Tracheal Intubation and Endoscopic Anatomy
Airway Anatomy
Upper Airway
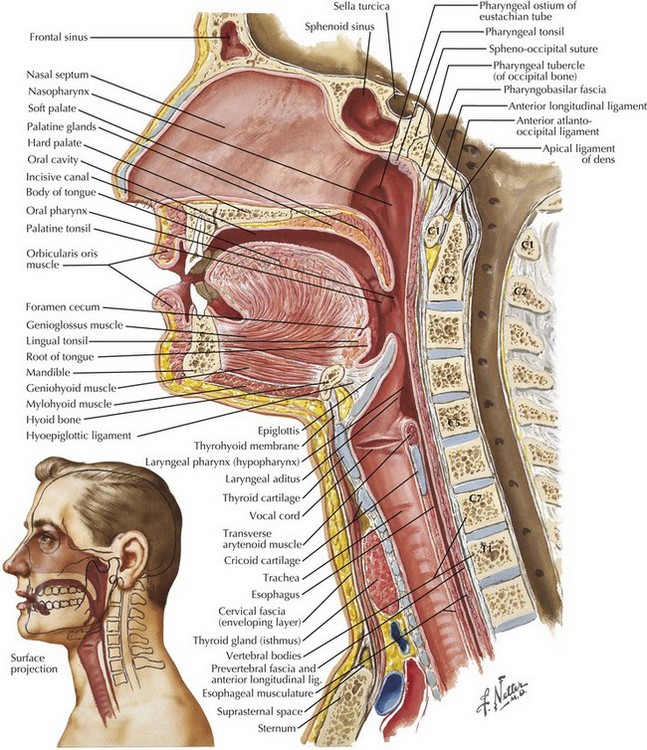
The upper airway consists of the nose, mouth, pharynx, and larynx. There are three pharyngeal segments: (1) nasopharynx, posterior to the soft palate; (2) oropharynx, posterior to the tongue from the tip of the uvula to the tip of the epiglottis; and (3) laryngopharynx, posterior to the epiglottis (Fig. 45-1). The pharyngeal segments are collapsible because the anterior and lateral walls lack bony support.
Larynx
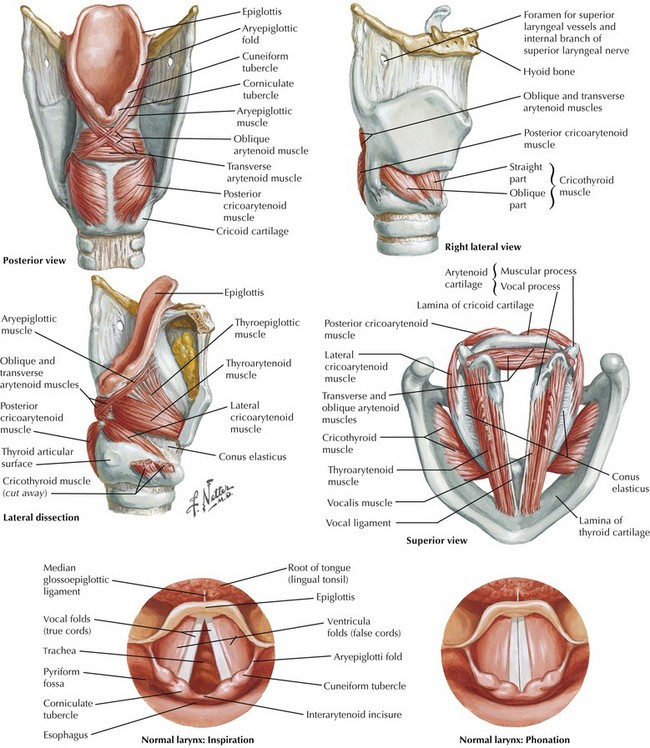
The larynx serves as the connecting structure between the upper and lower airways (Fig. 45-2). The adult larynx extends from the 4th to the 6th cervical vertebra, and it is composed of nine cartilages, with six paired and three single. The three single cartilages include the thyroid, cricoid, and epiglottis. The paired arytenoid cartilages secure the vocal cords to the larynx. The endolarynx is constructed of two pairs of folds that form the supraglottis and glottis.
