CHAPTER 12 Tibial Tubercle Transfer
The goal of patellofemoral stabilization surgery is central, tracking of the patella in the femoral trochlea. If stable tracking can be achieved using nonoperative means such as core stability physical therapy, and bracing, surgery should be avoided. The caregiver should also rule out retinacular1,2 or articular3,4 pain causing the knee to give way. A thorough history and examination,5 using pain diagrams6 as needed, is central to accurate diagnosis and appropriate surgical planning. Unfortunately, many patients with recurrent patellar instability require some form of stabilization to function adequately in work and daily life, particularly in more vigorous activities. This is particularly important because chronic lateral patellofemoral articular overload may eventually cause joint breakdown.7 Debate continues regarding the evolution of trochlea dysplasia,8,9 but it is likely that chronic lateral facet overload from lateral patellar tracking10 may contribute to or cause deficiency of lateral trochlear containment of the patella.
It must be considered that balanced patellar tracking with optimal load distribution across the joint is best for patients and presumably minimizes risk of eventual cartilage deterioration and arthritis. Therefore, balanced tracking is of paramount importance. Multiple factors are involved in patellar tracking, including femoral version, tibial version, articular geometry, lower extremity kinematic function, muscle imbalance, foot and ankle mechanics, ligamentory balance of the knee, varies, valgus, body habitus, and posture. Some of these are correctable by nonoperative measures and should therefore be addressed before considering surgery.11 Certainly, an articular lesion causing symptoms of giving way may be mistaken for patellar instability and should be treated appropriately, whether by simple débridement12 or articular resurfacing.13–18
Procedures such as trochleoplasty and femoral and tibial derotation may be appropriate in rare patients but carry risks that many surgeons and patients find unacceptable. Therefore, traditional patellofemoral stabilization, using lateral release, medial retinacular restoration (medial patellofemoral ligament [MPFL] imbrication or reconstruction), and/or medial tibial tubercle transfer remain mainstays of patellofemoral stabilization. Lateral release19–22 has been used widely in the past but has little relevance as an isolated procedure for patients with patellar instability23 and can cause medial patellar instability24 when used extensively or inappropriately.
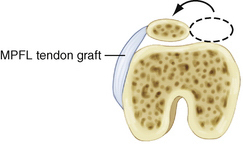
Restoration of patellofemoral balance by MPFL–medial capsule imbrication, often with release of a lateral retinaculum that has become adaptively tight, is desirable, particularly because it is known that the injured MPFL does heal,25 albeit elongated, in most patients. Sometimes, a tendon graft needs to be added to ensure adequate medial retinacular–MPFL support of the patella,26 but this should be done selectively, when less invasive surgery is judged to be insufficient. Many patients with less serious instability are happy to undergo a smaller procedure with the knowledge that another procedure might be needed in the future. This is occasionally preferable to the alternative risk of surgical complication from a more major surgical intervention. In any case, however, it is important to consider that the MPFL is an important restraint to lateral patellar instability27–29; be prepared to restore or reconstruct it selectively once adequate patellar tracking alignment had been ensured. Most important in this type of surgery is to avoid excessive patellofemoral joint loading, because the MPFL is a posteriorly oriented structure (Fig. 12-1). Tibial tubercle transfer is the best way to restore proper tracking of the patella in the trochlea in many cases, after which retinacular balance, including the MPFL, can be restored by imbrication or tendon graft reconstruction but without exerting force on the patella. Following tibial tubercle transfer balancing of the extensor mechanism, however, MPFL restoration is often unnecessary, because it usually adapts over time.
TREATMENT
Indications
In patients with more serious lateral patellar tracking, the medial-lateral distance30 between the tibial tuberosity and trochlear groove (TTTG) is often 15 to 20 mm or more. A well-done axial radiograph at 45 degrees of knee flexion31 and a precise lateral32 radiograph are extremely important in determining the resting position of the patella with respect to the trochlea. The patient with prominent J tracking and disability related to serious lateral patellar tracking will often benefit most from medial transfer of the tibial tubercle.33,34 This is a compensatory procedure that does not correct all the underlying structural problems; however, a medial tibial tubercle transfer yields functional stabilization of the patellofemoral joint quickly and without exerting a posteromedial pull vector on the patella. Tibial tubercle transfer yields balanced patellofemoral tracking, the possibility of immediate range of motion after surgery, and permanent stability when properly and accurately performed.
