Chapter 36 Transaxial Anterior Lumbar Interbody Fusion Using The AxiaLIF System
The rate of minimally invasive spine surgery (MISS) has increased in recent years because of the development of technology and new approaches to the spine. Open lumbar surgery is disadvantageous because of the need of muscle and neural retraction, ligamentous and osseous dissection, disruption of the anulus, and vascular exposure [1]. For most MISS techniques, the approach is like those used in open approaches to the spine—that is, posterolateral and extraforaminal exposure of the disc space and incision or excision of the anulus [2–9].
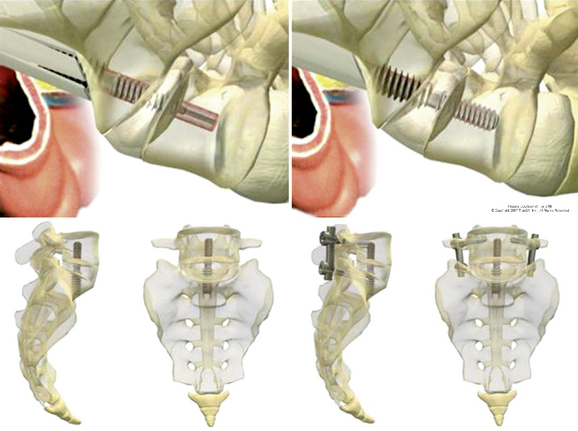
When stabilization of the lumbosacral spine is indicated, however, a less invasive axial lumbosacral surgery offers significant advantages over MISS techniques [10–13]. This technique, transaxial anterior lumbar interbody fusion, uses a percutaneous, presacral approach. Use of the AxiaLIF System, manufactured by TranS1, Inc. (Wilmington, NC), is described in this chapter, first for stabilization at one level, and then for stabilization at two levels.*
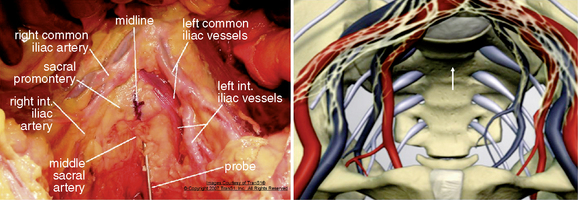
Presacral anatomy
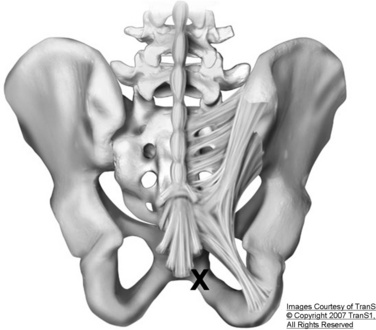
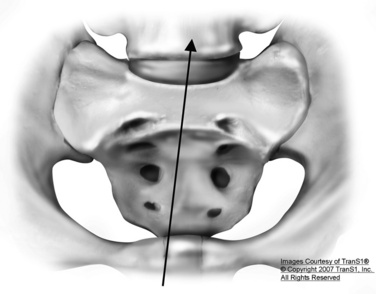
Axial anterior spinal access is accomplished by dilating an osseous tract through the upper sacrum. The midline entry point in to the sacral promontory at approximately the S1-S2 interspace is relatively bare area compared with the more complex vascular and neural structures encountered over the lower lumbar spine (Fig. 36-1) [14,15]. At the sacral level, the iliac vessels and their accompanying sympathetic hypogastric nerves have diverged by several centimeters. The middle sacral artery follows a variable course over the sacrum but is usually small at the S1-S2 level. The rectum and sigmoid colon are easily mobilized in the presacral region. The presacral space is filled with areolar tissue and fat between the parietal peritoneum on the anterior sacrum and the visceral peritoneum on the rectum (see Fig. 36-1). The space is relatively easily traversed with a blunt obturator or needle.