Note the location of the superior laryngeal nerve (important for nerve block anesthesia) adjacent to the hyoid bone (Fig. 45-2). Motor innervation of the laryngeal muscles is through the superior laryngeal nerve (cricothyroid muscle) and recurrent laryngeal nerve (remainder of laryngeal muscles). Stimulation of the supraglottic region, especially where the piriform recesses blend with the hypopharynx, can result in laryngospasm with complete glottic closure.
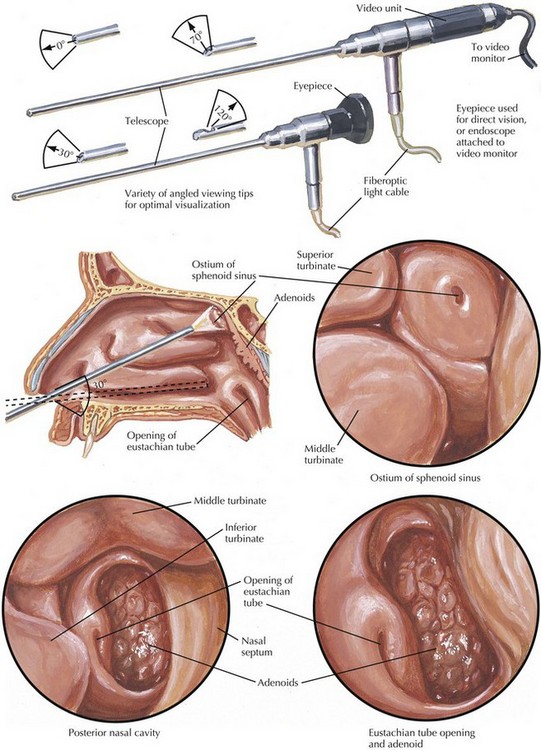
Nose and Nasopharynx
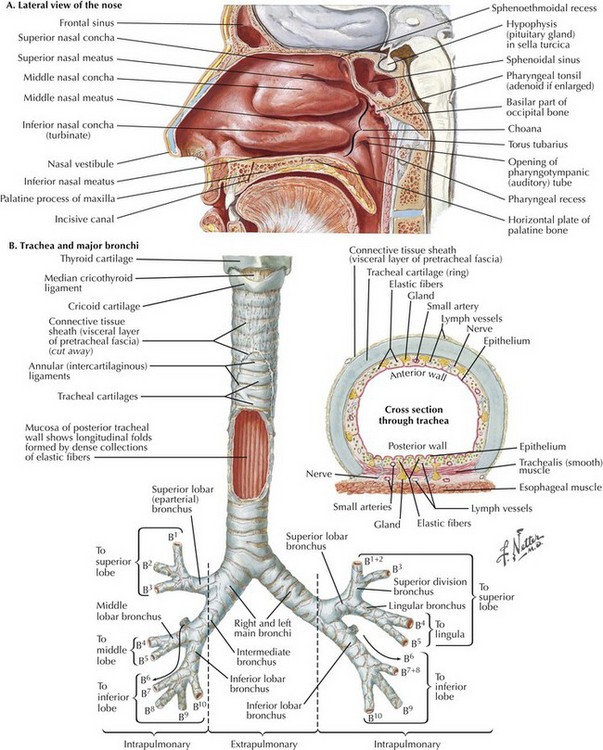
Nasotracheal intubation is an alternative approach to orotracheal intubation. The two nasal fossae extend from the nostrils to the nasopharynx. The nasal fossae are divided by the midline cartilaginous septum and medial portions of the lateral cartilages (Fig. 45-3, A). The nasal fossa is bounded laterally by inferior, middle, and superior turbinate bones. The mucosa covering the middle turbinate is highly vascular, receiving its blood supply from the anterior ethmoid artery, and also contains a large plexus of veins. The middle turbinate is susceptible to avulsion by trauma and is associated with massive epistaxis. The paranasal sinuses (sphenoid, ethmoid, maxillary, and frontal) open into the lateral wall of the nose. The inferior turbinate usually limits the size of the nasotracheal tube.
