Thorax
Conceptual overview
General description
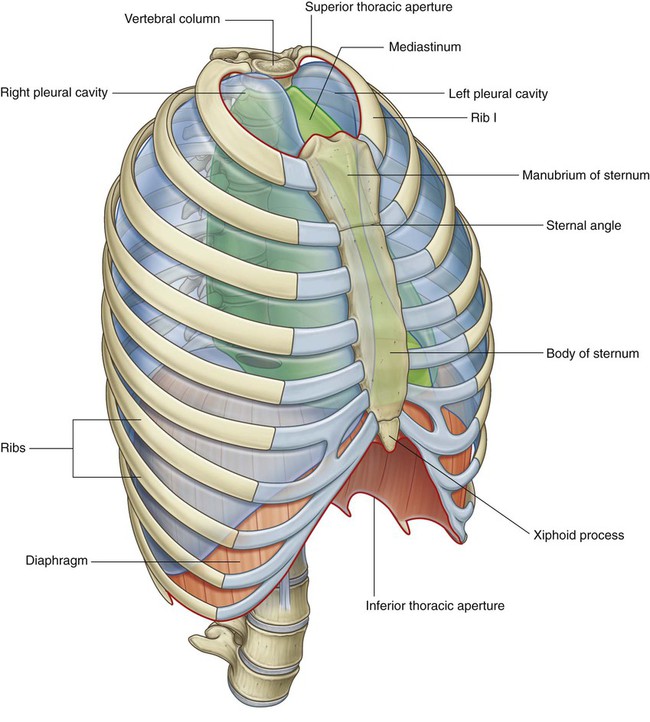
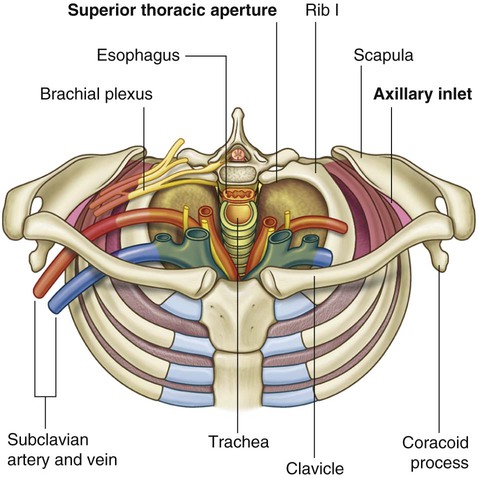
The thorax is an irregularly shaped cylinder with a narrow opening (superior thoracic aperture) superiorly and a relatively large opening (inferior thoracic aperture) inferiorly (Fig. 3.1). The superior thoracic aperture is open, allowing continuity with the neck; the inferior thoracic aperture is closed by the diaphragm.
Component parts
Thoracic wall
The thoracic wall consists of skeletal elements and muscles (Fig. 3.1):
 Posteriorly, it is made up of twelve thoracic vertebrae and their intervening intervertebral discs;
Posteriorly, it is made up of twelve thoracic vertebrae and their intervening intervertebral discs;
 Laterally, the wall is formed by ribs (twelve on each side) and three layers of flat muscles, which span the intercostal spaces between adjacent ribs, move the ribs, and provide support for the intercostal spaces;
Laterally, the wall is formed by ribs (twelve on each side) and three layers of flat muscles, which span the intercostal spaces between adjacent ribs, move the ribs, and provide support for the intercostal spaces;
 Anteriorly, the wall is made up of the sternum, which consists of the manubrium of sternum, body of sternum, and xiphoid process.
Anteriorly, the wall is made up of the sternum, which consists of the manubrium of sternum, body of sternum, and xiphoid process.
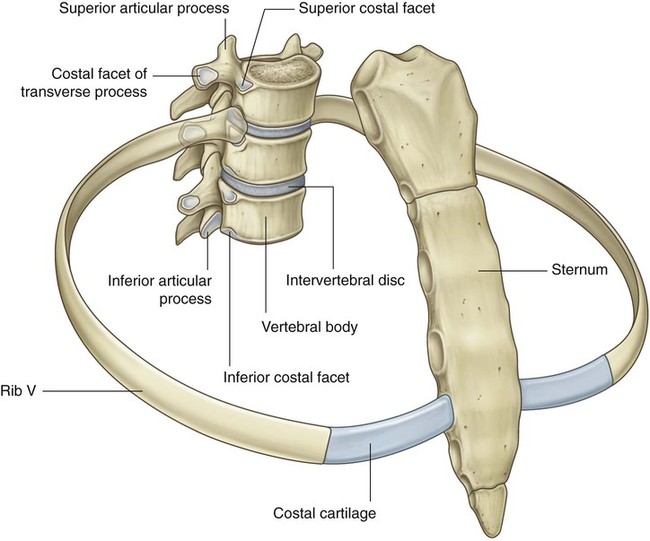
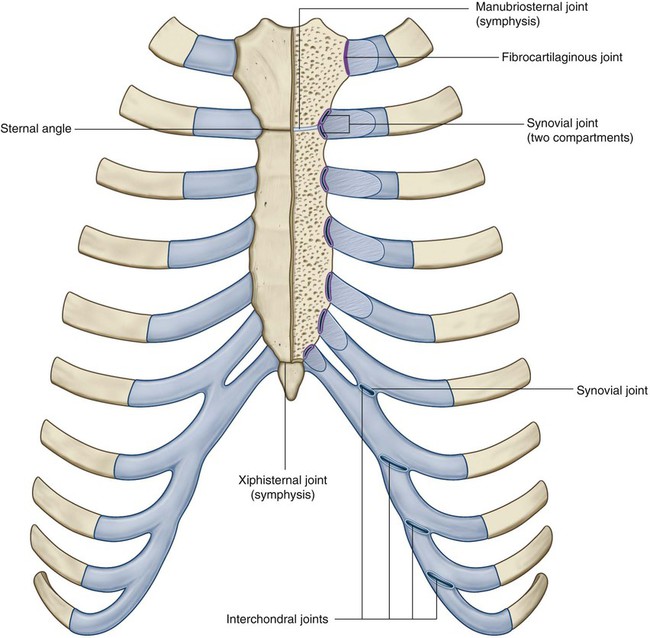
All ribs articulate with thoracic vertebrae posteriorly. Most ribs (from rib II to IX) have three articulations with the vertebral column. The head of each rib articulates with the body of its own vertebra and with the body of the vertebra above (Fig. 3.2). As these ribs curve posteriorly, each also articulates with the transverse process of its vertebra.
Anteriorly, the costal cartilages of ribs I to VII articulate with the sternum.
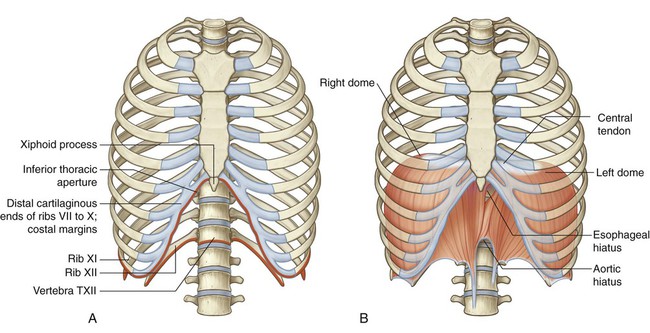
Inferior thoracic aperture
The inferior thoracic aperture is large and expandable. Bone, cartilage, and ligaments form its margin (Fig. 3.4A).
Skeletal elements of the inferior thoracic aperture are:
 the body of vertebra TXII posteriorly,
the body of vertebra TXII posteriorly,
 rib XII and the distal end of rib XI posterolaterally,
rib XII and the distal end of rib XI posterolaterally,
 the distal cartilaginous ends of ribs VII to X, which unite to form the costal margin anterolaterally, and
the distal cartilaginous ends of ribs VII to X, which unite to form the costal margin anterolaterally, and
When viewed anteriorly, the inferior thoracic aperture is tilted superiorly.
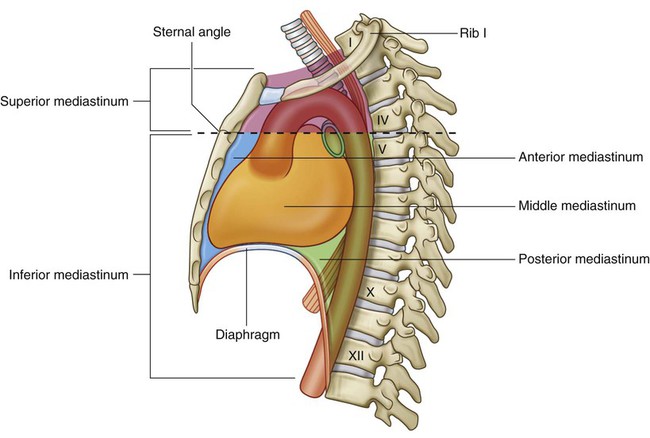
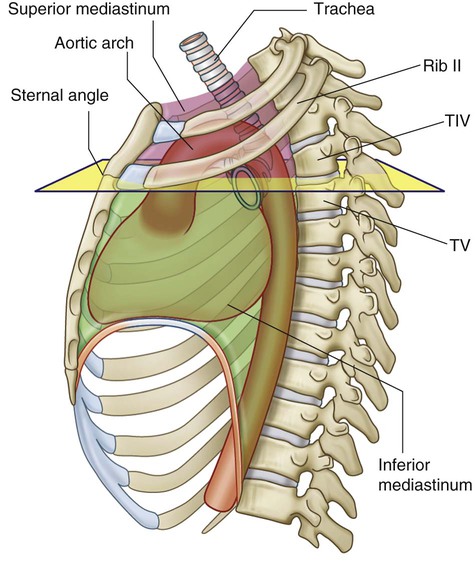
Mediastinum
A horizontal plane passing through the sternal angle and the intervertebral disc between vertebrae TIV and TV separates the mediastinum into superior and inferior parts (Fig. 3.5). The inferior part is further subdivided by the pericardium, which encloses the pericardial cavity surrounding the heart. The pericardium and heart constitute the middle mediastinum.
Relationship to other regions
Neck
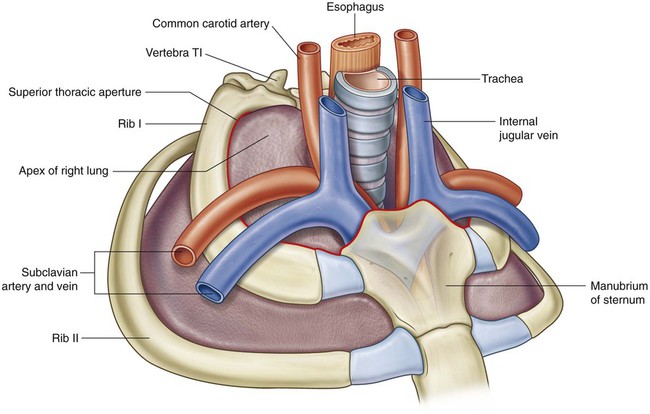
The superior thoracic aperture opens directly into the root of the neck (Fig. 3.7).
Upper limb
An axillary inlet, or gateway to the upper limb, lies on each side of the superior thoracic aperture. These two axillary inlets and the superior thoracic aperture communicate superiorly with the root of the neck (Fig. 3.7).
Each axillary inlet is formed by:
The base of the axillary inlet’s triangular opening is the lateral margin of rib I.
