Chapter 6 Transforaminal Epidural Block and Selective Nerve Root Block
TFEB requires a lower volume (1-3 mL) of injectate than conventional epidural block achieved by direct injection to the anterior epidural space. This smaller volume can decrease the toxicity from the injectate. No further injection is recommended if the first TFEB was not effective. If the initial response to TFEB is favorable but short-lived, a series of injections (3-6 times per year) or pulsed radiofrequency lesioning of the corresponding dorsal root ganglion (DRG) is recommended (see Chapter 7). The interval for sequential block varies from days to weeks for a series of injections.
Treatment objectives
Indications
Transforaminal Epidural Block
Contraindications
Contraindications to both TFEB and SNRB are as follows [11,16]:
Preoperative preparation
History
The history for a patient who is to undergo TFEB or SNRB should include questions about pain characteristics, such as the quality and location of the pain, onset, and any relieving and aggravating factors. Questions should also be asked to identify “red flags”—signs and symptoms that might indicate the presence of cancer, cauda equina syndrome, or infection (Table 6.1).
Table 6.1 “Red Flags” in a Patient to Undergo Spinal Nerve Block: Signs and Symptoms Needing Rapid Evaluation and Operation
| Cancer-related signs |
Anatomy and procedures
Cervical Region
Anatomy
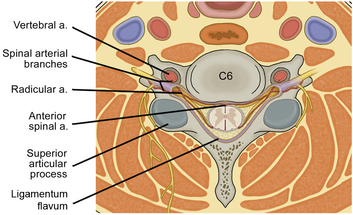
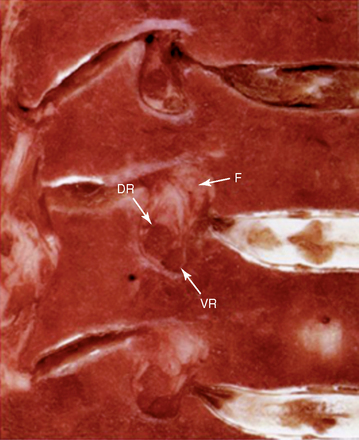
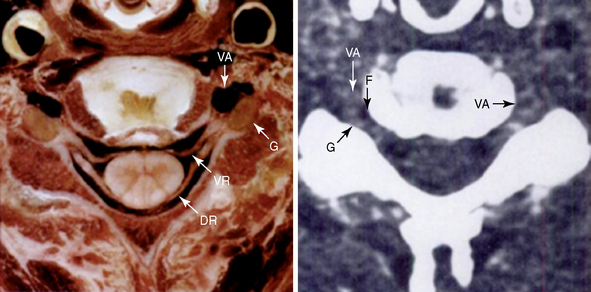
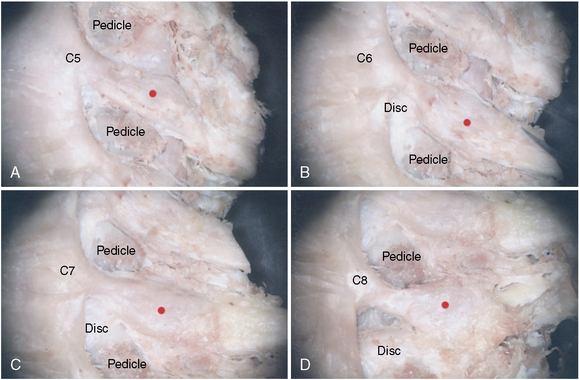
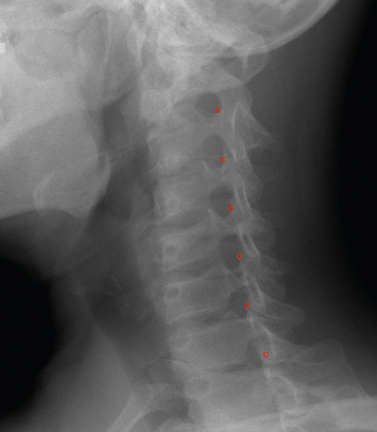
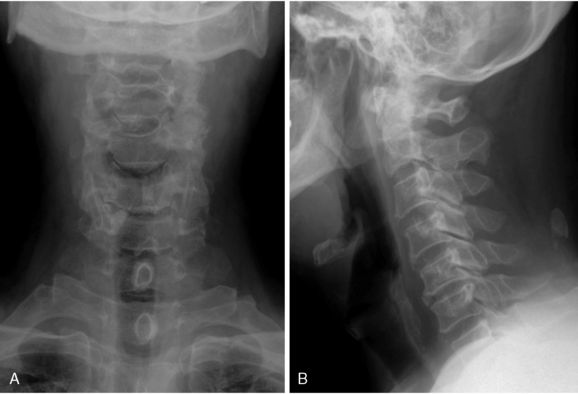
There are seven cervical vertebrae but eight cervical nerve roots. The first cervical nerve root is located between the occiput and the atlas, and each subsequent nerve root is located above its corresponding vertebra. If symptoms correlate with the seventh cervical nerve root, the C6-C7 foramen is the target for the block. The cervical neural foramen is a bony canal 4 to 5 mm long through which the cervical nerve roots pass anterolaterally (at about a 45-degree angle with respect to the coronal plane) and downward (at about a 10-degree angle with respect to the axial plane) (Figs. 6-1 to 6-4). Cervical spinal nerves from C3 to C7 exit the intervertebral foramen in the direction of the posterior, lower half of the foramen (Figs. 6-2 to 6-4). The cervical nerve roots occupy about one quarter to one third of the volume of the foramen and is accompanied by radicular arteries and veins (Figs. 6-1 and 6-2).
