Transitioning the Jumping Athlete Back to the Court
Christine Prelaz
Lower extremity injuries are prevalent in athletics. These injuries can range from minor sprains or strains to those that result in significant functional limitation and loss of time from work and/or sport.1 An estimated 3 to 5 million injuries occur each year among recreational and competitive athletes in the United States1 with the worldwide annual cost being estimated at $1 billion.2 The National Collegiate Athletic Association (NCAA) reported that more than 50% of injuries occurred in the lower extremity with the most common sites being the ankle and knee over a 16-year period.3 These data come from the NCAA Injury Surveillance System, which summarized surveillance data for 15 NCAA sports over a 16-year period.3 Research studies indicate that both intrinsic and extrinsic factors play a role in sustaining lower extremity injuries.2,4 Recent attention in the literature has focused on identifying modifiable and nonmodifiable associated risks with the overall goal of reducing such injuries. Given the frequency and cost of these injuries, the clinician is challenged not only with restoring function of the injured athlete but also with implementing interventions to prevent future injury. In today’s competitive environment, the health care team is faced with higher levels of pressure from the athlete, coaches, and parents to return the athlete back to sport as expediently and as safely as possible. Ongoing assessment and proper program design based on current evidence-based research can provide the clinician with the best information possible and guide him or her to determine an athlete’s readiness to return to sport.
Program Design
Numerous lower extremity rehabilitation protocols exist for both conservative management and surgical procedures. Each clinician has his or her unique approach to the rehabilitation of a specific athletic injury. For example, a survey of practices in ACL reconstruction by the American Orthopedic Society for Sports Medicine showed that rehabilitation protocols were the most variable factor among other practice factors that were surveyed.5 Other factors included in the survey were weight bearing, immobilization, bracing, length of physical therapy, and when to return to a sport. Such variability in protocols can lead to confusion as to what is appropriate and/or foster the practice of a “one size fits all” rehabilitation approach. Whatever the injury, a team approach consisting of close communication between the physician, physical therapist, athletic trainer, and other medical specialists should provide the best environment for returning the athlete to the sport. The clinician must have a comprehensive understanding of the structures involved, the surgical procedures, surgeon preferences, and tissue healing constraints. Because it is beyond the scope of this chapter to outline a program for each specific sport or injury, the goal of this chapter is to provide general rehabilitation guidelines, ideas, and resources for returning jumping athletes back to their respective sports successfully and safely.
Readiness to Prepare for Return
Regardless of the injury or surgical procedure, it is the clinician’s responsibility to determine the athlete’s level of readiness to progress to each phase of rehabilitation.
Continual monitoring of tissue tolerance by the clinician as the athlete progresses through each rehabilitation phase is critical. Knowledge of the type and extent of injury, surgical procedure, pain levels, swelling, ROM, strength, endurance, flexibility, patient’s goals, and psychologic readiness are all factors that should assist in the clinical decision process.
Individual goals must be set for each athlete dependent upon his or her current functional level, the level of competition to which they are to return, and the specific sport of the athlete. In general, the goals of the training program are to restore and/or improve flexibility, endurance, strength, balance, and agility. Once the athlete has completed his or her acute phase rehabilitation, the concept of a needs analysis may assist in establishing more sports-specific goals. The needs analysis takes into account the fitness needs of both the activity/sport and the individual athlete, thus designing a more customized versus a “cook book” program. To develop a needs analysis, both a physiologic and biomechanical analysis must be completed. When considering a specific event, one must look at the muscles involved, the energy system needs, speed/strength/power/endurance requirements, and any other specific needs of the event itself.6 Next, the current status and prior history of the athlete is determined and a program is then designed to progress him or her toward those specific goals. Sport-specific training is fundamental in returning the athlete back to his or her respective sport. The rehabilitation program should incorporate a whole body approach including core strengthening and exercises for the noninjured extremity.
