CHAPTER 26 Transblepharoplasty browlift
Physical evaluation
• In evaluation of the patient considering a transblepharoplasty browpexy, one performs a systematic assessment of the forehead and adjacent scalp and hairline, brow, upper eyelid and orbit.
• The patients should be examined with the frontalis muscle at rest.
• The central and lateral forehead and eyebrow and upper eyelid are evaluated separately.
• The brow is evaluated for prior incisions, symmetry, ptosis, and the relationship of the brow to the supraorbital rim.
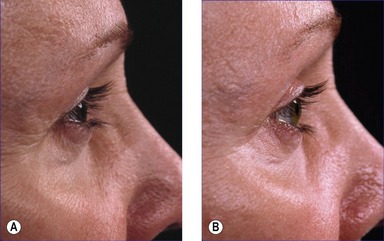
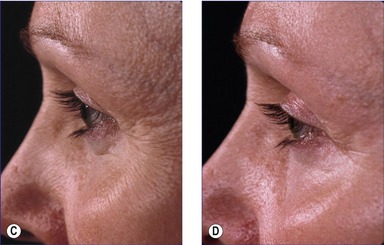
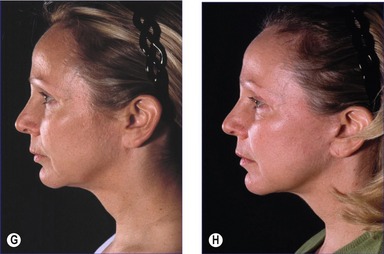
• In women, the brow should arch above the supraorbital rim peaking above the lateral limbus. In men, the brow traverses the supraorbital rim in a more horizontal manner. Signs of brow ptosis include descent below the supraorbital rim, and lateral upper eyelid hooding.
• Kaye describes a method in assessing the need for a browlift with or without an upper eyelid blepharoplasty. The surgeon gently elevates the forehead and brows in order to visualize the effect on the eyelid ptosis.
• As patients age, they may present with ptosis of the forehead and eyebrows and laxity and excess of the upper eyelid skin. These patients may not achieve an optimal result with blepharoplasty or browlift alone and would be ideal candidates for a transblepharoplasty browpexy.
Anatomy
Innervation to the forehead and supraorbital musculature is derived from the facial nerve (CN 7).
Technical steps
1. Upper eyelid incision and blepharoplasty.
2. If the browpexy is performed as an isolated procedure, or if a skin-only blepharoplasty is performed, a transverse incision is made through the orbicularis oculi muscle.
3. Develop a plane deep to the orbicularis oculi muscle and dissect in the cephalad direction approximately 3–4 cm above the supraorbital rim and 1–2 cm beyond the eventual point of fixation.
4. Release the nasal brow and perform corrugator and/or procerus excision.
5. Browpexy absorbable suture placement beginning at central eyebrow moving laterally (three or more sutures are usually placed). Sutures are placed securing the inferior surface of the orbicularis oculi to the periosteum and frontalis muscle deep at the desired level. The suture placement is overcorrected and differential.
6. Examine result of suture placement for contour symmetry and achieved brow elevation.
7. Replacement of sutures should be done to correct asymmetry and to correct obvious dimpling of the brow with a smaller bite of the underside of the orbicularis oculi muscle.
Postoperative care
• Acutely, the head is kept elevated and cool iced gauze is applied at the upper eyelids and brow region. Blood pressure is maintained within normal limits.
• The incision is managed with Steristrips, which are kept in place until suture removal at 3–4 days and then replaced.
• Long-term management includes gentle brow massage in cases of dimpling which resolves spontaneously and reassurance that forehead sensation will be restored.
Complications
Pearls & pitfalls
Pearls
• Dissect in the submuscular plane cephalad to the level of your intended suture placement. This will help smooth the contour of the brow and prevent notching above the brow.
• Place the sutures with a medial to lateral ascent.
• Obtain meticulous hemostasis and perform prudent dissection when possible with the Colorado tip electrocautery.
• Only elevate the middle to lateral third of the brow with suture placement. Elevation of the medial brow may be achieved by resecting the corrugator, procerus and medial orbicularis oculi muscle resection.
• Before wound closure, observe the patient for symmetry, contour abnormalities that could be remedied by suture replacement.
Pitfalls
• Do not elevate the middle or medial third of the brow as much as the lateral brow.
• Pay close attention to the location of the supraorbital and supratrochlear nerves.
• The goals of the surgery and eyebrow contour are different for a female or male patient.
• Do not use this procedure alone in cases of severe central brow ptosis.
Adamson PA, Johnson CM, Anderson JR, Dupin CL. The forehead lift: a review. Arch Otolaryngol. 1985;111:325.
Kaye BL. The forehead lift: a useful adjunct to the face-lift and blepharoplasty. Plast Reconstr Surg. 1977;60:161.
Knize DM. An anatomically based study of the mechanism of the eyebrow ptosis. Plast. Reconstr Surg. 1996;97:1321–1333.
Niechajev I. Transpalpebral browpexy. Plast Reconstr Surg. 2004;113:2172.
Paul MD. Subperiosteal transblepharoplasty forehead lift. Aesthetic Plast Surg. 1996;20:129.
Paul MD. The surgical management of upper eyelid hooding. Aesthetic Plast Surg. 1989;13:183.
Ramirez OM. Transblepharoplasty forehead lift and upper face rejuvenation. Ann Plast Surg. 1996;37:577.
Riefkohl R, Kosanin R, Georgiade GS. Complications of the forehead-browlift. Aesthet Plast Surg. 1983;7:135.
Sokol AB, Sokol TP. Transblepharoplasty brow suspension. Plast Reconstr Surg. 1982;69:940.
Zarem HA, Resnick JL, Carr RM, Wootton DG. Browpexy: lateral orbicularis muscle fixation as an adjunct to upper blepharoplasty. Plast Reconstr Surg. 1997;100:1258.