Tracheal Gas Insufflation
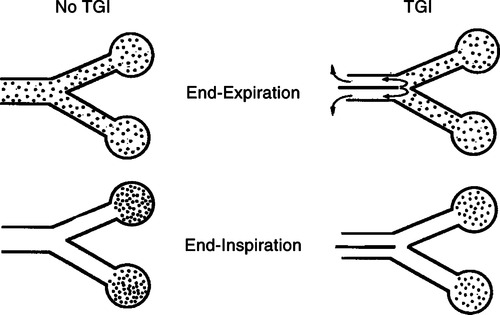
Tracheal gas insufflation (TGI): The addition of a secondary gas flow during mechanical ventilation at the level of the carina to wash CO2 from the deadspace of the large airways, endotracheal tube (ETT), and ventilator circuit (Figure 44-1).
A At end exhalation large airways, the ETT and the ventilator circuit deadspace contain a large amount of CO2.
B Washing the CO2 from these areas decreases the CO2 of the gas moving to the alveoli during the next inhalation.
C As a result, over time the arterial P2 decreases.
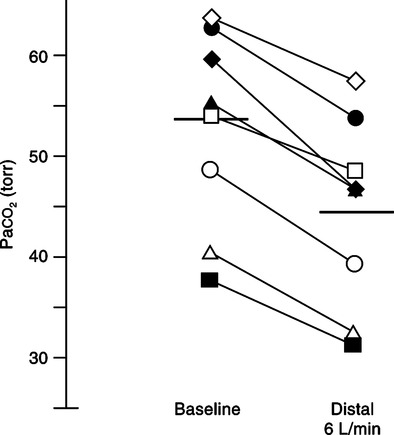
D Numerous case series in patients have demonstrated that TGI at flows of approximately 6 to 15 L/min decrease Paco2 (Figure 44-2).
E The greater the Paco2 at the time of initiating TGI, the greater the decrease in Paco2.
F The greater the TGI flow, the greater the effect on Paco2.
G The greater the volume of deadspace washed of CO2, the greater the effect on arterial Pco2.
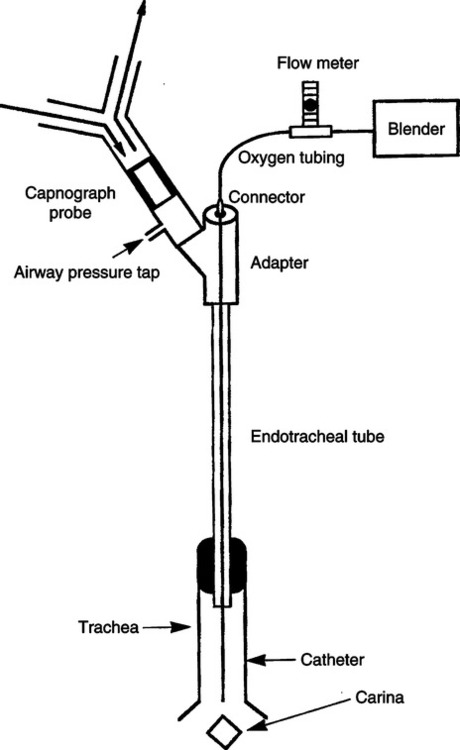
A Figure 44-3 illustrates a typical TGI system.
B A small-gauge catheter is placed into or along side the ETT with its tip setting just past the tip of the ETT in the trachea.
C In most settings the tube is directed toward the carina (direct TGI).
D However, the flow through the catheter may also be directed up toward the ETT (e.g., indirect or reverse TGI).
E TGI can also be applied continuously or intermittently (during exhalation only).
F By simply attaching the TGI catheter to a flowmeter, continuous flow TGI can be performed.
G To accomplish expiratory phase-only TGI, the flow delivery must be coordinated with the ventilator (i.e., activation of TGI flow must begin and end during the expiratory phase).
H There are also some data to show that tracheal gas exsufflation (TGE; negative pressure applied to the catheter during expiration) also reduces Pco2. However, TGE must be coordinated with the ventilator, only being applied during the expiratory phase.
A Humidification: Clearly the TGI flow must be humidified to avoid the development of dried retained secretions.
B Airway injury: A high flow of gas from the TGI catheter can cause the tip of the catheter to wipe in the airway causing injury to the tracheal wall.
