CHAPTER 14 Transconjunctival Approach to Resection of Lower Eyelid Herniated Orbital Fat
The transconjunctival approach to removal of herniated orbital fat is the preferred method of treatment in patients who have only herniated orbital fat with minimal or no evidence of dermatochalasis (excess skin) and no hypertrophic orbicularis oculi muscle. This technique is also especially advantageous for:
If there is horizontal lower eyelid laxity, this procedure can be easily combined with a horizontal eyelid tightening through a tarsal strip procedure (see Chapter 1).
A contraindication to this procedure is with patients with minimal lower eyelid fat, inferior orbital rim or nasojugal hollowing and depression. In these patients, fat repositioning or cheek–midface lifting are indicated (Chapters 17 and 19).
Surgical technique
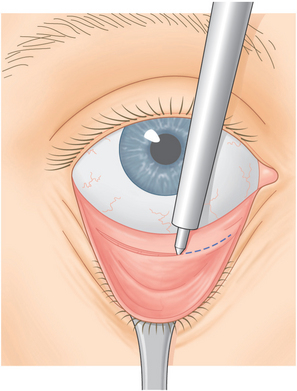
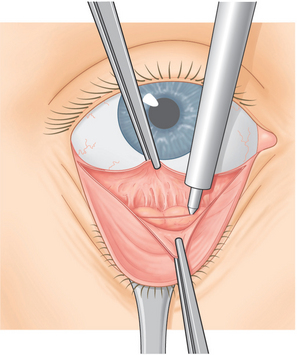
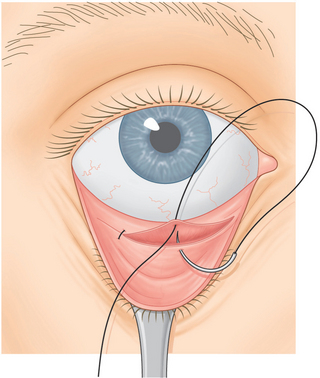
A Colorado needle or disposable cautery (Solan Accu-Temp, Xomed Surgical Products, Jacksonville, FL) is applied to the inferior palpebral conjunctiva. The Colorado needle or cautery are used to cut conjunctiva from the medial to temporal end of the eyelid halfway between the inferior palpebral fornix and the inferior tarsal border (Fig. 14-1). The surgeon grasps the inferior edge of the severed palpebral conjunctiva while the assistant grasps the adjacent, more superior edge with forceps and the assistant pulls the Desmarres retractor downward (Fig. 14-2). The two forceps are pulled apart. Further dissection with the Colorado needle or disposable cautery is carried out through Müller’s muscle and capsulopalpebral fascia until fat is seen.
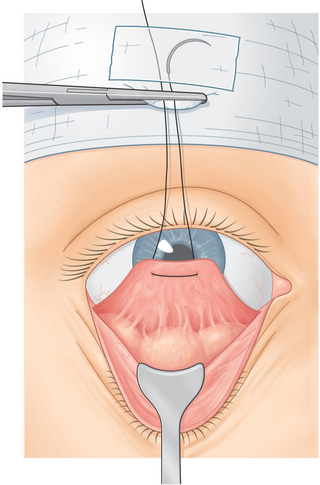
A 4-0 black silk double arm suture is passed through the inferior edge of conjunctiva, Müller’s muscle, and capsulopalpebral fascia and the suture arms are pulled upward and clamped to the drape (Fig. 14-3).
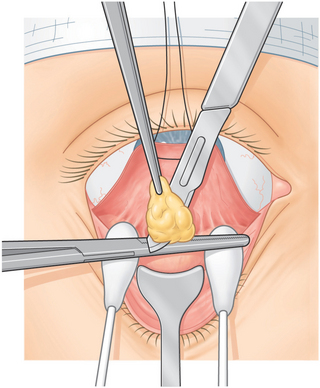
The temporal herniated orbital fat is isolated, and the fat that prolapses with gentle pressure on the eye is clamped with a hemostat and cut along the hemostat blade with a No. 15 Bard–Parker blade. Then cotton-tipped applicators are placed underneath the hemostat as a Bovie cautery is applied over the fat stump. The surgeon grasps the fat with a forceps before it is allowed to slide back into the orbit to make sure that there is no residual bleeding that might cause a second retrobulbar hemorrhage.1
After the first temporal fat pad is removed, the surgeon applies additional pressure to the eye to determine whether there is a second temporal fat pad.2 If a second temporal fat pad is found, it is also removed. The central and nasal fat pads are then removed in a similar manner (Fig. 14-4).
