TO THE PHYSICIAN TRAINEE
The long case is an art that needs mastering. Long case mastery will not only help candidates to pass the examination but will also equip the trainee with the skills and expertise to handle any complicated medical case. These skills are vital to the candidate’s future life as a physician. While preparing for the clinical examination, the candidate is expected to acquire as much expertise as possible within a very short time. Such intense learning will not happen at any other time in your career. Therefore, it is important to approach this time of preparation knowing what to do and how to go about doing it. The preparatory period should be well planned and executed, with utmost commitment to your goal. It is important to plan this preparation systematically, so that no aspect of clinical medicine is missed or omitted. It is also important to achieve your peak level of performance at the right time. Peaking too early can lead to exhaustion and a lacklustre performance by the time of the examination, and peaking too late may mean ‘missing the boat’.
An ideal way to start preparing is to fully understand what the preparation is for. It is therefore important to become familiar with the examination and what exactly will take place on the day. At the examination the candidate is usually given 1 hour to spend with the patient unobserved by the examiners or the ‘bulldog’ (the bulldog is a basic trainee registrar from the host hospital assigned to attend to the candidate on the day of the examination). During this period, a detailed history needs to be obtained, and a thorough physical examination performed, focusing particularly on the main system involved. The candidate is usually given a warning 10 minutes before the end of his or her time with the patient. Then another 10 minutes is given as preparation time before the candidate is introduced to the examiners. There are usually two examiners for each candidate on the long case, one being a member of the National Examining Panel (college representative or censor). Occasionally there may be a third member present, acting as an observer. This member of the examining team is usually a new examiner learning the examination process. The ‘grilling’ is carried out by the two main members of the examining team; later in the day, the ‘observer’ may swap seats with the college censor to actively participate in the ‘grilling’ process.
The examinee is expected to present a clear, sufficiently detailed and well-organised long case within 7–10 minutes and develop a comprehensive management plan. The candidate may be interrupted at any time during this period if further clarification is needed on any aspect of the case. The candidate usually spends 25 minutes with the examiners, and after the presentation there should be sufficient time for the examiners to assess the candidate’s knowledge. Of course, this is extremely valuable time for the candidate to demonstrate as much knowledge and clinical wisdom as they can. Ideally, if the candidate is confident with the case, they will be able to control the discussion, and this will convey an air of competence.
During the discussion, the candidate should mention the relevant investigations that they would perform. At this point, the examiners will present a radiological imaging study or a blood or serology test result and ask the candidate for an interpretation. Other investigation results—including electrocardiograms, lung function studies, nerve conduction studies, hormonal studies and nuclear medicine scans (but not pathological specimens)—may also be produced.
A practical tip
It is important to have a set approach to the long case, and to use this system repeatedly during practice cases until you have mastered the long case. Candidates should develop a format to address the history and the physical examination, and thereby avoid any ‘fatal’ mistakes or omissions.
A stack of cards can be very convenient for taking notes when with the patient. This also provides a hard surface to write on, as often there will not be a table available by the bedside. The best technique is to use the cards according to a prepared format. Mnemonics (see p 5) can be used to remember the format even in the stressful circumstances of the practice exams and the real exam. The way you organise the cards is also important. The long case can be divided into sections, and cards organised accordingly; this will make your presentation easier as well as neater. An average case may need about 20 cards, and these should be clearly numbered at the top right-hand corner.
• Card 1 should contain the patient’s name, age and the opening statement, which is a concise but sufficiently detailed introductory overview of the case.
• Card 2 should be for the presenting complaint and then associated conditions. Past history, medications, allergies, family history, occupational history and social history should be placed in that order.
The social history has to be very detailed; accordingly, this section comes as a subset of cards, with a separate mnemonic to help remember all aspects of the social history. Another advantage of using cards is that they can be held close to eye level with your head held high, thus facilitating constant eye contact with the examiners. It is important to maintain eye contact. (In fact, some senior examiners expect so much of it that one examiner advised his candidates to learn the long case by heart and stop using written records of the case at all.)
Taking a history
Establishing trust and confidence
The first 20 minutes of the hour with the patient should be spent on history taking. In the exam setting you should try to obtain as much help as you can from the patient by quickly explaining how important the exercise is to you. A strong bonding with the patient can be achieved from the outset by being very courteous and polite. Smile broadly and shake the patient’s hand warmly, using both hands. Generate genuine empathy with the patient and be considerate at all times. Try to create an atmosphere of trust and confidence. Establishing a good rapport will ensure that the patient opens up without any hesitation. It is easiest to begin by asking the patient about the medications he or she is currently taking. This may give you a comprehensive overview of the patient’s problems and save much valuable time. On some occasions at the real examination, the examiners leave the list of medications with the patient, with instructions to hand it to the candidate only if they request it.
