Chapter 18 Tibial Nerve
Popliteal Fossa and Leg
Anatomy
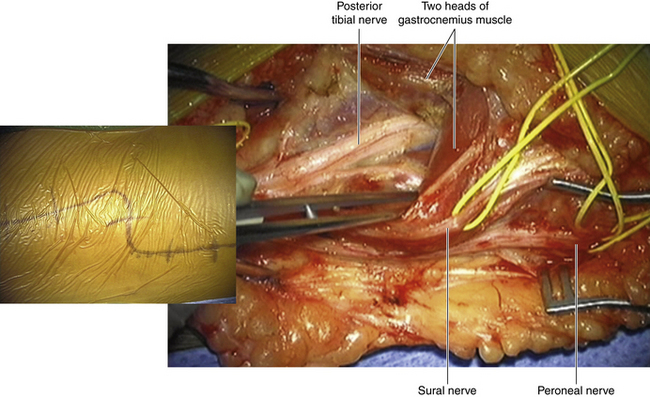
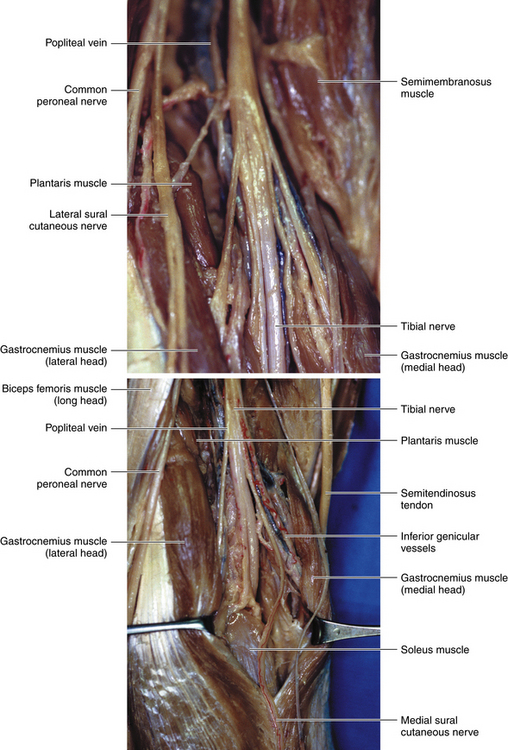
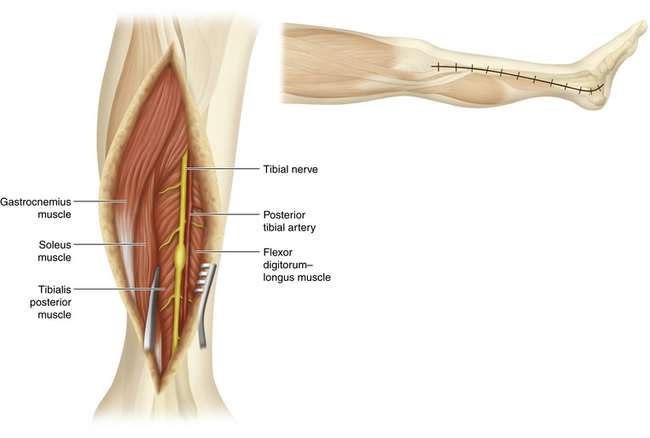
• The gastrocnemius arises from two heads that attach to the distal femur (Figure 18-1). The muscle is superficial to the soleus, and the two muscles jointly form the Achilles tendon, which inserts into the calcaneus. The soleus arises from the fibula and tibia, forming a fibrous arch between them. Just as the median nerve runs a straight course deep to the arch of origin of the flexor digitorum superficialis, so does the posterior tibial nerve run deep to the soleus arch (Figure 18-2).
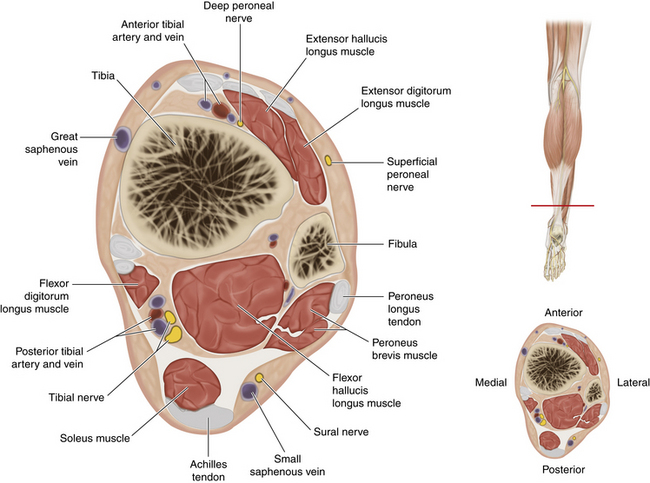
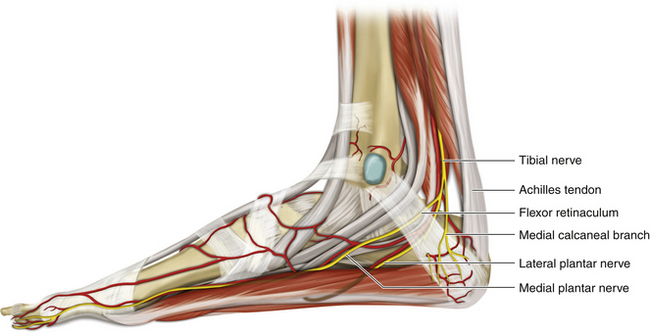
• The tendons of all three deep muscles of the calf run beneath the flexor retinaculum at the ankle. Characteristically, the flexor hallucis longus (FHL) maintains fleshy muscle fibers further distally than the other two (Figure 18-3). The posterior tibial nerve runs straight down the leg from the popliteal fossa to the flexor retinaculum, remaining medial to the border of the FHL throughout.