AxiaLIF at one level
Procedure
Patient Positioning
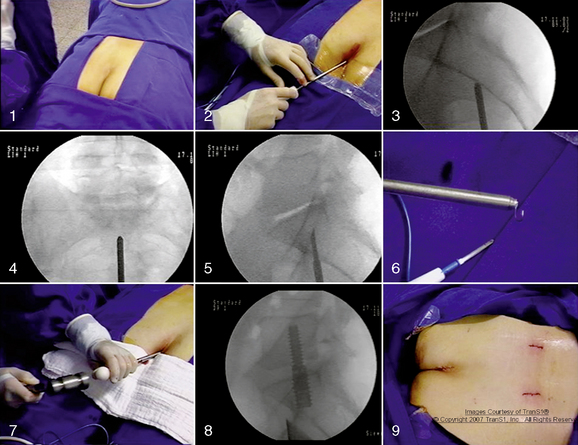
In the AxiaLIF technique, multiplanar imaging with magnetic resonance (MRI) and/or computed tomography (CT) is essential to determine whether the patient is a proper surgical candidate. A standard bowel preparation is performed. The patient is placed on a fluoroscopically compatible surgical table in the prone position (Fig. 36-2). Bolsters are positioned under the hips and shoulders to raise the sacrum and establish proper lumbosacral posture. A catheter is inserted into the rectum to allow insufflation of air. The operative site is prepared with an adhesive barrier to exclude the perineum. Two C-arm fluoroscopic units are positioned to allow frontal and lateral (biplanar) fluoroscopic visualization of the lumbosacral region. The procedure is currently performed using general anesthesia.
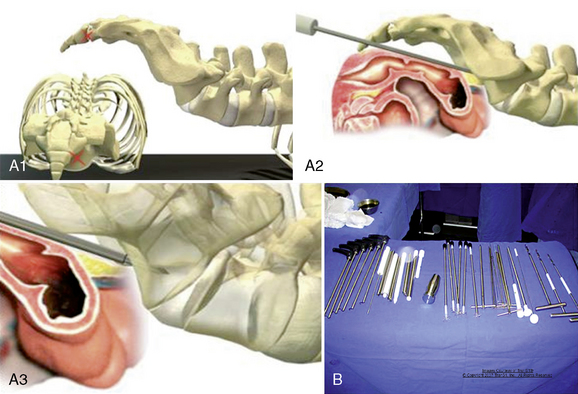
Approach
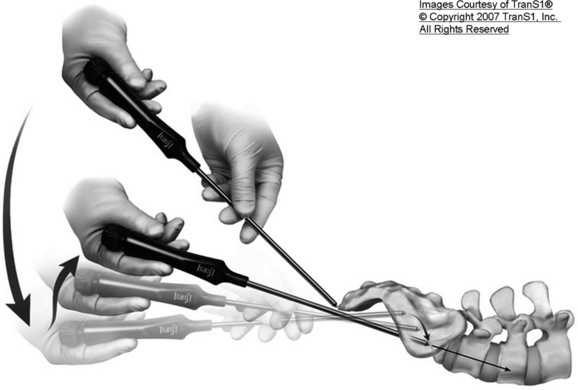
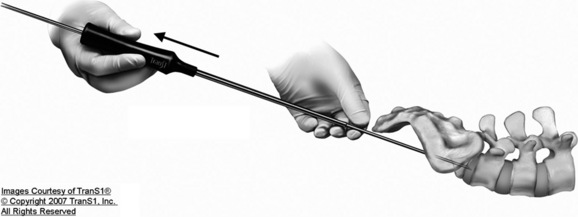
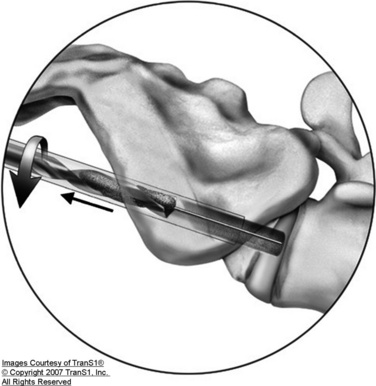
The AxiaLIF technique provides percutaneous access to the lumbar spine through the anterior presacral space (Fig. 36-3A). The developed instruments facilitate a safe and reproducible entrance to the L5-S1 disc space (Fig. 36-3B).