Tibial tubercle transfer can also unload the distal patella by adding obliquity to the cut behind the tibial tubercle (anteromedial tibial tubercle transfer), thereby lifting up and unloading the distal and lateral patellar articulating surfaces. These are frequently fragmented and/or painful in the patient with chronic lateral patellar tracking.35–40
As the lateral and distal patella manifest evidence of degenerative cartilage related to excessive lateral pressure, anteromedial tibial tubercle transfer becomes more important for redistribution of contact forces on the patella and for enhanced stability and joint preservation. Long-term results of anteromedial tibial tubercle transfer have been very good in properly selected patients with lateral and distal patellar articular damage.40,41 Medial patellofemoral ligament reconstruction is not as likely to help these patients and involves some risk of chronic pain if a fragmented distal medial patella receives added load following medial capsule ligamentous reconstruction.
Nonetheless, retinacular balancing in conjunction with tibial tubercle transfer can be helpful and sometimes necessary. In particular, when there is trochlear dysplasia,42 supplemental MPFL advancement, imbrication, or reconstruction may help in achieving an optimal, balanced end result. The key here is achieving balanced tracking of the patella first (this often requires tibial tubercle transfer when there is an elevated TTTG distance, Q angle, and trochlea dysplasia) and then adjusting the retinacular-ligamentous peripatellar restraints. Note that retinacular restraints to pull the patella into place should not be used because of the risk of creating articular overload. Additionally, MPFL reconstruction must be done with exquisite attention to accuracy or articular excessive articular loading will likely occur.43
Arthroscopic Technique
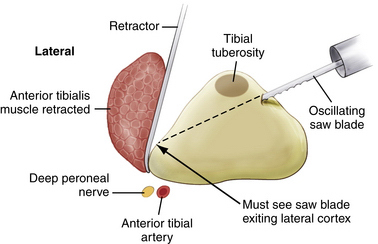
Exsanguinate the extremity and inflate the tourniquet. Incise the skin longitudinally from the midpatellar tendon to about 5 cm distal to the tibial tubercle. Release the anterior tibialis muscle from the anterior tibia and reflect posteriorly all the way to the posterior tibia subperiosteally (Fig. 12-2). Dissect behind patellar tendon enough to expose 1cm above patellar tendon insertion.
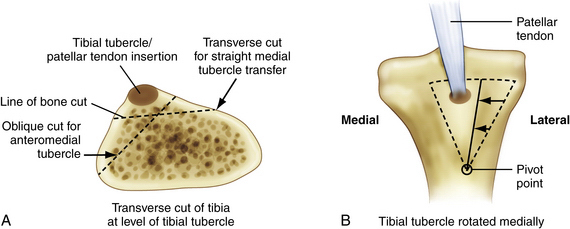
Plan the osteotomy to provide a flat cut (tapered to anterior tibia distally) for pure medial tibial tubercle transfer (Elmslie-Trillat procedure; Fig. 12-3). Perform an oblique osteotomy from the anteromedial tibia, adjacent to the patellar tendon insertion (see Fig. 12-3) to achieve anteromedial tibial tubercle transfer (see Figs. 12-2 and 12-3A). Be sure of exposure and use an oscillating saw to make the cut, using a guide system as needed, but be sure that the cut is appropriate for the desired medial and anterior transposition of the tibial tubercle. Again, be sure to taper the osteotomy to the anterior tibia distally (Fig. 12-4).
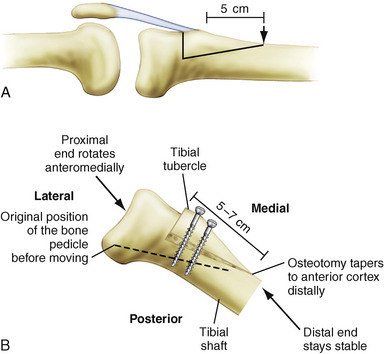
FIGURE 12-4 Lateral view of the patellofemoral joint. The osteotomy should be tapered to the anterior tibia distally.
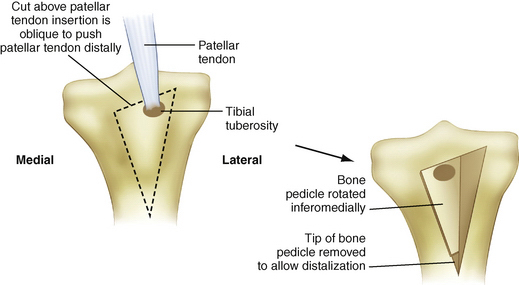
In the patient with documented patella alta, slight distalization of the tibial tubercle may be needed. This is not often necessary but is important in the patella alta patient to ensure proper timely entry of the patella into the trochlea. To accomplish distalization (usually no more than 5 to 8 mm), just enough to allow prompt entry of the patella into the trochlea arthroscopically at the initiation of flexion, remove about 1 cm of the distal tip of the bone pedicle, slide the pedicle distally the desired amount, and place an autogenous corticocancellous bone graft from the lateral metaphysis above the transferred pedicle. Then, secure the transferred bone pedicle, properly oriented, with two cortical lag screws into the posterior cortex. Another option is to make a proximal cut above the patellar tendon insertion, which is vertical and angled so that the tibial tubercle is forced slightly distally on medialization (Fig. 12-5). This technique is pertinent only when there is need for medialization at the time of tubercle distalization.
