Thoracic Trauma
Trauma is an important cause of morbidity and mortality in children. Although it accounts for a minority of trauma injuries (4–25%), thoracic trauma is associated with a 20-fold increase in mortality when compared with injured children without thoracic trauma.1–10 Isolated thoracic trauma in a child is associated with a mortality rate of approximately 5%, which is largely due to penetrating trauma.1 However, children with head trauma, thoracic trauma, and abdominal trauma can have a mortality rate that approaches 40%.
Epidemiologic studies have reported a two to threefold higher incidence of thoracic trauma in boys as compared with girls.9–15 Most injuries (80–95%) are the result of blunt trauma, typically resulting from a traffic accident in which the child is a passenger or pedestrian.2,10 Not surprisingly, many children will have involvement of other organ systems with a high injury severity score (ISS). When penetrating trauma occurs, older children and adolescents are more likely to be the victims and there is a higher mortality rate.5
Contusion or laceration of the pulmonary parenchyma is the most common thoracic injury and may be associated with rib fractures and pneumothorax or hemothorax. Injuries to other organs such as the tracheobronchial tree (<1%), esophagus (<1%), aorta (<1%), diaphragm (4%), and heart (6%) are uncommon, but not insignificant.12
Specific Injuries and Management
Thoracic injuries in children can be categorized by location as seen in Box 15-1.
Chest Wall
Rib Fractures
Young children have a compliant thorax and do not begin to resemble adults until around 8 to 10 years of age. As a consequence, rib fractures are relatively uncommon in young children and occur more frequently in adolescents. Rib fractures are often suspected on physical examination and are identified on a chest radiograph (CXR) during the initial assessment. Independently, rib fractures are infrequently a cause of major morbidity or mortality, but are indicators of significant energy transfer.16 If a rib fracture is found in a child younger than 3 years, nonaccidental trauma (NAT) should be considered.17,18 Bone scans and bone surveys are useful in diagnosing remote fractures of the bony thorax in abused children, and follow-up studies improve identification of these injuries.19 In older children, rib fractures should draw attention to the risk of an associated underlying injury. Fractures and dislocations of the bony thorax and joints may cause significant long-term pain. In addition to pneumothorax and hemothorax, children with first rib fractures may have fractures of the clavicle, central nervous system injury, facial fractures, pelvic fractures, extremity injuries, and major vascular trauma.20,21 When children present with multiple rib fractures, the mortality has been reported to be as high as 42%.21 A careful survey of the child must be performed to look for significant injuries in other regions of the body.
Flail Chest
Due to the increased pliability of the chest wall, multiple rib fractures in series (flail chest) are not commonly seen in younger children.22 As a result of the wide age and size range, the treatment of flail chest in children, whether surgical or nonsurgical, adds a level of complexity when compared to adults. Chest wall dynamics and physiology differ significantly in infants compared to teenagers. Furthermore, flail chest has been identified in the neonatal period which increases the complexity of management of these patients.23
When flail chest occurs, the patient’s respiratory effort can be depressed due to a paradoxical motion of the flail segment. The large force required to produce this injury invariably results in injury to the underlying lung, which contributes to the respiratory compromise. Like other thoracic injuries, treatment is tailored to avoid respiratory depression and pneumonia.24 Adequate pain control, supplemental oxygen, chest physiotherapy, and continuous positive-pressure ventilation are non-invasive treatment modalities utilized in these patients.
In selected adults, operative correction of the flail chest has been shown to decrease morbidity, time on the ventilator, intensive care stay, and hospital costs.25,26 Since thoracic operations can be performed in injured children with minimal morbidity and mortality, similar results should be expected.14 Indications for operative management include failure to wean from mechanical ventilation. Other indications for thoracotomy are flail chest with no associated contusion, severe dyspnea, and severe chest deformity, among others.27,28
There is no standard operative approach for correction of a flail chest. Currently used techniques include wire cerclage, clamping, screw fixation, and intramedullary fixation.29 The use of absorbable plates for rib trauma has also been described with good results.30 The optimal surgical treatment in children is unclear given the required future growth of a child’s thoracic cavity. A multidisciplinary approach between pediatric surgeons, orthopedic surgeons, and critical care physicians is important.