The vertebral artery at the caudal portion of the foramen is immediately anterior and medial to the ganglion (Figs. 6-1 to 6-4). In practice, the target points (red dots on Fig. 6-4) should lie directly over the dorsal part of the neural foramen so as to avoid vertebral artery injury.
Procedure
Transforaminal epidural block
Selective nerve root block
SNRB is performed by means of the same technique as for TFEB, except for the final position of the needle tip. The needle is advanced until the patient experiences paresthesia or until the needle tip is located just medial to the lateral articular process at the desired level. At this point, less than 0.5 mL of contrast dye is injected under real-time fluoroscopic guidance through a firmly fixed needle to confirm needle placement. The contrast dye will flow in a linear fashion and surround the nerve root, forming a tubular defect (Fig. 6-7).
For diagnostic specificity, the injectate should not go into the epidural space.
Thoracic Region
Anatomy
Thoracic spinal nerves exit the intervertebral foramen in the direction of the posterior, upper half of the foramen [25]. The anatomy of the upper thoracic levels (T1-T8)—the shape of the lamina, the narrow spaces between ribs, and the wide bases of the transverse processes—makes it difficult to reach the intervertebral foramen. Accurate positioning of the straight cannula for the TFEB or SNRB procedure is consequently also difficult. Use of a curved needle makes it easy to position the cannula accurately.
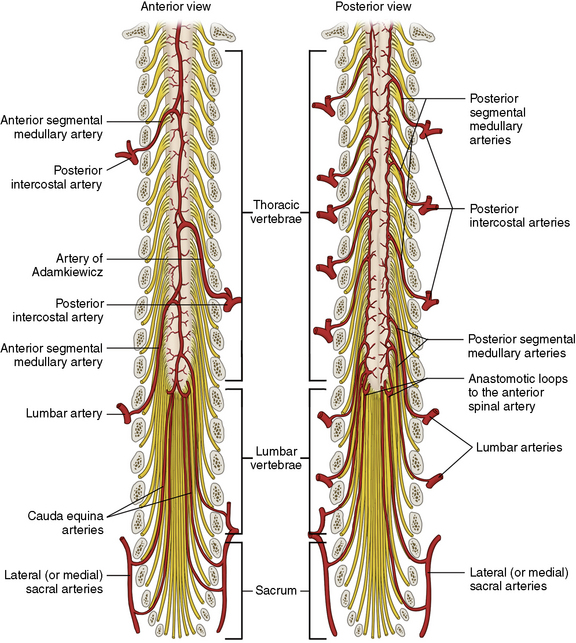
Understanding the anatomy of the artery of Adamkiewicz is crucial to the procedure of TFEB or SNRB (Fig. 6-8) [26]. This artery is the largest of the radicular arteries supplying the lower two thirds of the spinal cord. It is mostly found from T9 to L1 (approximately 80% of cases). Injury to the artery of Adamkiewicz can result in devastating ischemia of the lower spinal cord, causing anterior spinal artery syndrome. Care should be taken in performance of these interventional pain procedures at the neural foramina from T9 to L1.
