25 Tower technique of filler injection
Summary and Key Features
• Previous injection techniques for facial rejuvenation aimed at simply ‘filling’ lines and furrows
• Volume loss has become an important hallmark of the aging face, thanks to greater knowledge and understanding of how we age
• New techniques focus on providing structural support and are performed vertically, rather than horizontally
• The tower technique features 90° injections with gradually tapering product deposition as the needle is withdrawn
• In the vertical supraperiosteal depot technique, small aliquots of filling agent are deposited on the periosteum for maximum support
• Softer hyaluronic acid formulations are recommended for more superficial injection, whereas more robust and cohesive products may be chosen for deeper implantation
Anatomical considerations
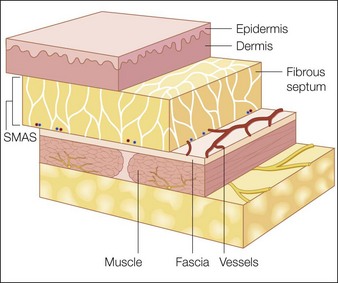
The facial skin and subcutaneous tissue (referred to as the soft tissue ‘flap’) comprise a dense, superficial formation of connective tissue that makes up the dermis and epidermis, a honeycomb web-like subdermal structure of connective tissue embedded in fat lobules, and muscle, which traverses the soft tissue flap (Fig. 25.1). Anatomical studies show that the immediate subdermal layer contains a large connective tissue network made up of small fat lobules with many septa, whereas the deeper subdermal layer features large fat lobules with only a few septa. Dynamic musculature presents in sometimes overlapping, multiple layers, and may even form entire complexes – as in the brow area where the frontalis, corrugator, and orbicularis muscles merge into one complex with the ability to move medially, proximally, and distally (F. Anderhuber, personal communication).
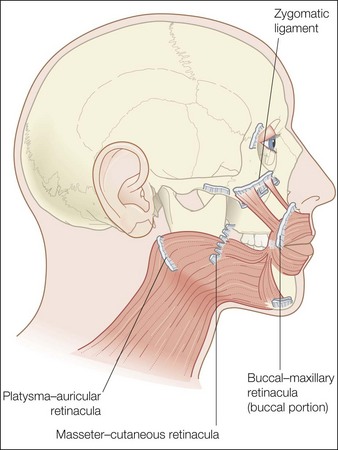
The analysis of the anatomical composition of the connective tissue is of greatest interest in volume augmentation. The soft tissue flap is attached to the underlying bony structure via connective tissue bands called retinacula or real retaining ligaments (Fig. 25.2), which show no or very limited elasticity. So-called false retaining ligaments – the most important of which include the nasolabial fold, the zygomatic ligament, and the maxillar–buccal ligament (Fig. 25.3) – add to the character of the flap surface. Although false retaining ligaments have no bony attachment, they act in a fence-like manner, compressing dynamic muscular activity and influencing the appearance, shape, and correction of the skin surface.
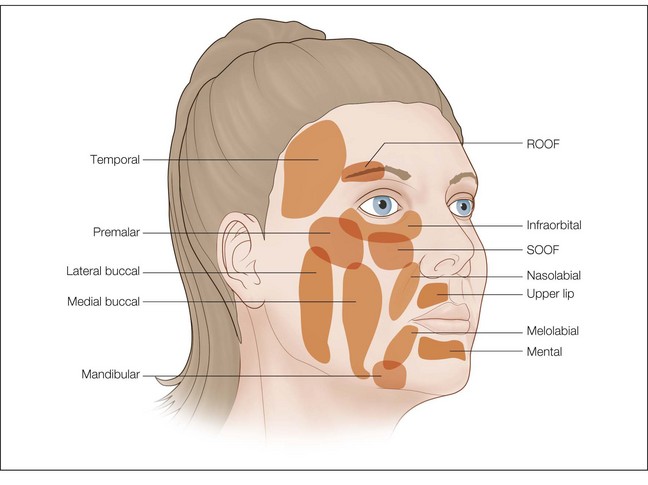
A brief description of the soft tissue anatomy of the human face is not complete without a discussion of the fat compartments, which are located around and below the eye, in the cheek, and in the perioral region (Fig. 25.4). The suborbicularis oculi fat (SOOF) and retro-orbicularis oculi fat (ROOF) pads are the dominant features of the periorbital region. As the most proximal entity in the mid-facial region with the least coverage of musculature structures, the SOOF pad plays a key role in the process of facial aging and has a direct impact on the clinical presence of the medial and lateral infraorbital hollow. Another important, shape relevant structure in the submalar area is induced by an indented groove from the medial orbital hollow to the lateral lower midface caused by the zygomatic ligament.