Mnemonics
History and physical examination are the cornerstones of your clinical assessment of the patient. Your whole plan of investigation and management as well projections on the prognosis will be based on what is garnered during your clinical assessment and the case that is built upon this vital information. Therefore, it is essential that your history taking and physical examination be comprehensive, foolproof and watertight—you cannot afford to miss anything! One proven way of ensuring that you don’t miss anything is to have a ready-made, comprehensive and complete checklist consisting of everything you need to learn during history taking and physical examination. You will need to memorise this checklist and be able to recall it readily during the examination. Mnemonics are a very useful tool in this regard. This section of the chapter introduces some mnemonics that have been developed for this purpose. Or you might find it easier to develop your own set of mnemonics.
The following mnemonic for history taking is comprehensive and covers almost all aspects of the history:
P P M A F O S T
P Presenting complaint and the details thereof
P Past history, intercurrent illnesses and relevant details
For each disease mentioned in this section of the history, it is important to get the following details:
1. When, how and who made the diagnosis.
2. What treatment has been administered and whether there have been any complications or side effects associated with it. For each drug the patient is currently taking, mention the dosage and frequency. The candidate is expected to know the generic name of each drug and should be able to identify the generic names of almost all the commonly used drugs.
3. What the current level of disease activity is and how the patient is affected by it.
M Medication history
If all the patient’s current medications have been mentioned already in the previous section, it will be sufficient just to mention the list of medications again as a brief summary. Some examiners like to hear the list separately. Listing the medications may also provide the candidate with an opportunity to see whether there are any drugs with significant interactions.
A Allergies
F Family history
O Occupational history
S Social history
T Travel history
Relevant in cases with infectious diseases and exotic conditions.
Social history
Many a fatal mistake can be made by not addressing the social history adequately. Therefore it is important to have a separate mnemonic to probe into all the important aspects of the social history. The mnemonic for the social history is:
S E M I G — C H D P — N S — D I P — V A S P
(It is easier to remember this if you break it up into five segments as suggested here and review it many times a day.)
S Smoking history
E Ethanol/alcohol history
M Marriage
Marital status, previous marriages and, if single, reason for not marrying etc.
I Independence
Level of independence with activities of daily living. If the patient needs assistance, find out who the main care provider is and how well they are coping.
G GP
Relationship with the patient’s general practitioner, frequency of visits etc.
C Children
Number of children and other relevant details such as ages, gender, who they live with if the patient has a broken relationship with their partner.
H House/home
This should include details such as the number of steps needed to climb to enter or exit the house, the number of steps the patient has to climb inside the house, whether the patient has any disability, how she or he manages at home, and whether the house has been modified to accommodate the patient’s needs.
D Driving
Ask whether the patient drives and, if not, how they get around.
P Pets
Whether the patient keeps any pets. This may be important in situations of socially isolated patients and also in patients suspected of having zoonotic infections such as psittacosis.
N Nutrition
S Sleep
Ask questions to exclude obstructive sleep apnoea, such as whether the patient has been told by their bed partner that they snore, whether the patient feels refreshed in the morning on waking up, any early-morning headaches, early-morning diuresis, daytime somnolence (e.g. falling asleep at the steering wheel of a vehicle while driving). Also ask about insomnia—whether it is initial (difficulty falling asleep, associated with depressive situations) or terminal (waking up too early, associated with anxiety disorders)—or any complaints from the bed partner about distressing leg movements (restless legs syndrome).
D Depression
Ask whether the patient has ever been depressed and, if so, when, why and what treatment they have had. Ask whether the patient is currently depressed—here it may be necessary to enquire into the presence of any vegetative symptoms of depression, such as anorexia, anhedonia (lack of interest in pleasurable activities) or initial insomnia.
I Insight
Check the patient’s insight into their medical condition. This also includes enquiring into the patient’s knowledge about the disease, about living with it and its prognosis.
P Problem
Ask what the patient’s biggest problem currently is, as they perceive it. For example, a patient who is critically ill with infective exacerbation of end-stage emphysema may still be more worried about his disabled wife, who is alone at home, than about his own illness. In such a situation, as much importance should be given to organising adequate care for the wife as to the treatment of the patient’s medical condition.
V Visits
If the patient’s usual residence is far from the hospital, it is important to ask who visits the patient at the hospital and how often this happens.
A Associations
Ask whether the patient belongs to any relevant association or an organised body (e.g. Multiple Sclerosis Association, Blind Society), where they can obtain information and support.