Procedure
Transforaminal epidural block
Lumbar Region
Anatomy
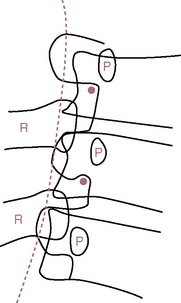
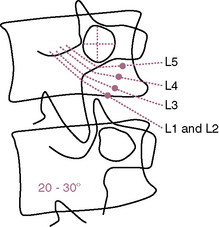
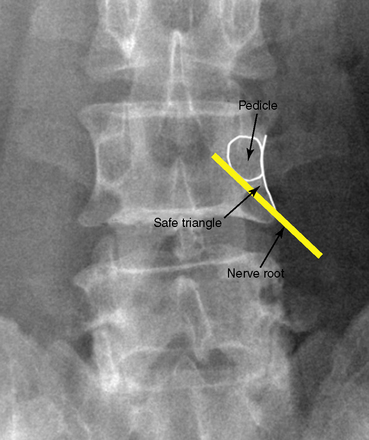
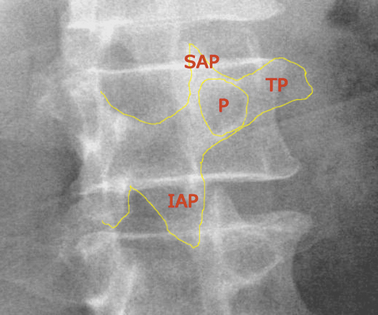
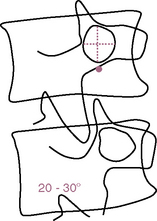
The lumbar nerve travels inferiorly and exits in a lateral plane, under the pedicle, with a downward course at varying angles from the horizontal according to the vertebral level, thus occupying the superior portion of each foramen (Fig. 6-15). A “safe triangle” has been defined for this procedure. It is the area between the horizontal base of the pedicle, the lateral border of vertebral body, and the connecting diagonal nerve root (Fig. 6-11) [27].
Procedure
Transforaminal epidural block
Selective nerve root block
The target points for L1 to L5 SNRB are located more laterally than those for TFEB, to avoid epidural spread of the injectate. The target points for L1 to L5 SNRB also differ according to the vertebral level involved (Fig. 6-15).
When the patient experiences paresthesia, 0.5 mL of contrast dye is injected under fluoroscopic guidance using an AP image. This injection confirms that the needle tip is appropriately placed near the nerve root and ensures that the injectate is not passing epidurally or intravascularly (Fig. 6-16).
Sacral Region
Anatomy
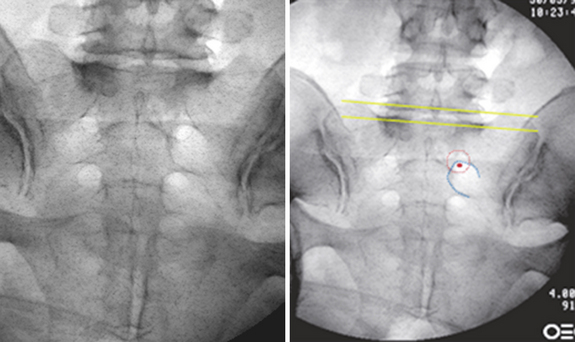
The large, wedge-shaped sacrum in adults is composed of five fused sacral vertebrae. The base of the sacrum is formed by the superior surface of the S1 vertebra. On the pelvic and dorsal surfaces are four pairs of sacral foramina for the exit of the rami of the first four sacral nerves and the accompanying vessels. The posterior sacral foramen appears as a small round circle (red dotted circle in Fig. 6-17), whereas the anterior foramen has a curvilinear shape (blue, C-shaped, dotted line in Fig. 6-17).
Procedure
Sacral Transforaminal Epidural Block
We do not perform TFEB at the sacral region, because caudal block is easier here.
