Transient Tachypnea of the Newborn
After reading this chapter, you will be able to:
• List the anatomic alterations of the lungs associated with transient tachypnea of the newborn.
• Describe the causes of transient tachypnea of the newborn.
• List the cardiopulmonary clinical manifestations associated with transient tachypnea of the newborn.
• Describe the general management of transient tachypnea of the newborn.
• Describe the clinical strategies and rationales of the SOAP presented in the case study.
• Define key terms and complete self-assessment questions at the end of the chapter and on Evolve.
Anatomic Alterations of the Lungs
Transient tachypnea of the newborn (TTN) (also called type II respiratory distress syndrome and “wet lung” syndrome) was first described in the literature in 1965. Within the first 4 to 6 hours after birth, TTN produces clinical signs very similar to those associated with the early stages of respiratory distress syndrome (see Chapter 34). However, the anatomic alterations of the lungs associated with TTN are much different from the pulmonary pathology seen in respiratory distress syndrome.
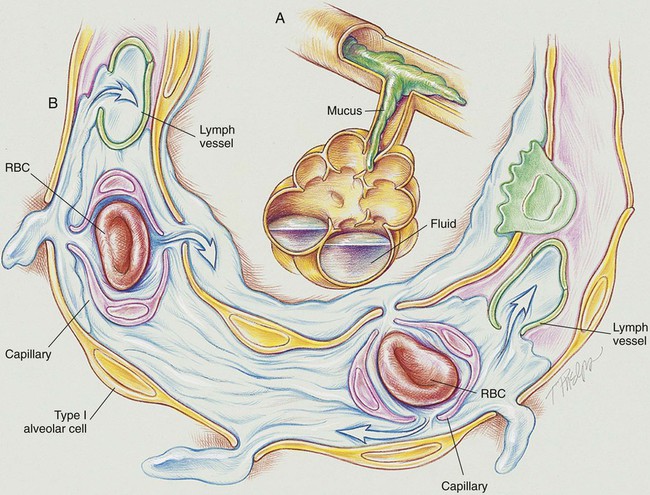
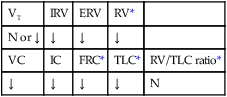
As shown in Figure 33-1, the infant with TTN has a delay in the pulmonary fluid absorption by the lymphatic system and pulmonary capillaries. It is thought that this condition results, in part, from the infant’s hypoxemia and inadequate inspiratory effort, producing a delay in clearance of pulmonary fluid. As this condition worsens, the infant develops pulmonary capillary congestion, interstitial edema, decreased lung compliance, decreased tidal volume, and increased dead space. Because the swallowing and cough efforts of infants with TTN are commonly depressed, the clearance of bronchial secretions is compromised. This condition often leads to air trapping and alveolar hyperinflation.
The major pathologic or structural changes associated with TTN are as follows:
General Management of Transient Tachypnea of the Newborn
Respiratory Care Treatment Protocols
Oxygen Therapy Protocol
Oxygen therapy is used to treat hypoxemia, decrease the work of breathing, and decrease myocardial work. Because of the hypoxemia that often develops in TTN, supplemental oxygen may be required (see Oxygen Therapy Protocol, Protocol 9-1).
Bronchopulmonary Hygiene Therapy Protocol
Because of the excessive airway secretions and accumulation associated with TTN, a number of bronchial hygiene treatment modalities may be used to enhance the mobilization of bronchial secretions (see Bronchopulmonary Hygiene Therapy Protocol, Protocol 9-2).
Mechanical Ventilation Protocol
Mechanical ventilation may occasionally be necessary to provide and support alveolar gas exchange and eventually return the patient to spontaneous breathing. Patients with TTN rarely require mechanical ventilation (see Mechanical Ventilation Protocols, Protocol 9-5, Protocol 9-6, and Protocol 9-7).