• The flexor retinaculum is a locally thickened band of fascia that runs between the medial malleolus and the calcaneus.
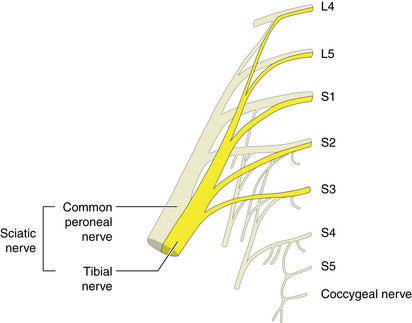
• The tibial nerve is a major branch of the sciatic nerve (Figure 18-4). When viewed from behind, the tibial nerve is overlapped proximally by the hamstring muscles. Becoming superficial in the popliteal fossa, it crosses the popliteal vessels and descends deep to the heads of gastrocnemius behind the knee joint, crossing the popliteus muscle to run beneath the fibrous arch in the soleus (see Figure 18-2).
• Muscular branches from the tibial nerve at the popliteal fossa arise between the heads of the gastrocnemius and supply the muscles of the popliteal fossa: (1) the plantaris, (2) the two heads of the gastrocnemius, (3) the soleus, and (4) the popliteus. The tibial nerve descends deep to the two heads of the gastrocnemius (see Figure 18-1).
• Distally, the posterior tibial nerve is covered only by skin and fascia.
• At the junction of the upper and middle thirds of the leg, branches to the tibialis posterior (responsible for foot inversion) and an additional branch to the soleus arise; slightly more distally, branches to the flexors of the big toe and the other toes originate.
Surgical Technique
Positioning and Incision
• For exposure of the tibial nerve in the distal thigh, popliteal space, and proximal calf, the surgeon should use a midline lower thigh incision. The incision should run in the flexor crease for a short distance before going down over the proximal calf. With the patient in a prone position, the nerve is superficial to the popliteal artery and vein.
Dissection
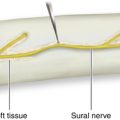
• The popliteal artery and vein and the peroneal nerve are in close proximity. The tibial nerve can be split away from the vessels and encircled with a Penrose drain. This drain is then used for gentle traction as the tibial motor branches are approached. Care must be taken to preserve tibial input to the sural nerve, which can originate at this level.
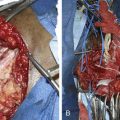
• When a scar involves both nerves and vessels, it requires a great deal of care to extract the branches and the deeper main tibial nerve without causing vascular damage to the main vessels. Small vascular branches, whether arteries or veins, can be divided.
Distal Nerve Exposure
Positioning and Incision
• The main tibial nerve can be traced into the upper third of the calf from the popliteal incision, but exposure of the more distal portion of the nerve requires a different approach.
• Lesions in the midleg segment are best approached by a vertical incision along the medial leg (Figure 18-5).
• For this approach, the patient is placed supine with the leg externally rotated.
• The gastrocnemius and soleus muscles are identified. This muscle mass is split away from its fascial attachment to the tibia for a distance and retracted.
• The nerve lies deep to the soleus, which is retracted with the gastrocnemius, and runs along the medial border of the FHL. The nerve can always be found at the flexor retinaculum and traced proximally if identification is impeded by heavy scar.
• If the patient is prone, a midleg dissection can be combined with an upper third and popliteal level dissection.
• Dissection of the nerve and adjacent vessels, which are sometimes injured along with the nerve, requires patience and perseverance. These are usually not easy dissections.
• As with nerve lesions elsewhere, it is best to expose the nerve both above (or proximal to) and below (or distal to) the lesion, encircle the more normal portion of the element, and then gradually work the dissection toward the lesion itself.
Ankle and Foot
Anatomy
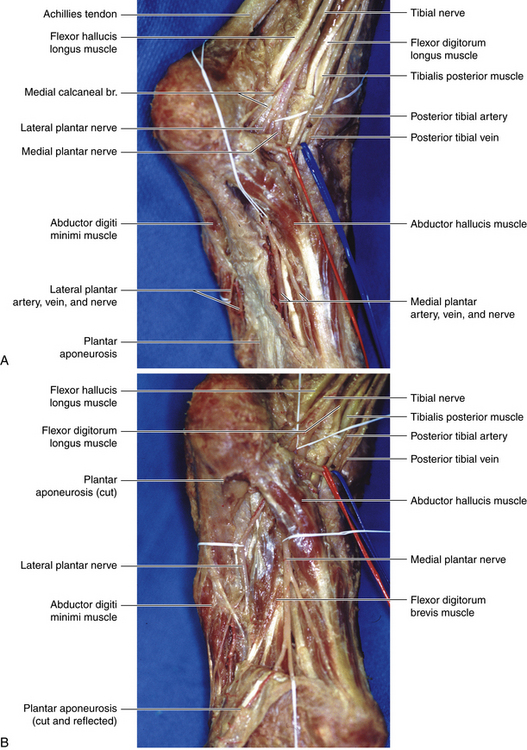
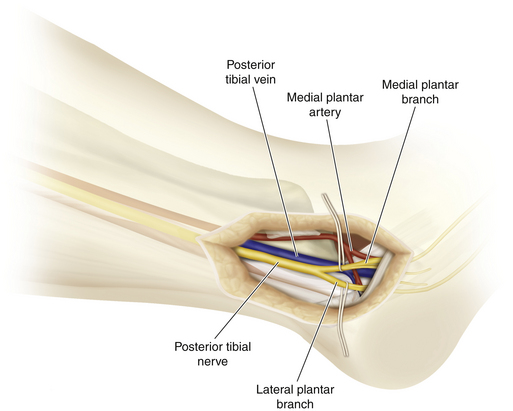
• Distally, the posterior tibial nerve gives medial calcaneal branches (S1 and S2) proximal to the flexor retinaculum to supply the skin of the heel and the medial side of the sole of the foot (Figure 18-6).
• The medial plantar nerve is the larger of the two terminal divisions of the tibial nerve. Having originated under the flexor retinaculum, the abductor hallucis longus courses lateral to the medial plantar artery, deep to the abductor hallucis lying between it and the flexor digitorum brevis.
• The lateral plantar nerve is comparable with the ulnar nerve in the hand, and has both cutaneous and muscular distribution. The lateral plantar nerve supplies the skin of the small toe and the lateral half of the fourth toe. The lateral plantar nerve supplies most deep muscles of the foot. It runs forward, medial to the lateral plantar artery, toward the tubercle of the fifth metatarsal and between the flexor digitorum brevis and the flexor digitorum accessorius longus.
• Between the flexor digitorum brevis and the abductor digiti minimi, the lateral plantar nerve ends by dividing into superficial and deep branches. The lateral plantar nerve supplies the flexor digitorum accessorius longus and abductor digiti minimi muscles before its division. Small branches pierce the plantar fascia to supply the skin of the lateral plantar side.
• The deep branch of the lateral plantar nerve, accompanying the lateral plantar artery, passes deep to the flexor tendons and the adductor hallucis (Figure 18-7). It supplies the second to fourth lumbricals, the adductor hallucis, and all the interossei except that of the fourth metatarsal space. The superficial branch of the lateral plantar nerve divides into two common plantar digital nerves to supply the lateral side of the fifth toe, the flexor digiti minimi brevis, and the interossei of the fourth intermetatarsal space.
Surgical Technique
Patient Positioning and Incision
• With the patient supine and the leg externally rotated, an incision is made beginning medial to the distal Achilles tendon and running beneath the medial malleolus.
• The incision can be extended to the instep area but not onto the weight-bearing portion of the plantar surface of the foot.
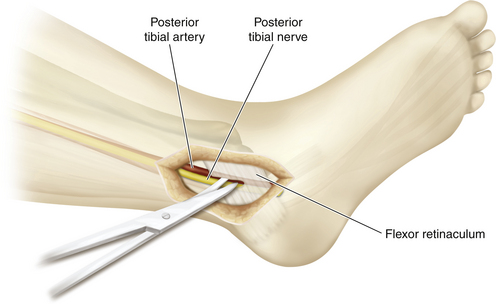
• The incision is deepened to expose the tibial nerve, first proximal to the flexor retinaculum and then beneath the medial malleolus. The flexor retinaculum is divided as the nerve is traced downward (Figure 18-8).
• The posterior tibial artery and vein are closely intertwined with the nerve. During dissection of the proximal portion of the tarsal tunnel, the artery is mobilized away from the nerve.
• Calcaneal branches leave the nerve posteriorly to supply sensation to the heel of the foot. They should be respected because they supply the weight-bearing area of the heel.
• Soon thereafter, the main tibial nerve divides into lateral and medial plantar nerves, and these in turn usually divide before the instep region of the foot is reached. This natural division can be increased proximally by sharp dissection with a scalpel. Vessels are dissected and retracted separately.
• It helps to encircle with plastic loops not only the nerve branches but also the major branches of the vessels to facilitate dissection of the nerve (Figure 18-9).
• In those few cases of tarsal tunnel syndrome that require surgery, the nerve is decompressed by dividing the flexor retinaculum, and the medial and lateral plantar nerves are dissected for 1 centimeter more to be certain there are no impingements on the proximal course of these nerves.