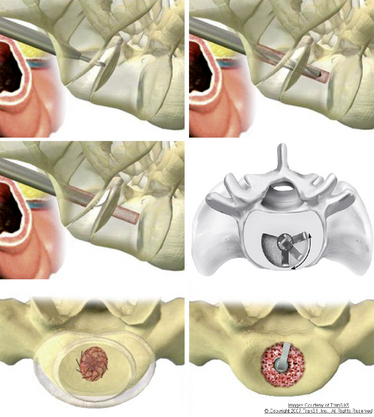
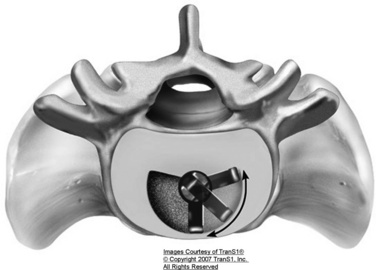
Radial Discectomy
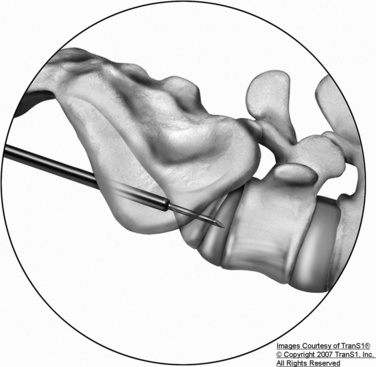
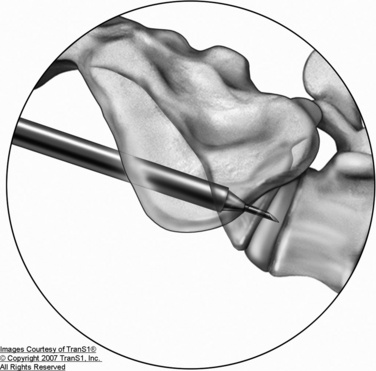
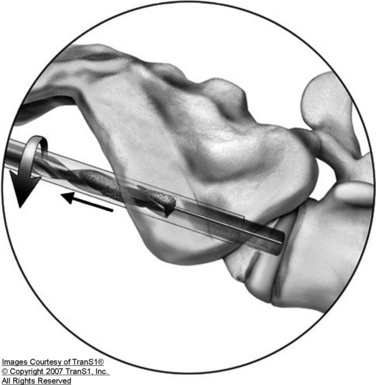
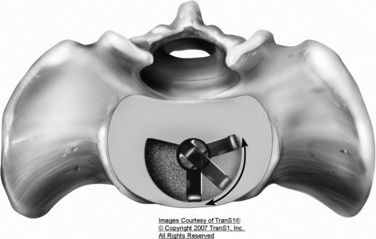
Axial disc access is accomplished through the 9-mm sacral working cannula. Custom MISS instruments for discectomy, end plate preparation, tissue removal, and bone grafting are inserted through the working cannula (Fig. 36-4). The instruments are monitored with biplanar fluoroscopy. Axial disc space entry facilitates the use of expansible, radial instruments that are aligned in the plane of the disc space and end plates. Thus minimally invasive discectomy is potentially easier and more complete with axial disc space entry than with horizontally oriented, posterolateral approaches.