Anterolateral tibial tubercle transfer (ALTTT) can be very effective in reversing a previous Hauser procedure. ALTTT can unload a worn out medial patellar articular surface. Anteromedial tibial tubercle transfer has been useful as an adjunct to articular resurfacing procedures and has been shown to be effective by Farr and associates.35
PEARLS& PITFALLS
PEARLS
Postoperative Management
Compression, elevation, and cryotherapy are helpful for 1 to 2 weeks. After almost all tibial tubercle transfer procedures, knee range of motion should be started as soon as possible. Thus, fixation must be secure enough to permit this. Early motion out of the postoperative splint should encourage 90 degrees of flexion, once daily, by 2 to 3 weeks after surgery. Crutches should be used for 5 to 6 weeks with a gradual increase of weight bearing to full weight by 6 weeks. Most patients will then benefit from physical therapy to optimize motion, strength, proprioception, and return to optimal function.
1. Fulkerson JP, Tennant R, Jaivin JS, Grunnet M. Histologic evidence of retinacular nerve injury associated with patellofemoral malalignment. Clin Orthop Relat Res. 1985;(197):196-205.
2. Biedert RM, Stauffer E, Friederich NF. Occurrence of free nerve endings in the soft tissue of the knee joint. A histologic investigation. Am J Sports Med. 1992;20:430-433.
3. Post WR. Anterior knee pain: diagnosis and treatment. J Am Acad Orthop Surg. 2005;13:534-543.
4. Post WR. Clinical evaluation of patients with patellofemoral disorders. Arthroscopy. 1999;15:841-851.
5. Fulkerson JP. Diagnosis and treatment of patients with patellofemoral pain. Am J Sports Med. 2002;30:447-456.
6. Post WR, Fulkerson J. Knee pain diagrams: correlation with physical examination findings in patients with anterior knee pain. Arthroscopy. 1994;10:618-623.
7. Ficat P. The syndrome of lateral hyperpressure of the patella. Acta Orthop Belg. 1978;44:65-76.
8. Dejour H, Walch G, Nove-Josserand L, Guier C. Factors of patellar instability: an anatomic radiographic study. Knee Surg Sports Traumatol Arthrosc. 1994;2:19-26.
9. Dejour H, Walch G, Neyret P, Adeleine P. Dysplasia of the femoral trochlea. Rev Chir Orthop Reparatrice Appar Mot. 1990;76:45-54.
10. Ostermeier S, Holst M, Hurschler C, et al. Dynamic measurement of patellofemoral kinematics and contact pressure after lateral retinacular release: an in vitro study. Knee Surg Sports Traumatol Arthrosc. 2007;15:547-554.
11. Ireland ML, Willson JD, Ballantyne BT, Davis IM. Hip strength in females with and without patellofemoral pain. J Orthop Sports Phys Ther. 2003;33:671-676.
12. Federico DJ, Reider B. Results of isolated patellar debridement for patellofemoral pain in patients with normal patellar alignment. Am J Sports Med. 1997;25:663-669.
13. Jones DG, Peterson L. Autologous chondrocyte implantation. J Bone Joint Surg Am. 2006;88:2502-2520.
14. Knutsen G, Drogset JO, Engebretsen L, et al. A randomized trial comparing autologous chondrocyte implantation with microfracture. Findings at five years. J Bone Joint Surg Am. 2007;89:2105-2112.
15. Knutsen G, Engebretsen L, Ludvigsen TC, et al. Autologous chondrocyte implantation compared with microfracture in the knee. A randomized trial. J Bone Joint Surg Am. 2004;86:455-464.
16. Lee G, Kelly MA. Isolated patellofemoral arthritis without malalignment. In: Fulkerson J, editor. Common Patellofemoral Problems. Rosemont, Ill: American Academy of Orthopaedic Surgeons; 2005:73-84.
17. Minas T. Autologous chondrocyte implantation for focal chondral defects of the knee. Clin Orthop Relat Res. 2001;(391 suppl):S349.
18. Saleh KJ, Arendt EA, Eldridge J, et al. Symposium. Operative treatment of patellofemoral arthritis. J Bone Joint Surg Am. 2005;87:659-671.