Lower Airway
The lower airway consists of the trachea, bronchus, bronchioles, respiratory bronchioles, and alveoli. The adult trachea, which begins at the cricoid cartilage opposite the 6th cervical vertebra, contains 16 to 20 cartilaginous rings. The posterior part of the trachea is devoid of cartilage (Fig. 45-3, B). Pressure over the cricoid cartilage (Sellick maneuver) is often applied during rapid-sequence induction and intubation (RSI) to minimize the risk of aspiration in unfasted (full stomach), anesthetized, and paralyzed patients before intubation. However, cricoid pressure may distort airway anatomy, making intubation more difficult.
Indications for Intubation
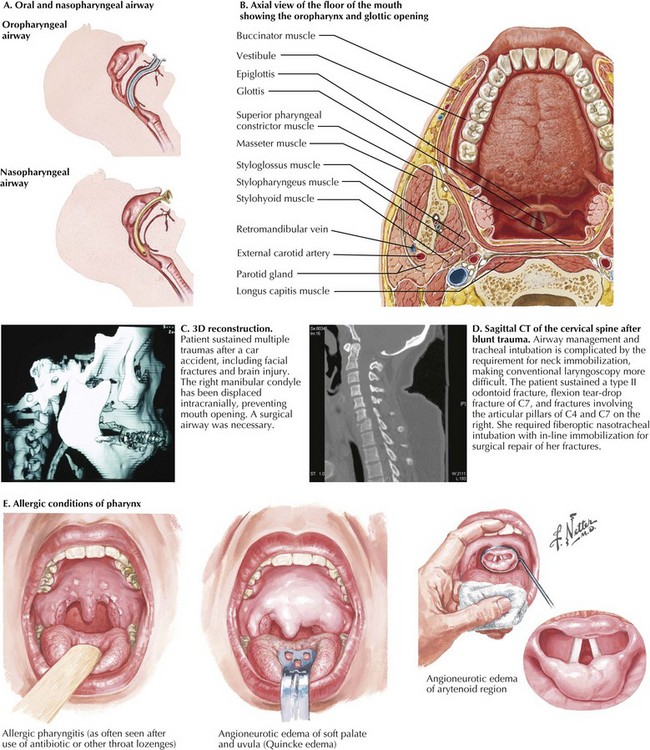
The nasopharyngeal airway is an uncuffed, trumpetlike tube that is inserted through the nasopharynx, bypassing the oropharynx and mouth. The distal end is just superior to the epiglottis and inferior to the base of the tongue. The proximal end has a flange to prevent the airway from migrating into the nose (Fig. 45-4, A).
Preintubation Airway Examination
Airway examination should include anatomic and pathologic factors that can predict likelihood of a difficult airway (Fig. 45-4, B). Anatomic factors that increase tracheal intubation difficulty include Mallampati class III (only soft palate visible when patient opens mouth wide and protrudes tongue), limited mouth opening, protruding maxillary incisors, narrow mouth width, cleft lip/palate, small oral cavity, large tongue, tumors, trauma, and infection.
Pathologic factors that further challenge practitioners include tumors, deep fascial plane infections of the face or neck, burns, congenital anomalies, airway trauma, thermal and inhalation injury, and cervical spine trauma (Fig. 45-4, C-E).
Laryngoscopy
After suitable anesthesia is given, an appropriate-sized laryngoscope blade is inserted to the right of the patient’s tongue, which must be displaced and compressed (Fig. 45-5, A). Head extension and the sniffing position facilitate line of sight for the practitioner to insert the tube through the vocal cords. With infants and neonates, use of a straight blade is preferred. Because of the proximity of the upper airway to the cervical spine (see Fig. 45-1), some movement of the atlanto-occipital and atlanto-axial segments generally occurs during laryngoscopy.