Flexibility
Controversy exists in the literature regarding static stretching.7 Several studies have shown that there is little evidence to support its role in injury prevention and determined that preexercise static stretching may actually negatively affect performance.8 Some researchers found decreases in muscle strength9 and decreases in jumping ability10 after passive stretching. The concept of using a dynamic warm-up instead of static stretching has gained popularity in both the literature and on the field. Some of the proposed benefits of a dynamic warm-up versus static stretching are that the muscles are in more continuous movement, thus increasing the overall temperature and achieving a more “true warm-up.” Dynamic stretching can also use more sports-specific movements to incorporate balance and motor control and mental preparation for the athlete, which may help to prime the neuromuscular system for the upcoming event.11 A few examples of dynamic warm-up exercises are heel/toe walking, marching, skipping, long leg kicks, gluteal kicks, lunge walking, carioca, and lateral slides. This does not mean that static stretching should be abandoned, however. Shrier8 contends that regular stretching as part of a comprehensive program and not before exercise can increase force, jump height, and speed.8 Athletes who need greater range of motion or need to increase overall flexibility may still benefit from static stretching (Box 33-1). Stretching after activity may also tend to relax the tissues and prevent general postactivity stiffness.
Strength
Before starting any training program, it is important to have a full understanding of the demands of the sport and the individual athlete. The needs analysis will enable the clinician to design a comprehensive specific program to develop strength, endurance, power, speed, agility, and balance.
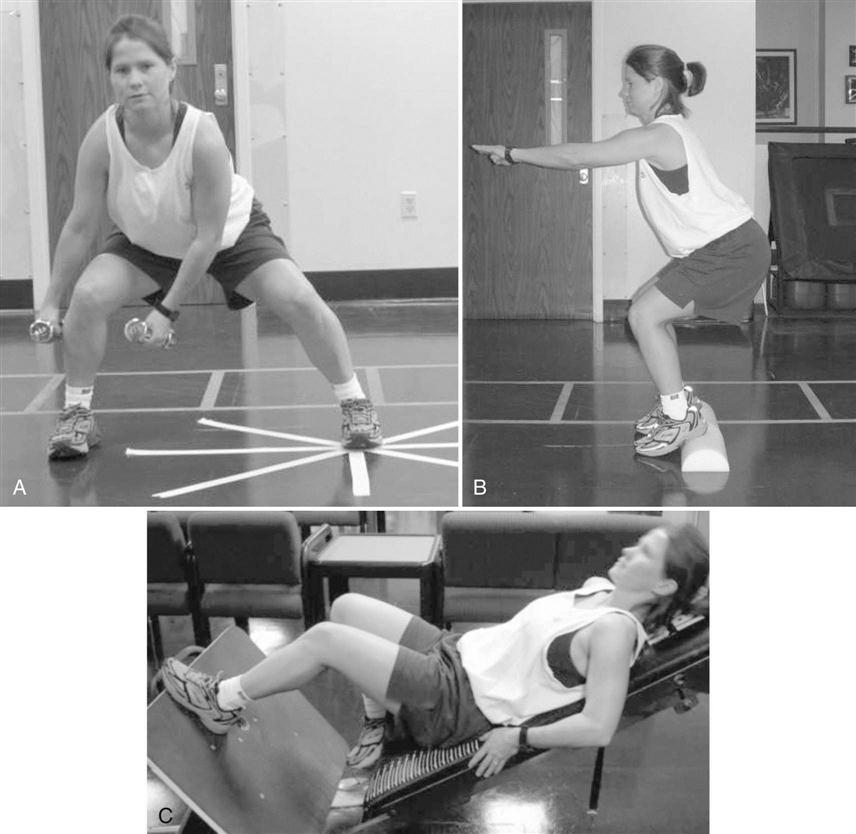
Special considerations must be given to injured athletes with regard to strengthening. Rehabilitation of knee injuries in particular has presented the clinician with a challenge. For example, the main goal of rehabilitation following ACL reconstruction is to restore lower extremity strength while protecting the reconstructed graft and the patellofemoral joint from excessive stresses. Selective quadriceps muscle atrophy occurs following injury and/or immobilization. Strength deficits in the quadriceps of up to 10% have been reported by Shelbourne and associates12 at an average follow-up of 4 years following ACL surgery. Debate exists between the uses of open kinetic chain (OKC) versus closed kinetic chain (CKC) exercises to build quadriceps strength (Fig. 33-1). Several authors have advocated the use of both after ACL reconstruction.13,14 A literature review by Ross and associates15 on OKC versus CKC exercises following ACL reconstruction indicates that the greatest amount of ACL strain and patellofemoral joint stress occurs at approximately 40° of knee flexion to full extension.16,17 It was therefore recommended that OKC exercises for quadriceps strengthening be performed with knee angles greater that 40° to avoid excessive stress on these structures. Closed chain activities beyond 60° were to be avoided since maximum stress on the patellofemoral joint occurs between 60° and 90° of flexion.17
Because of the predominant atrophy of type I (slow twitch) muscle fibers following injury or immobilization, high repetitions (6 to 10 sets, 12 to 15 repetitions) with low resistance is recommended early in the rehabilitation program.15 Establishing normal muscle balance for both involved and uninvolved limbs is one of the primary goals. A comprehensive strength training program should address core, hip, calf, and ankle musculature, as well as establish appropriate quadriceps/hamstring ratios. Strengthening of the hamstrings using both closed and open chain methods is important because of their role in assisting in the control of anterior tibial translation. Traditional and functional techniques can be incorporated for both variety and effectiveness (Box 33-2).