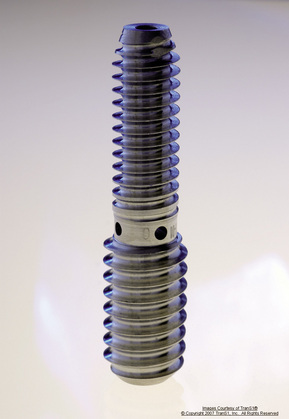
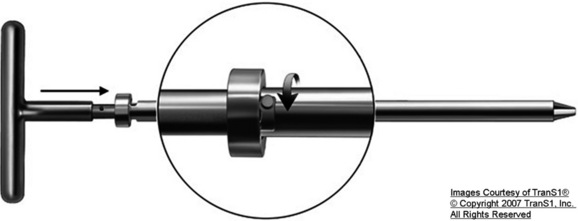
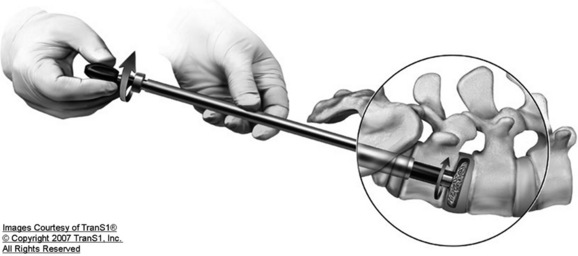
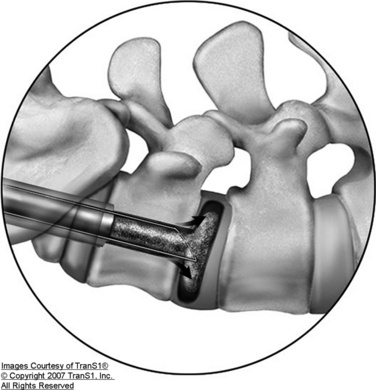
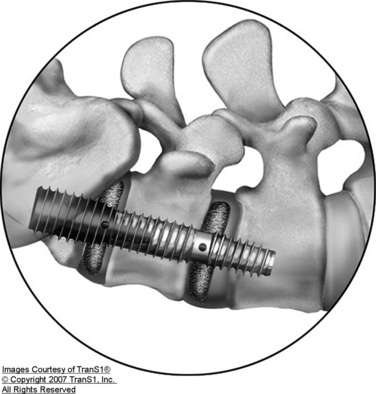
Distraction and Dynamic Decompression
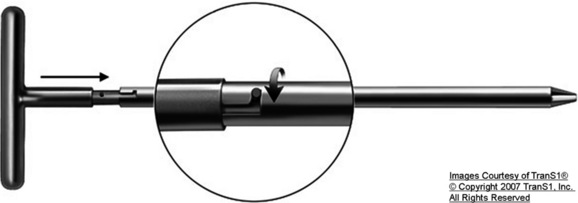
For the distraction, a 14-mm rod is inserted and engages the entirety of the transosseous tunnel from the sacrum to the L5 vertebral body. The rod is a proprietary temporary titanium device with a lumbar diameter of 9 mm and a sacral diameter of 12 mm. The differing diameters allow the rod to have two different thread pitches. When the rod is implanted (Fig. 36-5), its differential pitch produces distraction of the vertebral bodies at a rate that depends on the difference of the thread pitches. This dynamic distraction allows the surgeon to accurately reproduce the required disc height restoration and indirectly decompress the neural foramen.
Treatment Alternatives
Case Series [16,17]
Assessment consisted of the following:
 Measurement of disc height and fusion through radiography and CT evaluation by an independent radiologist
Measurement of disc height and fusion through radiography and CT evaluation by an independent radiologist Pain assessment by means of a visual analog scale (VAS), Oswestry Disability Questionnaire, and the SF-36 Health Survey
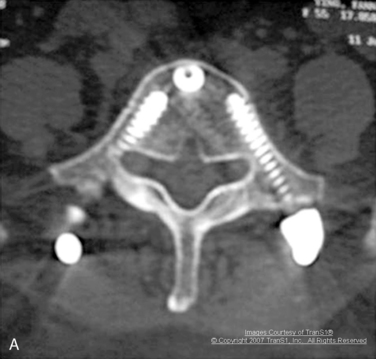
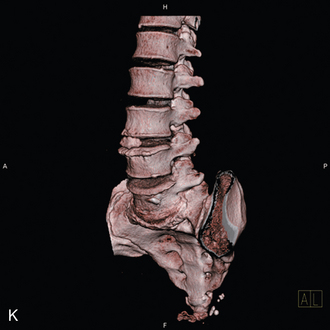
Pain assessment by means of a visual analog scale (VAS), Oswestry Disability Questionnaire, and the SF-36 Health SurveyA 45-year-old woman had discogenic-type low back pain that intensified with standing and flexion. In addition, she had neurogenic claudication symptoms. Preoperative MRI and radiography showed narrowing and desiccation of the L5-S1 disc space with a spondylolisthesis grade II (Fig. 36-7). She underwent the AxiaLIF procedure at the L5-S1 level (Fig. 36-8). Radiographs obtained 12 months after surgery showed osseous bridging of L5-S1 and reduction of the spondylolisthesis (Fig. 36-9). CT scans demonstrated no evidence of radiolucency on the pedicle screws and the distraction rod (Fig. 36-10) and, along with a three-dimensional reconstruction, also showed solid osseous fusion of the L5-S1 interspace (Fig. 36-11).