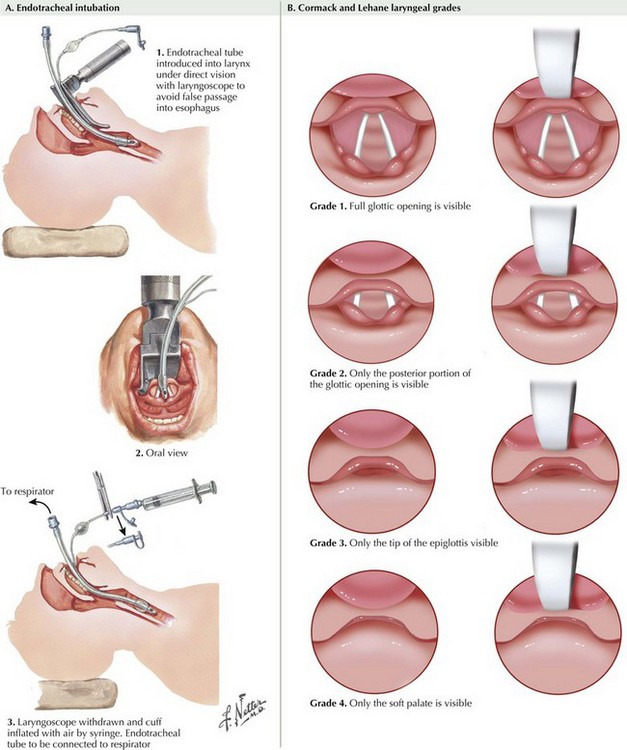
FIGURE 45–5 Laryngoscopy. (B illustrations courtesy of Mike Mustar, medical illustrator, MetroHealth Medical Center, Cleveland, Ohio.)
During intubation, different views of the glottic opening are achieved, depending on patient anatomy and practitioner skills (Fig. 45-5, B). Pressure over the thyroid cartilage often improves the view at laryngoscopy. The ETT is introduced through the vocal cords until the cuff disappears. Ventilation is confirmed by sustained presence of end-tidal carbon dioxide, auscultation of bilateral breath sounds with absence of air over the epigastrium, and chest rise. The tube is securely taped or tied at the appropriate depth. In adults, an average distance of 20 to 24 cm is required to place the distal end of the tube in the midtracheal position.
Flexible Fiberoptic Bronchoscopy
Nasotracheal Approach
As the nose is entered with the FOB, it is imperative to visualize the inferior and middle turbinates (Fig. 45-6). As the FOB is advanced from the anterior nasal cavity to the posterior nasal cavity, the following anatomic structures should be visualized:
Failed Intubation
It is essential to have contingency plans in the event that intubation is not successful. Such plans usually consist of BMV with oral and nasopharyngeal airways, a supraglottic device (e.g., laryngeal mask airway), or a surgical airway (see Chapter 2).
American Society of Anesthesiologists. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists task force on management of the difficult airway. Anesthesiology. 2013;118:251–270.
Cooper, RM, Pacey, JA, Bishop, MJ, McCluskey, SA. Early clinical experience with a new videolaryngoscope (GlideScope) in 728 patients. Can J Anaesth. 2005;52:191–198.
Crosby, E. Airway management after upper cervical spine injury: what have we learned? Can J Anesth. 2002;49:733–744.
Crosby, ET, Cooper, RM, Douglas, MJ, et al. The unanticipated difficult airway with recommendations for management. Can J Anaesth. 1998;45:757–776.
Kheterpal, S, Han, R, Tremper, KK, et al. Incidence and predictors of difficult and impossible mask ventilation. Anesthesiology. 2006;105:885–891.
Smith, CE, DeJoy, S. New equipment and techniques for airway management in trauma. Curr Opin Anaesthesiol. 2001;14:197–209.