The 4-0 silk suture that attaches conjunctiva, Müller’s muscle, and capsulopalpebral fascia to the superior drape is then removed. Conjunctiva is reapproximated with three 6-0 plain catgut buried sutures (Fig. 14-5). Gentamicin (Garamycin) is applied over the eye.
Postoperative care
To reduce edema postoperatively the patient lies in bed with the head approximately 45° higher than the rest of the body. Nurses should check for bleeding associated with proptosis, pain, or loss of vision every 15 minutes for the first two to three hours postoperatively or until the patient leaves the surgical facility. Every hour thereafter until bedtime, the family or patient should monitor the patient’s ability to count fingers and should check for residual proptosis and pain. If the patient cannot count fingers or has marked proptosis or pain, the family should take him or her to the emergency room. If loss of vision occurs secondary to retrobulbar hemorrhage, it could easily be detected by opening the incision involved.1 Garamycin ointment is applied to the eyes twice a day for the first two weeks.
Complications
Although this procedure has not caused any motility problems, in several patients in whom this procedure was combined with a tarsal strip procedure, ocular motility restriction and diplopia occurred secondary to scar tissue that developed between the globe and the temporal inferior orbital wall.3 There is also the possibility of residual herniated orbital fat in which case a second transconjunctival approach removal is indicated. Although a sunken lower eyelid is possible, it is fortunately rare with good patient selection. If it occurs, it can be treated with a cheek mid-face lift (Chapter 23), or fat injections, or grafts.
Results
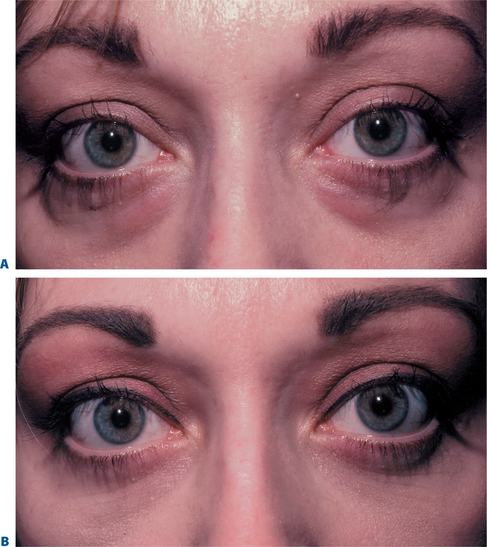
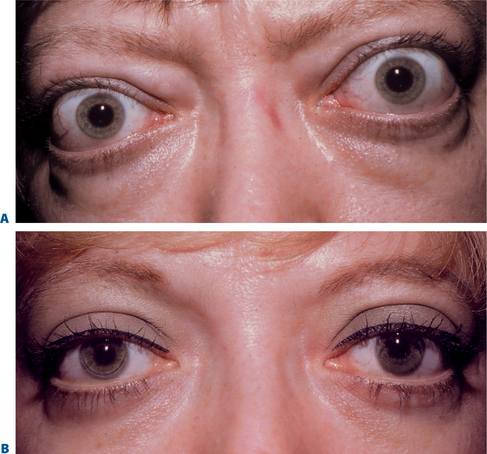
I have performed the transconjunctival approach in more than 1000 patients (Figs 14-6 & 14-7). The procedure has the advantage of causing less eyelid retraction and ectropion than with the skin flap or skin muscle flap approaches because the external lamellae is not manipulated. I believe that there is less ecchymosis because the orbicularis muscle and skin are not severed. There tends to be more conjunctival chemosis immediately postoperatively with this procedure than with the external technique. If it occurs, it is treated with pressure applied over the closed eyelids.4
1 Putterman AM. Temporary blindness after cosmetic blepharoplasty. Am J Ophthalmol. 1975;80:1081-1083.
2 Putterman AM. The mysterious second temporal fat pad. Ophthal Plast Reconst Surg. 1985;1:83-86.
3 Putterman AM. Acquired strabismus following cosmetic blepharoplasty [Letter to the Editor]. Plast Reconst Surg. 2004;113:1069-1071.
4 Putterman AM. Treatment of conjunctival prolapse. Arch Ophthalmol. 1995;113:553-554.