Abdomen
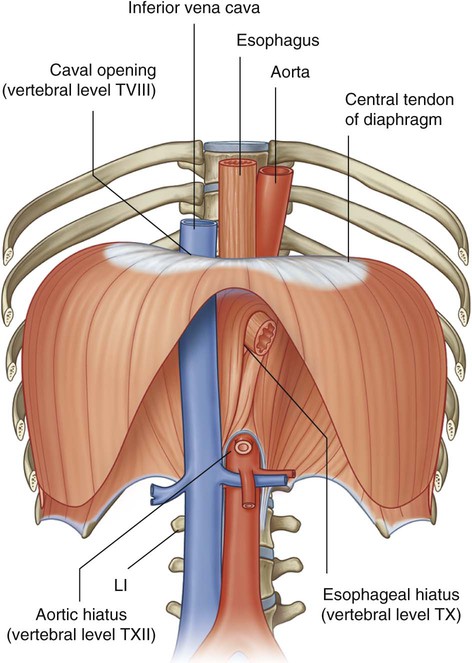
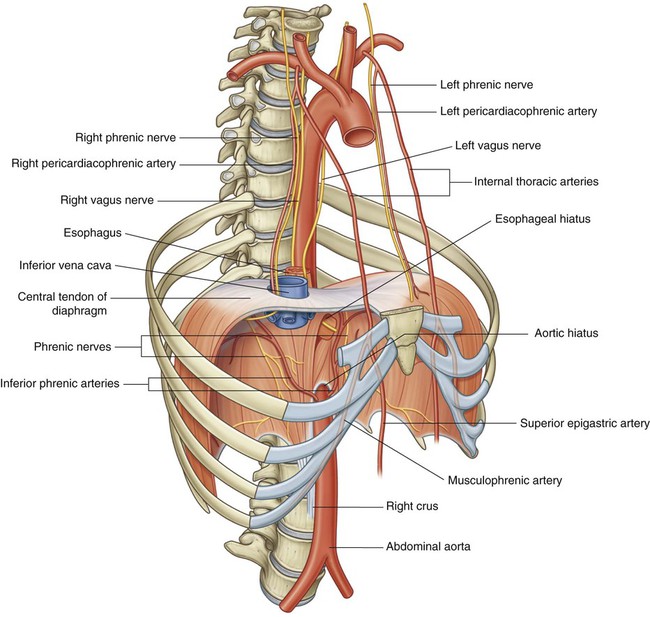
The diaphragm separates the thorax from the abdomen. Structures that pass between the thorax and abdomen either penetrate the diaphragm or pass posteriorly to it (Fig. 3.8):
 The inferior vena cava pierces the central tendon of the diaphragm to enter the right side of the mediastinum near vertebral level TVIII.
The inferior vena cava pierces the central tendon of the diaphragm to enter the right side of the mediastinum near vertebral level TVIII.
 The esophagus penetrates the muscular part of the diaphragm to leave the mediastinum and enter the abdomen just to the left of the midline at vertebral level TX.
The esophagus penetrates the muscular part of the diaphragm to leave the mediastinum and enter the abdomen just to the left of the midline at vertebral level TX.
 The aorta passes posteriorly to the diaphragm at the midline at vertebral level TXII.
The aorta passes posteriorly to the diaphragm at the midline at vertebral level TXII.
 Numerous other structures that pass between the thorax and abdomen pass through or posterior to the diaphragm.
Numerous other structures that pass between the thorax and abdomen pass through or posterior to the diaphragm.
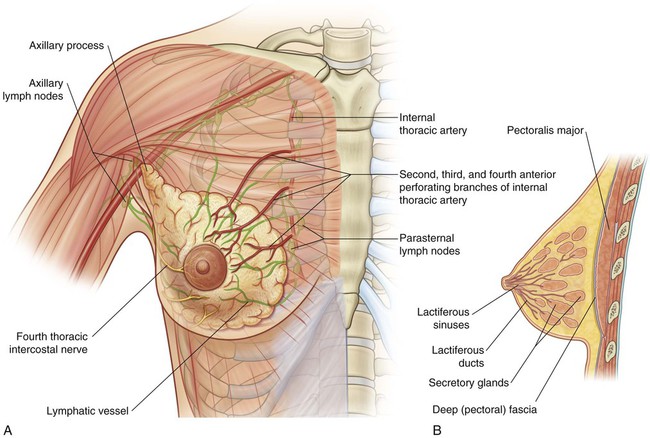
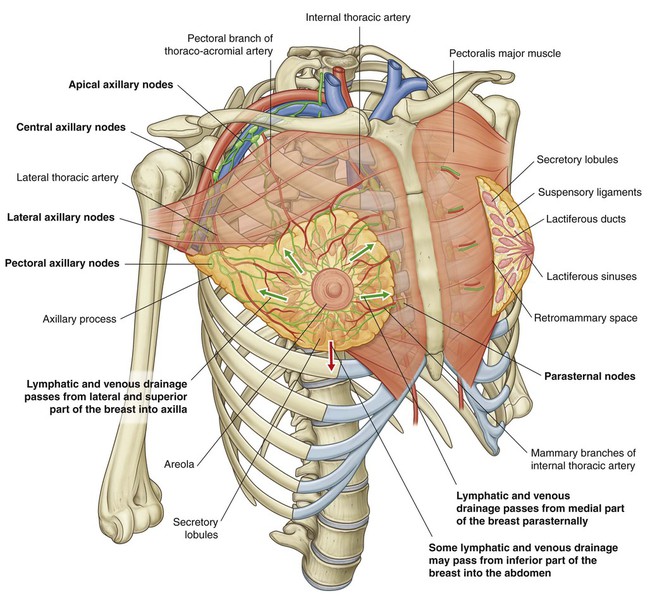
Breast
The breasts, consisting of secretory glands, superficial fascia, and overlying skin, are in the pectoral region on each side of the anterior thoracic wall (Fig. 3.9).
Vessels, lymphatics, and nerves associated with the breast are as follows:
 Branches from the internal thoracic arteries and veins perforate the anterior chest wall on each side of the sternum to supply anterior aspects of the thoracic wall. Those branches associated mainly with the second to fourth intercostal spaces also supply the anteromedial parts of each breast.
Branches from the internal thoracic arteries and veins perforate the anterior chest wall on each side of the sternum to supply anterior aspects of the thoracic wall. Those branches associated mainly with the second to fourth intercostal spaces also supply the anteromedial parts of each breast.
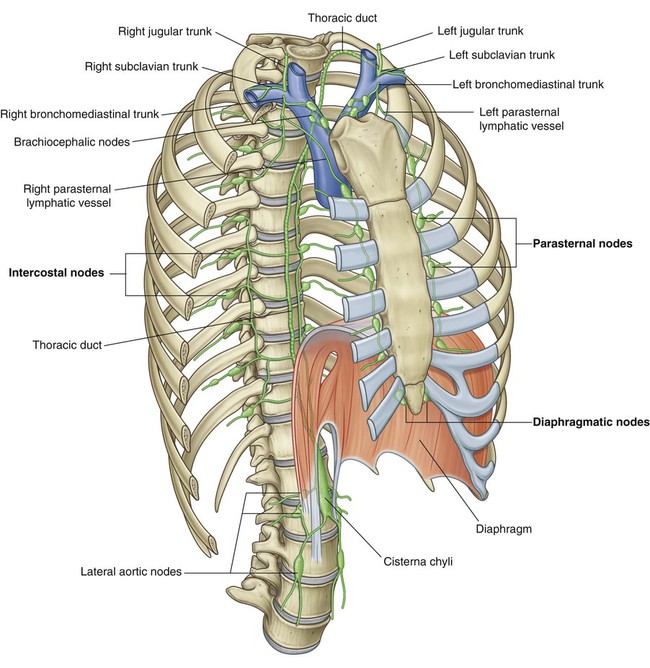
 Lymphatic vessels from the medial part of the breast accompany the perforating arteries and drain into the parasternal nodes on the deep surface of the thoracic wall.
Lymphatic vessels from the medial part of the breast accompany the perforating arteries and drain into the parasternal nodes on the deep surface of the thoracic wall.
 Vessels and lymphatics associated with lateral parts of the breast emerge from or drain into the axillary region of the upper limb.
Vessels and lymphatics associated with lateral parts of the breast emerge from or drain into the axillary region of the upper limb.
 Lateral and anterior branches of the fourth to sixth intercostal nerves carry general sensation from the skin of the breast.
Lateral and anterior branches of the fourth to sixth intercostal nerves carry general sensation from the skin of the breast.
Key features
Vertebral level TIV/V
The horizontal plane passing through the disc that separates thoracic vertebrae TIV and TV is one of the most significant planes in the body (Fig. 3.10) because it:
 passes through the sternal angle anteriorly, marking the position of the anterior articulation of the costal cartilage of rib II with the sternum. The sternal angle is used to find the position of rib II as a reference for counting ribs (because of the overlying clavicle, rib I is not palpable);
passes through the sternal angle anteriorly, marking the position of the anterior articulation of the costal cartilage of rib II with the sternum. The sternal angle is used to find the position of rib II as a reference for counting ribs (because of the overlying clavicle, rib I is not palpable);
 separates the superior mediastinum from the inferior mediastinum and marks the position of the superior limit of the pericardium;
separates the superior mediastinum from the inferior mediastinum and marks the position of the superior limit of the pericardium;
 marks where the arch of the aorta begins and ends;
marks where the arch of the aorta begins and ends;
 passes through the site where the superior vena cava penetrates the pericardium to enter the heart;
passes through the site where the superior vena cava penetrates the pericardium to enter the heart;
 is the level at which the trachea bifurcates into right and left main bronchi; and
is the level at which the trachea bifurcates into right and left main bronchi; and
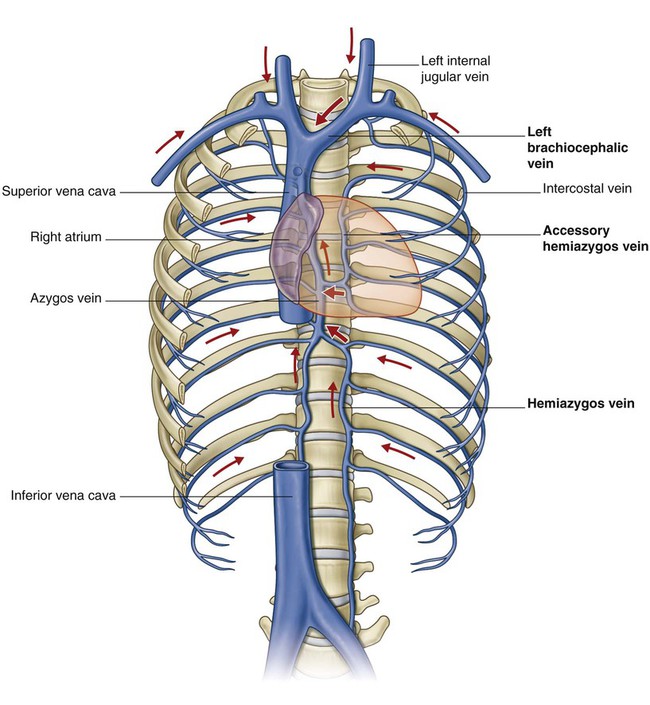
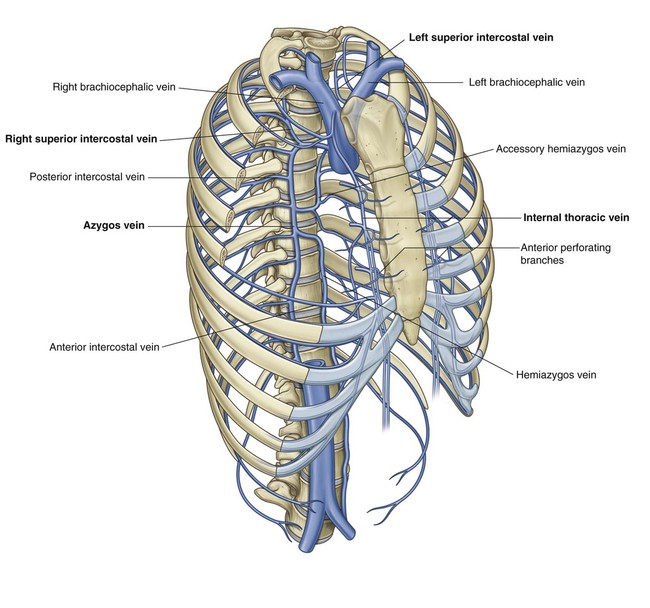
Venous shunts from left to right
The right atrium is the chamber of the heart that receives deoxygenated blood returning from the body. It lies on the right side of the midline, and the two major veins, the superior and inferior venae cavae, that drain into it are also located on the right side of the body. This means that, to get to the right side of the body, all blood coming from the left side has to cross the midline. This left-to-right shunting is carried out by a number of important and, in some cases, very large veins, several of which are in the thorax (Fig. 3.11).
