CHAPTER 150 Tinnitus and Hyperacusis
Tinnitus
Tinnitus is the perception of sound without an external source. Although 30 million Americans are estimated to have chronic tinnitus, for most it is not a problem sufficient for them to seek treatment. Tinnitus is a chronic sensation virtually all would prefer not to experience, but for most it is not disabling. Disturbing tinnitus occurs in 3% to 5% of individuals with tinnitus.1 Until more recently, treatments available for disturbing tinnitus were limited. Significant advances in auditory neuroscience have advanced the treatment of tinnitus beyond the traditional recommendation instructing the patient to “learn to live with it.” This chapter reviews current theories and mechanisms of idiopathic subjective tinnitus. It also outlines a clinical strategy for evaluating tinnitus and determining tinnitus subtypes, and reviews current management strategies for tinnitus.
Tinnitus can be classified as objective or subjective. Objective tinnitus can be detected by an observer using a stethoscope or ear canal microphone. Objective tinnitus arises from vascular or muscular sources. Objective tinnitus usually has a pulsatile quality. Table 150-1 lists the causes of pulsatile tinnitus. Many of these causes are uncommon and are not responsible for most instances of tinnitus. Because there are excellent reviews of treatments for objective tinnitus, this uncommon form is not addressed further.2
| Pulsatile |
In contrast to objective tinnitus, subjective tinnitus is not audible to an observer. This form is more common, with a 5-year incidence of 5.7%.3 Estimates of subjective tinnitus prevalence range from 8% to 30%, depending on the definition of tinnitus, tinnitus severity, the population sampled, and assessment methodology.3–5 In a large population-based study of participants 55 to 99 years old, combining detailed tinnitus questionnaires with audiologic assessment, 30% reported experiencing tinnitus, with prevalence related to audiometric threshold, but not age or gender.5 Mildly annoying tinnitus was reported in 50% of respondents, and extremely annoying tinnitus was reported in 16%. Tinnitus prevalence in individuals with normal hearing was 26.6% compared with 35.1% in individuals with hearing loss. An estimated 20% of individuals with profound hearing loss do not experience tinnitus.6 These data illustrate that chronic tinnitus is associated with, and may be triggered by, hearing loss, but they also indicate that hearing loss is not an invariable cause of tinnitus. The pathology necessary to initiate tinnitus may be quite subtle. The survey data also confirm that as a clinical problem tinnitus is more than the presentation of its sensory features.
Idiopathic Subjective Tinnitus
Subjective tinnitus can be subtyped based on etiology, the pattern of associated hearing loss, psychoacoustic features (simple versus complex), exacerbating factors, psychological comorbidities, and the presence of somatic modulators. Tinnitus subtype classification schemes can be useful in identifying forms of tinnitus that are responsive to specific targeted treatment programs. Table 150-2 lists some useful features for subtyping tinnitus.
Hearing Loss Subtypes
The two most common types of hearing loss associated with tinnitus are noise-induced hearing loss (NIHL) and presbycusis. NIHL is a significant and growing health problem. Although reduction of exposure to occupational noise has been effective in the last several decades, there has been a notable increase in the incidence of NIHL from recreational and leisure activity in children and adolescents, and military combat–related noise exposure in young adults.7–9 A Web-based survey of 9693 adolescents determined that 61% of respondents experienced hearing loss and temporary tinnitus after attending concerts.10 Acute transient tinnitus is nearly universal immediately after unprotected exposure to loud acoustic stimuli such as gunfire and amplified music. Tinnitus prevalence among Army personnel evaluated for hearing complaints after deployment was 30% compared with 1.5% in personnel not deployed.8
The prevalence of chronic tinnitus associated with NIHL is 50% to 70%.11 Subjectively, the sensory aspects of acute and chronic tinnitus can be very similar. Chronic tinnitus occurs in a delayed time course for a significant portion of individuals with a history of exposure to damaging sounds. It is unknown if the pathology of transient acoustic trauma–induced tinnitus is the same as the pathology responsible for chronic tinnitus associated with permanent noise-induced threshold shifts. Chronic tinnitus induced by acoustic trauma occurs at a younger age than tinnitus associated with other types of hearing loss. Consequently, acoustic trauma–induced tinnitus is experienced for a longer portion of the life span than other forms of tinnitus.
NIHL and associated tinnitus are preventable. In addition to obvious proactive methods, such as wearing ear protective hardware, intervention in the periexposure period may prove useful in preventing the onset or progression of NIHL, and possibly the incidence of tinnitus. Intense sound exposure triggers a reduction of blood flow and a cascade of metabolic events in the cochlea, with formation of reactive oxygen and nitrogen species that damage cellular lipids, proteins, and DNA, culminating in increased cell death.12 Interventions targeting these molecular mechanisms of NIHL include antioxidant therapy such as vitamin E, salicylate, and N-acetylcysteine.13 Ginkgo biloba extract contains multiple compounds with vasotropic, potential neuroprotective, and antioxidant effects. Although uncontrolled trials and anecdotal reports have suggested the efficacy of ginkgo, a more recent review failed to show efficacy in treating tinnitus.14
Serum magnesium levels have been correlated with NIHL in animals.15 Controlled studies in humans have shown the prophylactic efficacy of oral magnesium in preventing temporary and permanent NIHL.16,17 It is unknown, however, if these interventions are also effective in decreasing the risk of immediate or delayed onset of tinnitus after traumatic injury.
Presbycusis is sensorineural hearing loss related to aging. Most cases of presbycusis cannot be strictly and solely attributed to aging, but rather involve some combination of cochlear injury from additional sources, such as cumulative noise injury, metabolic or vascular dysfunction, and genetic predisposition. Elderly patients with diabetes have significantly higher pure-tone thresholds, lower otoacoustic emission amplitude, and lower speech recognition in noise18 than age-matched individuals without diabetes.19 Interactions between age and other factors affecting the cochlea and auditory pathway make identification of a single mechanism for presbycusis-associated tinnitus and an effectively targeted intervention a challenge.
Somatic Tinnitus Subtype
Somatic tinnitus is a unique form of tinnitus in which the loudness, laterality, or tonality of the tinnitus can by modulated by somatic stimuli. This form of tinnitus was originally observed in a small group of patients after surgical removal of large vestibular schwannomas.20,21 Postoperatively, these patients had the ability to modulate their chronic tinnitus by exaggerated eye movements, leg motion, or gentle cutaneous stimulation of the hands or face.22,23 The presumed mechanism of action for this unusual form of tinnitus is neural sprouting or aberrant reinnervation after auditory deafferentation. Subsequent to these observations, however, a more general form of somatosensory modulation has been found in patients with idiopathic tinnitus. In these cases, tinnitus is modulated by maneuvers or stimulation of the head and neck region. It has been reported that forceful isometric contraction of the head and neck muscles can modify the loudness and pitch of tinnitus in 65% to 80% of patients with mild, idiopathic tinnitus.24–26 Tinnitus can be induced by strong contractions of muscles in the jaw, head, or neck in 58% of subjects without a history of tinnitus.25
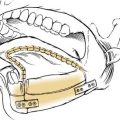
The association between tinnitus and somatic pathology of the head and neck is underscored by the reported higher incidence of tinnitus in individuals with temporomandibular joint dysfunction and normal audiometric thresholds compared with controls.27 One third of patients with symptoms of temporomandibular joint dysfunction reported modulation of tinnitus with jaw movement or pressure applied to the temporomandibular joint.28 When tinnitus occurs in association with disorders of the head and neck, such as temporomandibular joint dysfunction, unilateral facial pain, otalgia, and occipital or temporal headache, successful tinnitus alleviation may be possible using interventions targeting the somatic dysfunction.