S Support
Ask who provides the main social support base for the patient while in hospital and when discharged to the community.
P Pastime
Ask what the patient’s usual pastime is. This is important particularly in retired or disabled, homebound patients.
Physical examination
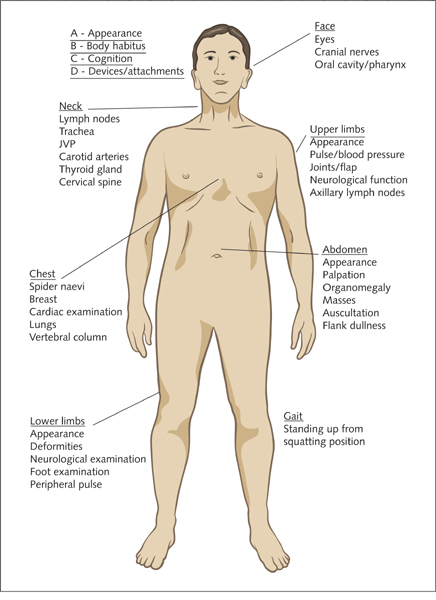
On completing the history, an adequately detailed physical examination should be performed, with the main emphasis on the system involved with the patient’s current presentation (Fig 1.1). It is wise to spend about 20 minutes on the physical examination. Elements of the physical examination include vital observations of the pulse rate, respiratory rate, temperature and blood pressure (postural pulse and blood pressure if indicated), and the systems-specific examination.
Initial components of the examination can easily be remembered as:
A B C D E F G (as easy as that!)
A Appearance
B Body mass index
An estimate would be sufficient, but some patients may be aware of their body weight and height.
C Cognition
It may be necessary to perform a Mini-Mental State Examination, particularly in such cases as suspected dementia, alcoholism, stroke and HIV infection.
D Devices and attachments
Do not forget to mention the intravenous catheters and the infusions running through them, an indwelling catheter, cardiac monitoring device attached to the patient, and any inhalants or continuous positive airway pressure devices lying on the table next to the patient.
The physical examination can be carried out by dividing it into different systems and examining each system separately. Some candidates may find this too time-consuming, particularly when there are significant time limitations. In such circumstances it may be wise to perform the examination from one end of the body to the other and then compartmentalise while writing up. The following is a simple model that is easy to remember.
E Entire body (head to toe)
Head:
Neck: lymph nodes, trachea, jugular venous pressure, carotid arteries, thyroid gland and the cervical spine
Upper limbs (distal to proximal):
Chest: cardiac examination, lungs, vertebral column, spider naevi, breast etc
Abdomen: appearance, palpation, organomegaly, masses, auscultation, flank dullness
Lower limbs: appearance, deformities, neurological examination (as per upper limb), foot examination, peripheral pulse
F Functionality
Assess limb movements and the ability to perform different functional tasks based on the clinical assessment thus far. This may involve assessment of muscle strength, neurological function and joint mobility. Check coordination if relevant.
G Gait
Study the patient’s gait and observe them standing up from a squatting position, to assess proximal weakness.
Remember to ask (the bulldog) for the results of the urine analysis and the per rectal examination, and for the temperature chart.
Presentation
In the presentation, the candidate can start off with the vital observations and go on to describe different systems, commencing with the main system involved. It is important to mention relevant negatives and the absence of signs that would be expected to have been present in the classic setting. If no abnormality was found in a certain system and the system is not involved in the presenting pathology, it may be adequate just to mention that the examination of the particular system was ‘unremarkable’. This may leave more time for the discussion.
If the history is very detailed and time is running short, it may be necessary to complete the latter part of the history while examining the patient. The mnemonics mentioned above may help in such a situation, and can be used as a checklist.
The last 20 minutes should be spent on clerical pursuits. It is important to arrange the presentation appropriately, to decide on which components to mention and what to withhold, and to prepare strong opening and closing statements. A comprehensive list of differential diagnoses should be thought of and relevant investigations should be decided on. When mentioning a particular test, it is vital to mention what is being looked for (e.g. ‘I would like to see the full blood count—looking for a polymorphonuclear leucocytosis’).
Discussion
Introduction
Much time and mental energy should go into preparing a suitable opening statement (Fig 1.2). This should be concise but detailed enough to give the examiners a broad overview of what is about to be presented. It should demonstrate the clinical maturity of the candidate, and a good opening statement can always put the examiners at ease and give vital points to the candidate. It is important to maintain full eye contact with the examiners during the opening statement and this can be achieved only by learning the statement by heart. A rambling and overly detailed opening statement will bore the examiners and give the impression that the candidate has not identified the crux of the case.