Biological characteristics of filler materials
New concepts in injection techniques
The tower technique
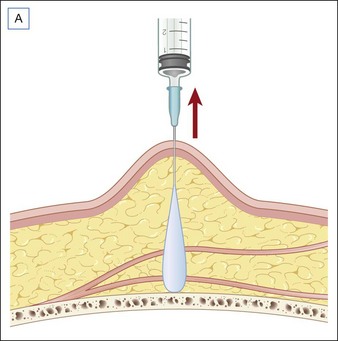
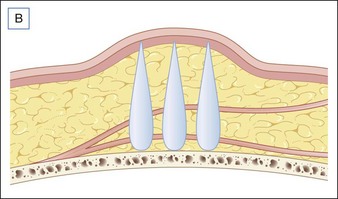
The tower technique – to be used with HA fillers alone – is a novel method of soft tissue augmentation that reintroduces structural support that has been lost through lipodystrophy and bone resorption. Horizontal layers of tissue (fascia, connective tissue, muscle, fat, and dermis) are attached to each other with a limited lateral flexibility. The tower technique deposits small amounts of HA in the tissue planes, like multiple washers between each layer (Fig. 25.5). By injecting filler vertically (90° to the base of the injection site) and gradually tapering product deposition as the needle is withdrawn, the clinician is able to build towers or columns of HA that serve as scaffolds for the overlying soft tissue structures, thus creating a deep base of support that extends through the entire subcutis.
The clinician gathers up the area to be injected between the thumb and second finger of the non-dominant hand. A 24–27-gauge, half-inch (1.25 cm) needle is inserted perpendicular to the skin at the desired depth based on the anatomical location (Table 25.1). After checking to ensure that the needle has not been placed in a vessel, the plunger is depressed and HA slowly injected as the needle is withdrawn vertically, using ever-decreasing amounts of product to create a pyramid-like support with a larger volume of HA deposited at the base and a gradual tapering of product deposition (Fig. 25.5A). The towers are usually placed in a line along the fold or groove, with each injection approximately 0.5–1 cm apart (Fig. 25.5B).
| Treatment area | Depth |
|---|---|
| Lateral brow | Periosteum |
| Infraorbital hollow | Periosteum |
| Cheek | Deep subcutis |
| Zygomatic ligament | Deep subcutis |
| Nasolabial folds | Deep subcutis |
| Inferior marionnette lines | Periosteum |
| Superior marionnette lines | Deep subcutis |
| Pre-jowl sulcus | Periosteum |
| Chin | Periosteum |
Vertical supraperiosteal depot technique
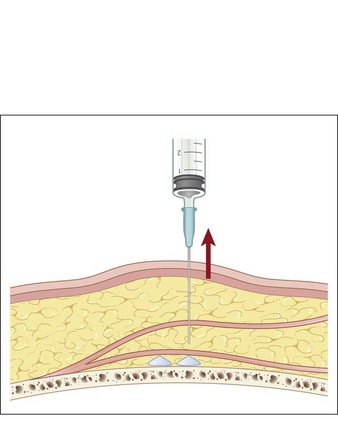
In comparison to the tower technique, the VSD technique features vertical injections directly on the bone, or more precisely – on the periosteum (Fig. 25.6). As in the tower technique, the clinician grasps the area to be injected between thumb and forefinger of the non-dominant hand for maximum penetration and pierces the skin at the thinnest entry point with a 24–27-gauge half-inch needle, using a 90° angle. After repositioning the cannula at the level of the bone and advancing slowly below the soft tissues, the augmenting agent can be deposited in aliquots of 0.1–0.3 mL at each injection point, depending on the depth of the defect, with a distance of up to 5 mm between injection sites.