Animal research has established that multimodal and in particular somatic inputs to the auditory pathway are evident from auditory brainstem to cortex.29–33 These inputs allow integration of information from vision, head position, and internal sound (e.g., vocalization) to be used in important functions, such as sound localization and auditory selective attention. It has been hypothesized that aberrations in these multimodal connections can either trigger tinnitus or modulate existing tinnitus. Reduction of normal afferent input to the auditory brainstem (e.g., cochlear nuclei) may trigger inappropriate compensatory up-regulation of somatosensory inputs to these regions. Stimulus-driven or spontaneous activity within the nonauditory somatic pathways may be perceived as an audible “sound.”33
Recognition of somatic tinnitus is important because it may be amenable to targeted intervention. Levine and colleagues34 systematically reviewed the efficacy of treatments targeting somatosensory systems. They defined somatic tinnitus syndrome as tinnitus that is (1) perceived in the ear and (2) ipsilateral to the somatic trigger and (3) not associated with any new hearing complaints. Tinnitus that is strongly lateralized to one ear in the presence of symmetric hearing (including symmetric hearing loss) would theoretically have a somatic etiologic component by the definition of Levine and colleagues.34 The review by these authors presents evidence that somatic tinnitus is often responsive to acupuncture, electric stimulation of the scalp and auricle, trigger point treatment, and treatment of temporomandibular joint dysfunction.34
Typewriter Tinnitus Subtype
Typewriter tinnitus is defined, as its name implies, by a characteristic sensation. The tinnitus has a staccato quality, similar to a typewriter tapping, popcorn popping, or Morse code signal. Its presence is intermittent and chronic. It may be confused with tinnitus arising from a muscular source, such as spasm of the tensor tympani or stapedius muscle, or palatal myoclonus. That typewriter tinnitus is a condition distinct from these somatic sources is supported by a case history of a patient with typewriter tinnitus that failed to respond to multiple treatments, including tensor tympani and stapedius resection. The patient was successfully treated, however, with carbamazepine (Tegretol). This case illustrates the importance of accurate recognition and diagnosis of typewriter tinnitus.35 A small case series reporting successful treatment with carbamazepine suggested that typewriter tinnitus may be caused by vascular compression of the auditory nerve ipsilateral to the tinnitus.36
Tinnitus Treatment Strategies
Auditory Deprivation and Neural Plasticity
A related phenomenon that illustrates the concept and treatment of deafferentation-induced cortical plasticity is phantom limb pain.37 The phantom limb syndrome is the continued sensation of the presence of an absent limb, in a distorted or painful manner, after amputation. Amputation of a limb is an extreme form of deafferentation. The parallels between tinnitus and phantom limb pain, in terms of onset rate, persistence, and affected ages, are striking. Greater than 90% of amputees experience a vivid limb phantom immediately after amputation.37 Phantoms are more likely to occur in adults than in children.38 In many cases, the phantom sensation fades after days or weeks, but it persists chronically for decades in 30% of patients.37
It is well known that the adult and the immature brain can undergo plastic change. Neural plasticity is the ability of a neuron or neural network to change its function, organization, and connectivity through long-term alterations in synaptic efficiency.39 Neurons can significantly alter their response to inputs, and receptive field sizes change, as a consequence of either decreased or increased input and training procedures.40 The changes can be extensive. Magnetoencephalographic studies have shown that stimulation of intact body areas distant from the amputation site is perceived, with corresponding central neural activity, at the cortical site of the amputated limb.41 Similar changes of auditory cortical representation may underlie tinnitus.42 Primary auditory cortex steady-state evoked magnetic fields were enhanced in tinnitus patients compared with controls, and the degree of enhancement correlated with the perceived intensity and intrusiveness of the tinnitus.43 Functional imaging studies in humans have suggested that expanded representation of frequency regions in the auditory cortex may underpin tinnitus.44–47
Animal models have been important in studying the deafferentation-loss-of-inhibition hypothesis of tinnitus, and have been used to evaluate sound therapy for reversal of pathologic neural plasticity. A key study by Norena and Eggermont48 illustrates the effect of noise trauma and therapeutic sound stimulation on receptive fields of primary and secondary auditory cortex. Cats exposed to a traumatizing noise were evaluated for changes in the location and responsiveness of auditory cortex neurons to acoustic stimuli. The frequency tuning of cortical neurons was altered after the trauma, distorting the overall representation of sound and over-representing frequencies surrounding the exposure sound. A second cohort of cats, exposed to the same traumatizing sound, was subsequently reared in an enriched acoustic environment for several weeks before mapping the auditory cortex. The enriched environment was spectrally composed to compensate for the anticipated frequency distortions induced by hearing loss.
Using Sound to Decrease Loudness and Annoyance of Tinnitus
Ambient Stimulation
The simplest method of increasing afferent input to reverse putative central reorganization and tinnitus is environmental sound enrichment. Use of supplemental environmental sound to treat tinnitus has been recommended for more than 50 years.49 Enrichment can be achieved using background music, relaxation tapes or CDs, tabletop nature sound machines, or waterfalls or fountains. Patients are typically instructed to use a source of constant background sound to decrease attention to their tinnitus. Sound enrichment is not intended to mask the tinnitus in the conventional sense of completely eliminating the tinnitus percept (discussed subsequently). Rather, by elevating the level of ambient sound using a constant, spectrally rich stimulus, the tinnitus sensation becomes less noticeable.
Hearing loss is present in more than 90% of patients with tinnitus. Conversely, epidemiologic studies have reported tinnitus prevalence of 50% in hearing-impaired patients.50 Effective use of sound stimulation for managing tinnitus in hearing-impaired patients can be achieved only with appropriate amplification. Typically, amplification is achieved with hearing aids. Even without supplemental sound, the therapeutic effect of hearing aids for tinnitus patients is well documented.51,52 Hearing aids reduce the awareness of tinnitus through amplification of ambient sound and reduce the perception that tinnitus masks hearing and impedes communication.
Surr and coworkers53 reviewed the initial effect of hearing aid use on tinnitus in 124 patients. Approximately one half of patients reported that the hearing aid reduced (26%) or eliminated (29%) the tinnitus. Folmer and Carroll54 reviewed their clinical experience with 50 patients with mild to moderate sensorineural hearing loss fitted with hearing aids for tinnitus management. Patients were re-evaluated 6 to 48 months after initial fitting (mean 18 months), and 70% reported significant improvement in their tinnitus. Similar results were obtained in a larger study of 1440 patients fitted with hearing aids for unilateral or bilateral hearing loss.55 In this study, digital hearing aids provided significantly greater tinnitus relief than analog hearing aids. Of patients fitted with digital hearing aids for unilateral hearing loss, 65% reported greater than 50% improvement in tinnitus compared with 39% reporting a similar degree of improvement after fitting with an analog aid. An even greater therapeutic effect was obtained with bilateral digital hearing aids: 85% of patients reported greater than 50% improvement in tinnitus compared with 30% fitted with bilateral analog aids.
Programmable digital hearing aids can selectively amplify within the high-frequency range, a region where most tinnitus patients typically have some measurable threshold loss. Current-generation digital aids have significant output gain up to 10 kHz, which significantly benefits tinnitus patients with hearing loss in the high-frequency range. An open-fit, nonoccluding ear mold is crucial to minimize the occlusion effect, which can amplify the tinnitus percept.56
Personal Listening Devices
Tinnitus management can be implemented through the use of personal listening devices, such as flash-memory music players. Miniaturization, data storage, and digital software have greatly expanded the available tools that clinicians and patients can use to produce a customized sound library. Inexpensive online sources are also available for downloading digital sound specifically developed for tinnitus therapy (e.g., http://www.vectormediasoftware.com). Patients can build and use a small library of sounds, which may include music to their liking, nature sounds, and noise bands of different spectral composition. Important key features of any regimen of amplified sound therapy are (1) use of open-fit, nonoccluding ear level drivers, (2) long-term exposure to the sounds, (3) sound spectral composition that is reasonably broad, and (4) sound levels below that of the perceived tinnitus.
Appropriate patient education is crucial to successful treatment. Many treatment failures occur because patients erroneously expect complete elimination of tinnitus after a few days to weeks of treatment. Patients must be counseled about the typical slow time course of improvement, and must be encouraged to have realistic expectations about the benefits of sound therapy. Sound therapy can decrease the subjective loudness and significantly decrease the annoyance of tinnitus, but this may require weeks to months of daily application.57,58
Total Masking Therapy
Total masking therapy is the use of sound with spectral characteristics and sufficient volume to render the tinnitus inaudible. This form of sound therapy has likely been used for centuries, and derives from empirical experience that certain environmental sounds are efficient tinnitus maskers. The clinical use of total masking therapy has a long history.59 A formal masking therapy program was first proposed by Vernon and Schleuning.60 Patients are fitted with ear-level devices that generate sound. The devices can be adjusted to have outputs with different frequency spectra and levels. There is no codified scheme for selecting effective masker characteristics. The general fitting principle is to determine the minimum level of broadband noise that masks the tinnitus without interfering with communication. The fitting is empirical because there is a wide range of patient preference in the type and level of sound that masks the tinnitus and is not perceived as annoying.61,62 Two significant benefits likely attend the successful application of total masking therapy: (1) Patients have control over their tinnitus, and (2) patients experience immediate relief with complete elimination of tinnitus.63
Benefits from masking therapy have been shown in a large prospective controlled study of chronic significant tinnitus in U.S. veterans.64 Validated standardized tinnitus severity questionnaires were used to screen and enroll 123 subjects with clinically significant tinnitus. Subjects were quasirandomly assigned to either the total masking group or a tinnitus retraining therapy (TRT) group. Subjects in the total masking group received hearing aids, maskers, or combination instruments, and all received information counseling over an 18-month follow-up period. Subjects in the TRT group received standardized TRT treatment (see later). All subjects were evaluated for response to treatment at 6, 12, and 18 months. Subjects in both treatment groups showed improvement on multiple measures of tinnitus over the course of the study. Subjects in the total masking group who rated their tinnitus as a “moderate” problem had effect sizes between 0.27 and 0.48 compared with effect sizes for the TRT group of 0.77 and 1.26 at 18 months. Mean effect sizes in subjects with tinnitus rated as a “very big problem” were 0.64 in the total masking group and 1.08 in the TRT group. Although both therapies resulted in clinically significant improvement in tinnitus with medium (>0.5) to large (>0.8) effect sizes, optimal outcomes were obtained with long-term TRT treatment.
Acoustic Stimulation Combined with Education and Counseling
TRT combines sound therapy with a formalized program of directive counseling to achieve habituation to tinnitus.65 TRT is based on the assumption that tinnitus distress derives from activation of an emotional and an autonomic response to tinnitus.66 Within this theoretical framework, tinnitus emerges as a result of damage or dysfunction within the auditory pathway, and is detected at subcortical levels of the brain. The critical event that leads to clinically significant tinnitus is not its sensory features, but rather the perception and evaluation of the tinnitus-related neural activity that occurs in the auditory cortex, and subsequent cortical interaction with the limbic system, prefrontal cortex, and cortical association areas.65 According to Jastreboff and Hazell,65 tinnitus becomes clinically significant when a negative affective response to the tinnitus has been established.
Jastreboff and Hazell65 described directive counseling as a teaching session in which patients are instructed on the mechanisms of tinnitus generation. Directive counseling demystifies tinnitus for the patient, and attempts to eliminate anxiety and fear of tinnitus through education. Auditory enrichment is typically achieved through the use of broadband noise generators. Ear-level devices physically similar in design to maskers are used, but sound output is distinctly lower than that used in masking therapy where sound levels render the tinnitus inaudible. In TRT, the volume of noise is set at a partial masking level, which allows continued perception of the tinnitus. The concept is that habituation would normally occur to the noise, much as one habituates to the background sound of a running air conditioner. Because the external noise and the internal tinnitus are equivalent in loudness, or “mixed,” habituation generalizes to the tinnitus and its attendant emotional reactions.
Retrospective clinical trials evaluating the efficacy of TRT have generally been positive with a consensus that TRT reduces the annoyance and impact of tinnitus within a time frame of 12 to 18 months. Sheldrake and associates67 reported a retrospective review of clinical outcomes on 224 patients completing a course of TRT. Outcome measures were percentage of time of tinnitus awareness, tinnitus distress, and the number of life factors affected by tinnitus. A successful outcome was defined as either a 40% improvement in tinnitus annoyance and awareness or 40% improvement in annoyance or awareness plus an improvement or facilitation of one life factor. At 6 months, 70% of patients had a successful outcome, and this percentage increased to 84% by 18 months. The mean awareness of and distress related to tinnitus before therapy were 63% and 45%, whereas after 18 months of therapy these percentages were 15% and 5%.
Bartnik and colleagues68 retrospectively reviewed the 12-month outcomes of 108 clinic patients treated with TRT for chronic tinnitus. Significant improvement was defined as a minimum decrease of 20% in at least three of these parameters (impact on daily life, time aware of tinnitus, degree of annoyance, and tinnitus intensity). Significant improvement was reported for patients treated with counseling alone (79%), counseling combined with noise generators (73%), and counseling combined with hearing aids (88%).
Berry and coworkers69 reported the 6-month results of a nonrandomized, prospective analysis of 32 patients treated with TRT. Treatment outcomes included psychophysical measures of loudness discomfort levels; minimal masking levels; and a standardized, validated measure of tinnitus severity and disability (Tinnitus Handicap Inventory [THI]; see later). Average THI score (pretreatment total score 52) significantly improved after 6 months of therapy (post-treatment total score 24; P < .001). Nine patients with sound sensitivity (hyperacusis) before treatment had a significant (P < .05) increase in sound tolerance after therapy, indicated by a 14 dB HL improvement in loudness discomfort level.
Acoustic Desensitization Protocol
The acoustic desensitization protocol is a proprietary tinnitus treatment program (Neuromonics, Bethlehem, PA) that combines features of sound therapy; systematic desensitization; directive counseling; and supportive intervention for stress management, sleep disruption, and coping strategies. Systematic desensitization is a psychological technique originally developed for the treatment of phobias. Progressive gradual controlled exposure to the phobic stimulus within the context of a deeply relaxed state of mind results in a gradual desensitization of the phobic response to the stimulus.70 This technique has been adapted to the treatment of tinnitus, by targeting the individual’s tinnitus as the stimulus that provokes the phobic, or at least negative emotional, response.
A Neuromonics-sponsored outcome study of the acoustic desensitization protocol has shown positive effects.71 In the study, 35 patients with moderate to severe tinnitus received Neuromonics tinnitus treatment and were tested for subjective (distress, awareness) and objective (minimum masking levels, loudness discomfort levels) changes at four time points, including 1 year, after therapy. Within the first 6 months of treatment, 91% of participants reported an improvement in tinnitus distress, reflecting a mean improvement of 65% in the Tinnitus Reaction Questionnaire. The reported “percent of time aware of tinnitus” before therapy was 90%, which was significantly reduced to 30% after 12 months of therapy.
Cognitive-Behavioral Therapy for Tinnitus
Cognitive-behavioral therapy (CBT) is a well-established psychotherapy based on identification of maladaptive behaviors and their modification using therapist-mediated cognitive restructuring. The technique has been successfully applied to tinnitus for many years, and forms the basis of another type of habituation therapy for tinnitus.66 CBT for tinnitus is based on the concept that the normal response to meaningless stimuli is habituation, and tinnitus distress results from a failure to habituate. Jakes and associates72 summarized the causes of habituation failure to include emotional responses, orientation to stimuli, arousal, and unfavorable signal-to-noise ratio. When a normal subject is presented repeatedly with a meaningless stimulus, responses to the stimulus, such as orientation, attention, and cognitive processing, soon habituate (i.e., the responses drop out). When the same subject is presented repeatedly with a noxious stimulus (e.g., the cry of a baby), sensitization occurs (i.e., the response to the stimulus becomes more pronounced and may have an emotional component). CBT uses techniques of reassurance, relaxation training, and selective attention distraction to induce habituation to tinnitus. It may be, as suggested by some, that defusing the emotional component of tinnitus, with or without concomitant changes in tinnitus loudness, is sufficient for improving patient outlook and perception.72
A review of CBT as a tinnitus treatment by the Cochrane Collaboration evaluated six trials comprising 285 participants.73 The primary outcome measure was subjective tinnitus loudness, and the secondary outcome measures were improvement in symptoms of mood disturbance and quality-of-life evaluation. The pooled results for the five trials reporting subjective loudness before and after treatment showed no significant difference between treatment with CBT and either a waiting list control or an alternative treatment. There was also no significant treatment effect for the secondary outcome measures of depression and mood disturbance. There was a significant improvement, however, in the quality of life of CBT participants, as measured by a global decrease in tinnitus severity, with a standardized mean difference of 0.70 (95% CI 0.33 to 1.08). The reviewers conclude that CBT has a significant impact on the qualitative aspects of tinnitus and contributes positively to the management of tinnitus.
Nevertheless, controversy continues regarding the relative benefits of CBT and sound stimulation in promoting psychological and physiologic habituation in patients who have chronic tinnitus. Hiller and Haerkotter74 followed 124 outpatients with chronic tinnitus, randomly assigned to either CBT alone or CBT combined with sound stimulation using noise generators. Tinnitus-related distress and psychosocial functioning were significantly improved in both groups, with no additive benefit observed in the sound-stimulation group.
Transcranial Magnetic Stimulation
The more recently developed diagnostic and treatment technique of transcranial magnetic stimulation (TMS) has opened a novel avenue for investigating the causal and associational aspects of tinnitus-related cortical activity, and may provide an effective tinnitus therapy for some patients. TMS uses a brief intense current in a surface coil applied to the scalp to induce a magnetic field in the underlying brain. The magnetic pulse induces a temporary focal disruption of neural activity in a discrete area of cortex. This “virtual lesion” briefly, and reversibly, disrupts cortical activity and allows the investigator to determine if the cortical region of interest contributes to a specific behavior or perception.75 The effect of a single pulse-induced magnetic field is short-lived, on the order of milliseconds. Repetitive TMS over seconds to minutes causes neuronal depolarization within the superficial cortex. Low-frequency (<1 Hz) repetitive TMS decreases cortical excitability,76 whereas high-frequency (5 to 20 Hz) repetitive TMS increases cortical excitability.77 All repetitive TMS frequency parameters can induce long-term plastic changes in cortical function that reportedly outlast the stimulation period by hours to days.78
TMS can be combined with functional imaging techniques to locate regions of interest for TMS application, and to examine the effect of cortical stimulation on distant structures. The combined techniques of TMS and functional brain imaging may be useful for investigating cortical mechanisms of tinnitus, and may be of clinical value as a treatment for some forms of tinnitus. Enhanced cerebral blood flow in temporoparietal cortex was shown using positron emission tomography (PET) imaging in patients who could modulate their tinnitus with orofacial movement46 or eye position.45 The association between tinnitus loudness and temporoparietal cortical blood flow was also observed in studies using lidocaine as a tinnitus modulator.47,79,80 To date, there have been no studies correlating changes in regional cerebral blood flow and altered tinnitus sensation modulated by repetitive TMS, although combining these methods might be revealing.
The functional relevance of temporoparietal cortex activity to tinnitus was first suggested by studies examining the effect of repetitive TMS on auditory hallucinations. Three patients with schizophrenia and persistent auditory hallucinations were studied in a double-blind crossover design using low-frequency (1 Hz) repetitive TMS to the left temporoparietal cortex versus sham stimulation. All three subjects reported significant improvement in severity of hallucinations after active treatment compared with sham stimulation. Two subjects had near-complete cessation of hallucinations for 2 weeks after treatment.81 Meta-analysis of the effect of repetitive TMS on auditory hallucinations in schizophrenic patients has supported these early results, and shows a significant positive effect.82
Plewnia and coworkers83 showed short-term suppression of idiopathic subjective tinnitus after high-frequency (10 Hz) TMS stimulation of temporoparietal cortex. Fourteen adults with chronic tinnitus were stimulated at 12 cortical locations with 10 Hz repetitive TMS for 3 seconds, repeated five times, and at two control locations for sham stimulation. Eight of the 14 subjects reproducibly reported on more than one trial an immediate decrease in tinnitus loudness after repetitive TMS, ranging from slight decrease to complete suppression. Five subjects did not perceive a reproducible attenuation of tinnitus, and one subject reported transient increase in tinnitus loudness that persisted for 2 weeks. Post-hoc analysis showed that the strongest tinnitus attenuation was obtained with stimulation of left temporal and left temporoparietal cortex.
Long-term inhibition of cortical hyperactivity can be induced using low-frequency repetitive TMS.76,84 In a double-blind, crossover, placebo-controlled (sham stimulation) trial of low-frequency repetitive TMS, PET-guided neuronavigation was used to target hyperactive areas within the superior temporal gyrus of 14 patients with chronic tinnitus (tinnitus durations of 1 to 30 years). The left temporal lobe was targeted in 12 patients, and the right lobe was targeted in 2 patients. After 5 days of treatment (2000 stimuli/day) there was a 7-day nontreatment interval, followed by 5 days of sham treatment. A significant reduction in standardized tinnitus questionnaire score was observed after active treatment (P < .005), but not after sham stimulation (P = .336).85 At 6-month follow-up, five patients reported worse tinnitus, with a mean increase in tinnitus questionnaire score of 5, and eight patients had an average 12. 4 decrease in tinnitus questionnaire score. Three of the eight patients had a clinically significant reduction in score of 16 to 34 points. There was no correlation between initial tinnitus severity or tinnitus duration and the response to active treatment.
Plewnia and coworkers86 subsequently examined the immediate effect of neuronavigated low-frequency repetitive TMS and sham stimulation on tinnitus loudness in another eight subjects in a single-blind crossover trial. Tinnitus loudness was assessed using an 11-point visual analog scale, with −5 indicating suppression of tinnitus, 0 no change, and +5 indicating increased loudness. Areas shown to be correlated with the tinnitus percept on PET imaging were primarily in sensory association cortex, but not primary auditory cortex. These included the left middle and inferior temporal cortex, the right gyrus angularis, and the posterior cingulum. Two of the eight subjects showed a decrease in tinnitus loudness (−3 and −5) after active low-frequency repetitiveTMS, and no change after sham stimulation. Three subjects were nonresponders during active and sham stimulation, and the three remaining subjects reported moderate (−2) to significant (−5) reduction in tinnitus loudness after active stimulation and sham stimulation. The outcomes of these evaluations of TMS were very mixed.
If TMS is effective in reversing neurogenic pathology, its mechanism of action remains unclear. High-frequency repetitive TMS can result in long-lasting clinical improvement in cases of chronic neurogenic pain, suggesting that the therapeutic effect may not be related to a reduction in cortical excitability, but rather be through reversal of chronic maladaptive plastic changes.87 The long-term effect of different repetitive TMS stimulation rates delivered to the left temporoparietal cortex was assessed in 39 subjects with chronic tinnitus (duration 6 months to 25 years).88 Subjects were randomly assigned to one of four stimulation groups (1 Hz, 10 Hz, 25 Hz, or sham stimulation) and treated with five sessions over a 2-week period. All subjects in the active repetitive TMS groups reported significant improvement (P < .05) in tinnitus severity on the standardized THI questionnaire at 4 months after completing treatment compared with the sham treatment group. Tinnitus improvement occurred regardless of stimulation rate for active repetitive TMS. A greater proportion of subjects experienced an 80% or greater improvement in THI score after treatment with 10 Hz (29%) and 25 Hz (35%), however, than after 1 Hz (6%). As reported in other studies, there was a negative correlation between tinnitus duration and percent improvement 4 months after treatment.
Further work is needed in this area to understand the mechanisms of TMS and its efficacy in treating tinnitus. It is unknown if the tinnitus-associated hyperactivity in secondary auditory cortex normalizes after subjectively successful treatment with repetitive TMS. There currently is no consensus on the relationship of hemispheric dominance and metabolic hyperactivity to tinnitus. Some studies have shown left temporoparietal activity is associated with tinnitus,45,46 and others have shown right-sided dominance.47,80 Finally, there are conflicting results on the effect of tinnitus duration on responsiveness to TMS.
Electric Stimulation
Electric stimulation has been used to treat tinnitus since the advent of Volta’s battery in the early 19th century.89 Although anodal direct current has been used by multiple investigators to suppress tinnitus, practical use is limited by tissue damage induced by chronic stimulation with direct current.90 Nondestructive methods of delivering electric current required the development of improved noninvasive techniques, such as transcutaneous electric stimulation, and surgically implanted devices using alternating current, such as cochlear implants and cortical stimulators.
Transcutaneous Electric Stimulation
Initial systematic attempts to decrease tinnitus using transcutaneous electric stimulation used the Audimax Theraband, a device that delivers inaudible, transdermal electric current to the mastoid eminence. Lyttkens and colleagues91 showed complete tinnitus suppression in one of five patients treated with transcutaneous stimulation. In a larger double-blind crossover study, 20 patients were treated first using the active device followed by a placebo device in which the internal circuitry was deactivated. Four patients (20%) reported reduction with the placebo, whereas two patients (10%) reported tinnitus reduction with the active device. One of the responders was examined further with random trials of either active or placebo stimulation, and reported a median 70% tinnitus decrease during active stimulation and 16% decrease during placebo stimulation.92 A subsequent single-blind crossover study of 30 patients showed a similar proportion of patients responded to stimulation.93 Levine and coworkers34 reviewed the characteristics of tinnitus patients who respond to transcutaneous electric stimulation and concluded that the common finding present in all cases is tinnitus with features of somatic modulation.
Herraiz and associates94 prospectively studied the effect of transcutaneous electric nerve stimulation in 26 patients with tinnitus categorized as somatically modulated. Although the trial lacked a placebo control, a striking effect was obtained in this sample from a selected population, with tinnitus elimination in 23% and tinnitus improvement in 23%. Further analysis by tinnitus type showed that the group most responsive to transcutaneous electric nerve stimulation treatment had typewriter tinnitus, with 88% experiencing improved or eliminated tinnitus.
Cochlear Implants
Suppression of tinnitus as a secondary benefit of cochlear implantation was noted in the early days of cochlear implant development.95 Although there is a large variability in the methods of assessing and reporting tinnitus, most studies report a consistent and clinically significant beneficial effect of cochlear implantation on tinnitus suppression.96 A significant proportion of patients (38% to 85%) report either a decrease or complete suppression of tinnitus after intracochlear electrode insertion before initial stimulation.97 Although there have not been extensive studies, there does not seem to be a significant difference in effective tinnitus suppression with different device manufacturers. Cochlear stimulation has been reported to reduce tinnitus intensity perceived in the ear contralateral and ipsilateral to the implant.97 This is not paradoxical because the brainstem cochlear nuclei have contralateral connections, and bilateral elevation of spontaneous activity in the dorsal cochlear nucleus has been shown in animals with tinnitus induced by unilateral acoustic trauma.98
Pharmacologic Tinnitus Treatments
Written accounts indicate medical treatment of tinnitus dates back to the Egyptians (2660-2160 B.C.E.).99 An ear that was bewitched or humming would be infused with oil, frankincense, tree sap, herbs, and soil. Mesopotamian writings considered the psychological aspects of tinnitus, possibly the earliest recognition that stress and emotional factors are significant components of tinnitus dysfunction. These early attempts at treatment contained elements that presage modern views of tinnitus pathology.
The hypothesis that tinnitus emerges from increased central neural activity after loss of inhibition can be used to guide pharmacologic intervention. Animal models of tinnitus support the loss of inhibition and enhanced neural activity hypothesis.98,100,101 The loss-of-inhibition hypothesis provides a rational basis for numerous pharmacologic interventions, including lidocaine, carbamazepine, alprazolam, and gabapentin.
Despite the increase in targeted tinnitus drug trials, using a single agent to treat a heterogeneous large sample of subjects has been for the most part unsuccessful. Several reasons, not mutually exclusive, may account for this lack of success. Most tinnitus clinical trials randomly select and assign participants to treatment groups. There is emerging evidence, however, that tinnitus is a heterogeneous disorder with variable pathologic features.34,102,103 Testing drugs with a single mechanism of action is unlikely to succeed when using randomly determined heterogeneous sample groups. For the same reason, trials using small dose ranges may fail.
Studies that enroll subjects with a single tinnitus etiology may be more likely to identify successful treatments. A study that examined the effect of gabapentin on tinnitus in two specific patient subpopulations obtained positive results.104 The study was designed to test the hypothesis that acoustic trauma leads to a loss of inhibition in the auditory pathway mediated by the inhibitory neurotransmitter γ-aminobutyric acid (GABA). The hypothesis was advanced after an animal experiment that showed gabapentin, a GABA analogue, to be effective in reducing the loudness of tinnitus in rats.100 This study used a very wide dose range, and tested one group of patients with objective and historical evidence of traumatic sound exposure, and a second group without such evidence. Gabapentin was found to reduce tinnitus annoyance significantly in the trauma group at a daily dose level of 1800 to 2400 mg. In contrast, a subsequent clinical trial studying the effect of only a single dose in a randomly selected group of patients did not obtain a significant effect.105 The therapeutic effect was likely missed because only a single dose level was used, and the treatment group included various tinnitus etiologies. Drugs with a specific mechanism of action are unlikely to be effective in all subjects characterized by such heterogeneity. Stratified study designs with segregation of tinnitus types, etiology, and hearing characteristics should be more successful in identifying effective drug therapies.
The most extensively used drugs for tinnitus treatment are antidepressants. Attempting to treat tinnitus with antidepressants is sensible for two reasons. There is a well-recognized association between severe tinnitus and mood disorders. The pharmacologic mechanism of action of many antidepressants involves receptors and neurotransmitters that are located in the auditory pathway.106 Although GABA deficiency seems to contribute to tinnitus pathology,104,107–109 the role of other neurotransmitter systems in triggering or maintaining tinnitus is currently unknown. Serotonin is known to function as a modulator of sensory systems, learning, and memory. Along with acetylcholine, serotonin can affect behavioral conditioning and associated plastic changes in auditory cortex. Both neurotransmitters may be important in the distress associated with tinnitus.
Treatment with sertraline, a selective serotonin reuptake inhibitor, improved tinnitus loudness (P = .014) and severity (P = .024) in a group of tinnitus patients with an associated depressive or anxiety disorder.110 Despite this positive evidence, it is unclear whether selective serotonin reuptake inhibitor treatment improved tinnitus directly or indirectly through alleviation of mood disorder. A placebo-controlled trial of the selective serotonin reuptake inhibitor paroxetine in a group of subjects without coexisting mood or anxiety disorder did not produce improvement in any tinnitus measure over placebo.111
Clinical Evaluation of Tinnitus
Standardized Outcome Measures
The THI is a widely used self-assessment tool.112 It is a 25-item questionnaire that has good construct validity, strong internal consistency, and good test-retest reliability. The THI yields a total score and three subscale scores. The subscales encompass functional limitations in mental (e.g., difficulty concentrating), social, occupational and physical domains (e.g., difficulty sleeping); emotional responses to tinnitus (e.g., anger, depression, anxiety); and catastrophic reactions to tinnitus (e.g., desperation, loss of control, failure to cope). In addition to its good internal consistency and test-retest reliability, the THI has high convergent validity with the 27-item Tinnitus Handicap Questionnaire and the 52-item Tinnitus Questionnaire.113 The 95% confidence interval for the THI is 20 points, suggesting that a difference in scores of 20 points or greater represents a statistically and clinically significant change.112
Tinnitus Comorbidities
As previously mentioned, severe debilitating tinnitus is frequently associated with depression, anxiety, and other mood disorders.114–116 Comorbid emotional disturbance is not unique to tinnitus, and has been shown to accompany many chronic illnesses.117,118 It is well recognized that coexisting mood disorders hamper improvement and interfere with treatment of conditions such as chronic pain and tinnitus. Identifying and treating comorbid conditions in tinnitus patients is an important aspect of the clinical evaluation. Tools are available to screen for mood disorders in an outpatient setting (e.g., Beck Depression Inventory, Hamilton Anxiety Scale). An important therapeutic adjunct is teaching coping skills through behavior modification and cognitive therapy.119
Tinnitus and Insomnia
Patients commonly report that tinnitus interferes with their ability to fall asleep, and sleep disruption is a significant comorbid condition in adults and children.120,121 A robust correlation has been shown between the reported loudness and severity of tinnitus and degree of sleep disruption.122,123 A positive feedback loop may exist in which tinnitus leads to sleep deprivation, and the sleep deprivation exacerbates somatic complaints, tinnitus among them. Depression and anxiety exacerbated by sleep loss may significantly interact with and compound the cycle of tinnitus and poor quality sleep. Coping ability may also deteriorate as a result of sleep deprivation or lack of restorative sleep. Interventions that break this cycle by improving sleep have been shown to improve tinnitus.
Pharmacologic sleep aids such as melatonin can reduce tinnitus severity, particularly in patients with pronounced sleep difficulties.14,125 Bedside sound generators have also been shown to improve sleep quality significantly and lessen tinnitus distress. The bedside sounds most frequently chosen are often selected for their perceived positive emotional effect.126
Sleep difficulties include insufficient sleep, poor quality sleep, and nonrestorative sleep. Psychological and behavioral management of sleep disturbance is an effective treatment modality.127 McKenna and Daniel128 have outlined a treatment strategy that addresses tinnitus and insomnia as components adversely affected by anxiety.
Hyperacusis
There is no single, universally accepted definition of hyperacusis, and there is no consensus on the physiologic mechanisms that cause the condition. Hyperacusis has been defined as noise intolerance, annoyance caused by ordinary sounds, and abnormal discomfort for suprathreshold sound.129 These definitions distinguish hyperacusis, considered by many to be a central phenomenon, from recruitment. Recruitment is the rapid growth of perceived loudness with increasing stimulus level, and is observed in association with cochlear hearing loss and outer cell dysfunction. Hyperacusis frequently occurs in association with tinnitus, but can be present without tinnitus or any associated hearing loss. Hyperacusis can occur after the loss of the stapedial reflex in association with acute facial paralysis,130 in association with general conditions such as migraine attacks,131 in association with Lyme disease,132 as a result of benzodiazepine withdrawal,133 or as part of a syndrome.134 Patients with tinnitus and hyperacusis frequently have loudness discomfort levels that are lower than loudness discomfort levels of individuals with similar levels of sensorineural hearing loss, indicating that these phenomena are distinctly different from recruitment.135
Andersson and associates136 assessed the prevalence of hyperacusis in the general population in two surveys of the adult Swedish population. The point prevalence of hyperacusis was 5.9% (postal survey) and 7.7% (Internet survey). Participants reporting hearing impairment were excluded from the prevalence calculations, minimizing the inclusion of patients with cochlear damage and reduced dynamic range in the sample. Other reports of hyperacusis prevalence in the general population are 22%.137 The prevalence of hyperacusis within the tinnitus population is unknown. Estimates range from 40% to 80%, but no systematic survey has been conducted for accurate estimation.138,139 In the general population and the tinnitus population, the adopted operational definition of hyperacusis would determine its estimated prevalence.
Objective tests of loudness discomfort or sound intolerance in patients with hyperacusis have been adapted from procedures developed for assessing recruitment.140,141 There are several variations on the technique for measuring loudness discomfort levels, but no consensus or standardization has been established. In addition, issues of intersubject and intrasubject variability,142 test-retest reliability,143 operator dependency, and poor face validity for test stimuli all limit the utility of adapting measures of loudness intolerance to patients with hyperacusis.
There are very few validated, well-established self-report questionnaires that specifically target hyperacusis. Two questionnaires developed in France are available, but have not yet been validated in English translation. Dauman and Bouscau-Faure139 have developed a scale for assessing hyperacusis in patients with tinnitus: The Multiple-Activity Scale for Hyperacusis (MASH). MASH employs a structured interview for rating the annoyance induced by sound exposure from different physical and social activities. Dauman and Bouscau-Faure139 reported hyperacusis was present in 197 of 249 (79%) clinical patients screened with the instrument, with substantial to severe annoyance from hyperacusis present in 42%. There was no correlation between the severity of hyperacusis, as indicated by MASH, and audiometric threshold shift, indicating that hyperacusis is a phenomenon distinct from loudness recruitment. The Hyperacusis Questionnaire is a 14-item instrument, also developed in French, in which hyperacusis is assessed using a four-alternative Likert scale.144
The impact of hypersensitivity to sound can range from general avoidance of social situations such as concerts and restaurants to specific sound aversions (e.g., vacuum cleaners, traffic, clinking dishes, children playing). In extreme cases, patients with severe hypersensitivity become housebound in an effort to control acoustic exposure, wearing ear plugs and ear muffs for extended periods. In all cases of sound hypersensitivity, it is important to address the physiologic component of loudness discomfort and reduced dynamic range, and the psychological component of fear, anxiety, social withdrawal, and maladaptation that accompanies the condition. The cognitive influence on sound sensitivity has been shown by the high correlation of loudness tolerance with anxiety.99
The efficacy of sound therapy for treating hyperacusis has had mixed results. Dauman and Bouscau-Faure139 reported that TRT was more effective in improving hyperacusis (63%) than tinnitus (47%) in 32 patients evaluated at three time points after therapy. They reported that hyperacusis remains a problem for a significant proportion of patients treated with TRT. Gold and associates145 reported a retrospective study on the effect of TRT on selected patients with reduced sound tolerance. Hyperacusis was defined as average loudness discomfort levels for 1 kHz, 2 kHz, 4 kHz, and 8 kHz below 100 dB HL and patient reports of physical discomfort with exposure to sounds. Hearing thresholds were unchanged between initial measures and follow-up after 9 months of therapy; however, mean loudness discomfort levels were improved 12.48 dB, and the dynamic range was significantly increased by a mean 11.32 dB. A corresponding improvement in the number of activities avoided because of sound tolerance problems was noted as well.
Aydemir G, Tezer MS, Borman P, et al. Treatment of tinnitus with transcutaneous electrical nerve stimulation improves patients’ quality of life. J Laryngol Otol. 2006;120:442-445.
Bauer CA, Brozoski TJ. Effect of gabapentin on the sensation and impact of tinnitus. Laryngoscope. 2006;116:675-681.
Bauer CA, Brozoski TJ, Myers K. Primary afferent dendrite degeneration as a cause of tinnitus. J Neurosci Res. 2007;85:1489-1498.
Bauer CA, Brozoski TJ, Myers KS. Acoustic injury and TRPV1 expression in the cochlear spiral ganglion. Int Tinnitus J. 2007;13:21-28.
Davis PB, Paki B, Hanley PJ. Neuromonics tinnitus treatment: third clinical trial. Ear Hear. 2007;28:242-259.
Folmer RL, Griest SE. Tinnitus and insomnia. Am J Otolaryngol. 2000;21:287-293.
Hebert S, Carrier J. Sleep complaints in elderly tinnitus patients: a controlled study. Ear Hear. 2007;28:649-655.
Herraiz C, Toledano A, Diges I. Trans-electrical nerve stimulation (TENS) for somatic tinnitus. Prog Brain Res. 2007;166:389-553.
Jakes SC, Hallam RS, Rachman S, et al. The effects of reassurance, relaxation training and distraction on chronic tinnitus sufferers. Behav Res Ther. 1986;24:497-507.
Kirsch CA, Blanchard EB, Parnes SM. Psychological characteristics of individuals high and low in their ability to cope with tinnitus. Psychosom Med. 1989;51:209-217.
Levine RA. Typewriter tinnitus: a carbamazepine-responsive syndrome related to auditory nerve vascular compression. ORL J Otorhinolaryngol Relat Spec. 2006;68:43-46.
Lockwood AH, Salvi RJ, Coad ML, et al. The functional neuroanatomy of tinnitus: evidence for limbic system links and neural plasticity. Neurology. 1998;50:114-120.
Mardini MK. Ear-clicking “tinnitus” responding to carbamazepine. N Engl J Med. 1987;317:1542.
Martinez Devesa P, Waddell A, Perera R, et al. Cognitive behavioural therapy for tinnitus. Cochrane Database Syst Rev. 2007;(1)CD005233.
Norena AJ, Eggermont JJ. Enriched acoustic environment after noise trauma reduces hearing loss and prevents cortical map reorganization. J Neurosci. 2005;25:699-705.
Robinson SK, Viirre ES, Bailey KA, et al. Randomized placebo-controlled trial of a selective serotonin reuptake inhibitor in the treatment of nondepressed tinnitus subjects. Psychosom Med. 2005;67:981-988.
Rosenberg SI, Silverstein H, Rowan PT, et al. Effect of melatonin on tinnitus. Laryngoscope. 1998;108:305-310.
Rubinstein B, Axelsson A, Carlsson GE. Prevalence of signs and symptoms of craniomandibular disorders in tinnitus patients. J Craniomandib Disord. 1990;4:186-192.
Shulman A, Goldstein B. Pharmacotherapy for severe, disabling, subjective, idiopathic tinnitus: 2005-2006. Int Tinnitus J. 2006;12:161-171.
Trotter MI, Donaldson I. Hearing aids and tinnitus therapy: a 25 year experience. J Laryngol Otol. 2008;122:1052-1056.
Tyler, Tyler RS, editor. Tinnitus Treatment: Clinical Protocols. New York: Thieme Medical Publishers, 2006.
Zoger S, Svedlund J, Holgers KM. The effects of sertraline on severe tinnitus suffering—a randomized, double-blind, placebo-controlled study. J Clin Psychopharmacol. 2006;26:32-39.
1. Cooper JCJr. Health and Nutrition Examination Survey of 1971-1975, part II: tinnitus, subjective hearing loss, and well-being. J Am Acad Audiol. 1994;5:37.
2. Sismanis A. Tinnitus: Advances in Evaluation and Management. Philadelphia: Saunders; 2003.
3. Nondahl DM, Cruickshanks KJ, Wiley TL, et al. Prevalence and 5-year incidence of tinnitus among older adults: the epidemiology of hearing loss study. J Am Acad Audiol. 2002;13:323.
4. Evered D, Lawrenson G. Tinnitus. Summit, NJ: Ciba Pharmaceutical Co. Medical Education Administration; 1981.
5. Sindhusake D, Golding M, Newall P, et al. Risk factors for tinnitus in a population of older adults: the Blue Mountains Hearing Study. Ear Hear. 2003;24:501.
6. Levine RA. Somatic (craniocervical) tinnitus and the dorsal cochlear nucleus hypothesis. Am J Otolaryngol. 1999;20:351.
7. Barney R, Bohnker BK. Hearing thresholds for U.S. Marines: comparison of aviation, combat arms, and other personnel. Aviat Space Environ Med. 2006;77:53.
8. Helfer TM, Jordan NN, Lee RB. Postdeployment hearing loss in U.S. Army soldiers seen at audiology clinics from April 1, 2003, through March 31, 2004. Am J Audiol. 2005;14:161.
9. Niskar AS, Kieszak SM, Holmes AE, et al. Estimated prevalence of noise-induced hearing threshold shifts among children 6 to 19 years of age: the Third National Health and Nutrition Examination Survey, 1988-1994, United States. Pediatrics. 2001;108:40.
10. Chung JH, Des Roches CM, Meunier J, et al. Evaluation of noise-induced hearing loss in young people using a web-based survey technique. Pediatrics. 2005;115:861.
11. Axelsson A, Sandh A. Tinnitus in noise-induced hearing loss. Br J Audiol. 1985;19:271.
12. Le Prell CG, Hughes LF, Miller JM. Free radical scavengers vitamins A, C, and E plus magnesium reduce noise trauma. Free Radic Biol Med. 2007;42:1454.
13. Kopke R, Bielefeld E, Liu J, et al. Prevention of impulse noise-induced hearing loss with antioxidants. Acta Otolaryngol. 2005;125:235.
14. Hilton M, Pinder D. The Epley (canalith repositioning) manoeuvre for benign paroxysmal positional vertigo. Cochrane Database Syst Rev. 2004;(2):CD003162.
15. Gunther T, Ising H, Joachims Z. Biochemical mechanisms affecting susceptibility to noise-induced hearing loss. Am J Otol. 1989;10:36.
16. Attias J, Sapir S, Bresloff I, et al. Reduction in noise-induced temporary threshold shift in humans following oral magnesium intake. Clin Otolaryngol Allied Sci. 2004;29:635.
17. Attias J, Weisz G, Almog S, et al. Oral magnesium intake reduces permanent hearing loss induced by noise exposure. Am J Otolaryngol. 1994;15:26.
18. Bainbridge KE, Cowie CC, Rust KF, et al. Mitigating case mix factors by choice of glycemic control performance measure threshold. Diabetes Care. 2008;31:1754.
19. Frisina ST, Mapes F, Kim S, et al. Characterization of hearing loss in aged type II diabetics. Hear Res. 2006;211:103.
20. Wall M, Rosenberg M, Richardson D. Gaze-evoked tinnitus. Neurology. 1987;37:1034.
21. Whittaker CK. Tinnitus and eye movement. Am J Otol. 1982;4:188.
22. Cacace AT, Cousins JP, Parnes SM, et al. Cutaneous-evoked tinnitus, II: review of neuroanatomical, physiological and functional imaging studies. Audiol Neurootol. 1999;4:258.
23. Cacace AT, Cousins JP, Parnes SM, et al. Cutaneous-evoked tinnitus, I: phenomenology, psychophysics and functional imaging. Audiol Neurootol. 1999;4:247.
24. Abel MD, Levine RA. Muscle contractions and auditory perception in tinnitus patients and nonclinical subjects. Cranio. 2004;22:181.
25. Levine RA, Abel M, Cheng H. CNS somatosensory-auditory interactions elicit or modulate tinnitus. Exp Brain Res. 2003;153:643.
26. Sanchez TG, Guerra GC, Lorenzi MC, et al. The influence of voluntary muscle contractions upon the onset and modulation of tinnitus. Audiol Neurootol. 2002;7:370.
27. Chole RA, Parker WS. Tinnitus and vertigo in patients with temporomandibular disorder. Arch Otolaryngol Head Neck Surg. 1992;118:817.
28. Rubinstein B, Axelsson A, Carlsson GE. Prevalence of signs and symptoms of craniomandibular disorders in tinnitus patients. J Craniomandib Disord. 1990;4:186.
29. Itoh K, Kamiya H, Mitani A, et al. Direct projections from the dorsal column nuclei and the spinal trigeminal nuclei to the cochlear nuclei in the cat. Brain Res. 1987;400:145.
30. Ryugo DK, Cahill HB, Rose LS, et al. Separate forms of pathology in the cochlea of congenitally deaf white cats. Hear Res. 2003;181:73.
31. Shore SE. Multisensory integration in the dorsal cochlear nucleus: unit responses to acoustic and trigeminal ganglion stimulation. Eur J Neurosci. 2005;21:3334.
32. Shore SE, Sumner CJ, Bledsoe SC, et al. Effects of contralateral sound stimulation on unit activity of ventral cochlear nucleus neurons. Exp Brain Res. 2003;153:427.
33. Shore SE, Zhou J. Somatosensory influence on the cochlear nucleus and beyond. Hear Res. 2006;90:216.
34. Levine RA, Nam EC, Oron Y, et al. Evidence for a tinnitus subgroup responsive to somatosensory based treatment modalities. Prog Brain Res. 2007;166:195.
35. Mardini MK. Ear-clicking “tinnitus” responding to carbamazepine. N Engl J Med. 1987;317:1542.
36. Levine RA. Typewriter tinnitus: a carbamazepine-responsive syndrome related to auditory nerve vascular compression. ORL J Otorhinolaryngol Relat Spec. 2006;68:43.
37. Ramachandran VS, Hirstein W. The perception of phantom limbs. The D. O. Hebb lecture. Brain. 1998;121(Pt 9):1603.
38. Simmel ML. Phantom experiences following amputation in childhood. J Neurol Neurosurg Psychiatry. 1962;25:69.
39. Moller AR. The role of neural plasticity in tinnitus. Prog Brain Res. 2007;166:37.
40. Merzenich MM, Nelson RJ, Stryker MP, et al. Somatosensory cortical map changes following digit amputation in adult monkeys. J Comp Neurol. 1984;224:591.
41. Yang TT, Gallen CC, Ramachandran VS, et al. Noninvasive detection of cerebral plasticity in adult human somatosensory cortex. Neuroreport. 1994;5:701.
42. Muhlnickel W, Elbert T, Taub E, et al. Reorganization of auditory cortex in tinnitus. Proc Natl Acad Sci U S A. 1998;95:10340.
43. Diesch E, Struve M, Rupp A, et al. Enhancement of steady-state auditory evoked magnetic fields in tinnitus. Eur J Neurosci. 2004;19:1093.
44. Arnold W, Bartenstein P, Oestreicher E, et al. Focal metabolic activation in the predominant left auditory cortex in patients suffering from tinnitus: a PET study with [18F]deoxyglucose. ORL J Otorhinolaryngol Relat Spec. 1996;58:195.
45. Giraud AL, Chery-Croze S, Fischer G, et al. A selective imaging of tinnitus. Neuroreport. 1999;10:1.
46. Lockwood AH, Salvi RJ, Coad ML, et al. The functional neuroanatomy of tinnitus: evidence for limbic system links and neural plasticity. Neurology. 1998;50:114.
47. Mirz F, Pedersen B, Ishizu K, et al. Positron emission tomography of cortical centers of tinnitus. Hear Res. 1999;134:133.
48. Norena AJ, Eggermont JJ. Enriched acoustic environment after noise trauma reduces hearing loss and prevents cortical map reorganization. J Neurosci. 2005;25:699.
49. Goodhill V. The management of tinnitus. Laryngoscope. 1950;60:442.
50. Davis AC, Lovell EA, Smith PA, et al. The contribution of social noise to tinnitus in young people—a preliminary report. Noise Health. 1998;1:40.
51. Bentler RA, Tyler RS. Tinnitus management. ASHA. 1987;29:27.
52. Satzman M, Ersner MS. The hearing aid in mixed deafness. Arch Otolaryngol. 1949;50:249.
53. Surr RK, Montgomery AA, Mueller HG. Effect of amplification on tinnitus among new hearing aid users. Ear Hear. 1985;6:71.
54. Folmer RL, Carroll JR. Long-term effectiveness of ear-level devices for tinnitus. Otolaryngol Head Neck Surg. 2006;134:132.
55. Trotter MI, Donaldson I. Hearing aids and tinnitus therapy: a 25-year experience. J Laryngol Otol. 2008;122:1052.
56. Del Bo L, Ambrosetti U. Hearing aids for the treatment of tinnitus. Prog Brain Res. 2007;166:341.
57. Al-Jassim AH. The use of the Walkman mini-stereo system in the management of tinnitus. J Laryngol Otol. 1987;101:663.
58. Pineda JA, Moore FR, Viirre E. Tinnitus treatment with customized sounds. Int Tinnitus J. 2008;14:17.
59. Jones IH, Knudson VO. Certain aspects of tinnitus, particularly treatment. Laryngoscope. 1928;38:597.
60. Vernon J, Schleuning A. Tinnitus: a new management. Laryngoscope. 1978;88:413.
61. Terry AM, Jones DM. Preference for potential tinnitus maskers: results from annoyance ratings. Br J Audiol. 1986;20:277.
62. Vernon JA, Meikle MB. Tinnitus masking: unresolved problems. Ciba Found Symp. 1981;85:239.
63. Tyler RS. Neurophysiological Psychological Models. New York: Thieme; 2006.
64. Henry JA, Schechter MA, Zaugg TL, et al. Clinical trial to compare tinnitus masking and tinnitus retraining therapy. Acta Otolaryngol Suppl. 2006;556:64.
65. Jastreboff PJ, Hazell JW. A neurophysiological approach to tinnitus: clinical implications. Br J Audiol. 1993;27:7.
66. Hallam R. Psychological Aspects of Tinnitus, Vol 3. Oxford: Pergamon. 1984.
67. Sheldrake JB, Hazell JWP, Graham RL. Results of tinnitus retraining therapy. In Sixth International Tinnitus Seminar, Cambridge, United Kingdom, 1999.
68. Bartnik G, Fabijanska A, Rogowski M. Effects of tinnitus retraining therapy (TRT) for patients with tinnitus and subjective hearing loss versus tinnitus only. Scand Audiol Suppl. 2001;52:206.
69. Berry JA, Gold SL, Frederick EA, et al. Patient-based outcomes in patients with primary tinnitus undergoing tinnitus retraining therapy. Arch Otolaryngol Head Neck Surg. 2002;128:1153.
70. Yulis S, Brahm G, Charnes G, et al. The extinction of phobic behavior as a function of attention shifts. Behav Res Ther. 1975;13:173.
71. Davis PB, Paki B, Hanley PJ. Neuromonics tinnitus treatment: third clinical trial. Ear Hear. 2007;28:242.
72. Jakes SC, Hallam RS, Rachman S, et al. The effects of reassurance, relaxation training and distraction on chronic tinnitus sufferers. Behav Res Ther. 1986;24:497.
73. Martinez Devesa P, Waddell A, Perera R, et al. Cognitive behavioural therapy for tinnitus. Cochrane Database Syst Rev. 2007;(1):CD005233.
74. Hiller W, Haerkotter C. Does sound stimulation have additive effects on cognitive-behavioral treatment of chronic tinnitus? Behav Res Ther. 2005;43:595.
75. Bestmann S, Ruff CC, Blakemore C, et al. Spatial attention changes excitability of human visual cortex to direct stimulation. Curr Biol. 2007;17:134.
76. Chen R, Cohen LG, Hallett M. Role of the ipsilateral motor cortex in voluntary movement. Can J Neurol Sci. 1997;24:284.
77. Pascual-Leone A, Valls-Sole J, Wassermann EM, et al. Responses to rapid-rate transcranial magnetic stimulation of the human motor cortex. Brain. 1994;117(Pt 4):847.
78. Wang H, Wang X, Scheich H. LTD and LTP induced by transcranial magnetic stimulation in auditory cortex. Neuroreport. 1996;7:521.
79. Andersson G, Lyttkens L, Hirvela C, et al. Regional cerebral blood flow during tinnitus: a PET case study with lidocaine and auditory stimulation. Acta Otolaryngol. 2000;120:967.
80. Reyes SA, Salvi RJ, Burkard RF, et al. Brain imaging of the effects of lidocaine on tinnitus. Hear Res. 2002;171:43.
81. Hoffman RE, Boutros NN, Berman RM, et al. Transcranial magnetic stimulation of left temporoparietal cortex in three patients reporting hallucinated “voices.”. Biol Psychiatry. 1999;46:130.
82. Aleman A, Sommer IE, Kahn RS. Efficacy of slow repetitive transcranial magnetic stimulation in the treatment of resistant auditory hallucinations in schizophrenia: a meta-analysis. J Clin Psychiatry. 2007;68:416.
83. Plewnia C, Bartels M, Gerloff C. Transient suppression of tinnitus by transcranial magnetic stimulation. Ann Neurol. 2003;53:263.
84. Lee L, Siebner HR, Rowe JB, et al. Acute remapping within the motor system induced by low-frequency repetitive transcranial magnetic stimulation. J Neurosci. 2003;23:5308.
85. Kleinjung T, Eichhammer P, Langguth B, et al. Long-term effects of repetitive transcranial magnetic stimulation (rTMS) in patients with chronic tinnitus. Otolaryngol Head Neck Surg. 2005;132:566.
86. Plewnia C, Reimold M, Najib A, et al. Moderate therapeutic efficacy of positron emission tomography-navigated repetitive transcranial magnetic stimulation for chronic tinnitus: a randomised, controlled pilot study. J Neurol Neurosurg Psychiatry. 2007;78:152.
87. Khedr EM, Kotb H, Kamel NF, et al. Long-lasting antalgic effects of daily sessions of repetitive transcranial magnetic stimulation in central and peripheral neuropathic pain. J Neurol Neurosurg Psychiatry. 2005;76:833.
88. Khedr EM, Rothwell JC, Ahmed MA, et al. Effect of daily repetitive transcranial magnetic stimulation for treatment of tinnitus: comparison of different stimulus frequencies. J Neurol Neurosurg Psychiatry. 2008;79:212.
89. Grappengiesser C. Versuche den Galvanismus zur heilung einiger Krankheiten anzuwenden. Berlin, 1801.
90. Rubenstein JT, Tyler RS. Electrical suppression of tinnitus. In: Snow J, editor. Tinnitus: Theories and Mechanisms. Shelton, CT: PMPH, 2003.
91. Lyttkens L, Lindberg P, Scott B, et al. Treatment of tinnitus by external electrical stimulation. Scand Audiol. 1986;15:157.
92. Dobie RA, Hoberg KE, Rees TS. Electrical tinnitus suppression: a double-blind crossover study. Otolaryngol Head Neck Surg. 1986;95:319.
93. Thedinger BS, Karlsen E, Schack SH. Treatment of tinnitus with electrical stimulation: an evaluation of the Audimax Theraband. Laryngoscope. 1987;97:33.
94. Herraiz C, Toledano A, Diges I. Trans-electrical nerve stimulation (TENS) for somatic tinnitus. Prog Brain Res. 2007;166:389.
95. Brackmann DE. Reduction of tinnitus in cochlear-implant patients. J Laryngol Otol Suppl. 1981;4:163.
96. Baguley DM, Atlas MD. Cochlear implants and tinnitus. Prog Brain Res. 2007;166:347.
97. Quaranta N, Wagstaff S, Baguley DM. Tinnitus and cochlear implantation. Int J Audiol. 2004;43:245.
98. Brozoski TJ, Bauer CA, Caspary DM. Elevated fusiform cell activity in the dorsal cochlear nucleus of chinchillas with psychophysical evidence of tinnitus. J Neurosci. 2002;22:2383.
99. Stephens SD. The treatment of tinnitus—a historical perspective. J Laryngol Otol. 1984;98:963.
100. Bauer CA, Brozoski TJ. Assessing tinnitus and prospective tinnitus therapeutics using a psychophysical animal model. J Assoc Res Otolaryngol. 2001;2:54.
101. Kaltenbach JA, Zhang J, Afman CE. Plasticity of spontaneous neural activity in the dorsal cochlear nucleus after intense sound exposure. Hear Res. 2000;147:282.
102. Bauer CA, Brozoski TJ, Myers K. Primary afferent dendrite degeneration as a cause of tinnitus. J Neurosci Res. 2007;85:1489.
103. Bauer CA, Brozoski TJ, Myers KS. Acoustic injury and TRPV1 expression in the cochlear spiral ganglion. Int Tinnitus J. 2007;13:21.
104. Bauer CA, Brozoski TJ. Effect of gabapentin on the sensation and impact of tinnitus. Laryngoscope. 2006;116:675.
105. Piccirillo JF, Finnell J, Vlahiotis A, et al. Relief of idiopathic subjective tinnitus: is gabapentin effective? Arch Otolaryngol Head Neck Surg. 2007;133:390.
106. Thompson GC, Thompson AM, Garrett KM, et al. Serotonin and serotonin receptors in the central auditory system. Otolaryngol Head Neck Surg. 1994;110:93.
107. Bauer CA, Brozoski TJ. Gabapentin. In: Langguth B, Hajak G, Kleinjung T, et al, editors. Tinnitus: Pathophysiology and Treatment. New York: Elsevier, 2007.
108. Brozoski TJ, Spires TJ, Bauer CA. Vigabatrin, a GABA transaminase inhibitor, reversibly eliminates tinnitus in an animal model. J Assoc Res Otolaryngol. 2007;8:105.
109. Shulman A, Strashun AM, Seibyl JP, et al. Benzodiazepine receptor deficiency and tinnitus. Int Tinnitus J. 2000;6:98.
110. Zoger S, Svedlund J, Holgers KM. The effects of sertraline on severe tinnitus suffering—a randomized, double-blind, placebo-controlled study. J Clin Psychopharmacol. 2006;26:32.
111. Robinson SK, Viirre ES, Bailey KA, et al. Randomized placebo-controlled trial of a selective serotonin reuptake inhibitor in the treatment of nondepressed tinnitus subjects. Psychosom Med. 2005;67:981.
112. Newman CW, Sandridge SA, Jacobson GP. Psychometric adequacy of the Tinnitus Handicap Inventory (THI) for evaluating treatment outcome. J Am Acad Audiol. 1998;9:153.
113. Baguley DM, Humphriss RL, Hodgson CA. Convergent validity of the tinnitus handicap inventory and the tinnitus questionnaire. J Laryngol Otol. 2000;114:840.
114. Halford JB, Anderson SD. Anxiety and depression in tinnitus sufferers. J Psychosom Res. 1991;35:383.
115. Henry JL, Wilson PH. Coping with tinnitus: two studies of psychological and audiological characteristics of patients with high and low tinnitus-related distress. Int Tinnitus J. 1995;1:85.
116. Katon W, Sullivan M, Russo J, et al. Depressive symptoms and measures of disability: a prospective study. J Affect Disord. 1993;27:245.
117. Egede LE. Major depression in individuals with chronic medical disorders: prevalence, correlates and association with health resource utilization, lost productivity and functional disability. Gen Hosp Psychiatry. 2007;29:409.
118. Katon WJ. The Institute of Medicine “Chasm” report: implications for depression collaborative care models. Gen Hosp Psychiatry. 2003;25:222.
119. Caffier PP, Haupt H, Scherer H, et al. Outcomes of long-term outpatient tinnitus-coping therapy: psychometric changes and value of tinnitus-control instruments. Ear Hear. 2006;27:619.
120. Kentish RC, Crocker SR, McKenna L. Children’s experience of tinnitus: a preliminary survey of children presenting to a psychology department. Br J Audiol. 2000;34:335.
121. Tyler RS, Baker LJ. Difficulties experienced by tinnitus sufferers. J Speech Hear Disord. 1983;48:150.
122. Folmer RL, Griest SE. Tinnitus and insomnia. Am J Otolaryngol. 2000;21:287.
123. Hebert S, Carrier J. Sleep complaints in elderly tinnitus patients: a controlled study. Ear Hear. 2007;28:649.
124. Megwalu UC, Finnell JE, Piccirillo JF. The effects of melatonin on tinnitus and sleep. Otolaryngol Head Neck Surg. 2006;134:210.
125. Rosenberg SI, Silverstein H, Rowan PT, et al. Effect of melatonin on tinnitus. Laryngoscope. 1998;108:305.
126. Handscomb L. Use of bedside sound generators by patients with tinnitus-related sleeping difficulty: which sounds are preferred and why? Acta Otolaryngol Suppl. 2006;556:59.
127. Espie CA, Inglis SJ, Tessier S, et al. The clinical effectiveness of cognitive behaviour therapy for chronic insomnia: implementation and evaluation of a sleep clinic in general medical practice. Behav Res Ther. 2001;39:45.
128. McKenna L, Daniel HC. Tinnitus-related insomnia treatment. In: Tyler RS, editor. Tinnitus Treatment Clinical Protocols. New York: Thieme, 2006.
129. Mathisen H. Phonophobia after stapedectomy. Acta Otolaryngol. 1969;68:73.
130. Citron D3rd, Adour KK. Acoustic reflex and loudness discomfort in acute facial paralysis. Arch Otolaryngol. 1978;104:303.
131. Woodhouse A, Drummond PD. Mechanisms of increased sensitivity to noise and light in migraine headache. Cephalalgia. 1993;13:417.
132. Nields JA, Fallon BA, Jastreboff PJ. Carbamazepine in the treatment of Lyme disease–induced hyperacusis. J Neuropsychiatry Clin Neurosci. 1999;11:97.
133. Gordon AG. Abnormal middle ear muscle reflexes and audiosensitivity. Br J Audiol. 1986;20:95.
134. Johnson LB, Comeau M, Clarke KD. Hyperacusis in Williams syndrome. J Otolaryngol. 2001;30:90.
135. Stouffer JL, Tyler RS. Characterization of tinnitus by tinnitus patients. J Speech Hear Disord. 1990;55:439.
136. Andersson G, Lindvall N, Hursti T, et al. Hypersensitivity to sound (hyperacusis): a prevalence study conducted via the Internet and post. Int J Audiol. 2002;41:545.
137. Rubinstein B. Tinnitus and craniomandibular disorders—is there a link? Swed Dent J Suppl. 1993;95:1.
138. Bartnik G, Fabijanska A, Rogowski M. Our experience in treatment of patients with tinnitus and/or hyperacusis using the habituation method. In Sixth International Tinnitus Seminar, Cambridge, United Kingdom, 1999.
139. Dauman R, Bouscau-Faure F. Assessment and amelioration of hyperacusis in tinnitus patients. Acta Otolaryngol. 2005;125:503.
140. Hawkins DB, Prosek RA, Walden BE, et al. Binaural loudness summation in the hearing impaired. J Speech Hear Res. 1987;30:37.
141. Sherlock LP, Formby C. Estimates of loudness, loudness discomfort, and the auditory dynamic range: normative estimates, comparison of procedures, and test-retest reliability. J Am Acad Audiol. 2005;16:85.
142. Stephens SD, Blegvad B, Krogh HJ. The value of some suprathreshold auditory measures. Scand Audiol. 1977;6:213.
143. Bornstein SP, Musiek FE. Loudness discomfort level and reliability as a function of instructional set. Scand Audiol. 1993;22:125.
144. Khalfa S, Dubal S, Veuillet E, et al. Psychometric normalization of a hyperacusis questionnaire. ORL J Otorhinolaryngol Relat Spec. 2002;64:436.
145. Gold SL, Frederick EA, Formby C. Shifts in dynamic range for hyperacusis patients receiving tinnitus retraining therapy (TRT). In Sixth International Tinnitus Seminar, Cambridge, United Kingdom, 1999.