Segmental neurovascular supply of thoracic wall
 the thoracic aorta, which is in the posterior mediastinum, and
the thoracic aorta, which is in the posterior mediastinum, and
 a pair of vessels, the internal thoracic arteries, which run along the deep aspect of the anterior thoracic wall on either side of the sternum.
a pair of vessels, the internal thoracic arteries, which run along the deep aspect of the anterior thoracic wall on either side of the sternum.
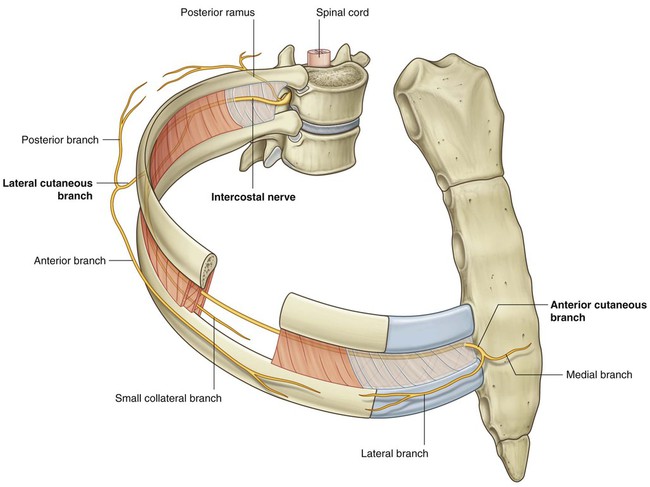
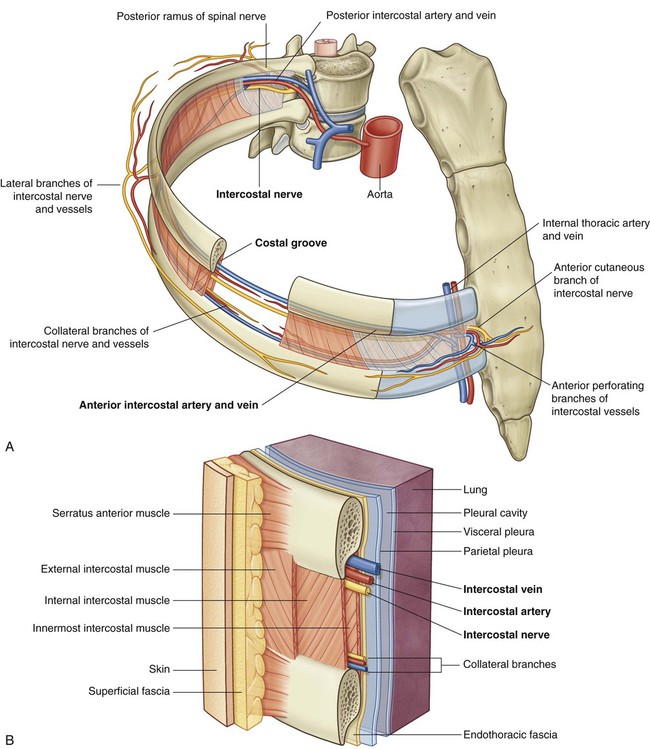
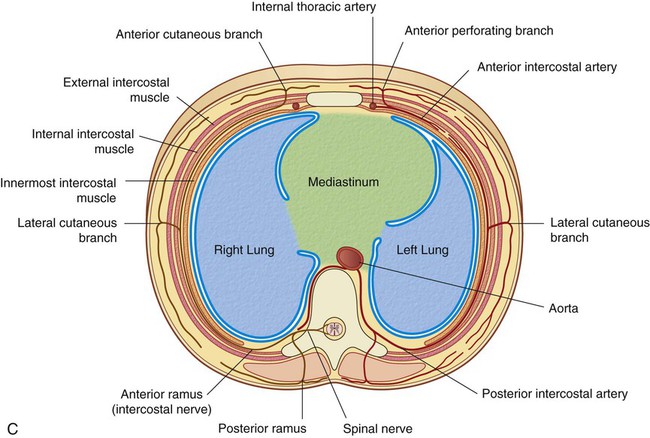
Posterior and anterior intercostal vessels branch segmentally from these arteries and pass laterally around the wall, mainly along the inferior margin of each rib (Fig. 3.12A). Running with these vessels are intercostal nerves (the anterior rami of thoracic spinal nerves), which innervate the wall, related parietal pleura, and associated skin. The position of these nerves and vessels relative to the ribs must be considered when passing objects, such as chest tubes, through the thoracic wall.
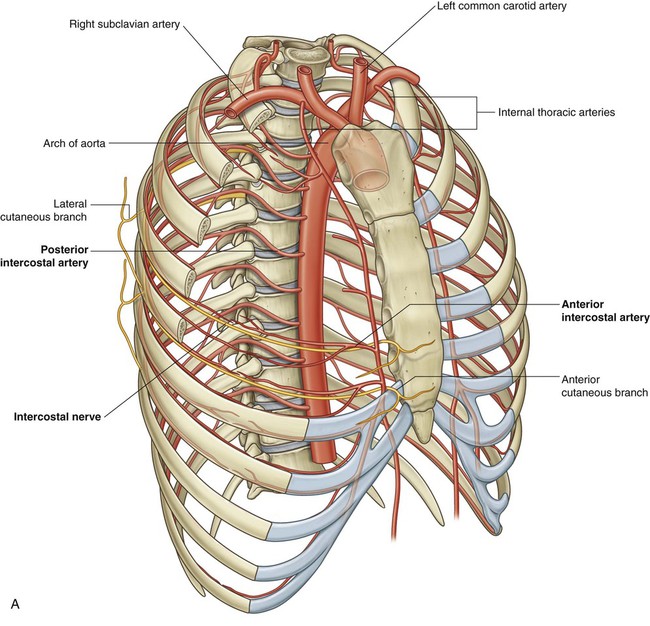
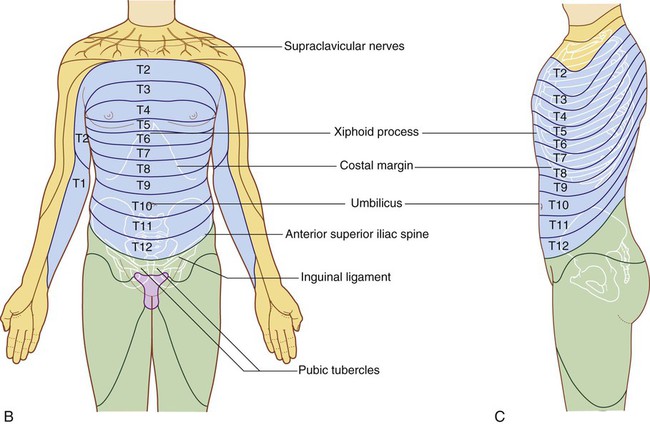
Dermatomes of the thorax generally reflect the segmental organization of the thoracic spinal nerves (Fig. 3.12B). The exception occurs, anteriorly and superiorly, with the first thoracic dermatome, which is located mostly in the upper limb, and not on the trunk.
Dermatomes of T7 to T12 follow the contour of the ribs onto the anterior abdominal wall (Fig. 3.12C).
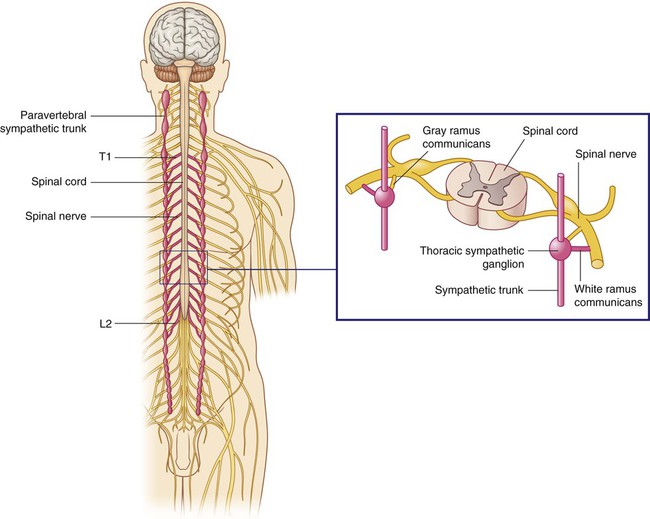
Sympathetic system
All preganglionic nerve fibers of the sympathetic system are carried out of the spinal cord in spinal nerves T1 to L2 (Fig. 3.13). This means that sympathetic fibers found anywhere in the body ultimately emerge from the spinal cord as components of these spinal nerves. Preganglionic sympathetic fibers destined for the head are carried out of the spinal cord in spinal nerve T1.
Regional anatomy
The cylindrical thorax consists of:
Pectoral region
 a superficial compartment containing skin, superficial fascia, and breasts; and
a superficial compartment containing skin, superficial fascia, and breasts; and
 a deep compartment containing muscles and associated structures.
a deep compartment containing muscles and associated structures.
Breast
The breasts consist of mammary glands and associated skin and connective tissues. The mammary glands are modified sweat glands in the superficial fascia anterior to the pectoral muscles and the anterior thoracic wall (Fig. 3.16).
Lymphatic drainage
Lymphatic drainage of the breast is as follows:
 Approximately 75% is via lymphatic vessels that drain laterally and superiorly into axillary nodes (Fig. 3.16).
Approximately 75% is via lymphatic vessels that drain laterally and superiorly into axillary nodes (Fig. 3.16).
 Most of the remaining drainage is into parasternal nodes deep to the anterior thoracic wall and associated with the internal thoracic artery.
Most of the remaining drainage is into parasternal nodes deep to the anterior thoracic wall and associated with the internal thoracic artery.
 Some drainage may occur via lymphatic vessels that follow the lateral branches of posterior intercostal arteries and connect with intercostal nodes situated near the heads and necks of ribs.
Some drainage may occur via lymphatic vessels that follow the lateral branches of posterior intercostal arteries and connect with intercostal nodes situated near the heads and necks of ribs.
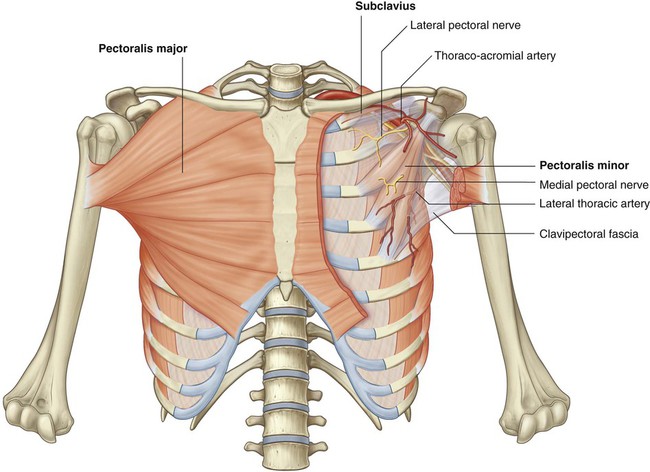
Muscles of the pectoral region
Each pectoral region contains the pectoralis major, pectoralis minor, and subclavius muscles (Fig. 3.17 and Table 3.1). All originate from the anterior thoracic wall and insert into bones of the upper limb.