19. Lattermann C, Toth J, Bach BRJr. The role of lateral retinacular release in the treatment of patellar instability. Sports Med Arthrosc Rev. 2007;15:57-60.
20. Ford DH, Post WR. Open or arthroscopic lateral release. Indications, techniques, and rehabilitation. Clin Sports Med. 1997;16:29-49.
21. Fulkerson JP, Schutzer SF, Ramsby GR, Bernstein RA. Computerized tomography of the patellofemoral joint before and after lateral release or realignment. Arthroscopy. 1987;3:19-24.
22. Panni AS, Tartarone M, Patricola A, et al. Long-term results of lateral retinacular release. Arthroscopy. 2005;21:526-531.
23. Fithian DC, Paxton EW, Post WR, Panni AS. Lateral retinacular release: a survey of the International Patellofemoral Study Group. Arthroscopy. 2004;20:463-468.
24. Hughston JC, Deese M. Medial subluxation of the patella as a complication of lateral retinacular release. Am J Sports Med. 1988;16:383-388.
25. Tom A, Fulkerson J. Restoration of native MPFL support after patella dislocation. Sports Med Arthrosc Rev. 2007;15:68-71.
26. Bicos J, Fulkerson JP, Amis A. Current concepts review: the medial patellofemoral ligament. Am J Sports Med. 2007;35:484-492.
27. Amis AA, Firer P, Mountney J, et al. Anatomy and biomechanics of the medial patellofemoral ligament. Knee. 2003;10:215-228.
28. Arendt EA, Fithian DC, Cohen E. Current concepts of lateral patella dislocation. Clin Sports Med. 2002;21:499-519.
29. Nomura E, Horiuchi Y, Kihara M. Medial patellofemoral ligament restraint in lateral patellar translation and reconstruction. Knee. 2000;7:121-127.
30. Goutallier D, Bernageau J, Lecudonnec B. The measurement of the tibial tuberosity. Patella groove distance technique and results (author’s transl). Rev Chir Orthop Reparatrice Appar Mot. 1978;64:423-428.
31. Merchant AC, Mercer RL, Jacobsen RH, Cool CR. Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am. 1974;56:1391-1396.
32. Malghem J, Maldague B. Profile of the knee. Differential radiologic anatomy of the articular surfaces. J Radiol. 1986;67:725-735.
33. Pritsch T, Haim A, Arbel, R, et al. Tailored tibial tubercle transfer for patellofemoral malalignment: analysis of clinical outcomes. Knee Surg Sports Traumatol Arthrosc. 2007;15:994-1002.
34. Trillat A, Dejour HL, Coutette A. Diagnostic et traitement des subluxations recidivantes de la rotule. Rev Chir Orthop. 1964;50:813-824.
35. Farr J, Schepsis A, Cole B, et al. Anteromedialization: review and technique. J Knee Surg. 2007;20:120-128.
36. Fulkerson JP. Anteromedialization of the tibial tuberosity for patellofemoral malalignment. Clin Orthop Relat Res. 1983;(177):176-181.
37. Fulkerson JP, Becker GJ, Meaney JA, et al. Anteromedial tibial tubercle transfer without bone graft. Am J Sports Med. 1990;18:490-496.
38. Fulkerson JP. Anteromedial tibial tubercle transfer. In: Jackson DW, editor. Master Techniques in Orthopaedic Surgery: Reconstructive Knee Surgery. Philadelphia: Lippincott, Williams & Wilkins; 2003:13-25.
39. Karamehmetoglu M, Ozturkmen Y, Azboy I, Caniklioglu M. Fulkerson osteotomy for the treatment of chronic patellofemoral malalignment. Acta Orthop Traumatol Turc. 2007;41:21-30.
40. Pidoriano AJ, Weinstein RN, Buuck DA, Fulkerson JP. Correlation of patellar articular lesions with results from anteromedial tibial tubercle transfer. Am J Sports Med. 1997;25:533-537.
41. Buuck D, Fulkerson J. Anteromedialization of the tibial tubercle: a 4- to 12-year follow-up. Oper Tech Sports Med. 2000;8:131-137.
42. Schottle PB, Scheffler SU, Schwarck A, Weiler A. Arthroscopic medial retinacular repair after patellar dislocation with and without underlying trochlear dysplasia: a preliminary report. Arthroscopy. 2006;22:1192-1198.
43. Elias JJ, Cosgarea AJ. Technical errors during medial patellofemoral ligament reconstruction could overload medial patellofemoral cartilage: a computational analysis. Am J Sports Med. 2006;34:1478-1485.