There has been an increasing amount of literature in recent years regarding the relationship of hip and core strength as factors in lower extremity injuries. Unfortunately, this relationship is not quite clear. For example, weakness of the hip abductors and external rotators has been shown to contribute to increased hip adduction and internal rotation motion observed in female runners with patellofemoral pain or iliotibial band syndrome. However, it has also been shown that these motion abnormalities can exist even though no strength deficits are present. This indicates an apparent disconnect between muscle strength and observed abnormal kinematics in some cases. Therefore, it has been suggested that additional factors such as altered proprioception and neuromuscular control of the lumbo-pelvic and hip regions should also be considered in the clinical assessment and treatment plan of individuals with lower extremity injuries.18
Plyometrics
General Principles
Plyometric exercises use the stretch-shortening cycle to store potential energy. The stretch-shortening cycle consists of the eccentric phase where preloading occurs as the muscle is placed on stretch, thus storing potential energy. The amortization phase refers to the time period between the eccentric and concentric contraction. The amortization phase must be kept short; the longer it is, the greater the loss of stored energy. The final phase is the concentric phase, in which the stored energy is used in an opposite reaction (i.e., the muscle contracts concentrically to provide the force necessary for the required movement).19
When designing a plyometric training program, consideration must be given to age, body weight, current strength and conditioning level, experience, previous injury, and demands of the sport (Boxes 33-3 through 33-5).19,20
Warm Up/Cool Down
Warm-up exercises can consist of a combination of general and specific skill enhancement drills such as marching, skipping, shuffling, and footwork drills.20 Static and dynamic stretching should also be performed.
Proper Technique
Proper instruction and monitoring of technique is critical not only for proper neuromuscular retraining but also to avoid injury. Verbal, visual, and manual cues may be used to teach the athlete proper control. If the athlete fails to demonstrate proper control during any part of the exercise, he or she should be stopped and given a brief rest period before continuing. If improper technique is still present, the exercise should be discontinued for that session. Explaining and reinforcing the importance of proper technique to the athlete will help to prevent overuse and injury during the training program.
Frequency
Perform one to three sessions per week. Two sessions is the norm for most off-season sports programs.21 Frequency should be determined by the intensity of the sessions and the phase of rehabilitation or cycle in the sport season.
Volume
Volume is expressed in number of foot contacts per workout. Volume should be 60 to 100 foot contacts for beginners; 100 to 150 for intermediate level and 120 to 200 for advanced off-season workouts.20 If intensity is high, volume should be low to medium. Volume may also be expressed as a specific distance.21 Adjust the number of contacts down for younger, inexperienced or postinjury individuals. Elite athletes may perform 200 to 400 foot contacts.19
Intensity
Intensity refers to the amount of stress on the tissues during the plyometric activity. It can be classified as low (Fig. 33-2), medium, or high (Fig. 33-3). ![]() In general, as intensity increases, volume should decrease. Athletes weighing more than 220 lb should not perform depth jumps from heights greater than 18 inches.19
In general, as intensity increases, volume should decrease. Athletes weighing more than 220 lb should not perform depth jumps from heights greater than 18 inches.19
Progression
Adequate strength and conditioning levels should be present before the athlete can progress. It is recommended that the athlete be able to squat 1.5 times body weight before starting shock types of plyometric training such as depth jumps.22 Progression should be based on a current evaluation of the athlete, the establishment of sport-specific goals, attainment of proper technique and control, and the absence of any signs or symptoms of overuse. In general, the following progression guidelines are suggested to avoid overtraining and to prevent injury during the plyometric program23:
Recovery
Adequate recovery time must be given between repetitions and sets, as well between workout sessions. Plyometrics are not intended to be an aerobic conditioning workout. Rest time between repetitions and sets is dependent upon the intensity of the exercise and the individual. Allow 30 seconds up to 3 minutes for recovery.19 Plyometric sessions should not be performed on consecutive days. In general, plyometric workouts should allow 48 to 72 hours between sessions.24
Direction of Motion
A needs analysis should determine if the sport requires speed and power in a vertical plane, horizontal plane, lateral or diagonal directions, or a combination. Most sports require a combination of directions. Drills that specifically enhance the required components of the sport should be chosen for the program.