Table 3.1
Muscles of the pectoral region
| Muscle | Origin | Insertion | Innervation | Function |
| Pectoralis major | Medial half of clavicle and anterior surface of sternum, first seven costal cartilages, aponeurosis of external oblique | Lateral lip of intertubercular sulcus of humerus | Medial and lateral pectoral nerves | Adduction, medial rotation, and flexion of the humerus at the shoulder joint |
| Subclavius | Rib I at junction between rib and costal cartilage | Groove on inferior surface of middle third of clavicle | Nerve to subclavius | Pulls clavicle medially to stabilize sternoclavicular joint; depresses tip of shoulder |
| Pectoralis minor | Anterior surfaces of the third, fourth, and fifth ribs, and deep fascia overlying the related intercostal spaces | Coracoid process of scapula | Medial pectoral nerves | Depresses tip of shoulder; protracts scapula |
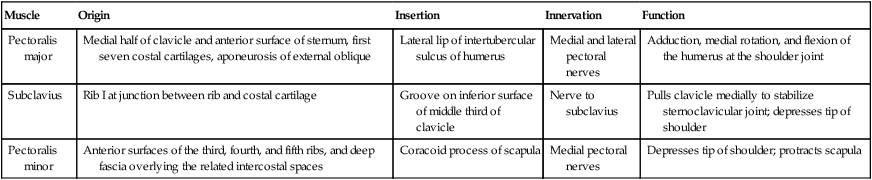
Subclavius and pectoralis minor muscles
The subclavius and pectoralis minor muscles underlie the pectoralis major:
 The subclavius is small and passes laterally from the anterior and medial part of rib I to the inferior surface of the clavicle.
The subclavius is small and passes laterally from the anterior and medial part of rib I to the inferior surface of the clavicle.
 The pectoralis minor passes from the anterior surfaces of ribs III to V to the coracoid process of the scapula.
The pectoralis minor passes from the anterior surfaces of ribs III to V to the coracoid process of the scapula.
Both the subclavius and pectoralis minor pull the tip of the shoulder inferiorly.
Thoracic wall
 the superior thoracic aperture, bordered by vertebra TI, rib I, and the manubrium of the sternum; and
the superior thoracic aperture, bordered by vertebra TI, rib I, and the manubrium of the sternum; and
 the inferior thoracic aperture, bordered by vertebra TXII, rib XII, the end of rib XI, the costal margin, and the xiphoid process of the sternum.
the inferior thoracic aperture, bordered by vertebra TXII, rib XII, the end of rib XI, the costal margin, and the xiphoid process of the sternum.
Skeletal framework
Thoracic vertebrae
There are twelve thoracic vertebrae, each of which is characterized by articulations with ribs.
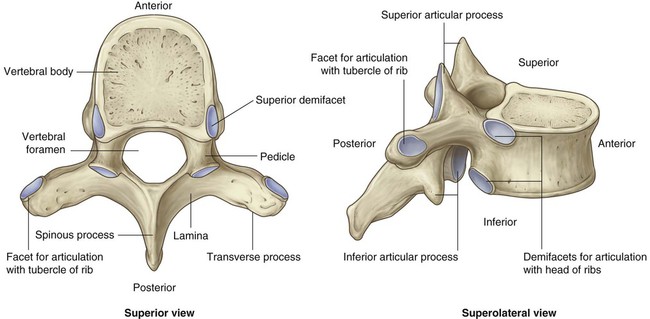
Typical thoracic vertebra
A typical thoracic vertebra has a heart-shaped vertebral body, with roughly equal dimensions in the transverse and anteroposterior directions, and a long spinous process (Fig. 3.18). The vertebral foramen is generally circular and the laminae are broad and overlap with those of the vertebra below. The superior articular processes are flat, with their articular surfaces facing almost directly posteriorly, while the inferior articular processes project from the laminae and their articular facets face anteriorly. The transverse processes are club shaped and project posterolaterally.
Articulation with ribs
A typical thoracic vertebra has three sites on each side for articulation with ribs.
 Two demifacets (i.e., partial facets) are located on the superior and inferior aspects of the body for articulation with corresponding sites on the heads of adjacent ribs. The superior costal facet articulates with part of the head of its own rib, and the inferior costal facet articulates with part of the head of the rib below.
Two demifacets (i.e., partial facets) are located on the superior and inferior aspects of the body for articulation with corresponding sites on the heads of adjacent ribs. The superior costal facet articulates with part of the head of its own rib, and the inferior costal facet articulates with part of the head of the rib below.
 An oval facet (transverse costal facet) at the end of the transverse process articulates with the tubercle of its own rib.
An oval facet (transverse costal facet) at the end of the transverse process articulates with the tubercle of its own rib.
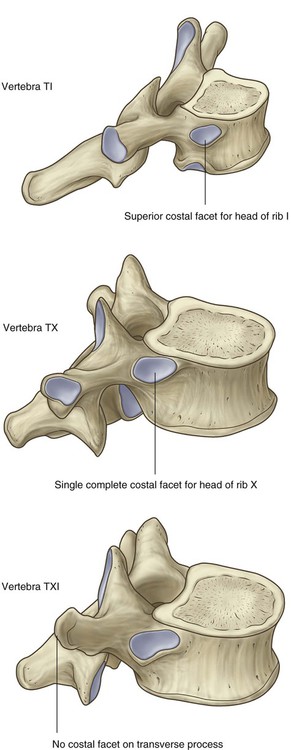
Not all vertebrae articulate with ribs in the same fashion (Fig. 3.19):
 The superior costal facets on the body of vertebra TI are complete and articulate with a single facet on the head of its own rib—in other words, the head of rib I does not articulate with vertebra CVII.
The superior costal facets on the body of vertebra TI are complete and articulate with a single facet on the head of its own rib—in other words, the head of rib I does not articulate with vertebra CVII.
 Similarly, vertebra TX (and often TIX) articulates only with its own ribs and therefore lacks inferior demifacets on the body.
Similarly, vertebra TX (and often TIX) articulates only with its own ribs and therefore lacks inferior demifacets on the body.
 Vertebrae TXI and TXII articulate only with the heads of their own ribs—they lack transverse costal facets and have only a single complete facet on each side of their bodies.
Vertebrae TXI and TXII articulate only with the heads of their own ribs—they lack transverse costal facets and have only a single complete facet on each side of their bodies.
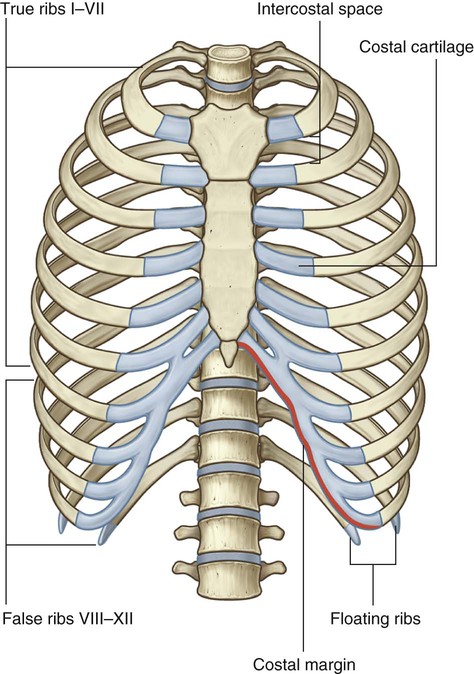
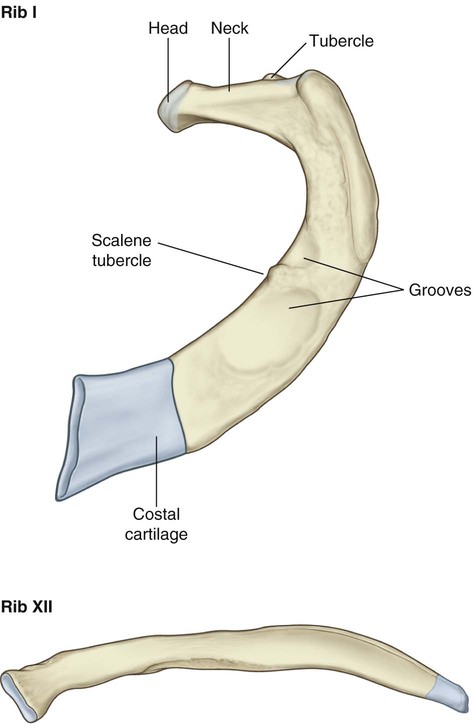
Ribs
There are twelve pairs of ribs, each terminating anteriorly in a costal cartilage (Fig. 3.20).
 The costal cartilages of ribs VIII to X articulate anteriorly with the costal cartilages of the ribs above.
The costal cartilages of ribs VIII to X articulate anteriorly with the costal cartilages of the ribs above.
 Ribs XI and XII have no anterior connection with other ribs or with the sternum and are often called floating ribs.
Ribs XI and XII have no anterior connection with other ribs or with the sternum and are often called floating ribs.
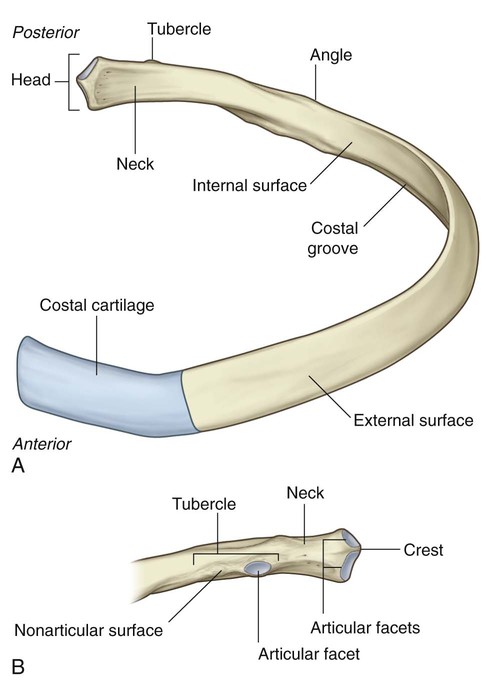
A typical rib consists of a curved shaft with anterior and posterior ends (Fig. 3.21). The anterior end is continuous with its costal cartilage. The posterior end articulates with the vertebral column and is characterized by a head, neck, and tubercle.
The neck is a short flat region of bone that separates the head from the tubercle.
 The articular part is medial and has an oval facet for articulation with a corresponding facet on the transverse process of the associated vertebra.
The articular part is medial and has an oval facet for articulation with a corresponding facet on the transverse process of the associated vertebra.
 The raised nonarticular part is roughened by ligament attachments.
The raised nonarticular part is roughened by ligament attachments.
The shaft is generally thin and flat with internal and external surfaces.
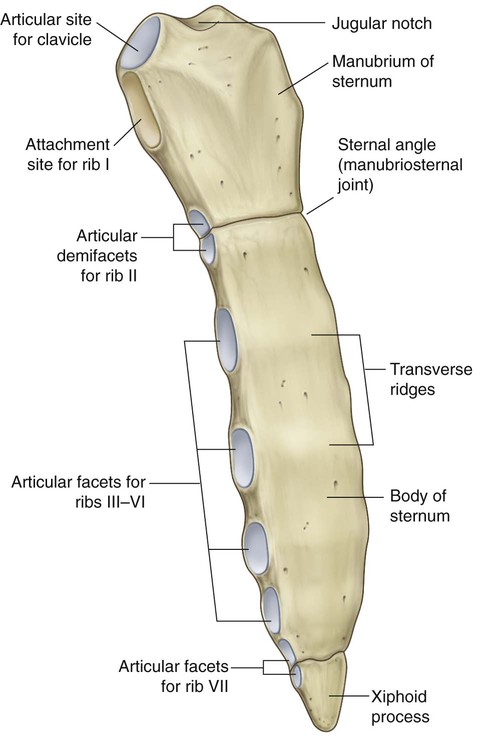
Sternum
The adult sternum consists of three major elements: the broad and superiorly positioned manubrium of the sternum, the narrow and longitudinally oriented body of the sternum, and the small and inferiorly positioned xiphoid process (Fig. 3.23).
