15 Thromboembolic Phenomena and Vegetations
Background
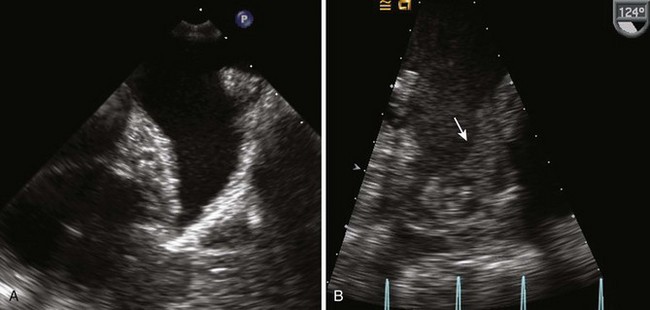
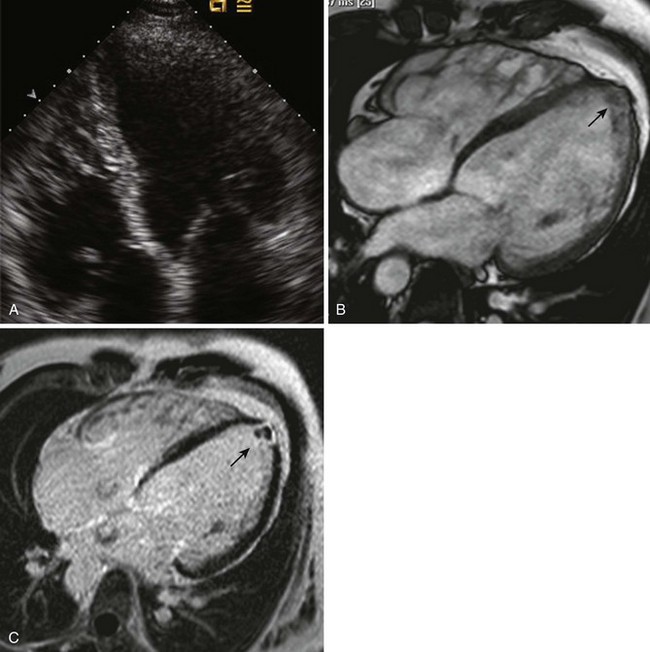
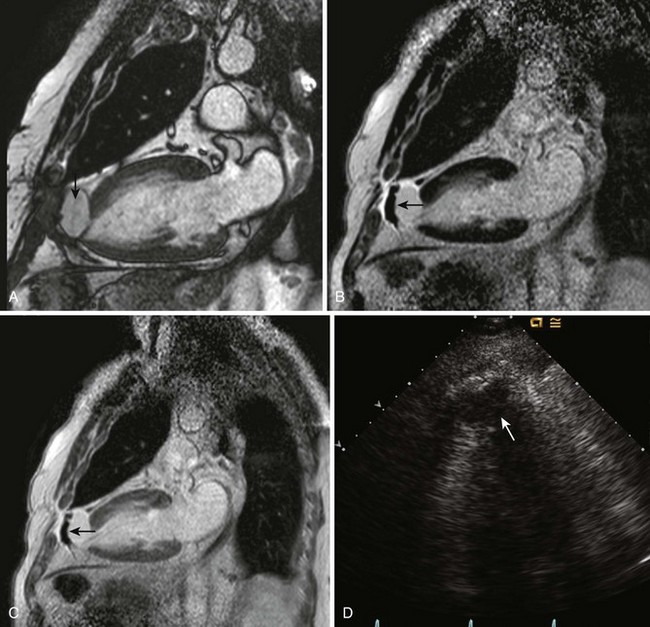
Thrombus
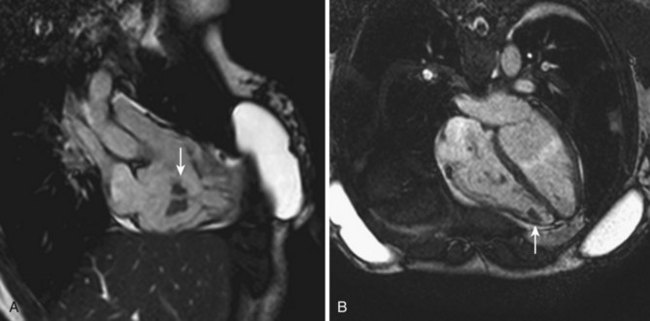
Vegetations
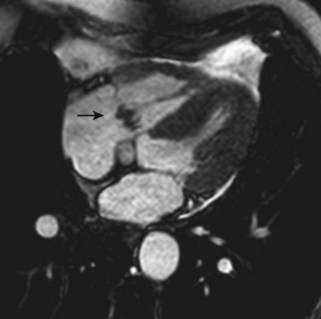
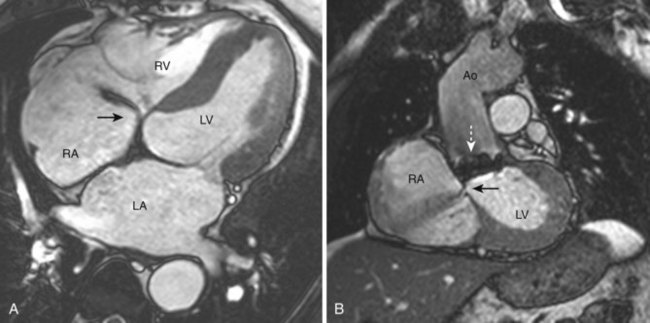
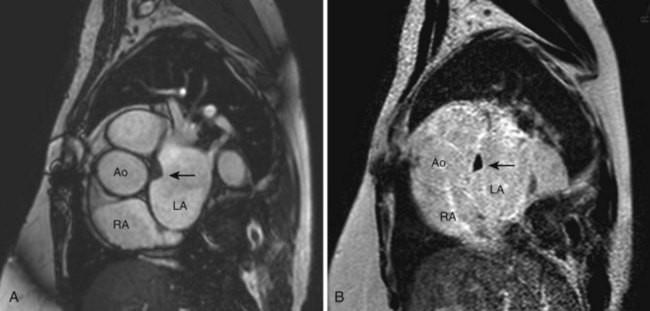
Figure 15-6 4C SSFP cine MRI demonstrating a tricuspid valve vegetation (arrow) on the atrial side of the valve.