Proper technique and control is crucial before progressing to the next level.
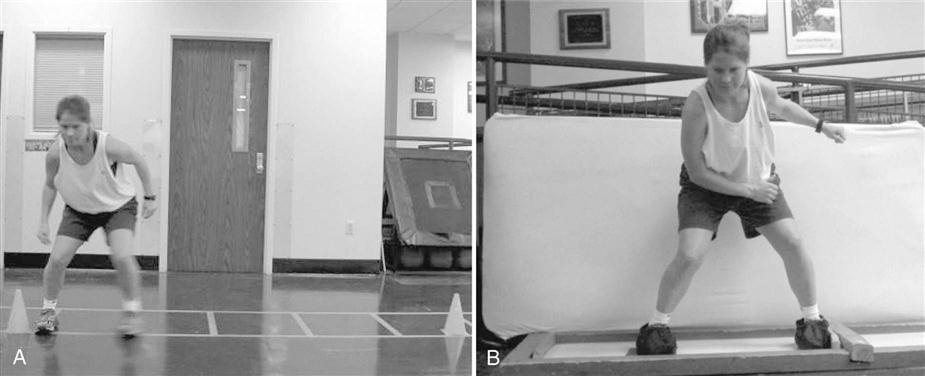
Speed and Agility
Agility is the ability to rapidly change body direction, accelerate, or decelerate. It is influenced by balance, strength, coordination, and skill level. Agility can be improved by first developing an adequate base of strength and conditioning that is appropriate for the difficulty level of the athlete. After this is achieved, drills designed to enhance reactive and explosive motor skills can be progressively incorporated (Fig. 33-4).
Guidelines for speed and agility training are as follows:
• The athlete should have an appropriate strength/conditioning base for the selected drills
• Allow adequate rest between sets and repetitions. Heart rate and respiration should return to almost normal levels after the drill. A 1 : 4-6 work-to-rest ratio is recommended.22
Box 33-6 lists various speed and agility drills. This list provides examples only; the reader may wish to refer to specific resources on speed, agility, and plyometric training for a more comprehensive list and description of drills.20,22,25,26
Neuromuscular Training
Neuromuscular control is the ability to produce controlled movement through coordinated muscle activity.27 It is the efferent motor response to sensory input from the somatosensory (proprioceptive and kinesthetic) system, the visual system, and the vestibular system. Stability is achieved by continuous feedback to the central nervous system from the integration of input from these three systems. The somatosensory system uses several different types of sensory input from proprioceptors and the sensory nerve terminals found in muscles, tendons, and joint capsules. Proprioceptors relay information relating to movement and position sense.
Visual input received in the cortex and vestibular nuclei provides information for the vestibular and somatosensory systems to make adjustments to maintain stability and balance. Dynamic joint stability is the ability of the joint to remain stable under the rapidly changing loads during activity.27
Following an injury, deafferentation to ligament and capsular mechanoreceptors may occur. The presence of tissue swelling and pain can also compound sensory damage by disrupting sensory feedback that can alter reflexive joint stabilization and neuromuscular coordination.