Sacral Selective Nerve Root Block
Postprocedural care and follow-up [17]
Signs and symptoms of infection after TFEB or SNRB are as follows:
Possibly more serious problems may cause the following signs and symptoms:
CASE STUDY 6.1 Cervical Transforaminal Epidural Block
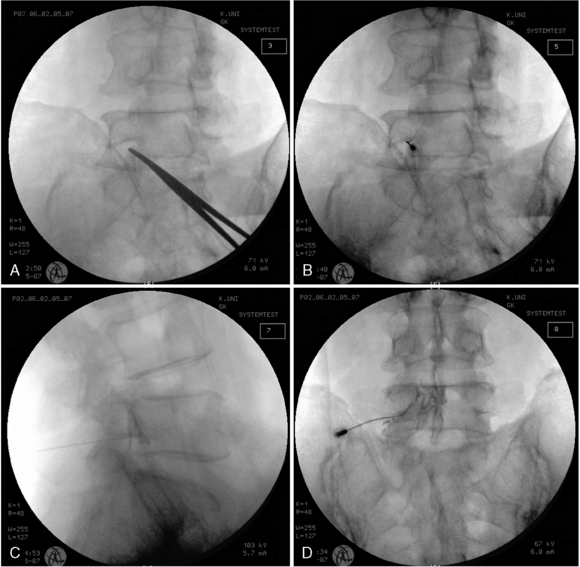
Imaging Findings and Intervention Procedure
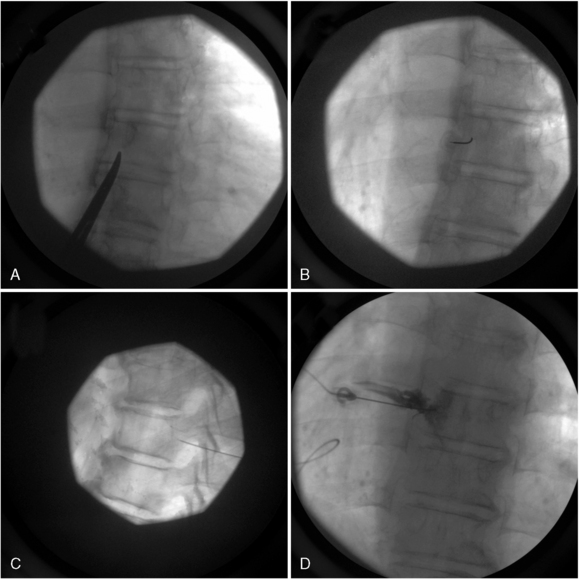
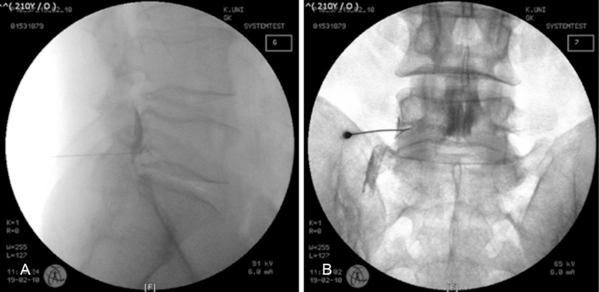
Simple cervical spine radiographs and magnetic resonance imaging demonstrated degenerative right foraminal stenosis at C5-C6 and C6-C7 levels as well as compression of the right C6 and C7 nerve roots (Figs. 6-19 and 6-20). With the patient in the supine position, two block needles were introduced directly to the anterior border of the superior articular process via a right anterolateral approach (Fig. 6-21A). When the needles touched the target point, the needle tips were more carefully advanced, touching the posterior border of the neural foramen. When the needles reached the halfway point between the medial and lateral borders of the articular pillars in the anteroposterior projection, contrast dye was injected (Figs. 6-21B and 6-21C). After confirmation of the correct needle placement, 2 mL of a mixed solution of 0.19% ropivacaine and 20 mg of triamcinolone was injected at each site.
CASE STUDY 6.2 Lumbar Transforaminal Epidural Block
History
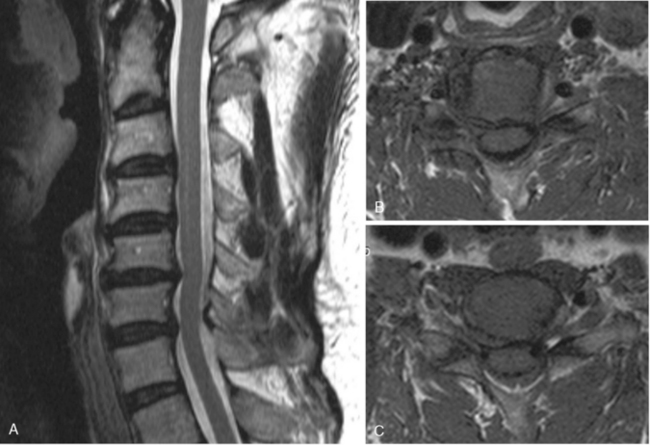
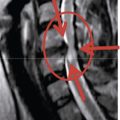
A 47-year-old man was referred to our pain management center with a five-month-history of low back pain with radiating pain to left buttock, posterolateral thigh and lateral calf. He had undergone a microscopic lumbar discectomy one month before the referral for the treatment of acute ruptured disc herniation at the L5-S1 level, causing compression of thecal sac and left S1 nerve root (Fig. 6-22A). However, he is still suffering from pain after the surgery. Neurologic examinations yielded no significant findings to suggest the cause of the presenting symptoms.