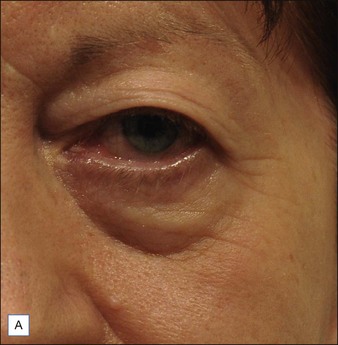
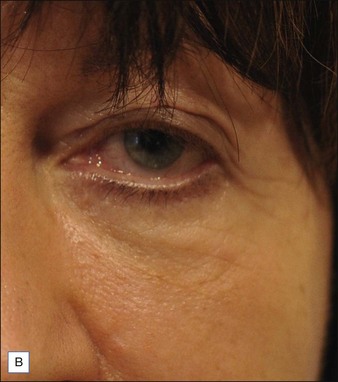
Because of the bony support, only a minimal amount of filler is needed in order to have a pronounced correction on the surface of the skin – as can be observed in the area of the orbital hollow over the medial part of the orbital rim (Fig. 25.7) or the zygomatic bone. Using small amounts of filling agent reduces the incidence of overcorrection and risk of associated side effects. Other areas that may benefit from the VSD technique include the upper orbital rim just below the brow, the dorsal area of the nose, the mandibular bone, and the entire forehead.
Injection tips and post-treatment recommendations
Treatment begins with 4 mL hyaluronic acid (HA) (Juvéderm® Voluma) injected into each side of the mid-face region using the vertical supraperiosteal depot injection technique, with another 2 mL injected using the tower technique into the nasolabial fold and marionette lines. Superficial rhytides in those areas are treated with a lighter HA product (Juvéderm® Ultra II). A total of 50 U botulinum toxin type A (BoNT-A; BOTOX Cosmetic®) is injected into the glabella, both eyebrows, the lateral canthal rhytides, mid-forehead, and the chin. Approximately 1 month later, the patient returns for an additional 1 mL of HA (Juvéderm® Voluma) into each side of the residual existing zygomatic ligaments using the tower technique. After another month, the treating clinician performs a bilateral upper eyelid blepharoplasty and removal of four nevi in both cheeks and right upper lip, under local anesthesia. The stitches are removed after 5 days. The following month, the patient receives another touch-up of 2 mL HA (Juvéderm® Voluma) in the cheeks, zygomatic ligaments, nasolabial folds, and marionette lines, along with treatment of superficial wrinkles using 1 mL of lower viscosity HA (Juvéderm® Ultra II). Botulinum toxin follows, with another 50 U in the glabella, eyebrows, lateral canthal rhytides, mid-forehead, and chin. Two injections of 0.3 mL hyaluronidase – spaced 1 month apart – are required in the very superficial aspect of each tear trough and zygomatic ligament. The patient receives a total of five treatment sessions in 5 months, with follow-up 1 year later (Fig. 25.8).
A 41-year-old female who considers herself ‘an early ager’ wants to improve her appearance and receives a total of four injectable treatments: three treatments of 50 U per session of BoNT-A (Xeomin®) in the area of the glabella, brows, lateral canthal rhytides, and the chin; and soft tissue augmentation of the cheek with 4 mL of high-viscosity hyaluronic acid (HA) (Belotero® Intense; vertical supraperiosteal depot technique), plus an additional 8 mL of lower viscosity HA (Belotero® Basic) to fill the nasolabial folds and marionette lines using the tower technique. To complete her rejuvenation, the patient undergoes an upper blepharoplasty under local anesthetic (Fig. 25.9).