Joints
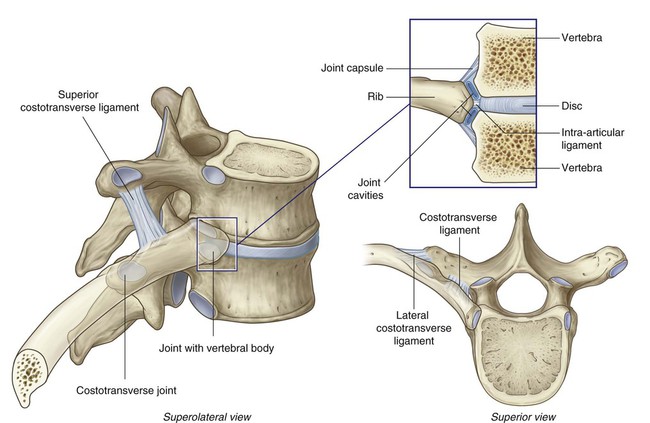
Costovertebral joints
A typical rib articulates with:
 the bodies of adjacent vertebrae, forming a joint with the head of the rib; and
the bodies of adjacent vertebrae, forming a joint with the head of the rib; and
 the transverse process of its related vertebra, forming a costotransverse joint (Fig. 3.24).
the transverse process of its related vertebra, forming a costotransverse joint (Fig. 3.24).
Costotransverse joints are synovial joints between the tubercle of a rib and the transverse process of the related vertebra (Fig. 3.24). The capsule surrounding each joint is thin. The joint is stabilized by two strong extracapsular ligaments that span the space between the transverse process and the rib on the medial and lateral sides of the joint:
 The costotransverse ligament is medial to the joint and attaches the neck of the rib to the transverse process.
The costotransverse ligament is medial to the joint and attaches the neck of the rib to the transverse process.
 The lateral costotransverse ligament is lateral to the joint and attaches the tip of the transverse process to the roughened nonarticular part of the tubercle of the rib.
The lateral costotransverse ligament is lateral to the joint and attaches the tip of the transverse process to the roughened nonarticular part of the tubercle of the rib.
Slight gliding movements occur at the costotransverse joints.
Manubriosternal and xiphisternal joints
The joints between the manubrium and the body of the sternum and between the body of the sternum and the xiphoid process are usually symphyses (Fig. 3.25). Only slight angular movements occur between the manubrium and the body of the sternum during respiration. The joint between the body of the sternum and the xiphoid process often becomes ossified with age.
In addition, the sternal angle lies on a horizontal plane that passes through the intervertebral disc between vertebrae TIV and TV (see Fig. 3.10). This plane separates the superior mediastinum from the inferior mediastinum and marks the superior border of the pericardium. The plane also passes through the end of the ascending aorta and the beginning of the arch of the aorta, the end of the arch of the aorta and the beginning of the thoracic aorta, and the bifurcation of the trachea, and just superior to the pulmonary trunk (see Fig. 3.79 and 3.86).
Intercostal spaces
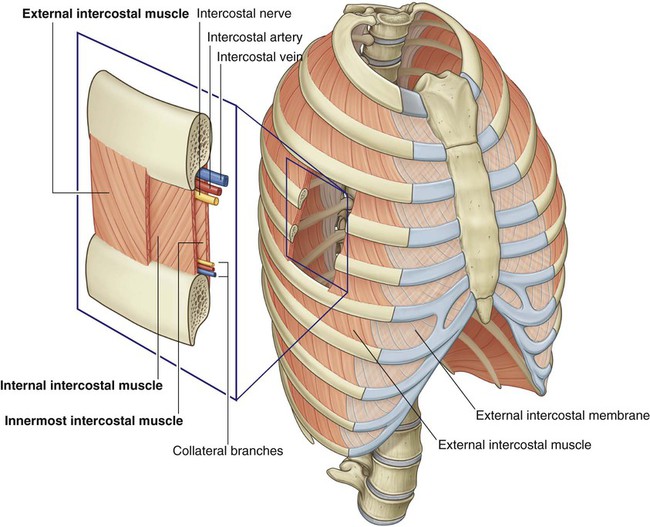
Intercostal spaces lie between adjacent ribs and are filled by intercostal muscles (Fig. 3.26).
Muscles
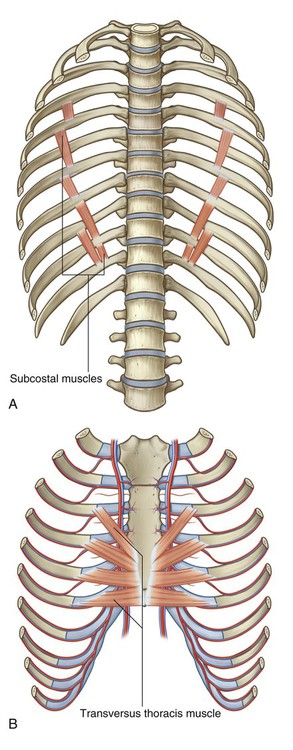
Muscles of the thoracic wall include those that fill and support the intercostal spaces, those that pass between the sternum and the ribs, and those that cross several ribs between costal attachments (Table 3.2).
Table 3.2
| Muscle | Superior attachment | Inferior attachment | Innervation | Function |
| External intercostal | Inferior margin of rib above | Superior margin of rib below | Intercostal nerves; T1–T11 | Most active during inspiration; supports intercostal space; moves ribs superiorly |
| Internal intercostal | Lateral edge of costal groove of rib above | Superior margin of rib below deep to the attachment of the related external intercostal | Intercostal nerves; T1–T11 | Most active during expiration; supports intercostal space; moves ribs inferiorly |
| Innermost intercostal | Medial edge of costal groove of rib above | Internal aspect of superior margin of rib below | Intercostal nerves; T1–T11 | Acts with internal intercostal muscles |
| Subcostales | Internal surface (near angle) of lower ribs | Internal surface of second or third rib below | Related intercostal nerves | May depress ribs |
| Transversus thoracis | Inferior margins and internal surfaces of costal cartilages of second to sixth ribs | Inferior aspect of deep surface of body of sternum, xiphoid process, and costal cartilages of ribs IV–VII | Related intercostal nerves | Depresses costal cartilages |
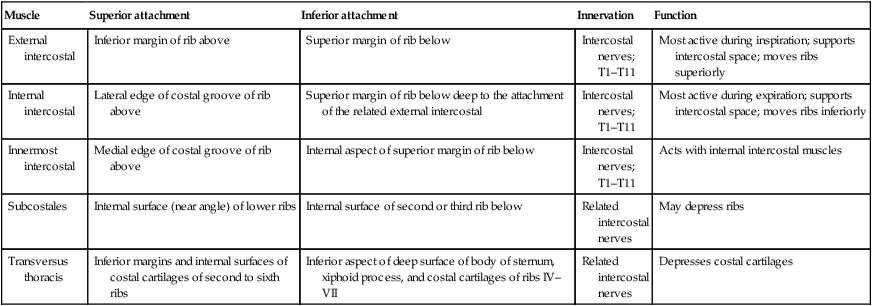
Intercostal muscles
The intercostal muscles are three flat muscles found in each intercostal space that pass between adjacent ribs (Fig. 3.27). Individual muscles in this group are named according to their positions:
 The external intercostal muscles are the most superficial.
The external intercostal muscles are the most superficial.
 The internal intercostal muscles are sandwiched between the external and innermost muscles.
The internal intercostal muscles are sandwiched between the external and innermost muscles.
 The innermost intercostal muscles are the deepest of the three muscles.
The innermost intercostal muscles are the deepest of the three muscles.
The eleven pairs of external intercostal muscles extend from the inferior margins (lateral edges of costal grooves) of the ribs above to the superior margins of the ribs below. When the thoracic wall is viewed from a lateral position, the muscle fibers pass obliquely anteroinferiorly (Fig. 3.27). The muscles extend around the thoracic wall from the regions of the tubercles of the ribs to the costal cartilages, where each layer continues as a thin connective tissue aponeurosis termed the external intercostal membrane. The external intercostal muscles are most active in inspiration.
The eleven pairs of internal intercostal muscles pass between the most inferior lateral edge of the costal grooves of the ribs above, to the superior margins of the ribs below. They extend from parasternal regions, where the muscles course between adjacent costal cartilages, to the angle of the ribs posteriorly (Fig. 3.27). This layer continues medially toward the vertebral column, in each intercostal space, as the internal intercostal membrane. The muscle fibers pass in the opposite direction to those of the external intercostal muscles. When the thoracic wall is viewed from a lateral position, the muscle fibers pass obliquely posteroinferiorly. The internal intercostal muscles are most active during expiration.
The innermost intercostal muscles are the least distinct of the intercostal muscles, and the fibers have the same orientation as the internal intercostals (Fig. 3.27). These muscles are most evident in the lateral thoracic wall. They extend between the inner surfaces of adjacent ribs from the medial edge of the costal groove to the deep surface of the rib below. Importantly, the neurovascular bundles associated with the intercostal spaces pass around the thoracic wall in the costal grooves in a plane between the innermost and internal intercostal muscles.
The subcostales are in the same plane as the innermost intercostals, span multiple ribs, and are more numerous in lower regions of the posterior thoracic wall (Fig. 3.28A). They extend from the internal surfaces of one rib to the internal surface of the second (next) or third rib below. Their fibers parallel the course of the internal intercostal muscles and extend from the angle of the ribs to more medial positions on the ribs below.
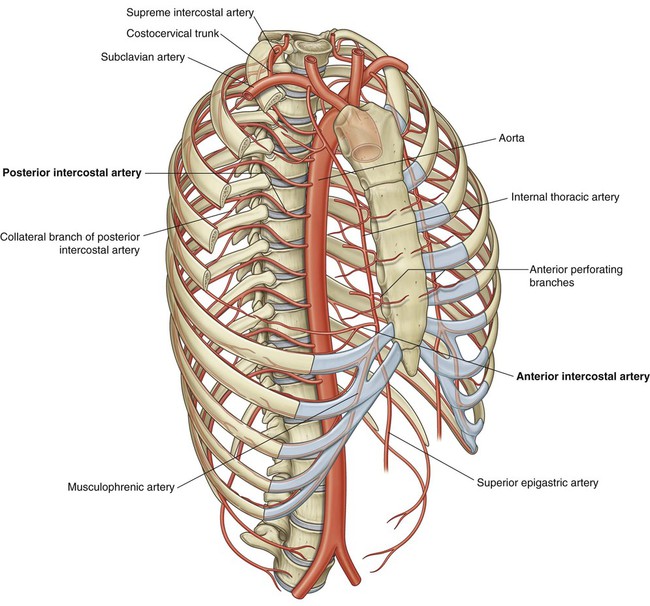
Arterial supply
Vessels that supply the thoracic wall consist mainly of posterior and anterior intercostal arteries, which pass around the wall between adjacent ribs in intercostal spaces (Fig. 3.29). These arteries originate from the aorta and internal thoracic arteries, which in turn arise from the subclavian arteries in the root of the neck. Together, the intercostal arteries form a basket-like pattern of vascular supply around the thoracic wall.
Posterior intercostal arteries
Posterior intercostal arteries originate from vessels associated with the posterior thoracic wall. The upper two posterior intercostal arteries on each side are derived from the supreme intercostal artery, which descends into the thorax as a branch of the costocervical trunk in the neck. The costocervical trunk is a posterior branch of the subclavian artery (Fig. 3.29).
Anterior intercostal arteries
The anterior intercostal arteries originate directly or indirectly as lateral branches from the internal thoracic arteries (Fig. 3.29).
 the superior epigastric artery, which continues inferiorly into the anterior abdominal wall (Fig. 3.29);
the superior epigastric artery, which continues inferiorly into the anterior abdominal wall (Fig. 3.29);
 the musculophrenic artery, which passes along the costal margin, goes through the diaphragm, and ends near the last intercostal space.
the musculophrenic artery, which passes along the costal margin, goes through the diaphragm, and ends near the last intercostal space.