CASE STUDY
Transient Tachypnea of the Newborn
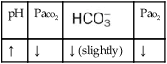
Admitting History and Physical Examination
In the NICU, the baby was placed in a warmed isolette, and an umbilical artery catheter was inserted. An IV line and nasogastric tube also were inserted. Warm, humidified oxygen was started via a high-flow nasal cannula (HFNC)* at 4 L/min and an Fio2 of 0.5. Ten minutes later the infant’s vital signs were as follows: heart rate 155 bpm, blood pressure 75/40, and respiratory rate 75/min. The infant’s ventilatory pattern was described by the neonatologist as fast and shallow. In other words, even though the infant was breathing fast and not very deeply, she did not appear to be working hard to breathe. She had no intercostal retractions or nasal flaring at this time. Arterial blood gas values were as follows: pH 7.33, Paco2 31,  21, and Pao2 42. The baby’s Spo2 was 75%.
21, and Pao2 42. The baby’s Spo2 was 75%.
Respiratory Assessment and Treatment Plan
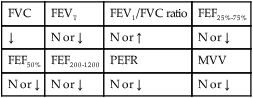
O Vital signs: HR 170/min, BP 75/45, and RR 110/min. Chest retractions, nasal flaring. Skin pale and blue. Moderate to severe bilateral rhonchi and crackles. CXR: Infiltrates and microatelectasis over both lungs, generalized hyperinflation. ABGs on HFNC at 4 L/min and Fio2 0.50: pH 7.52, Paco2 28,  22, Pao2 35, Spo2 58%.
22, Pao2 35, Spo2 58%.
• TTN (neonatologist, CXR, history)
• Infiltrates and atelectasis (CXR film)
• Excessive bronchial secretions (rhonchi and crackles)
• Acute alveolar hyperventilation with severe hypoxemia (ABGs)
P Lung Expansion Therapy Protocol (nasal CPAP at +2 cm H2O). Increase Oxygen Therapy Protocol (Fio2 0.60 via CPAP at +2 cm H2O setup). Bronchopulmonary Hygiene Therapy Protocol (CPT q2h). Continue to monitor closely.
Discussion
This case reinforces the importance of observation and inspection in the assessment process. The respiratory care practitioner must continuously inspect and analyze infants with TTN. This baby, for example, born at 35 weeks, may have had respiratory distress syndrome (RDS; see Chapter 34), but the clinical symptoms ruled out the diagnosis. For example, babies with RDS have alveolar collapse and consolidation, whereas babies with TTN have airway trapping and alveolar hyperinflation. In addition, babies with RDS generally breathe hard, quickly, and deeply, whereas infants with TTN usually breathe rapidly and shallowly. In fact, this rapid and shallow breathing pattern often is considered a hallmark of TTN. Certainly, the rapid shallow breathing seen in this baby was caused, in part, by the Increased Alveolar-Capillary Membrane Thickness (Figure 9-10)—and decreased lung compliance—associated with TTN.



 values will be lower than expected for a particular Pa
values will be lower than expected for a particular Pa



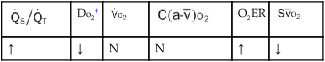
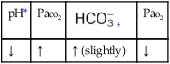
 , Arterial-venous oxygen difference; DO2, total oxygen delivery; O2ER, oxygen extraction ratio;
, Arterial-venous oxygen difference; DO2, total oxygen delivery; O2ER, oxygen extraction ratio;  , pulmonary shunt fraction;
, pulmonary shunt fraction;  , mixed venous oxygen saturation;
, mixed venous oxygen saturation;  , oxygen consumption.
, oxygen consumption.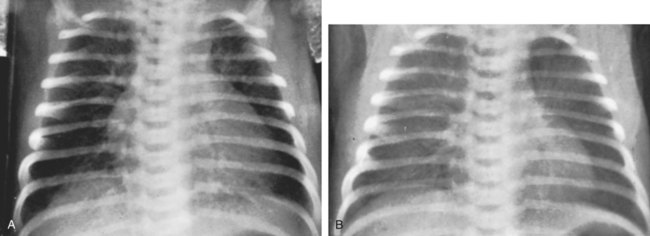
 22, and Pa
22, and Pa 24, Pa
24, Pa