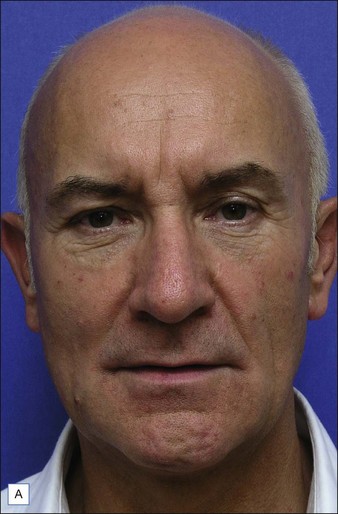
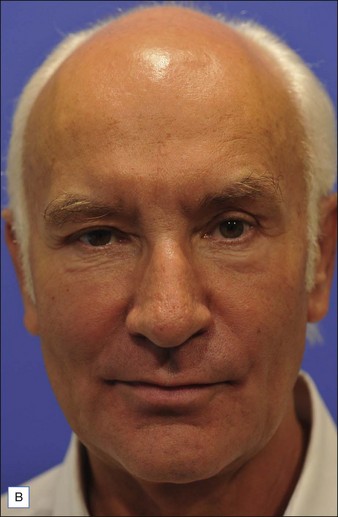
A 62-year-old male has the impression that his outward appearance looks too ‘hard’ and does not reflect his romantic emotionality. He requests a softer, more attractive look (Fig. 25.10). He receives a total of five treatment sessions performed at intervals of about 2 months. Invasive procedures include surgeries (an upper blepharoplasty, a subcision of the submental fold, and multiple nevi excisions), and ablative carbon dioxide laser resurfacing of his lower eyelids (Fraxel® re : pair). The tower and vertical supraperiosteal depot techniques are used to augment his face with different formulations of hyaluronic acid (Restylane®, Perlane®, and SubQ®) to a total of 14 mL in the cheeks, nasolabial folds, lower eyelid margins, and marionette lines. In addition BoNT-A (Xeomin®) is administered three times, 50 U per session, in the glabella, forehead, brows, lateral canthal rhytides, and chin.
Bartus CL, Sattler G, Hanke CW. The tower technique: A novel technique for the injection of hyaluronic acid fillers. Journal of Drugs in Dermatology. 2011;10:1277–1280.
Coleman SR, Grover R. The anatomy of the aging face: Volume loss and changes in 3 dimensional topography. Aesthetic Surgery Journal. 2006;26(1S):S4–S9.
Donofrio LM. Fat distribution: A morphologic study of the aging face. Dermatologic Surgery. 2000;26:1107–1112.
Rohrich RJ, Pessa JE. The retaining system of the face: Histologic evaluation of the septal boundaries of the subcutaneous fat compartments. Plastic and Reconstructive Surgery. 2008;121:1804–1809.
Sattler G, Sommer B. Bildatlas der ästhetischen Augmentationsverfahren mit Fillern. Dr Kolster: KVM; 2010.
Sattler G, Sommer B, Kolster BC. Filler in der ästhetischen Medizin (Patientenratgeber). Dr Kolster: KVM; 2010.
Shaw RB, Jr., Katzel EB, Koltz PF, et al. Aging of the facial skeleton: Aesthetic implications and rejuvenation strategies. Plastic and Reconstructive Surgery. 2011;127:374–383.
Wang F, Garza LA, Kang S, et al. In vivo stimulation of de novo collagen production caused by cross-linked hyaluronic acid dermal filler injections in photodamaged human skin. Archives of Dermatology. 2007;143(2):155–163.