CHAPTER 10 Transgastric cystgastrostomy
Step 1. Surgical anatomy
♦ Preoperative imaging, typically an abdominal computed tomography scan, is imperative to determine the location of the pancreatic pseudocyst relative to the stomach. For the transgastric approach, the cyst needs to be directly posterior to the stomach.
♦ Attention should be paid to the location of the splenic artery, to make certain that it is not at risk for injury when creating the cystgastrostomy.
♦ If the cyst is not directly posterior to the stomach, an alternative approach is necessary. A cystojejunostomy is ideal in such cases and can often be performed laparoscopically.
Step 2. Preoperative considerations
Patient preparation
♦ The diagnosis of pancreatic pseudocyst should be firmly established. The patient typically has a history of pancreatitis, but further investigation is necessary to confirm the diagnosis.
♦ Preoperative evaluation includes a computed tomography scan to determine the size and location of the cyst, as well as an endoscopic retrograde cholangiopancreatogram (ERCP) to assess for communication between the pancreatic duct and the cyst.
♦ In some instances, endoscopic ultrasound or aspiration of the cyst for amylase and lipase levels may be warranted. Pancreatic pseudocysts typically have high levels of amylase and lipase.
♦ Once the diagnosis of pseudocyst is made, the cyst wall should be allowed to mature for at least 6 weeks prior to surgical drainage.
Step 3. Operative steps
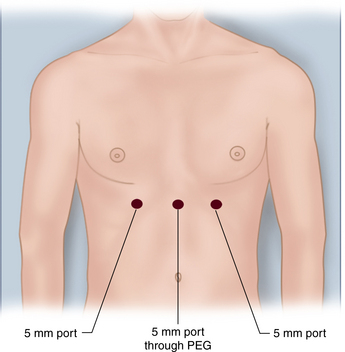
Port placement
♦ A 5-mm trocar is placed through the PEG tube to allow insufflation of the stomach with carbon dioxide to 15 mm Hg. Two additional 5-mm trocars are placed on either side of the PEG. The endoscope is used to visualize placement of these trocars. Following placement of the trocars, the endoscope is retracted back into the midesophagus. Ideally, the additional trocars should have an internal buttress or balloon to ensure apposition of the anterior gastric wall to the anterior abdominal wall (Figure 10-1).
♦ Alternatively, no PEG is placed, and the trocars are inserted directly into the gastric lumen with laparoscopic guidance. In this technique, intraperitoneal access is obtained at the umbilicus, and the peritoneum is insufflated to 5 to 8 mm Hg. An endoscope is passed into the stomach, and the stomach is insufflated. Three balloon trocars are then inserted through the upper abdomen and into the gastric lumen. The balloons are then inflated, and the gastric wall is pulled against the abdominal wall. The stomach is then insufflated while the peritoneum is desufflated.
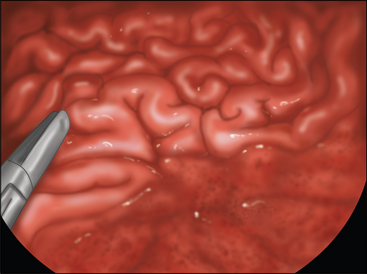
Cyst localization
♦ The cyst is localized with an aspirator. In most instances, the cyst makes a visible bulge in the posterior stomach (Figure 10-2).
♦ If the location of the cyst is not obvious, intraoperative ultrasound can be used. After aspiration of the cyst confirms cyst fluid, the aspirator is left in place in the posterior gastric wall.
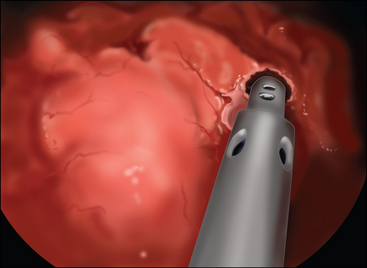
Creation of cystgastrostomy
♦ With the aspirator still in place to confirm the location of the cyst, a cystgastrostomy is created with the ultrasonic shears adjacent to the aspirator. The aspirator is then withdrawn, and the cystgastrostomy is enlarged with the ultrasonic shears (Figure 10-3). Alternatively, the laparoscopic stapler may be used in the patient when there is bleeding at the cystogastrostomy or if the area seems particularly well-vascularized.
♦ A portion of the cyst wall should be sent for pathologic evaluation. Hook cautery can also be used to expand the opening.
♦ Suction should be available to remove the liquid contents of the cyst.
♦ Bleeding is typically minimal. If bleeding persists from the edge of the cystgastrostomy, it can be controlled with sutures.
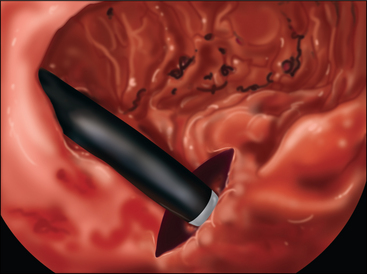
Endoscopy of the cyst
♦ To ensure adequate drainage of the cyst, the endoscope is again passed into the stomach, through the cystgastrostomy, and into the pseudocyst. The cystgastrostomy should be large enough (approximately 2 cm) to permit passage of a standard endoscope. Any remaining cyst contents can be aspirated through the endoscope (Figure 10-4).
Removal of trocars and closure of gastrotomies
♦ The stomach is desufflated and the endoscope is removed. The trocars are backed out of the stomach such that they now only traverse the abdominal wall. The PEG is removed as well, and a new trocar is placed through the abdominal wall where the PEG had been. The abdomen is now insufflated, creating a typical laparoscopic environment.
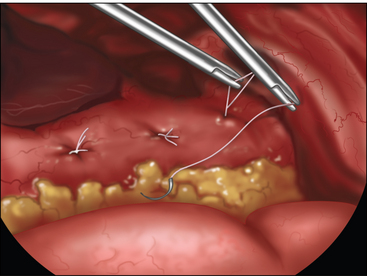
♦ The three anterior gastrotomies are sutured closed laparoscopically. In some instances, a fourth 5-mm trocar is inserted to provide optimal suturing of the anterior gastric wall (Figure 10-5).
♦ The abdomen is then desufflated, all trocars are removed, and the skin incisions are closed.
Step 5. Pearls and pitfalls
♦ The pseudocyst should be localized directly posterior to the posterior wall of the stomach to enable this approach.
♦ A large PEG tube should be used to enable passage of a 5-mm trocar.
♦ The cystgastrostomy should be sufficiently large (approximately 2 cm in diameter) to allow adequate drainage of the pseudocyst.
♦ This approach makes it difficult to adequately biopsy the cyst wall. If the diagnosis of pseudocyst is not certain and there is concern for malignancy, an alternative approach that enables a biopsy should be performed. A laparoscopic stapled cystgastrostomy is an excellent alternative in this instance.