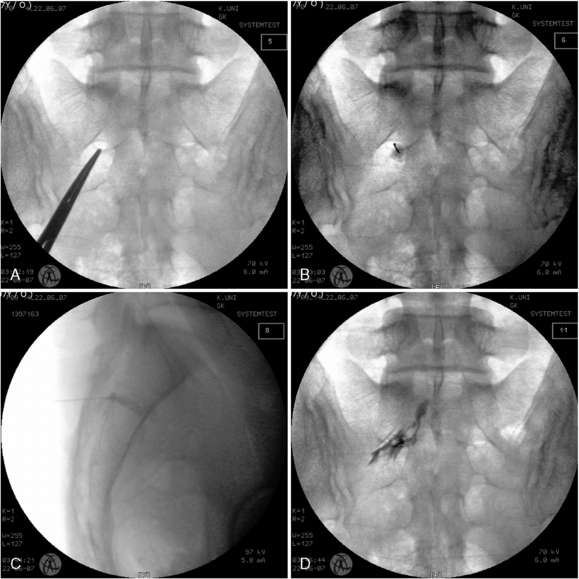
Imaging Findings and Intervention Procedure
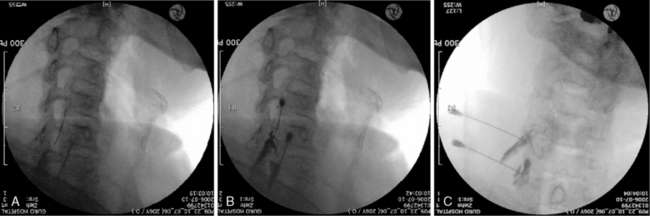
Magnetic resonance imaging demonstrated a remnant extruded disc herniation, causing compression of the thecal sac and left S1 nerve root (Figs. 6-22B and 6-22C). Epidurogram revealed significant obstruction of cephalad epidural spread of contrast at the left L5-S1 junction (Fig. 6-22D). Left L5 TFEB was performed under the fluoroscopic guidance. With the patient in the prone position, a 22-gauge spinal needle was introduced directly into the safe triangle using a tunnel vision technique in an oblique projection of C-arm, on which the “Scotty dog” formation appears. During the careful advance of the needle to the target point, AP and lateral fluoroscopic images were frequently checked to confirm the location of needle tip. When the needle touched the posterior border of the vertebral body in the lateral projection of C-arm, contrast medium was injected and followed by injection of 3 mL of a mixed solution of 0.19% ropivacaine and 40 mg of triamcinolone (Fig. 6-23).
1 Slipman C.W., Lipetz J.S., DePalma M.J., et al. Therapeutic selective nerve root block in the nonsurgical treatment of traumatically induced cervical spondylotic radicular pain. Am J Phys Med Rehabil. 2004;83:446-454.
2 Slipman C.W., Lipetz J.S., Jacksom H.B., et al. Therapeutic selective nerve root block in the neurosurgical treatment of atraumatic cervical spondylotic radicular pain: A retrospective analysis with independent clinical review. Arch Phys Med Rehabil. 2000;81:741-746.
3 Gajraj N.M. Selective nerve root blocks for low back pain and radiculopathy. Reg Anesth Pain Med. 2004;29:243-256.
4 Rathmell J.P., Aprill C., Bogduk N. Cervical transforaminal injection of steroids. Anesthesiology. 2004;100:1595-1600.
5 Depalma M.J., Bhargava A., Slipman C.W. A critical appraisal of the evidence for selective nerve root injection in the treatment of lumbosacral radiculopathy. Arch Phys Med Rehabil. 2005;86:1477-1483.
6 Lutz G.E., Vad V.B., Wisneski R.J. Fluoroscopic transforaminal lumbar epidural steroids: An outcome study. Arch Phys Med Rehabil. 1998;79:1362-1366.
7 Botwin K.P., Gruber R.D., Bouchlas C.G., et al. Fluoroscopically guided lumbar transformational epidural steroid injections in degenerative lumbar stenosis: An outcome study. Am J Phys Med Rehabil. 2002;81:898-905.
8 Bhargava A., DePalmac M.J., Ludwigb S., et al. Injection therapy for lumbar radiculopathy. Curr Opin Orthop. 2005;16:152-157.
9 Vad V.B., Bhat A.L., Lutz G.E., et al. Transforaminal epidural steroid injections in lumbosacral radiculopathy: A prospective randomized study. Spine. 2002;27:11-16.
10 Delport E.G., Cucuzzella A.R., Marley J.K., et al. Treatment of lumbar spinal stenosis with epidural steroid injections: A retrospective outcome study. Arch Phys Med Rehabil. 2004;85:479-484.
11 Blankenbaker D.G., Davis K.W., Choi J.J. Selective nerve root blocks. Semin Roentgenol. 2004;39:24-36.
12 Wolff A.P., Groen G.J., Crul B.J. Diagnostic lumbosacral segmental nerve blocks with local anesthetics: A prospective double-blind study on the variability and interpretation of segmental effects. Reg Anesth Pain Med. 2001;26:147-155.
13 Patel V. Diagnostic modalities for low back pain. Semin Pain Med. 2004;2:145-153.
14 North R.B., Kidd D.H., Zahurak M., et al. Specificity of diagnostic nerve blocks: A prospective, randomized study of sciatica due to lumbosacral spine disease. Pain. 1996;65:77-85.
15 Sasso R.C., Macadaeg K., Nordmann D., et al. Selective nerve root injections can predict surgical outcome for lumbar and cervical radiculopathy: Comparison to magnetic resonance imaging. J Spinal Disord Tech. 2005;18:471-478.
16 Kelekis A.D., Somon T., Yilmaz H., et al. Interventional spine procedures. Eur J Radiol. 2005;55:362-383.
17 Fenton D.S., Czervionke L.F. Image-Guided Spine Intervention. Philadelphia: Saunders, 2003.
18 Windsor R.E., Falco F.J.E. Paraplegia following selective nerve blocks. Int Spinal Inject Soc Sci Newsl. 2001;4:53.
19 Huntoon M.A. Anatomy of the cervical intervertebral foramina: Vulnerable arteries and ischemic neurologic injuries after transforaminal epidural injections. Pain. 2005;117:104-111.
20 Rozin L., Rozin R., Koehler S.A., et al. Death during transforaminal epidural steroid nerve root block (C7) due to perforation of the left vertebral artery. Am J Forensic Med Pathol. 2003;24:351-355.
21 Furman M.B., Giovanniello M.T., O’Brien E.M. Incidence of intravascular penetration in transforaminal cervical epidural steroid injections. Spine. 2003;28:21-25.
22 Botwin K.P., Gruber R.D., Bouchlas C.G., et al. Complications of fluoroscopically guided transforaminal lumbar epidural injections. Arch Phys Med Rehabil. 2000;81:1045-1050.
23 Houten J.K., Errico T.J. Paraplegia after lumbosacral nerve root block: Report of three cases. Spine J. 2002;2:70-75.
24 Tiso R.L., Cutlerb T., Catania J.A., et al. Adverse central nervous system sequelae after selective transforaminal block: The role of corticosteroids. Spine J. 2004;4:468-474.
25 Stolker R.J., Vervest A.C.M., Ramos L.M.P., et al. Electrode positioning in thoracic percutaneous partial rhizotomy: An anatomical study. Pain. 1994;57:241-251.
26 Alleyne C.H.Jr, Cawley C.M., Sphengelaia G.G., et al. Microsurgical anatomy of the artery of Adamkiewicz and its segmental artery. J Neurosurg. 1998;89:791-795.
27 Hasegawa T., Mikawa Y., Watanabe R., et al. Morphometric analysis of the lumbosacral nerve roots and dorsal root ganglia by magnetic resonance imaging. Spine. 1996;21:1005-1009.