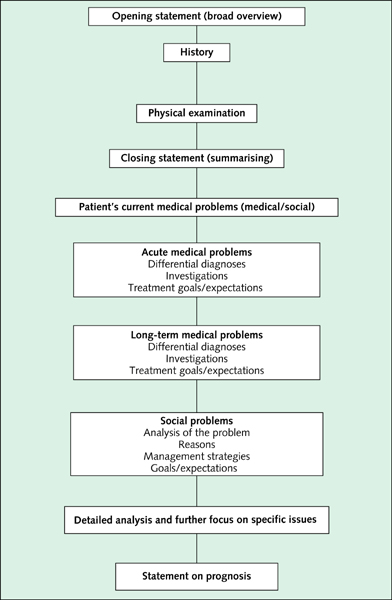
Figure 1.2 Structure of the discussion
Closing statement
The closing statement is a recapitulation of the essential aspects of the case. This must be concise but sufficiently detailed, like the opening statement. The difference between the opening and the closing statements is that the former is an anticipatory statement, and the latter a conclusive statement with indications of diagnostic possibilities and management options. After the closing statement comes the ‘main issues’ section.
The issue(s)
Most cases may have a single extremely important issue, which is the ‘main plot’, and identification of this issue is consistent with the expected level of maturity of the candidate at the examination. There may then be significant other issues that need to be identified. These can be discussed under two major headings: acute issues and long-term issues. Each of these can be further analysed under two subheadings: social issues and medical issues. Candidates should also mention how many problems they have identified before coming up with the list (e.g. ‘I have identified two acute medical problems and a social problem. There is also a long-term medical problem that needs addressing.’).
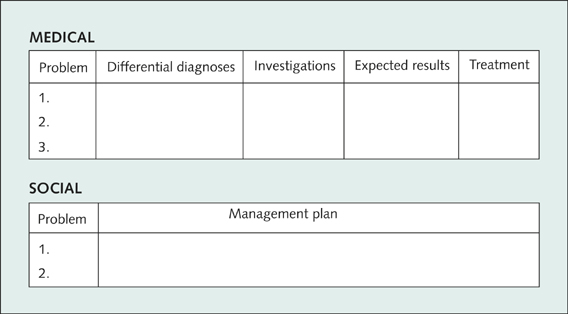
Management plan
After describing the issues that matter, a broad management plan should be introduced. The problems identified can be expanded under the medical and social subheadings according to the following compartmentalisation:
With regard to investigations, the candidate is expected to propose the most judicious investigation appropriate to the clinical setting, and to avoid giving long lists of non-specific investigations. When suggesting an invasive investigation, the candidate should be able to justify the risks involved in view of the benefits expected. The candidate should be aware of the costs involved with different investigations, and all decisions should be cost-effective in the general setting.
The candidate’s treatment plan should be comprehensive, and he or she is expected to make decisions with confidence and the competence of a general physician, with a
sound knowledge of all specialties of internal medicine. The candidate should be capable of defending the plan of management based on the most up-to-date evidence. It therefore pays to be thorough with the current treatment guidelines and pathways developed and introduced by various authorities (e.g. National Heart Foundation), reputed institutions and hospitals (e.g. Mayo Clinic). I cannot over-emphasise the importance of being familiar with the latest results of major randomised controlled multi-centre trials and other ground-breaking large-scale studies that define the practice of contemporary evidence-based medicine.
It is very important to emphasise a team approach to the management of issues in the broader sense, with the participation of the relevant specialists, the patient’s general practitioner (GP) and allied health workers, such as disease educators, social worker, occupational therapist, physiotherapist, speech pathologist and, of course, a diversional therapist as required. If the patient’s management problem is discharge planning and post-discharge care, it is important to demonstrate a sound knowledge of the community resources available for such patients. Here the family conference and liaison with the GP are important concepts.
Contemporary medicine attaches great significance to after-care and follow-up of patients. Candidates need to have a wide appreciation of the different chronic disease management programs and ambulatory care programs available for the ongoing care of patients in the community setting. The candidate is also required to provide plans on how to educate the patient, develop satisfactory insight into their condition and ensure good compliance with the management plan.
TO THE MEDICAL STUDENT
This book aims to provide an introduction for medical students entering and progressing through the clinical years of their training. Clinical integration involves putting together the subject matter learnt in the preclinical stages (also called basic science information) in the context of the patient. This programs your thinking to exercise clinical rationalising based on the background knowledge gained in the preclinical learning. Essentially it is an exercise for the student to start thinking like a doctor.
This book aims to aid the system of problem-based learning (PBL) and case-based learning (CBL) that has become the cornerstone of teaching in many medical schools. It provides the basic clinical information required to approach the more commonly encountered clinical challenges in internal medicine. Students are introduced to thinking in a systematic manner when approaching a patient. When you have become proficient in obtaining a general history and performing a good general physical examination (as discussed earlier in this chapter), you will then be ready to take on the more specialised clinical scenarios discussed in this book.
The physician plays the role of detective, gathering all the vital clues and evidence to build the case at hand. The clues are gathered during your history and physical examination. Therefore it is important that you have a clear idea of what you are looking for when taking the history and performing the physical examination. Once you have obtained a detailed history and have performed a thorough physical examination, you are then ready to put your thoughts together, to build the case. This involves coming up with a set of differential diagnoses based on the evidence you have gathered and your clinical reasoning. Then you should think of the investigations you need to order or refer the patient to, for the purpose of proving or excluding the various differential diagnoses. Based on the results of the investigations, you can reorganise your list of differential diagnoses and rank them from the most likely to the least likely. If you can identify a single diagnosis as the absolute based on the evidence at hand, it becomes your definitive diagnosis.
Now you are ready to come up with your plan of management. This needs to be comprehensive and should include direct therapeutics (pharmacological, interventional or surgical) and supportive measures (patient education, psychosocial aid, physiotherapy, rehabilitation etc). You should know what outcomes to expect from the different therapeutic decisions you make. Optimal monitoring of the patient’s response to treatment is very important.
Once the patient is treated for the acute condition, you should think of ongoing management once discharged from the care of the acute care provider. This involves building a long-term management plan in the setting of ambulatory care (outpatient follow-up), general practice and community care.
Remember: clinical medicine can only be learnt at the patient’s bedside! Only practice will make you a good clinician. Proactively participating in ward rounds, spending time with the resident staff, performing clinical duties under the supervision of junior medical staff, and participating in departmental clinical and teaching meetings are some activities that will help you immensely and facilitate your efforts to make the most of what is available for learning in the teaching hospital setting.
So, in summary, when approaching the patient (see box on p 15) you should be alert to the important clues with diagnostic, prognostic and management implications. Look for these initially during the clinical assessment (history and physical examination). Once you have completed your clinical assessment, you must develop a list of differential diagnoses. The next step in the clinical work-up is to decide on and perform the relevant investigations. The investigations are aimed at proving or excluding the differential diagnoses in order to narrow them down to a definitive diagnosis. Investigations need to be relevant and cost effective. (Medical students and inexperienced junior doctors are notorious for blindly ordering all the tests in the book.) Once you have arrived at the definitive diagnosis, the next step is to plan the management. Management has two main arms: treating the presenting complaints, and preventing recurrences or future clinical events.
Case vignettes and long case discussions
The clinical vignettes in the coming chapters are there to stimulate your thoughts. Once you have gained a good insight into the vignette you may find answers to some of your questions in the text that follows. Some questions may require further more specialised and detailed research. The text sets the stage and guides you through this learning exercise.
The case discussions in the third part of the book will give you an in-depth appreciation of how advanced clinical reasoning is done. Although this is aimed at medical registrars, these cases will give you a solid foundation upon which to build your clinical career.
Approach to the patient
1. Ensure that the patient is clinically and haemodynamically stable. If the patient is unstable (e.g. desaturating, hypotensive), you might first be required to provide acute care to stabilise the situation.
2. When you are sure the patient is stable, introduce yourself and establish the necessary confidence and trust. Build a rapport with the patient.
3. Obtain essential clues by observing the patient’s surroundings (immediate environment).
4. Obtain a detailed history, with particular focus on the presenting complaint. Ensure that the patient is well oriented and of satisfactory mental status. This will have a major bearing on the accuracy of the information you expect to gather. If the patient is not of sound mental state, the history may need to be obtained from a second party who is privy to the patient’s health status, such as the wife, husband, partner, parent, sibling or even the GP.
5. Perform a detailed physical examination with a particular focus on the system related to the presenting complaint.
6. Decide on a list of differential diagnoses.
7. Based on clinical reasoning, try to arrive at a definitive diagnosis.
8. Decide on the most relevant and useful investigations.
9. Order or perform the said investigations.
10. Decide on the plan of management, based on the clinical assessment as well as the results of the investigations.
11. Decide on the long-term management and means of preventing future clinical events.
12. Identify and address the patient’s psychological, social and occupational needs.
13. Provide patient education—a very important aspect of total medical care.