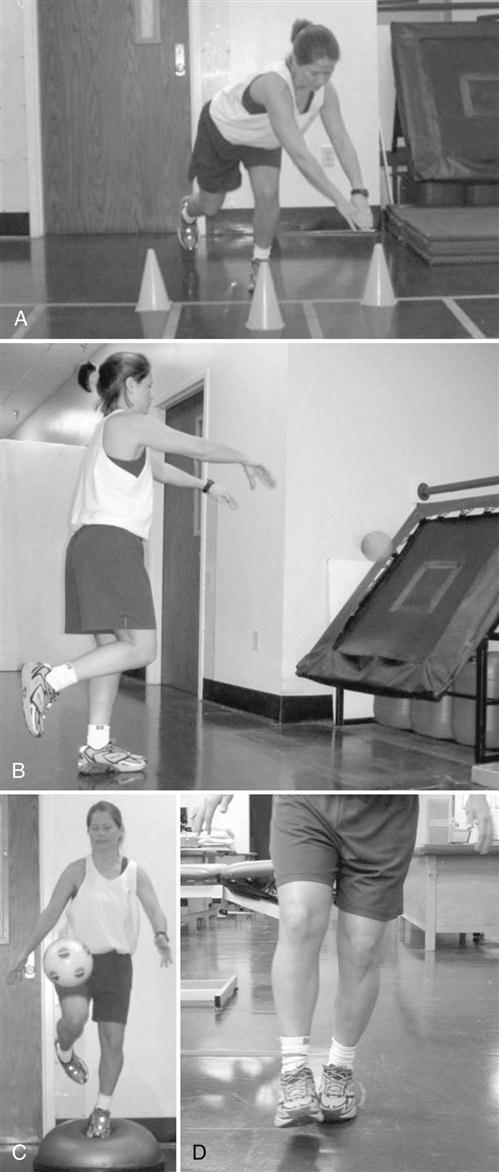
Neuromuscular training programs aimed at enhancing or restoring neuromuscular control following injury have been developed and have been shown to reduce the incidence of injury.28–32 A comprehensive neuromuscular program would integrate exercises that challenge all three regulatory systems: the somatosensory, visual, and vestibular systems. The neuromuscular program should incorporate a multilevel approach, which includes combinations of strength training, flexibility, balance, agility, and plyometric exercises. Activities that induce adaptations to the system may include open and/or closed chain exercise, eccentric training, balance activities, reflex facilitation, stretch-shortening, biofeedback training, and controlled position training. Balance training might include stationary and dynamic surfaces, such as wobble boards, balance beams, and foam pads, to enhance both static and dynamic balance. Functional training, such as jumping and landing, agility, and perturbation training, should also be included depending on sport demands. Fig. 33-5 illustrates several examples of neuromuscular training exercises.
As mentioned previously, the clinician must continually monitor the athlete for tissue tolerance and to determine readiness to proceed to the next phase in the rehabilitation process. Myer and associates have proposed a progressive end-stage return to sport protocol following ACL reconstruction that is based on the athlete meeting specific criteria before being able to progress to the next phase.33 The protocol consists of four stages: dynamic stabilization, functional strengthening, power development, and sports performance symmetry. One significant limitation of this protocol is that some of the criteria were based on the use of specialized testing equipment such as a stabilometer and isokinetic equipment, which most clinicians would not have available.
Returning to Sport
As previously stated, the goal of the rehabilitation program is to return the athlete to the highest functional level. Rehabilitation programs are based on current scientific principles that include knowledge of the healing process, anatomy/physiology, biomechanics, and kinematics. Keep in mind that these principles and concepts are ever-changing as new research becomes available.
Typically, return to sport is based on various subjective and objective criteria. Many clinicians have either developed their own compilation of tests or have adopted those used by others to determine when an athlete is ready to return to sport.
