified personnel with the necessary equipment. It is the responsibility of the referring physician, in consultation with the receiving physician, to choose a mode of transport from among the available teams.
 Unique Aspects of Pediatric Transport
Unique Aspects of Pediatric Transport
EMS Cannot Provide Ideal Care for All Children
The majority of children are transported by EMS providers with variable educational backgrounds and experience. Currently there are no national regulations for EMS as they relate to children. Pediatric guidelines for EMS are just beginning to evolve from the various national organizations that represent children.37
Limited pediatric training coupled with limited exposure to pediatric patients may hamper the ability of EMS providers to respond appropriately to pediatric emergencies. In 2000, nationally registered paramedics received a median 358 total hours of instruction, less than 5% of which was dedicated to pediatrics. Most paramedics in this study were not required to take pediatric continuing medical education (CME) training.18 Less than 10% of all EMS transports nationwide are for infants and children; 12% of those involve advanced life support, and even fewer provide critical care.38,39 Overall, this translates into 3 pediatric patients per month for 60% of the nation’s paramedics. Although pediatric advanced life support training has been associated with an improvement in ability to secure a pediatric airway or to obtain vascular or intraosseous access, this training is not required for EMS technicians.40
Babl and associates demonstrated that in a program with 50 active ALS providers in the current milieu of EMS, each provider would be expected to have one pediatric bag-valve-mask case every 1.7 years, one pediatric intubation every 3.3 years, and one intraosseous cannulation every 6.7 years.41 Without repeated reinforcement, cognitive and interventional skills deteriorate over time. The poor performance of paramedics in advanced airway management in children is well documented and has led to recommendations that EMS crews avoid tracheal intubation in favor of bag-valve mask ventilation.42
Gausche et al. found that children in the field who were younger than 14 years were more likely to be undertreated compared to adults (33% versus 3%).43 Studies of pediatric trauma victims make it clear that prehospital providers could do a better job with children. Children were twice as likely to die of trauma in the field compared with adults, a finding attributed to the lack of pediatric training.38,42,44
Finally, referring hospitals are often not equipped to care for critically ill and injured children. Two independent studies reported that as recently as 2003, only 6% of emergency rooms were appropriately equipped to care for children. Items frequently unavailable included laryngeal mask airways and infant and neonatal equipment.44 Esposito and coworkers found that frequent errors occur in ED management of pediatric trauma, leading to about 9% preventable mortality.45 They reported a 64% error rate in management of children, including gross violations of basic trauma care. Han et al. found that resuscitation practice in a community ED was consistent with American College of Critical Care Medicine Pediatric Advanced Life Support (ACCM-PALS) guidelines in only 30% of children who presented with septic shock.11
Specialized Teams Improve Outcome
Early investigations of the use of specialized teams for interfacility transport of neonates and children found improved hemodynamic stability and fewer preventable insults with the use of specialized teams.46–49 In a case-control study of preventable insults in head-injured children, Macnab et al. determined that the increase in adverse events with transport by nonspecialty teams resulted in $135,952 in additional costs of care.49 Most importantly, two recent studies have documented an improvement in risk-adjusted mortality with the use of specialized teams for interhospital transfer of pediatric patients.50,51
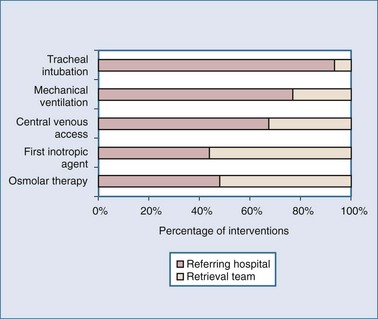
Pediatric specialized teams bring ICU care to the patient and often perform additional stabilization maneuvers, including upon arrival at the referring facility. In a prospective observational study, pediatric teams initiated sedation 23% of the time, inotropes 44% of the time, and osmolar therapies for intracranial hypertension nearly 50% of the time when the referring facility had failed to do so. Retrieval teams also initiated mechanical ventilation, acquired central venous access, and placed or adjusted tracheal tubes52 (Figure 225-1). Time at the bedside for specialized retrieval teams can be relatively long (97 minutes for neonates and 50 minutes for pediatric patients) because of these interventions, but scene time is not associated with mortality.46,53
Delivery of goal-directed therapy may be hampered by the inability of practitioners to recognize shock. Infants and children have a greater capacity to increase systemic vascular resistance in shock states and tend to preserve blood pressure until very late in the evolution of shock.54 Pediatric shock resuscitation protocols developed by a consensus of experts in the field call for symptomatic treatment of shock using clinical signs including age-specific targets for heart rate and blood pressure and relatively subtle indicators of perfusion as therapeutic endpoints.13 Specialized pediatric teams may be more capable of recognizing deviation from age-specific norms and recognizing the subtle signs of compensated shock in children.
 In-Hospital Transport
In-Hospital Transport
Recent Research
Critically ill adults who require transport out of the ICU for interventions or diagnostic procedures have higher admission severity-of-illness scores with the attendant increase in use of critical care resources than those who do not require transport.55 Because of this, it is difficult to assess the clinical impact of physiologic derangements reported in early evaluations of the safety of in-hospital transport. Still, it is clear that unplanned events are common. In a prospective observational study of in-hospital transports of critically ill patients from the ED, 68% of transports were associated with one or more unplanned events, mostly equipment failures. In the same study, serious unplanned events (hypotension, need for intubation, or elevated intracranial pressure) occurred in 5% of transports.56 High level of experience in the accompanying physician was associated with decreased frequency of unplanned events. A similar series of transports of critically ill patients from the ED to the ICU reported changes in cardiorespiratory physiology requiring intervention in 6% of transports.57
General Principles of In-Hospital Transport
Specific guidelines for in-hospital transport have been published by the American Society for Critical Care Medicine. The general principles of in-hospital transport are the same as those for interfacility transport.58 Patients who require transport from the ICU for procedures and diagnostic studies are sicker on the whole than patients requiring interfacility transport. Patients should be stabilized before the trip. Potential causes of deterioration during transport should be included in planning. Particular attention must be paid to maintenance of hypothermia in patients to whom this therapy has been applied, since rapid rewarming can be devastating to the injured brain. The need for additional sedation should be anticipated. Transfer of critically ill patients to another location should be treated as an extension of intensive care. In the sickest patients, mechanical ventilation is superior to hand ventilation. Adequate medical supervision should be provided during the entire in-hospital transport. Some studies have documented a decrease in unplanned events with greater experience level of the accompanying physician.55
Key Points
Grissom TE, Farmer JC. The provision of sophisticated critical care beyond the hospital: lessons from physiology and military experiences that apply to civil disaster medical response. Crit Care Med. 2005;33:S13-S21.
Han YY, Carcillo JA, Dragotta MA, et al. Early reversal of pediatric-neonatal septic shock by community physicians is associated with improved outcome. Pediatrics. 2003;12:793-799.
Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368-1377.
Warren J, Fromm REJr, Orr RA, Rotello LC, Horst HM. American College of Critical Care Medicine. Guidelines for the inter- and intrahospital transport of critically ill patients. Crit Care Med. 2004;32:256-262.
Orr RA, Felmet KA, Han Y, McCloskey KA, Dragotta MA, Bills DM, et al. Pediatric specialized transport teams are associated with improved outcomes. Pediatrics. 2009;124:40-48.
1 Singh JM, MacDonald RD, Bronskill SE, Schull MJ. Incidence and predictors of critical events during urgent air-medical transport. CMAJ. 2009;181(9):579-584.
2 MacDonald RD, Banks BA, Morrison M. Epidemiology of adverse events in air medical transport. Acad Emerg Med. 2008;15(10):923-931.
3 Baker GR, Norton PG, Flintoft V, Blais R, Brown A, Cox J, et al. The Canadian Adverse Events Study: the incidence of adverse events among hospital patients in Canada. CMAJ. 2004;170(11):1678-1686.
4 Edge WE, Kanter RK, Weigle CG, Walsh RF. Reduction of morbidity in interhospital transport by specialized pediatric staff. Crit Care Med. 1994;7:1186-1191.
5 Philpot C, Day S, Marcdante K, Gorelick M. Pediatric interhospital transport: diagnostic discordance and hospital mortality. Pediatr Crit Care Med. 2008;9(1):15-19.
6 Orr RA, Felmet KA, Han Y, McCloskey KA, Dragotta MA, Bills DM, et al. Pediatric specialized transport teams are associated with improved outcomes. Pediatrics. 2009;124(1):40-48.
7 Spaite DW, Stiell IG, Bobrow BJ, de Boer M, Maloney J, Denninghoff K, et al. Effect of transport interval on out-of-hospital cardiac arrest survival in the OPALS study: implications for triaging patients to specialized cardiac arrest centers. Ann Emerg Med. 2009;54(2):248-255.
8 Newgard CD, Schmicker RH, Hedges JR, Trickett JP, Davis DP, Bulger EM, et alResuscitation Outcomes Consortium Investigators. Emergency medical services intervals and survival in trauma: assessment of the “golden hour” in a North American prospective cohort. Ann Emerg Med. 2010;55(3):235-246.