C With TGE, humidification and airway injury are not problems because the system only removes gas from the airway.
D A major concern with TGI is the ability to shut down the system if there is an obstruction of the airway proximal to the tip of the catheter (i.e., between the ventilator circuit “wye” and the tip of the TGI catheter).
E If the TGI flow is not stopped when this occurs, rapid overdistention of the airway and the potential for barotrauma rapidly develop.
1. To avoid these problems the TGI system must shut down whenever the ventilator senses obstruction.
2. This is necessary regardless whether the TGI flow is continuous or intermittent.
F Direct TGI causes the total applied positive end-expiratory pressure (PEEP) to increase because the TGI flow is directed toward the lower airway at end expiration.
G Indirect TGI causes the total PEEP to decrease because flow is directed toward the endotracheal tube and ventilator tubing, causing a Venturi effect and reducing PEEP.
H Monitoring of airway pressures and tidal volumes (Vts) is difficult during TGI.
1. With continuous flow TGI it is impossible to measure Vt, plateau pressure, and PEEP level.
2. During expiratory TGI if the TGI flow is coordinated with the ventilator, plateau pressure and PEEP can be measured by flow interruption.
3. Actual Vt in volume ventilation delivered during continuous flow TGI can be estimated by subtracting the TGI volume (flow × inspiratory time) from the total exhaled volume.
4. During expiratory TGI the inspiratory Vt can be easily measured.
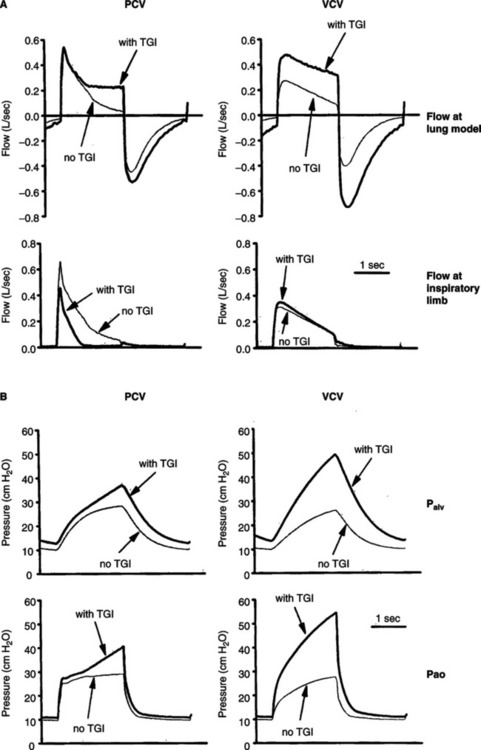
A During continuous TGI, Vt and airway pressure are increased during volume ventilation (Figure 44-4) unless the Vt is adjusted downward by a volume equal to the TGI flow added during inspiration.
1. If 6 L/min of continuous TGI flow is delivered, 100 ml volume of gas is delivered each second by the TGI system.
2. If inspiratory time is 1.0 second, decrease the delivered Vt by 100 ml to keep the delivered Vt and plateau pressure constant.
B In pressure control ventilation, continuous flow TGI will increase the Vt and plateau pressure if the ventilator-delivered flow decreases to zero before the end of the inspiratory phase (see Figure 44-4).
1. When the ventilator flow returns to zero, the ventilator cannot maintain a constant plateau pressure if a secondary flow of gas (TGI) is maintained.
2. Thus adding a continuous TGI flow has a high probability of increasing Vt and plateau pressure during pressure control ventilator.
C Pressure relief and flow relief valves can be added to the ventilator circuit to avoid pressure and volume increases.
D The use of expiratory phase-only TGI avoids the increase in volume and pressure during volume- and pressure-targeted ventilation.
E However, to measure plateau pressure and end expiratory pressure during TGI (continuous and intermittent) the TGI flow must be coordinated with the ventilator.
A TGI is useful during permissive hypercapnia for patients with acute respiratory distress syndrome (ARDS) with an existent metabolic acidosis or a marked respiratory acidosis.
B It is useful for ARDS patients in whom it is desirable to decrease plateau pressure without necessarily changing Paco2 (i.e., to maintain the same Paco2 in patients with increased intracranial pressure who also have ARDS) and to maintain a normal Paco2 without exposing the lungs to high peak alveolar pressure and Vts.