Single-leg hop tests are commonly used to determine an athlete’s progress in his/her rehabilitation program and to determine the readiness to return to sport. Various single-leg hop tests either used alone or in combination have been described in the literature.34–38 These tests include single-leg hop and stop tests,36 single-leg hop for distance and time, triple hop, and the triple crossover hop.34–39 Several studies have shown these tests to be reliable with intraclass coefficients between 0.66 to 0.97.40–42 Barber and associates recommended using at least two hop tests and achieving a limb symmetry score of 85%.34
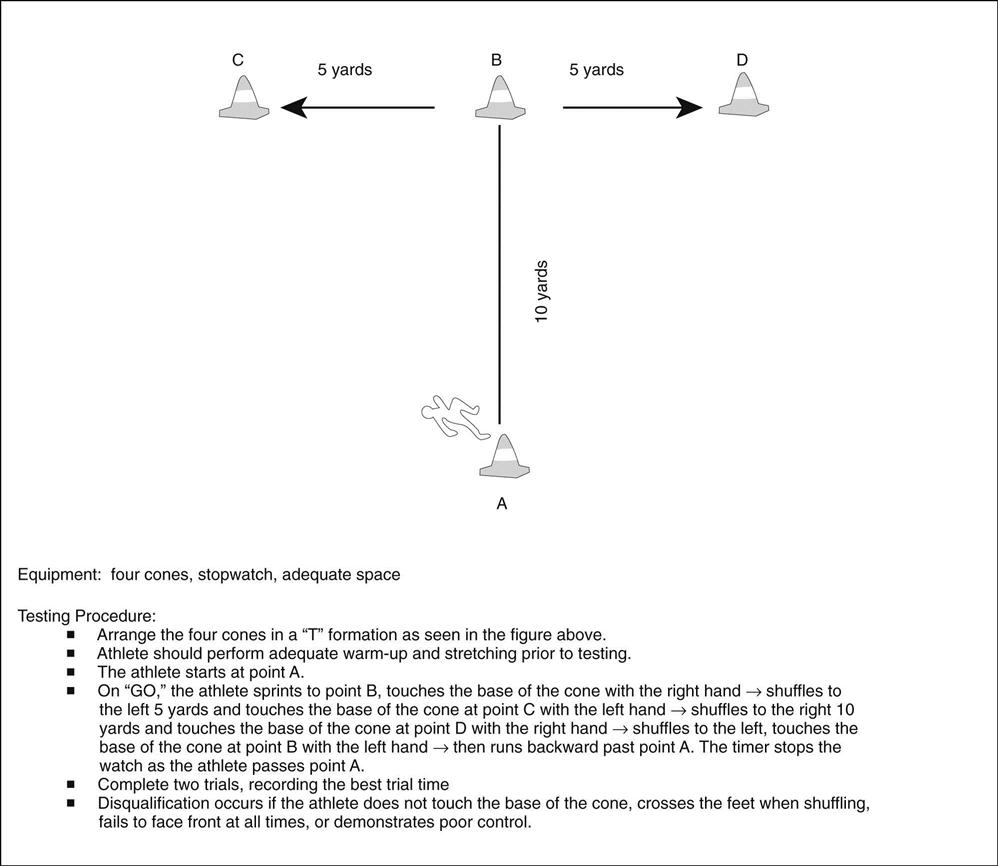
Other test measures have been used to determine return to sport as well. Vertical jump height (Fig. 33-6) and isokinetic testing have been used to assess function and strength.43,44 A 1 repetition maximum (RM) leg press test or squat can also be used to assess strength. The shuttle run and figure eight run have been used to test the ability to run, cut, and pivot.34,45,46 The T-test (Fig. 33-7) and the Edgren side step test are two tests that can be used to assess agility and body control.47 These tests can also be used in the rehabilitation program as functional drills.

Speed tests measure the body’s displacement per unit of time. Testing speed for clinical purposes is usually limited because of lack of appropriate space. The majority of the research on these tests has been with ACL deficient or ACL reconstruction individuals; however, the tests may be used in other lower extremity patient populations as well. Standard health and fitness tests for flexibility, local endurance, aerobic power, and agility/speed such as those described in The Essentials of Strength and Conditioning47 may also be incorporated into the testing protocol and compared with available normative data.
Davies48 has developed a functional testing algorithm that uses a systematic functional progression of testing and exercise. It is designed to progressively increase stresses on the athlete while gradually lessening clinical control. The algorithm includes the following: subjective information, basic measurements, KT 1000 test, balance testing, closed and open chain strength testing, two-leg jump test, unilateral hop test, lower extremity functional test, and sports-specific testing.48 Very specific criterion must be met before the athlete is allowed to progress to the next level. Frequent testing and monitoring of the patient allows the clinician to always know the status of that patient. A specific rehabilitation program can then be designed to address individual deficits instead of following a preset clinical protocol.