9 Carcillo JA, Kuch BA, Han YY, Day S, Greenwald BM, McCloskey KA, et al. Mortality and functional morbidity after use of PALS/APLS by community physicians. Pediatrics. 2009;124(2):500-508.
10 de Oliveira CF, de Oliveira DS, Gottschald AF, et al. ACCM/PALS haemodynamic support guidelines for paediatric septic shock: an outcomes comparison with and without monitoring central venous oxygen saturation. Intensive Care Med. 2008;34(6):1065.
11 Han YY, Carcillo JA, Dragotta MA, et al. Early reversal of pediatric-neonatal septic shock by community physicians is associated with improved outcome. Pediatrics. 2003;12:793-799.
12 Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368-1377.
13 Brierley J, Carcillo JA, Choong K, et al. Clinical practice parameters for hemodynamic support of pediatric and neonatal septic shock: 2007 update from the American College of Critical Care Medicine. Crit Care Med. 2009;37(2):666-688.
14 Kumar A, Roberts D, Wood KE, et al. Duration of hypotension prior to initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med. 2006;34:1589.
15 Barnato AE, Kahn JM, Rubenfeld GD, McCauley K, Fontaine D, Frassica JJ, et al. Prioritizing the organization and management of intensive care services in the United States: the PrOMIS Conference. Crit Care Med. 2007;35(4):1003-1011.
16 Jones JH, Murphy MP, Dickson RL, Somerville GG, Brizendine EJ. Emergency physician-verified out-of-hospital intubation: miss rates by paramedics. Acad Emerg Med. 2004;11(6):707-709.
17 Jemmett ME, Kendal KM, Fourre MW, Burton JH. Unrecognized misplacement of endotracheal tubes in a mixed urban to rural emergency medical services setting. Acad Emerg Med. 2003;10(9):961-965.
18 Katz SH, Falk JL. Misplaced endotracheal tubes by paramedics in an urban emergency medical services system. Ann Emerg Med. 2001;37(1):32-37.
19 National Association of EMS Physicians (NAEMSP). Air Medical Dispatch: Guidelines for Trauma Scene Response. Lenexa, KS: National Association of EMS Physicians; 1992.
20 Baxt WG, Moody P. The impact of a physician as part of the aeromedical emergency care service on trauma mortality. JAMA. 1987;257:3246-3250.
21 Moylan JA, Fitzpatrick KT, Beyer AJ3rd, et al. Factors improving survival in multisystem trauma patients. Ann Surg. 1988;207:679-685.
22 McVey J, Petrie DA, Tallon JM. Air versus ground transport of the major trauma patient: a natural experiment. Prehosp Emerg Care. 2010;14(1):45-50.
23 Davis DP, Peay J, Serrano JA, Buono C, Vilke GM, Sise MJ, et al. The impact of aeromedical response to patients with moderate to severe traumatic brain injury. Ann Emerg Med. 2005;46(2):115-122.
24 Thomas SH, Harrison TH, Buras WR, et al. Helicopter transport and blunt trauma mortality: A multicenter trial. J Trauma Injury Infect Crit Care. 2010;52:136-145.
25 Grissom TE, Farmer JC. The provision of sophisticated critical care beyond the hospital: lessons from physiology and military experiences that apply to civil disaster medical response. Crit Care Med. 2005;33(1 Suppl):S13-S21.
26 Hunt RC, Bryan DM, Brinkley VS. Inability to assess breath sounds during air medical transport by helicopter. JAMA. 1991;265:1982-1984.
27 Bassi M, Zuercher M, Erne JJ, Ummenhofer W. Endotracheal tube intracuff pressure during helicopter transport. Ann Emerg Med. 2010;56(2):89-93.
28 Rodriquez DJr, Branson RD, Dorlac W, Dorlac G, Barnes SA, Johannigman JA. Effects of simulated altitude on ventilator performance. J Trauma. 2009;66(4 Suppl):S172-S177.
29 Flynn JG, Singh B. The performance of Dräger Oxylog ventilators at simulated altitude. Anaesth Intensive Care. 2008;36(4):549-552.
30 Maguire BJ, Hunting KL, Smith GS, Levick NR. Occupational fatalities in emergency medical services: a hidden crisis. Ann Emerg Med. 2002;40:625-632.
31 Accreditation Standards of the Commission on Accreditation of Air Medical Services. 2nd ed. Anderson, SC: The Commission; 2002.
32 American Academy of Pediatrics section on transport medicine: Guidelines for air and ground transport of neonatal and pediatric patients. 3rd ed. Elk Grove Village, IL: American Academy of Pediatrics; 2006.
33 Garner A. Addition of physicians to paramedic helicopter services decreases blunt trauma mortality. Aust NZ J Surg. 1999;69:697-701.
34 Schoettker P. Ejection as a key word for the dispatch of a physician staffed helicopter: The Swiss experience. Resuscitation. 2001;49:169-173.
35 Fell MJ. The Emergency Medical Treatment and Active Labor Act of 1986: Providing protection from discrimination in access to emergency medical care. Spec Law Dig Health Care Law. 1996;204:9-42.
36 Omnibus Budget Reconciliation Act of 1989, sec. 6018 42 USC 1395cc (West Suppl. 1990).
37 Guidelines for pediatric equipment and supplies for emergency departments. Committee on pediatric equipment and supplies for emergency. Ann Emerg Med. 1998;31:54-57.
38 Seidel JS. A needs assessment of advanced life support and emergency medical services in the pediatric patient: state of the art. Circulation. 1986;74:129-173.
39 Glaeser PW, Linzer J, Tunik MG, et al. Survey of nationally registered emergency medical services providers: Pediatric education. Ann Emerg Med. 2000;36:33-38.
40 Baker TW, King W, Soto W, Asher C, Stolfi A, Rowin ME. The efficacy of pediatric advanced life support training in emergency medical service providers. Pediatr Emerg Care. 2009;25(8):508-512.
41 Babl FE, Vinci RJ, Bauchner H, et al. Pediatric prehospital advanced life support care in an urban setting. Pediatr Emerg Care. 2001;17:36-37.
42 Gerritse BM, Draaisma JM, Schalkwijk A, van Grunsven PM, Scheffer GJ. Should EMS-paramedics perform paediatric tracheal intubation in the field? Resuscitation. 2008 Nov;79(2):225-229. 25
43 Gausche M. Out-of-hospital intravenous access: Unnecessary procedures and excessive cost. Acad Emerg Med. 1998;5:878-882.
44 Middleton KR, Burt CW. Availability of pediatric services and equipment in emergency departments: United States, 2002-03. Adv Data. 2006;367:1-16.
45 Esposito TJ, Sanddal ND, Dean JM, et al. Analysis of preventable pediatric trauma deaths and inappropriate trauma. J Trauma. 1999;47:243-251.
46 Macnab AJ. Optimal escort for interhospital transport of pediatric emergencies. J Trauma. 1991;31:205-209.
47 Edge WE, Kanter RK, Weigle CG, et al. Reduction of morbidity in interhospital transport by specialized pediatric staff. Crit Care Med. 1994;22:1186-1191.
48 Orr R, Venkataraman S, Seidberg N, et al. Pediatric specialty care teams are associated with reduced morbidity during pediatric interfacility transport. Crit Care Med. 1999;27:A30.
49 Macnab AJ, Wensley DF, Sun C. Cost-benefit of trained transport teams: estimates for head-injured children. Prehosp Emerg Care. 2001;5:1-5.
50 Orr RA, Felmet KA, Han Y, et al. Pediatric specialized transport teams are associated with improved outcomes. Pediatrics. 2009;124(1):40-48.
51 Ramnarayan P, Thiru K, Parslow R, Harrison DA, Draper ES, Rowan KM. Effect of specialist retrieval teams on outcomes in children admitted to paediatric intensive care units in England and Wales: a retrospective cohort study. The Lancet. 2010;376(9742):698-704.
52 Lampariello S, Clement M, Aralihond AP, Lutman D, Montgomery MA, Petros AJ, et al. Stabilisation of critically ill children at the district general hospital prior to intensive care retrieval: a snapshot of current practice. Arch Dis Child. 2010;95(9):681-685.
53 Abdel-Latif ME, Berry A. Analysis of the retrieval times of a centralised transport service, New South Wales, Australia. Arch Dis Child. 2009;94(4):282-286.
54 Pediatric advanced life support provider manual. Dallas: American Heart Association, 2002.
55 Voigt LP, Pastores SM, Raoof ND, Thaler HT, Halpern NA. Review of a large clinical series: intrahospital transport of critically ill patients: outcomes, timing, and patterns. J Intensive Care Med. 2009;24(2):108-115.
56 Papson JP, Russell KL, Taylor DM. Unexpected events during the intrahospital transport of critically ill patients. Acad Emerg Med. 2007;14(6):574-577.
57 Gillman L, Leslie G, Williams T, Fawcett K, Bell R, McGibbon V. Adverse events experienced while transferring the critically ill patient from the emergency department to the intensive care unit. Emerg Med J. 2006;23(11):858-861.
58 Warren J, Fromm REJr, Orr RA, Rotello LC, Horst HM, American College of Critical Care Medicine. Guidelines for the inter- and intrahospital transport of critically ill patients. Crit Care Med. 2004;32(1):256-262.