250 Thrush
Salient features
Examination
• Superficial white patches or large fluggy membranes that are easily detachable (e.g. by a tongue depressor), leaving underlying erythema (Figs 250.1 and 250.2)
• Erythema, transverse fissuring and maceration may be seen at the angles of the mouth (perleche) as an associated finding.
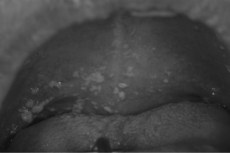
Fig. 250.1 Pseudomembranous candidiasis of the palate demonstrating multiple areas of Candida colonization.
(With permission from Lerman MA, Laudenbach J, Marty FM. Management of oral infections in cancer patients. Dental Clin North Am 2008;52:129–53.)
• Look for other sites of candidal infection (eczematoid lesions in moist areas of the skin, such as inframammary folds, inguinal creases, between the fingers and toes).
• Look for id reactions (which are hypersensitivity cutaneous reactions remote from the site of infection).
• Ask the patient about dysphagia (oesophagitis).
• Tell the examiner that you would like to investigate for underlying:
Questions
With which type of antibiotics is candidal infection common?
Broad-spectrum antibiotics, e.g. tetracycline, chloramphenicol.
How would you treat candidal infection?
• Effective antifungal therapy may be achieved with fluconazole, ketoconazole, clotrimazole or nystatin. Amphotericin lozenges may be useful in oral candidal infection. Itraconazole may be substituted when there is concomitant dermatophyte disease.
• Sexual partners of oral or vaginal disease should be screened and appropriately treated.
What are the features of disseminated candidiasis?
• Disseminated candidiasis manifests with systemic features including fever, toxicity, pulmonary involvement, endocarditis and retinal abscesses. Very rarely, it may cause focal manifestations including pustular skin abscesses, osteomyelitis, myositis, brain abscess or meningitis. It often causes sepsis associated with intravenous catheterization.
How is disseminated candidiasis treated?
• Patients with blood cultures with Candida should receive intravenous amphotericin B. For candidaemia in those with renal failure, fluconazole is an alternative because of the absence of restrictions on intravenous administration in patients with a creatinine clearance <50 ml/min.
• Echonocandins and newer generation azoles may be considered if fluconazole fails or patients are intolerant to amphotericin B. The echinocandins (caspofungin, anidulafungin, micafungin) have a broad spectrum of activity against a variety of Candida spp. and, therefore, may be preferred when C. glabrata or C. krusei is identified or suspected. The choice of an echinocandin, as opposed to an azole, for initial therapy of candidaemia in a patient who does not have neutropenia is not well established. The echinocandins are not well absorbed orally and must be administered intravenously. Renal insufficiency does not require dose adjustment.