Recent research by Hewett and associates49 has focused on biomechanical loading measurements in female athletes in an attempt to predict those who are at risk for ACL injury. They concluded that increased valgus motion and valgus moments at the knee were key predictors for potential ACL injury (Fig. 33-8). If predictive factors associated with lower extremity injuries can be identified, specific screening programs and training programs could potentially be designed to reduce the risk for injury.
In general, there is currently no standard accepted series of tests to determine when an athlete is ready to return safely to sport. The decision should be based on ROM, strength, symptomatology, and functional testing. Box 33-7 provides a list of tests that the clinician may select to assist in the decision. It is recommended that a minimum of two hop tests,34 a strength assessment, and an agility/body control test be used. The athlete must demonstrate proper form and technique throughout the test procedures. A deficit of 10% or less with good control is currently used in many facilities to allow return to sport. There are obvious limitations to the tests; however, they appear to be the most commonly used in various combinations. Further research is needed not only to determine risk factors, but also to determine what testing procedures would be best to predict safe return to sport.
Summary
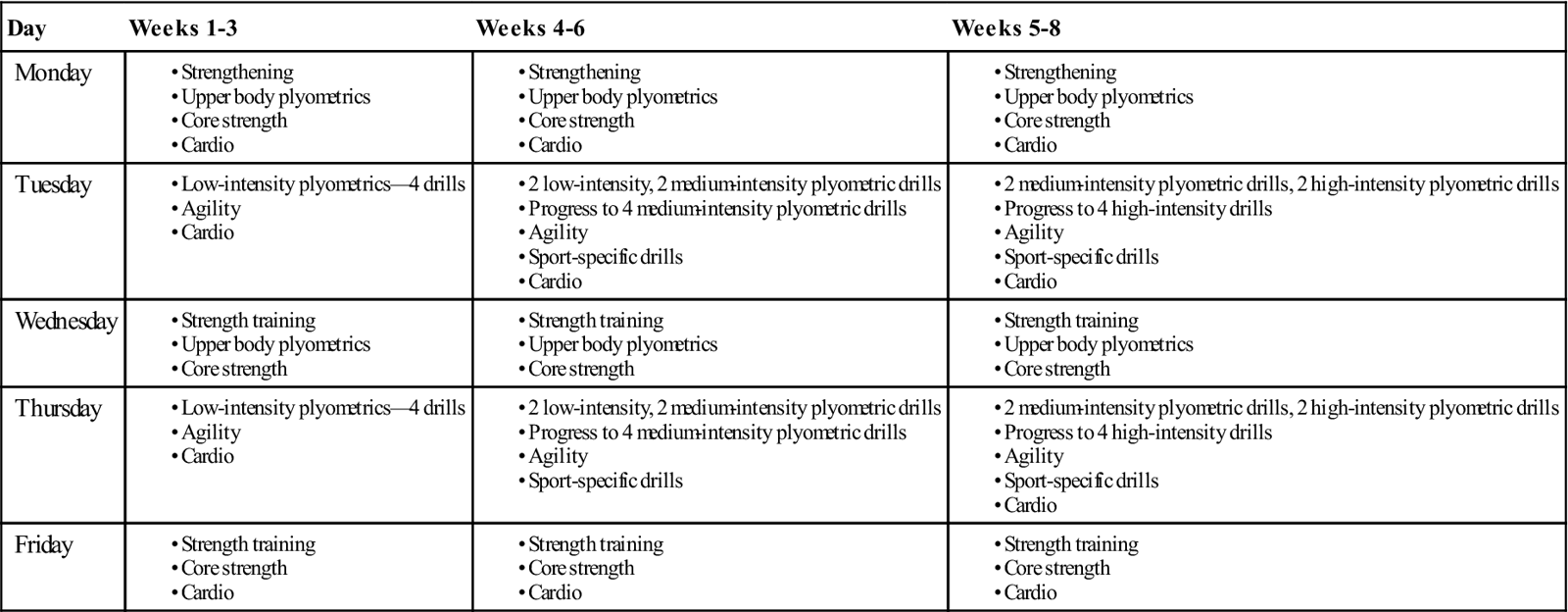
Returning the jumping athlete back to sport as safely and efficiently as possible is the primary goal of the rehabilitation program. The length of time to return depends on many factors. It is the clinician’s responsibility to have the scientific knowledge base and clinical skills to determine when and how the athlete is to progress through the program. Current testing procedures have their limitations; however, they provide some objective data to assist the clinician in deciding when the athlete may resume sport activities. It is impossible to design one rehabilitation protocol for all athletes lest it be a cookbook approach. Table 33-1 provides only one example of how the various training components can be combined. It was the goal of this chapter to provide the clinician with guidelines, ideas, and resources for returning the jumping athlete back to sport; hopefully, it accomplished its goals.