In each intercostal space, the anterior intercostal arteries usually have two branches:
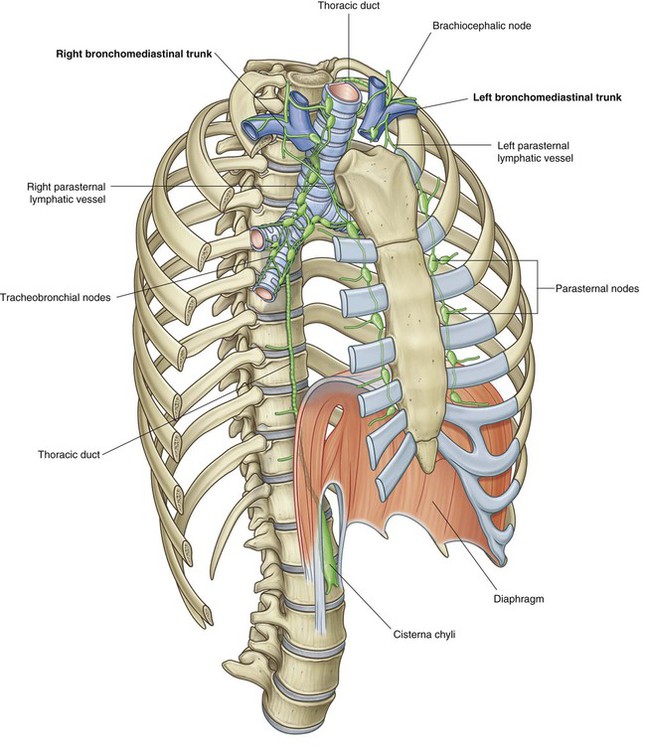
Lymphatic drainage
Lymphatic vessels of the thoracic wall drain mainly into lymph nodes associated with the internal thoracic arteries (parasternal nodes), with the heads and necks of ribs (intercostal nodes), and with the diaphragm (diaphragmatic nodes) (Fig. 3.31). Diaphragmatic nodes are posterior to the xiphoid and at sites where the phrenic nerves penetrate the diaphragm. They also occur in regions where the diaphragm is attached to the vertebral column.
Innervation
Intercostal nerves
Innervation of the thoracic wall is mainly by the intercostal nerves, which are the anterior rami of spinal nerves T1 to T11 and lie in the intercostal spaces between adjacent ribs. The anterior ramus of spinal nerve T12 (the subcostal nerve) is inferior to rib XII (Fig. 3.32).
In the thorax, the intercostal nerves carry:
 somatic motor innervation to the muscles of the thoracic wall (intercostal, subcostal, and transversus thoracis muscles),
somatic motor innervation to the muscles of the thoracic wall (intercostal, subcostal, and transversus thoracis muscles),
 somatic sensory innervation from the skin and parietal pleura, and
somatic sensory innervation from the skin and parietal pleura, and
In addition to innervating the thoracic wall, intercostal nerves innervate other regions:
 The anterior ramus of T1 contributes to the brachial plexus.
The anterior ramus of T1 contributes to the brachial plexus.
 The lateral cutaneous branch of the second intercostal nerve (the intercostobrachial nerve) contributes to cutaneous innervation of the medial surface of the upper arm.
The lateral cutaneous branch of the second intercostal nerve (the intercostobrachial nerve) contributes to cutaneous innervation of the medial surface of the upper arm.
 The lower intercostal nerves supply the muscles, skin, and peritoneum of the abdominal wall.
The lower intercostal nerves supply the muscles, skin, and peritoneum of the abdominal wall.
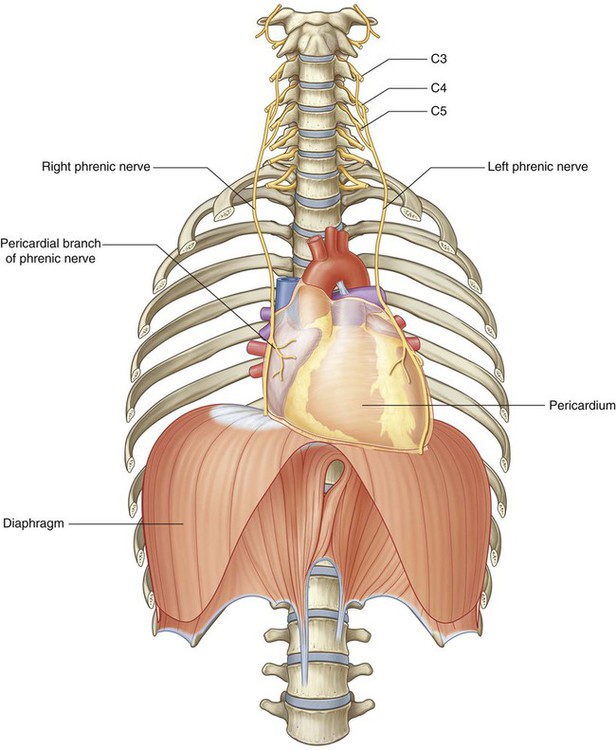
Diaphragm
The diaphragm is a thin musculotendinous structure that fills the inferior thoracic aperture and separates the thoracic cavity from the abdominal cavity (Fig. 3.33 and see Chapter 4). It is attached peripherally to the:
 xiphoid process of the sternum,
xiphoid process of the sternum,
 costal margin of the thoracic wall,
costal margin of the thoracic wall,
 ligaments that span across structures of the posterior abdominal wall, and
ligaments that span across structures of the posterior abdominal wall, and
 The inferior vena cava passes through the central tendon at approximately vertebral level TVIII.
The inferior vena cava passes through the central tendon at approximately vertebral level TVIII.
 The esophagus passes through the muscular part of the diaphragm, just to the left of midline, approximately at vertebral level TX.
The esophagus passes through the muscular part of the diaphragm, just to the left of midline, approximately at vertebral level TX.
 The vagus nerves pass through the diaphragm with the esophagus.
The vagus nerves pass through the diaphragm with the esophagus.
 The aorta passes behind the posterior attachment of the diaphragm at vertebral level TXII.
The aorta passes behind the posterior attachment of the diaphragm at vertebral level TXII.
 The thoracic duct passes behind the diaphragm with the aorta.
The thoracic duct passes behind the diaphragm with the aorta.
 The azygos and hemiazygos veins may also pass through the aortic hiatus or through the crura of the diaphragm.
The azygos and hemiazygos veins may also pass through the aortic hiatus or through the crura of the diaphragm.
Arterial supply
The arterial supply to the diaphragm is from vessels that arise superiorly and inferiorly to it (see Fig. 3.33). From above, pericardiacophrenic and musculophrenic arteries supply the diaphragm. These vessels are branches of the internal thoracic arteries. Superior phrenic arteries, which arise directly from lower parts of the thoracic aorta, and small branches from intercostal arteries contribute to the supply. The largest arteries supplying the diaphragm arise from below it. These arteries are the inferior phrenic arteries, which branch directly from the abdominal aorta.
Movements of the thoracic wall and diaphragm during breathing
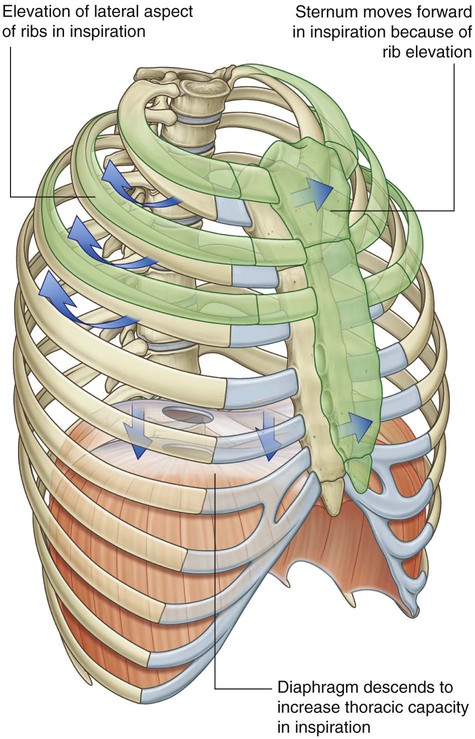
Changes in the anteroposterior and lateral dimensions result from elevation and depression of the ribs (Fig. 3.34). The posterior ends of the ribs articulate with the vertebral column, whereas the anterior ends of most ribs articulate with the sternum or adjacent ribs.
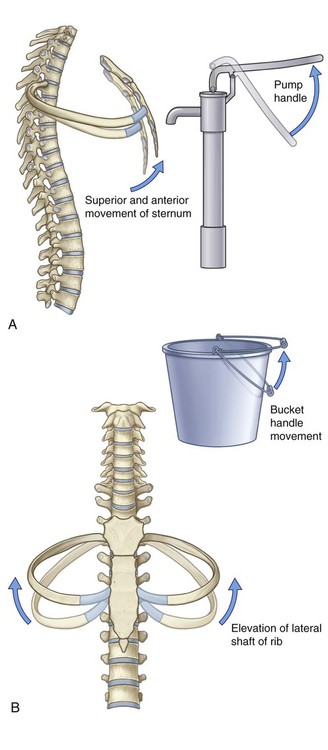
Because the anterior ends of the ribs are inferior to the posterior ends, when the ribs are elevated, they move the sternum upward and forward. Also, the angle between the body of the sternum and the manubrium may become slightly less acute. When the ribs are depressed, the sternum moves downward and backward. This “pump handle” movement changes the dimensions of the thorax in the anteroposterior direction (Fig. 3.34A).
As well as the anterior ends of the ribs being lower than the posterior ends, the middles of the shafts tend to be lower than the two ends. When the shafts are elevated, the middles of the shafts move laterally. This “bucket handle” movement increases the lateral dimensions of the thorax (Fig. 3.34B).
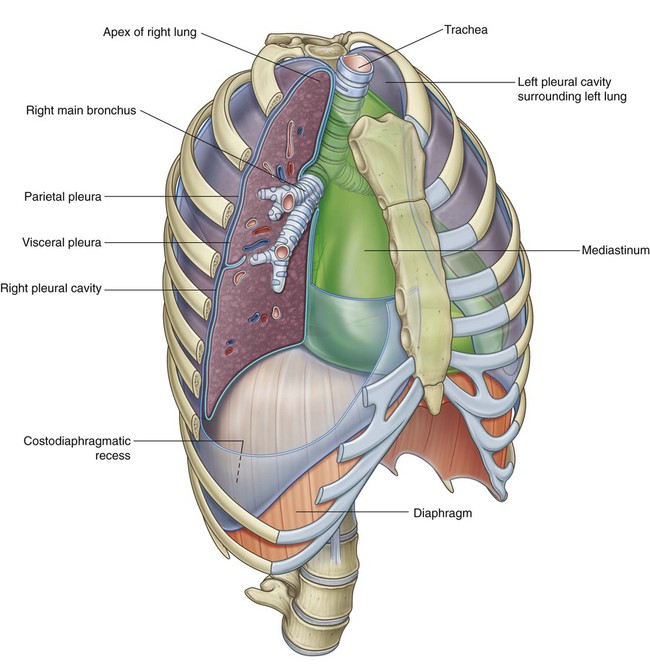
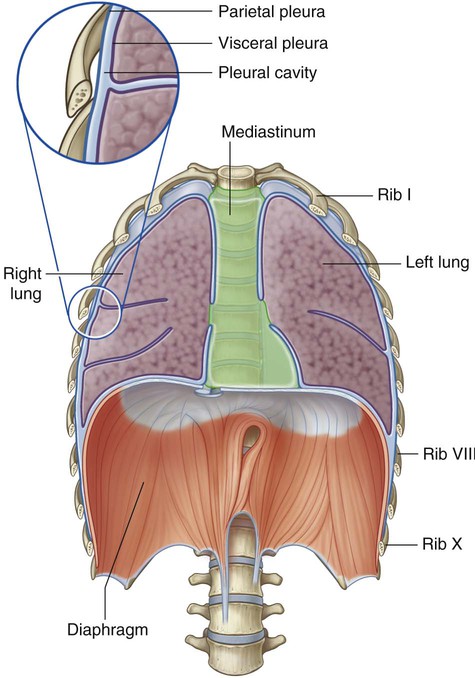
Pleural cavities
Two pleural cavities, one on either side of the mediastinum, surround the lungs (Fig. 3.35):
 Superiorly, they extend above rib I into the root of the neck.
Superiorly, they extend above rib I into the root of the neck.