Figure 36–7 Case Study 36.1: Preoperative sagittal MRI (B) and lateral radiograph (A) shows narrowing and desiccation of the L5-S1 disc space with a spondylolisthesis grade II.
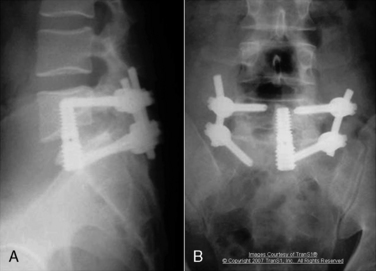
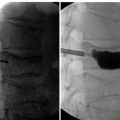
Figure 36–9 Case Study 36.1: Lateral (A) and anteroposterior (B) radiographs obtained 12 months after surgery show osseous bridging of the L5-S1 interspace and reduction of the spondylolisthesis.
in VAS, Oswestry, and SF-36 values measured again at 2 years after surgery. The mean VAS score decreased from a preoperative value of 8.3 to 3.4. The mean Oswestry Disability Index improved from 43.1 to 21.0. Radiographic analysis concluded that there was no evidence of implant back-out, damage, bone resorption, fractures, or sacral abnormalities.
Two measurements of the disc height were made preoperatively and postoperatively, one in the midline and the other in the posterior border of the disc space. Preoperatively, mean midline disc height was 6.06 (range 2-11), and mean posterior border disc height was 4.8 (range 2-9). Postoperatively, the mean midline disc height was 7.5 [range 5–11], and mean posterior border disc height was 6.06 (range 3-9). CT scans demonstrated of fusion rate to be 89.5% at 12-month follow-up, and 94.7% at 30 months after surgery (18 of 19 patients).
AxiaLIF at two levels
The AxiaLIF (Axial Lumbar Interbody Fusion) 2L System (TranS1, Inc.) includes surgical instruments for “creating a safe and reproducible presacral access route to the L4-S1 vertebral bodies [18].” The technique features instrumentation to enable standard of care fusion principles, distraction, and stabilization of the anterior lumbar column while mitigating the soft tissue trauma associated with traditional lumbar fusion through open surgical incisions. With the use of this system, the lumbar spine is accessed through an axial channel in the sacrum. This approach spares the supporting soft tissue including muscles and ligaments which reduces pain in recovery and the chances of soft tissue associated complications.
Contraindications
The AxiaLIF 2L System and procedure should not be used in patients with the following conditions:
Precautions
Preoperative
Portions of this system are supplied nonsterile and need to be cleaned and sterilized according to the instructions in the product insert [18].
Procedure
Step 1: Access and Trajectory
Step 2: Discectomy at L5-S1
NOTE: The blade must be retracted before being removed from the disc space.
NOTE: Flush and aspirate as needed with saline, adding antibiotic according to standard procedure.
Step 3: Bone Grafting at L5-S1
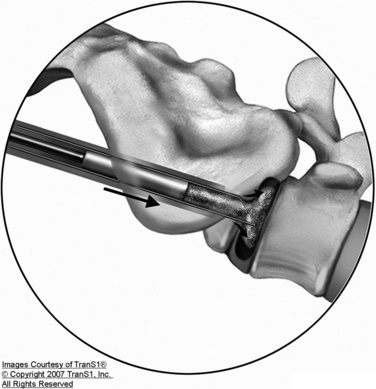
Step 4: Advance Access to L4-L5
NOTE: The blade must be retracted before being removed from the disc space.
Tissue Extractors are used to remove disc material loosened by the cutting devices. Tissue Extractors may be used after each cutter or after cutting is mostly complete (Fig. 36-39), as follows:
Step 6: Bone Grafting at L4-L5
Step 7: Implant Selection and Delivery
L4-L5 implant selection

Figure 36–44 Use of the .092-inch Guide Pin to locate the cephalad L4 end plate and mark it with a clamp.

Figure 36–45 Use of the .092-inch Guide Pin to locate the caudal L5 end plate and mark it with a clamp.
A Fixation Wire is then used to anchor the Exchange Cannula to the sacrum, as follows:
L4-L5 implant delivery
L5-S1 implant selection
L5-S1 implant placement
Step 8: Graft Material
Potential Complications and Management
The complications and management are the same described in this chapter for AxiaLIF at one level.
Case Series [19]
CASE STUDY 36.2
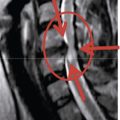
A 38-year-old man had axial pain with 2 years’ evolution. Results of a discogram were positive at L4-L5 and L5-S1. MRI and lateral radiographs showed spondylolisthesis grade I as well as narrowing and desiccation of the L5-S1 disc space with Modic II changes (Fig. 36-52A). The patient underwent the AxiaLIF 2L Procedure. Radiographs performed 12 months after surgery demonstrated solid fusion of L4-L5 and L5-S1, and CT scanning confirmed solid fusion of the L4-L5 and L5-S1 interspaces (Fig. 36-52B to D).
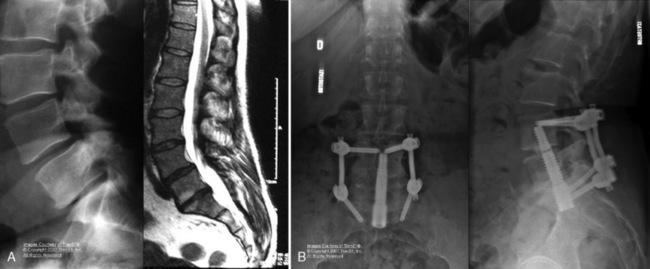
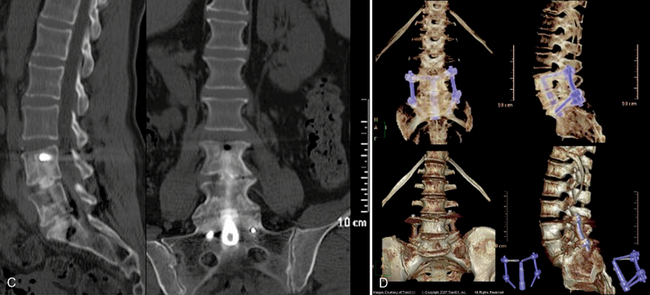
Figure 36–52 Case Study 36.2: (A) Preoperative sagittal magnetic resonance image and lateral radiograph show a black disc L4-L5 with spondylolisthesis grade I and a narrowing and desiccation of the L5-S1 disc space with Modic II changes. (B) Postoperative anteroposterior and lateral radiographs shows solid fusion of the L4-L5 and L5-S1 interspaces 12 months after surgery. (C) One year postoperatively, sagittal and coronal computed tomography scans show solid fusion of the L4-L5 and L5-S1 interspaces. (D) Three-dimensional reconstruction shows fusion at both levels.
was conducted by means of the Visual Analog Scale (VAS), Oswestry Disability Questionnaire, and SF-36 Health Survey.
1 Perez-Cruet M.J., Fessler R.G., Perin N.I. Review: Complications of minimally invasive spinal surgery. Neurosurgery. 2002;51(Suppl.):S26-S36.
2 Leu H.F., Hauser R.K. Percutaneous endoscopic lumbar spine fusion. Neurosurg Clin N Am. 1996;7:107-117.
3 Mathews H.H. Percutaneous interbody fusion. Orthop Clin North Am. 1998;29:647-653.
4 McAfee P.C., Regan J.J., Geis W.P., Fedder I.L. Minimally invasive anterior retroperitoneal approach to the lumbar spine: Emphasis on the lateral BAK. Spine. 1998;23:1476-1484.
5 Muhlbauer M., Pfisterer W., Eyb R., Knosp E. Minimally invasive retroperitoneal approach for lumbar corpectomy and anterior reconstruction: Technical note. J Neurosurg. 2000;93(Suppl.):161-167.
6 O’Dowd J.K. Laparoscopic lumbar spine surgery. Eur Spine J. 2000;9(Suppl. 1):S3-S7.
7 Olinger A., Hildebrandt V., Mutschler W., Menger M.D. First clinical experience with an endoscopic retroperitoneal approach for anterior fusion of lumbar spine fractures from levels T12 to L5. Surg Endosc. 1999;13:1215-1219.
8 Regan J.J., Yuan H., McAfee P.C. Laparoscopic fusion of the lumbar spine: Minimally invasive spine surgery: A prospective multicenter study evaluating open and laparoscopic lumbar fusion. Spine. 1999;24:402-411.
9 Thalgott J.S., Chin A.K., Ameriks J.A., et al. Minimally invasive 360 degrees instrumented lumbar fusion. Eur Spine J. 2000;9(Suppl. 1):S51-S56.
10 Cragg A., Carl A., Casteneda F., et al. New percutaneous access method for minimally invasive anterior lumbosacral surgery. J Spinal Disord Tech. 2004;17:21-28.
11 Cragg A., Carl A., Casteneda F., et al. Percutaneous axial lumbar spine surgery (AxiaLIF). In: Perez Cruet M., Khoo L., Fessler R.G., editors. An Anatomical Approach to Minimally Invasive Spine Surgery. St. Louis: Quality Medical, 2006. 38-1–38-17
12 Ledet E., Tymeson M., Salerno S., et al. Biomechanical evaluation of a novel lumbosacral axial fixation device. J Biomech Eng. 2005;127:929-933.
13 Khoo L., Marotta N., Cosar M., Pimenta L. Novel minimally-invasive presacral approach and instrumentation technique for anterior l5–s1 intervertebral discectomy and fusion: Technical description and case presentations. Neurosurg Focus. 2006;20(1):E9.
14 Ledet E.H., Carl A.L., Cragg A. Novel lumbosacral axial fixation techniques. Expert Rev Med Devices. 2006;3:327-334.
15 Yuan P., Day T., Albert T., et al. Anatomy of the percutaneous presacral space for a novel fusion technique. J Spinal Disord Tech. 2006;19:237-241.
16 Asgarzadie F., Khoo L., Cosar M., Marotta N., Pimenta L. One Year Outcomes of Minimally-Invasive Presacral Approach And Instrumentation Technique For Anterior Lumbosacral Intervertebral Discectomy And Fusion. Spine J. 2007;7(5):26S-27S.
17 Minimal Invasive Percutaneous Presacral Axial Lumbar Fusion (AxiaLIF) – Prospective Clinical and Radiographic Results After 36 Months Follow-up. Presented at Weill Cornell Medical College Meeting in 2007.
18 AxiaLIF®. The Least Invasive Solution to Lumbar Fusion. 2009 Available at http://www.trans1.com/products
19 Two Levels Presacral Axial Lumbar Interbody Fusion (AxiaLIF) – A Prospective 12 Months Follow up: Clinical And Radiological Results. Presented at SpineWeek 2008 in Geneva.