Clinical Case Review
1Matt is a 42-year-old male who has had an ACL reconstruction. He has completed his early postoperative rehabilitation and is in phase I (dynamic stabilization and strengthening) of his return to a sport program. What criteria might you use to assess whether Matt is ready to progress to functional strengthening exercises (stage II)?
• No pain
• Full ROM
• Single-limb squat and hold symmetry (60° knee flexion, 5-second hold)
• Audibly rhythmic foot strike patterns with treadmill running
These criteria are based on the Return to Sport algorithm developed by Myer and associates.33 Matt should have been allowed to progress from stage I into stage II by having a minimum International Knee Documentation Committee score of 70 and baseline strength scores. This algorithm is somewhat limiting because much of the testing uses equipment that is not available to most clinicians. However, the clinician may still incorporate this criterion-based approach by using other “low technology” tests and measures: a 1 RM test, the lateral step test, and the Star Excursion Balance test are a few examples.
2Matt is now 6 months after surgery for an ACL/meniscal repair. He had been going to the gym to work on his strengthening and cardiovascular training while attending rehabilitation sessions once per week to progress and focus on his functional training. He had been progressing extremely well—good control with landings and agility exercises, etc. He is very motivated and eager to return to basketball. At 6 months after surgery, he performed a functional assessment that included four single-leg hop tests. Although he had no pain or symptoms during the test, the following day Matt experienced significant swelling and discomfort in the knee. How would you modify his program at this point?
• Reexamine the knee for signs of instability or possible meniscal pathology
• Apply modalities to reduce effusion and pain
• Notify physician and/or refer to physician if any suspicion of reinjury
3Julie is a 36-year-old woman with a grade II ankle sprain who plays recreational volleyball. She has had several sprains in the past, but this was her worst. Her walking boot was discontinued several weeks ago and she is progressing well with her rehabilitation. Although Julie’s physician released her to return to volleyball, she still has mild swelling and slight pain with some of the light plyometric exercises. Should she be allowed to return to play?
Julie did not return to play at that time for the following reasons:
• She had pain with even light plyometric and agility drills
• She demonstrated 4/5 ankle evertor strength
• She had balance deficits on the Star Excursion Balance test
• Julie is a recreational player and not under any pressure to return
4Andy has completed a rehabilitation program following a grade II hamstring strain. He returned to tennis but reinjured the hamstring after only 3 weeks. He had no complaints of pain with jogging, cutting, or jumping. He demonstrated 5/5 strength with manual muscle testing. What factors could have lead to his reinjury?
It has been reported that nearly one third of hamstring strain injuries will recur within the first year after return to sport. This high recurrence rate suggests inadequate rehabilitation, premature return to sport, or a combination of both. Heiderscheit and associates50 proposed recommendations for diagnosis, rehabilitation progression, and injury prevention. Factors that may contribute to reinjury may include persistent weakness, decreased extensibility of the musculotendinous unit, and/or compensatory changes in biomechanics and motor patterns following injury. Proper diagnosis through examination, appropriate phase progression, and use of the best available evidence to determine return to sport may be beneficial in reducing recurrence rates. Therapeutic exercises that strengthen and promote neuromuscular control of the lower extremity and lumbo-pelvic musculature should be key components of the program. Manual therapy techniques to restore mobility should be included as indicated.50
Strength testing to assist with determining return to play should be performed prone with the knee at both 90° and 15° of flexion. The athlete should be able to perform four pain-free maximal effort contractions. Isokinetic testing would be more optimal if available and should demonstrate a less than 5% deficit in the ratio of eccentric hamstring to concentric quadriceps strength.50
5Matt is now 7-months postoperation for an ACL/meniscal repair. What testing criteria might you use to determine if he is ready to return to basketball?
The choice of testing depends on the physician and/or clinician’s preference, as well as the specific sport demands of the patient. The following are examples of commonly used criteria: