Transducers and Instrumentation
Christopher J. Gallagher and John C. Sciarra
Piezoelectric Effect
Understanding the piezoelectric effect takes the mystery out of “Just what the hell is that little gizmo at the end of my probe, anyway?”
To make a sound wave, you need to wiggle something.

No go. We need a better way to get so much wiggling. The guy banging the gong just won’t do.
Millions of times per second? Better go to electricity, that’s the only thing that can give you that many wiggles per second. But how to get electricity to wiggle something? Electrify a gong?

(Who the hell figures this stuff out the very first time, I want to know.)
Crystal Thickness and Resonance
A thin crystal resonates at a high frequency (think of a thin wine glass that goes “TING!” when you tap it). A thick crystal (think glass beer stein; better yet, get one and fill it to the top if you’re slogging through this physics junk) resonates at a low frequency. No big shocker there.
Axial and Lateral Resolution
(Here again, we’re chopping up stuff that should run together.)
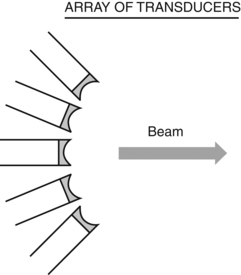
Arrays
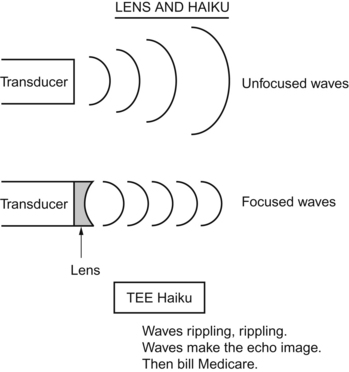
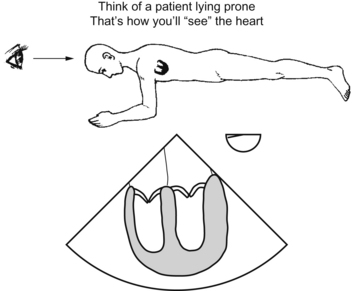
To get the vast amount of information necessary for a “movie of the heart,” you could have one “supertransducer” sweeping back and forth. That doesn’t fly, though; instead, modern TEE relies on a bunch of transducers spread out and all looking in the same direction. Some kick-ass mathematics and computer stuff straighten all those signals out.
Instrumentation
A quarter-million-dollar rolling TV?
More knobs than Miami Beach has sand granules?
That’s MY summary of TEE instrumentation, but the test may go into more detail than that. The scope itself is a modified gastroscope with the precious transducer at the end. Ancient probes, unearthed in Pompeii, had only one plane or two planes, but all the modern ones have the omniplane capability.
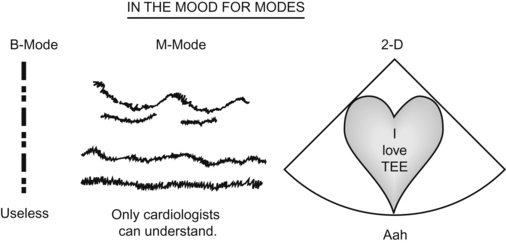
B-Mode, M-Mode, and Two-dimensional Echocardiography
B-mode
The “B” stands for “brightness.” This would just show different brightness at various interfaces and isn’t of much use to us. It is an “ice-pick” view.
Questions
Answers
1. True. When you press the freeze the machine stops sending signals. This may help cool the probe if it is overheating.
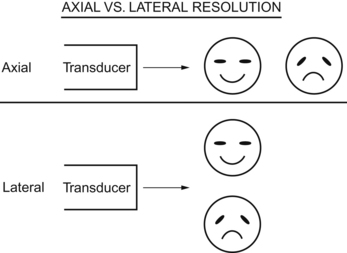
2. D. Beam width is the major determiner of lateral resolution. Make your whole scanning sector smaller for better resolution.
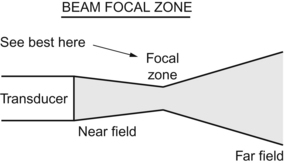
4. B. The focal point can be moved, but it is between the near field and far field. It is in the focal zone, which begins right after the focal length.