A more detailed discussion of the evaluation of endocarditis can be found in Chapter 14 of the Echocardiography Review Guide by C. M. Otto and R. G. Schwaegler.
Overview of Echocardiographic Approach
Two-Dimensional
Color Doppler
Anatomic Imaging
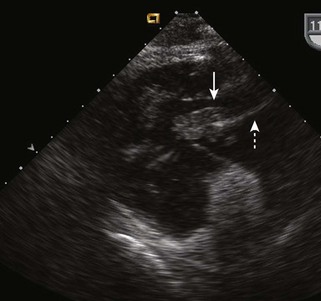
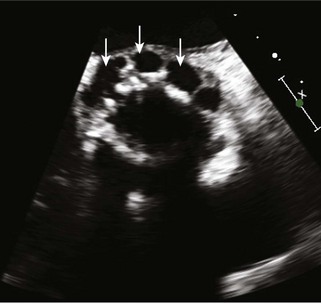
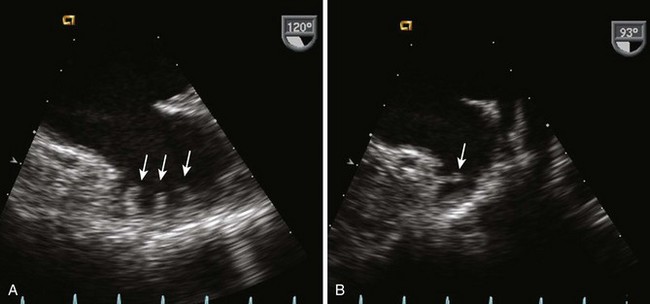
Left Atrial Thrombus
Image Acquisition
Pitfalls
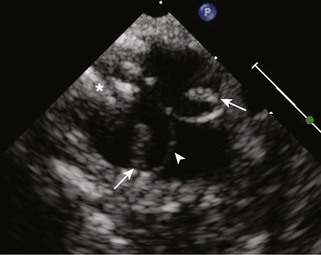
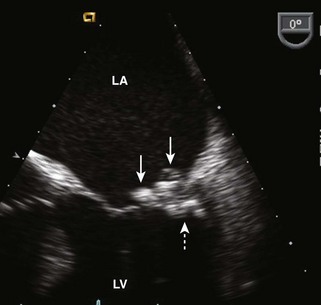
Left Ventricular Thrombus
Image Acquisition
Pitfalls
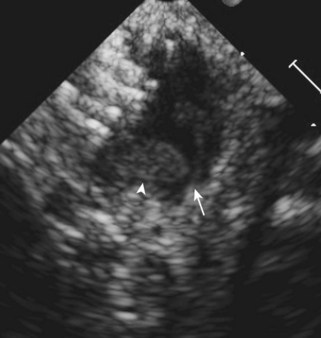
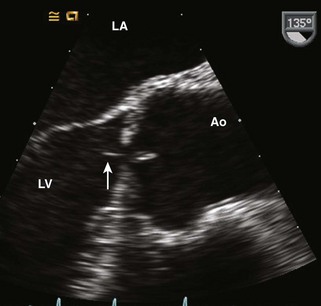
Valve Vegetations
Image Acquisition (Whether TEE or TTE)
Pitfalls
Alternate Approaches
Key Points
1 Shanewise JS, Cheung AT, Aronson S, et al. ASE/SCA guidelines for performing a comprehensive intraoperative multiplane transesophageal echocardiography examination: recommendations of the American Society of Echocardiography Council for Intraoperative Echocardiography and the Society of Cardiovascular Anesthesiologists Task Force for Certification in Perioperative Transesophageal Echocardiography. J Am Soc Echocardiogr. 1999;12:884-900.
2 Bonow RO, Carabello BA, Chatterjee K, et al. ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing Committee to Revise the 1998 guidelines for the management of patients with valvular heart disease) developed in collaboration with the Society of Cardvascular Anesthesiologists endorsed by the Society for Cardiovascular Angiography and Interventions and the Society of Thoracic Surgeons. J Am Coll Cardiol. 2006;48:e1-e148.
3 Zoghbi WA, Chambers JB, Dumesnil JG, et al. Recommendations for evaluation of prosthetic valves with echocardiography and Doppler ultrasound: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Task Force on Prosthetic Valves, developed in conjunction with the American College of Cardiology Cardiovascular Imaging Committee, Cardiac Imaging Committee of the American Heart Association, the European Association of Echocardiography, a registered branch of the European Society of Cardiology, the Japanese Society of Echocardiography and the Canadian Society of Echocardiography, endorsed by the American College of Cardiology Foundation, American Heart Association, European Association of Echocardiography, a registered branch of the European Society of Cardiology, the Japanese Society of Echocardiography, and Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2009;22:975-1014.
4 Otto CM, Schwaegler RG. Echocardiography Review Guide. Philadelphia: Saunders; 2007.