 Inferiorly, they extend to a level just above the costal margin.
Inferiorly, they extend to a level just above the costal margin.
Pleura
The pleura is divided into two major types, based on location:
 Pleura associated with the walls of a pleural cavity is parietal pleura (Fig. 3.35).
Pleura associated with the walls of a pleural cavity is parietal pleura (Fig. 3.35).
 Pleura that reflects from the medial wall and onto the surface of the lung is visceral pleura (Fig. 3.35), which adheres to and covers the lung.
Pleura that reflects from the medial wall and onto the surface of the lung is visceral pleura (Fig. 3.35), which adheres to and covers the lung.
Parietal pleura
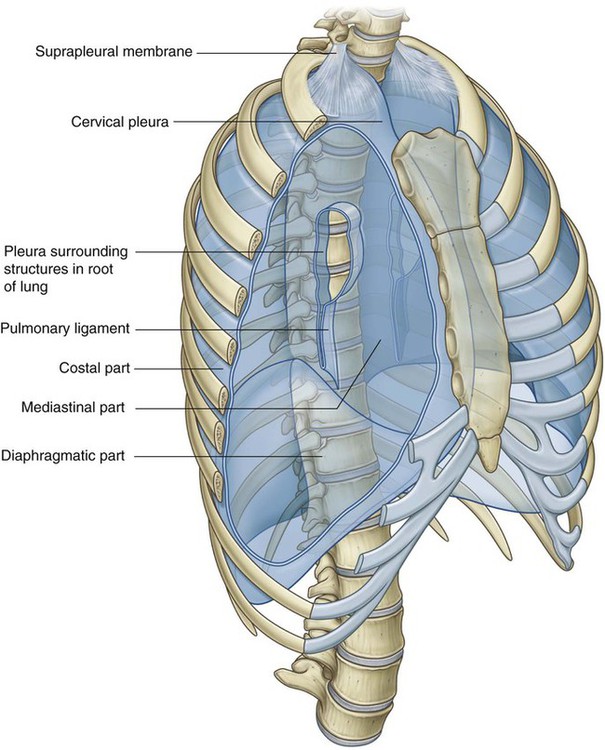
The names given to the parietal pleura correspond to the parts of the wall with which they are associated (Fig. 3.36):
 Pleura related to the ribs and intercostal spaces is termed the costal part.
Pleura related to the ribs and intercostal spaces is termed the costal part.
 Pleura covering the diaphragm is the diaphragmatic part.
Pleura covering the diaphragm is the diaphragmatic part.
 Pleura covering the mediastinum is the mediastinal part.
Pleura covering the mediastinum is the mediastinal part.
 The dome-shaped layer of parietal pleura lining the cervical extension of the pleural cavity is cervical pleura (dome of pleura or pleural cupola).
The dome-shaped layer of parietal pleura lining the cervical extension of the pleural cavity is cervical pleura (dome of pleura or pleural cupola).
Covering the superior surface of the cervical pleura is a distinct dome-like layer of fascia, the suprapleural membrane (Fig. 3.36). This connective tissue membrane is attached laterally to the medial margin of the first rib and behind to the transverse process of vertebra CVII. Superiorly, the membrane receives muscle fibers from some of the deep muscles in the neck (scalene muscles) that function to keep the membrane taught. The suprapleural membrane provides apical support for the pleural cavity in the root of the neck.
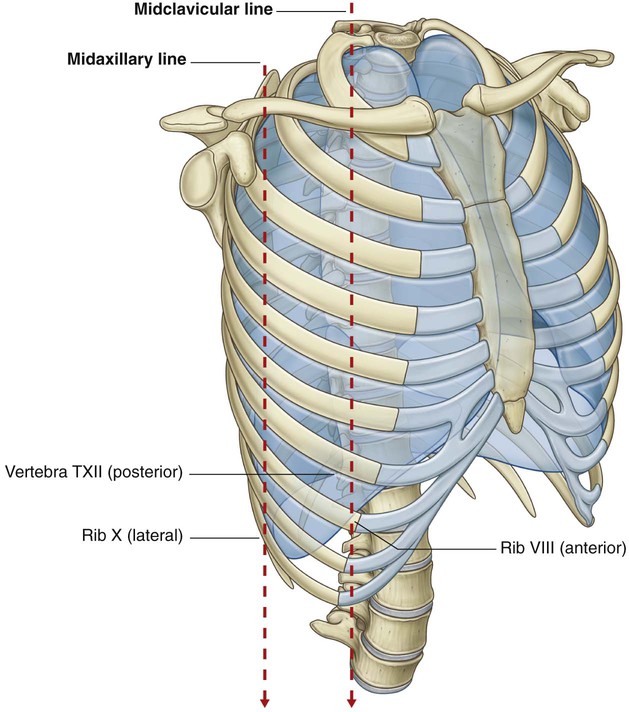
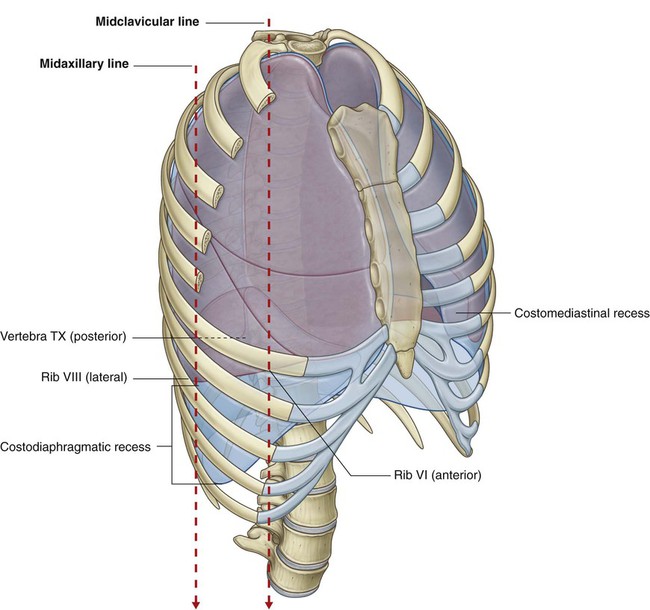
Pleural recesses
The lungs do not completely fill the anterior or posterior inferior regions of the pleural cavities (Fig. 3.38). This results in recesses in which two layers of parietal pleura become opposed. Expansion of the lungs into these spaces usually occurs only during forced inspiration; the recesses also provide potential spaces in which fluids can collect and from which fluids can be aspirated.
Costodiaphragmatic recesses
The largest and clinically most important recesses are the costodiaphragmatic recesses, which occur in each pleural cavity between the costal pleura and diaphragmatic pleura (Fig. 3.38). The costodiaphragmatic recesses are the regions between the inferior margin of the lungs and inferior margin of the pleural cavities. They are deepest after forced expiration and shallowest after forced inspiration.
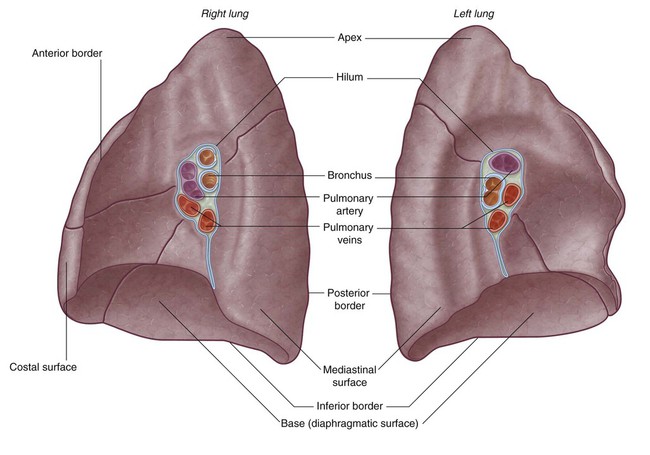
Lungs
Each lung has a half-cone shape, with a base, apex, two surfaces, and three borders (Fig. 3.39).
 The base sits on the diaphragm.
The base sits on the diaphragm.
 The apex projects above rib I and into the root of the neck.
The apex projects above rib I and into the root of the neck.
 The two surfaces—the costal surface lies immediately adjacent to the ribs and intercostal spaces of the thoracic wall. The mediastinal surface lies against the mediastinum anteriorly and the vertebral column posteriorly and contains the comma-shaped hilum of the lung, through which structures enter and leave.
The two surfaces—the costal surface lies immediately adjacent to the ribs and intercostal spaces of the thoracic wall. The mediastinal surface lies against the mediastinum anteriorly and the vertebral column posteriorly and contains the comma-shaped hilum of the lung, through which structures enter and leave.
 The three borders—the inferior border of the lung is sharp and separates the base from the costal surface. The anterior and posterior borders separate the costal surface from the medial surface. Unlike the anterior and inferior borders, which are sharp, the posterior border is smooth and rounded.
The three borders—the inferior border of the lung is sharp and separates the base from the costal surface. The anterior and posterior borders separate the costal surface from the medial surface. Unlike the anterior and inferior borders, which are sharp, the posterior border is smooth and rounded.
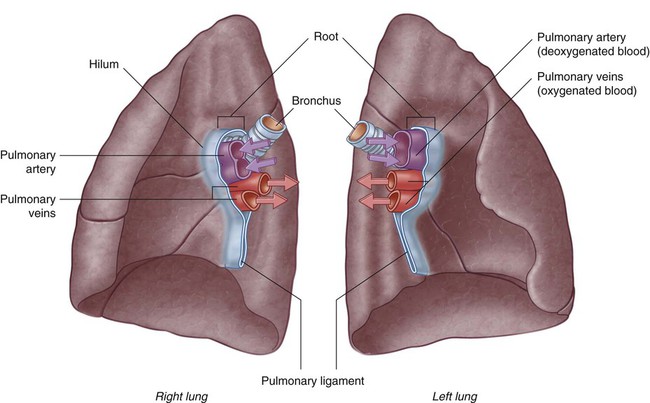
Root and hilum
The root of each lung is a short tubular collection of structures that together attach the lung to structures in the mediastinum (Fig. 3.40). It is covered by a sleeve of mediastinal pleura that reflects onto the surface of the lung as visceral pleura. The region outlined by this pleural reflection on the medial surface of the lung is the hilum, where structures enter and leave.
Within each root and located in the hilum are:
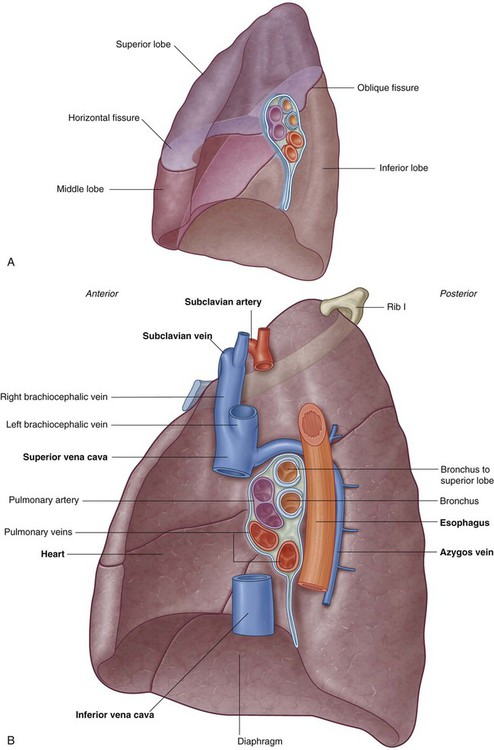
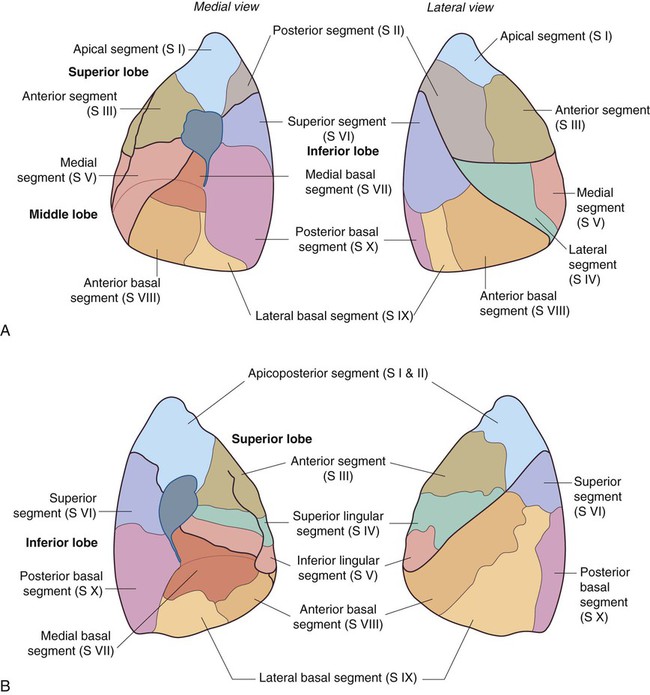
Right lung
The right lung has three lobes and two fissures (Fig. 3.41A). Normally, the lobes are freely movable against each other because they are separated, almost to the hilum, by invaginations of visceral pleura. These invaginations form the fissures:
 The oblique fissure separates the inferior lobe (lower lobe) from the superior lobe and the middle lobe of the right lung.
The oblique fissure separates the inferior lobe (lower lobe) from the superior lobe and the middle lobe of the right lung.
 The horizontal fissure separates the superior lobe (upper lobe) from the middle lobe.
The horizontal fissure separates the superior lobe (upper lobe) from the middle lobe.
The approximate position of the oblique fissure on a patient, in quiet respiration, can be marked by a curved line on the thoracic wall that begins roughly at the spinous process of the vertebra TIV level of the spine, crosses the fifth interspace laterally, and then follows the contour of rib VI anteriorly (see p. 239).
When listening to lung sounds from each of the lobes, it is important to position the stethoscope on those areas of the thoracic wall related to the underlying positions of the lobes (see p. 240).
The medial surface of the right lung lies adjacent to a number of important structures in the mediastinum and the root of the neck (Fig. 3.41B). These include the:
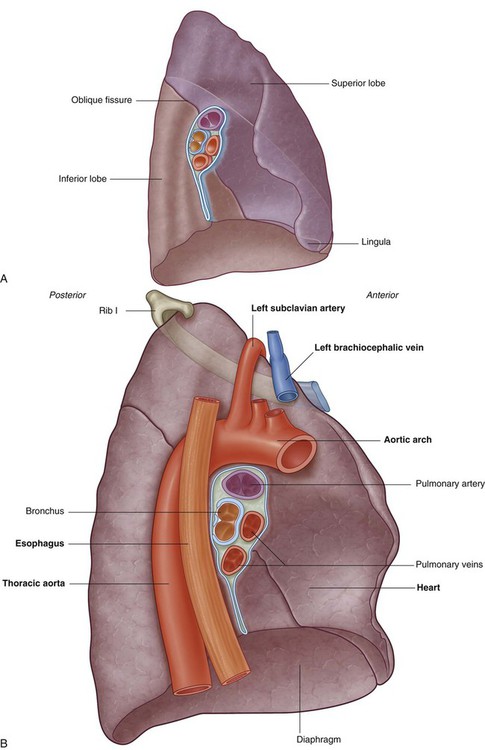
Left lung
The left lung is smaller than the right lung and has two lobes separated by an oblique fissure (Fig. 3.42A). The oblique fissure of the left lung is slightly more oblique than the corresponding fissure of the right lung.
During quiet respiration, the approximate position of the left oblique fissure can be marked by a curved line on the thoracic wall that begins between the spinous processes of vertebrae TIII and TIV, crosses the fifth interspace laterally, and follows the contour of rib VI anteriorly (see pp. 237–238).
When listening to lung sounds from each of the lobes, the stethoscope should be placed on those areas of the thoracic wall related to the underlying positions of the lobes (see p. 240).
The medial surface of the left lung lies adjacent to a number of important structures in the mediastinum and root of the neck (Fig. 3.42B). These include the:
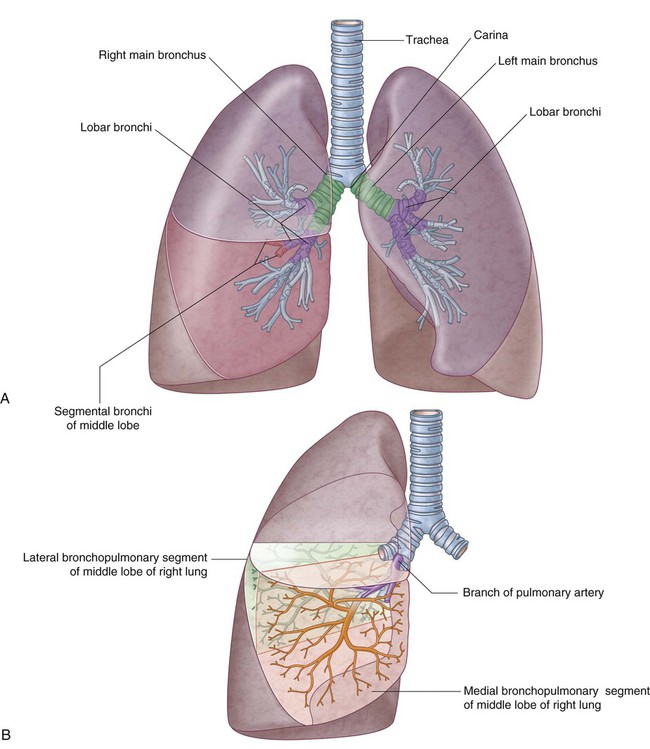
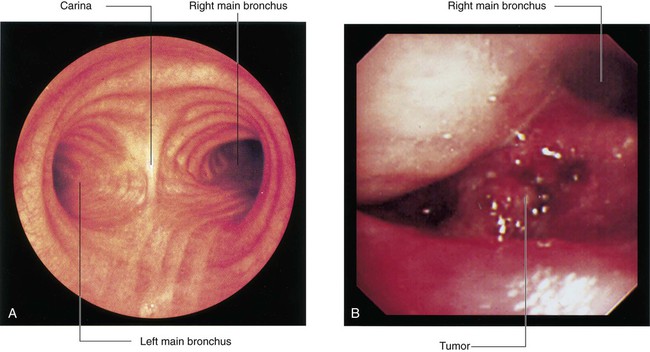
Bronchial tree
The trachea is a flexible tube that extends from vertebral level CVI in the lower neck to vertebral level TIV/V in the mediastinum where it bifurcates into a right and a left main bronchus (Fig. 3.43). The trachea is held open by C-shaped transverse cartilage rings embedded in its wall—the open part of the C facing posteriorly. The lowest tracheal ring has a hook-shaped structure, the carina, that projects backwards in the midline between the origins of the two main bronchi. The posterior wall of the trachea is composed mainly of smooth muscle.
Each main bronchus enters the root of a lung and passes through the hilum into the lung itself. The right main bronchus is wider and takes a more vertical course through the root and hilum than the left main bronchus (Fig. 3.43A). Therefore, inhaled foreign bodies tend to lodge more frequently on the right side than on the left.
The lobar bronchi further divide into segmental bronchi (tertiary bronchi), which supply bronchopulmonary segments (Fig. 3.43B).
Pulmonary arteries
The right and left pulmonary arteries originate from the pulmonary trunk and carry deoxygenated blood to the lungs from the right ventricle of the heart (Fig. 3.45).
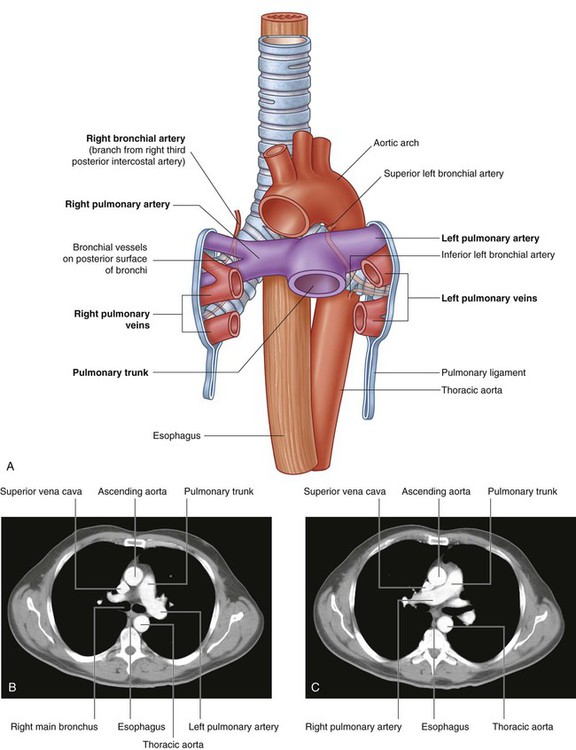
Right pulmonary artery
The right pulmonary artery is longer than the left and passes horizontally across the mediastinum (Fig. 3.45). It passes:
Bronchial arteries and veins
The bronchial arteries (Fig. 3.45) and veins constitute the “nutritive” vascular system of the pulmonary tissues (bronchial walls and glands, walls of large vessels, and visceral pleura). They interconnect within the lung with branches of the pulmonary arteries and veins.
The bronchial arteries originate from the thoracic aorta or one of its branches:
 A single right bronchial artery normally arises from the third posterior intercostal artery (but occasionally, it originates from the upper left bronchial artery).
A single right bronchial artery normally arises from the third posterior intercostal artery (but occasionally, it originates from the upper left bronchial artery).
 Two left bronchial arteries arise directly from the anterior surface of the thoracic aorta—the superior left bronchial artery arises at vertebral level TV, and the inferior one inferior to the left bronchus.
Two left bronchial arteries arise directly from the anterior surface of the thoracic aorta—the superior left bronchial artery arises at vertebral level TV, and the inferior one inferior to the left bronchus.
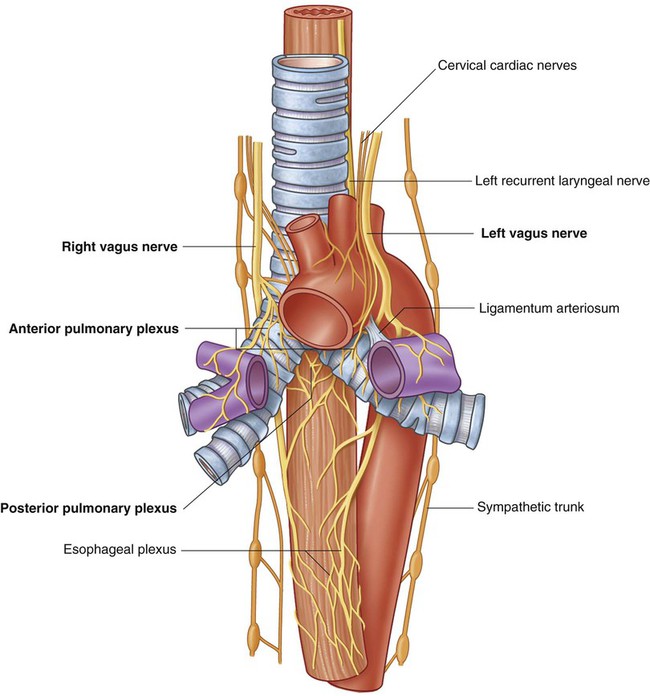
Innervation
Structures of the lung, and the visceral pleura, are supplied by visceral afferents and efferents distributed through the anterior pulmonary plexus and posterior pulmonary plexus (Fig. 3.46). These interconnected plexuses lie anteriorly and posteriorly to the tracheal bifurcation and main bronchi. The anterior plexus is much smaller than the posterior plexus.
Lymphatic drainage
Superficial, or subpleural, and deep lymphatics of the lung drain into lymph nodes called tracheobronchial nodes around the roots of lobar and main bronchi and along the sides of the trachea (Fig. 3.47). As a group, these lymph nodes extend from within the lung, through the hilum and root, and into the posterior mediastinum.