Open Pneumothorax
Open pneumothorax (sucking chest wound) occurs when there is a gaping defect in the chest wall, and typically is caused by a blast injury, a severe avulsion injury, or an impalement (Fig. 15-1). This is not often seen in children but can be life threatening when it occurs. The negative pressure in the pleural cavity created by spontaneous breathing sucks air into the thorax. Air trapping results in collapse of the ipsilateral lung and mediastinal shift, similar to a tension pneumothorax. Treatment requires placement of an occlusive dressing to prevent further air from entering the chest cavity as well as chest tube or catheter insertion to drain a hemo/pneumothorax that may have developed.
Traumatic Asphyxia
Traumatic asphyxia is typically caused by a large compressive force against the chest wall combined with deep inspiration against a closed glottis (Valsalva maneuver). The increased thoracic pressure compresses the right atrium, excludes blood return from the superior vena cava, and results in rupture of venules and capillaries about the face and head.31 Patients will exhibit conjunctival hemorrhages, facial swelling, and petechial hemorrhages on the face and upper chest. Although severe cases may result in loss of vision or other permanent neurologic sequelae, the morbidity and mortality associated with traumatic asphyxia is generally related to the associated injuries. The majority of children who survive have good outcomes.32,33
Pleural Cavity and Pulmonary Parenchyma
Pneumothorax–Pulmonary Lacerations
Pneumothorax may occur with a penetrating injury to the chest wall or air leak into the pleural space from a pulmonary laceration or disruption of the proximal airway. It is a relatively common finding in children with blunt and penetrating thoracic trauma. The air leak may dissect under the pleura to cause pneumomediastinum and subcutaneous emphysema. A simple pneumothorax is often asymptomatic because the lack of increased intrathoracic pressure limits the recognition of symptoms. For this reason, a screening CXR is an important component in the evaluation of thoracic injury in children. Air within the pleural cavity can layer anteriorly, posteriorly, or in the subpulmonic space. A simple pneumothorax can be easily missed on chest film, but can be found on a subsequent computed tomographic (CT) scan.34 However, a recent study analyzing the utility of CT scan as a screening modality to replace initial CXR concluded that although a CT scan is highly sensitive, it should not be used as a primary imaging tool given its cost and the acceptable sensitivity of routine CXR.35 Ultrasonography (US) is another diagnostic modality that has been shown to be nearly as sensitive as CT in determining the presence of an occult pneumothorax and has gained wide acceptance as a screening tool.36,37
The need for intervention in the presence of a simple pneumothorax will depend on its severity and the child’s clinical condition. Some authors have suggested that if the volume of the pneumothorax is greater than 20% of the pleural space, then drainage is needed.38 Although insertion of a chest tube can be considered appropriate in almost every circumstance of traumatic pneumothorax, there are alternatives to conventional chest tubes, such as pigtail catheters.39 Additionally, there may be a benefit in treating with supplemental oxygen alone. The rationale for this therapy is that atmospheric gas (78% nitrogen) comprises the majority of the entrapped air collection. If the nitrogen level in the blood is ‘washed out’ by increased inspired oxygen, a nitrogen gradient will be created that will cause accelerated absorption of the air. Oxygen can be delivered by way of nasal cannula, a hood, or a mask. Treatment with supplemental oxygen may be required for 24 to 48 hours.
In contrast, a tension pneumothorax is a life-threatening condition that requires expeditious decompression. A tension pneumothorax likely causes symptoms initially from hypoxemia and later from increased intrapleural pressure with subsequent decreased venous return and cardiovascular collapse.40 If the clinician suspects a tension pneumothorax in a patient with appropriate signs and symptoms, it is reasonable to proceed with decompression without waiting for a CXR. If rapid drainage of intrapleural air cannot be accomplished with a needle, insertion of a pigtail catheter or a chest tube should be performed. A tension pneumothorax treated initially with needle decompression will require chest tube or pigtail catheter insertion due to the continuing collection of air under pressure in the involved hemithorax. If one or both lungs have been compressed for a long time, re-expansion pulmonary edema may develop.41
Systemic air embolism can occur with any pulmonary parenchymal injury and increased intrabronchial pressure, creating a bronchopulmonary venous fistula.42 This is most often seen when positive-pressure ventilation is required to support the injured patient. Sudden neurologic findings or cardiovascular decompensation may be the initial sign that air has embolized to the coronary or cerebral vessels. If this complication is recognized, steps should be taken to prevent further air embolism. If possible, the removal of the intravascular air should be considered. Treatment options include tube thoracostomy, but more often an emergency thoracotomy will provide immediate reversal of the physiology promoting the air embolism. The hilum of the lung should be occluded to prevent further escape of air into the venous system, and operative control of the bronchial–venous interface should be obtained. The mortality associated with this complication is high.
Hemothorax
Hemothorax can result from blunt or penetrating injury to any of the intrathoracic vessels, the chest wall vessels, the pleura, or the pulmonary parenchyma. Occasionally, a rib fracture can lacerate an intercostal vessel or the lung. Rarely, the aorta or vena cava may be injured by pressure or shearing. Unless the volume of blood is large, a hemothorax may be asymptomatic. Smaller volumes may be more easily detected on CT scan, which also allows for measurement of Hounsfield density to aid in the diagnosis.43 Each hemithorax can hold approximately 40% of a child’s blood volume and it is difficult to estimate the amount of blood loss on a CXR.44 Prompt chest tube placement allows for evacuation of the blood from the pleural space and re-expansion of the lung. It also allows the surgeon to assess the volume of blood loss and whether the hemorrhage is ongoing.
There are instances in which an operation may be needed to stop ongoing intrathoracic bleeding. After tube thoracostomy, the immediate blood return of 15 mL/kg, or ongoing losses of 2–3 mL/kg/h for 3 or more hours, are indicators for thoracic exploration.45,46 If undrained, the hemothorax can become organized with the development of a fibrothorax that can cause a restrictive lung defect. This predisposes to atelectasis, ventilation–perfusion mismatching, and subsequent pneumonia.
Residual blood is also an excellent culture medium, and empyema and sepsis can result from infection of an undrained hemothorax. Tube thoracostomy may not adequately evacuate an organizing post-traumatic hemothorax in up to 12% of patients.47 In this situation, thoracoscopy may be useful to evacuate the residual clot. Patients who undergo early thoracoscopy may experience less morbidity.48,49 However, there are also data to suggest that thrombolytic therapy is equally effective in treating a chronic hemothorax.47 The use of intrapleural tissue plasminogen activator (tPA) has also been used for the treatment of traumatic residual hemothoraces and other parapneumonic processes with good results.50,51
Pulmonary Contusion
One of the most common thoracic injuries in children is a pulmonary contusion, which can occur with blunt or penetrating trauma.1 The flexible chest wall of a child allows for contusion of the lung without rib fracture, resulting in areas of lung consolidation and chest wall contusion. Microscopically, pulmonary contusions show alveolar hemorrhage, consolidation, and edema. The presence of a pulmonary contusion contributes to decreased pulmonary compliance, hypoxia, hypoventilation, and a ventilation–perfusion mismatch. A CXR taken during the initial assessment may demonstrate the pulmonary contusion. However, because this is invariably a supine film, it is sometimes difficult to differentiate fluid/blood in the pleural space from a lung contusion. To this end, a chest CT scan can show areas of pulmonary contusion not appreciated on the chest radiograph and can differentiate a parenchymal process (contusion) from free fluid.52 However, when a contusion is seen on CXR, these children typically have a larger parenchymal volume that has been injured with a higher degree of impaired oxygenation.53 Also, a significant percentage will require ventilatory support. When a pulmonary contusion is seen only on CT, the morbidity of the injured child does not appear to be affected when compared with children with normal CT findings.54 The overall injury severity, associated injuries, and outcomes in these patients are similar to those seen in adults.52 Treatment includes appropriate fluid resuscitation, supplemental oxygen, pain management, and strategies to prevent atelectasis and pneumonia.
A significant percentage of patients may develop pneumonia or acute respiratory distress syndrome (ARDS) after pulmonary contusion.13 Occasionally, the pulmonary contusion can cause life-threatening hypoxia that cannot be supported with conventional ventilation, including high-frequency oscillation. Extracorporeal life support has been used in extreme circumstances to support patients with severe pulmonary contusions or ARDS.55 Children with pulmonary contusions can have prolonged changes in respiratory function and radiographic abnormalities. These changes may persist for an extended period of time after resolution of the symptoms.56 However, these children do not appear to suffer any significant long-term sequelae.15
Diaphragmatic Injuries
Blunt diaphragmatic rupture is an uncommon occurrence. The left diaphragm is involved more often because of the protective effect of the right lobe of the liver. There have been occasional reports of bilateral diaphragmatic injury (Fig. 15-2).57,58 The frequency of associated injuries, especially liver and spleen injuries, is very high.58 Blunt injury to the diaphragm can have several manifestations, but usually include chest pain that radiates to the shoulder, shortness of breath, or abdominal pain. Breath sounds may be diminished and bowel sounds may be heard on the ipsilateral side.59
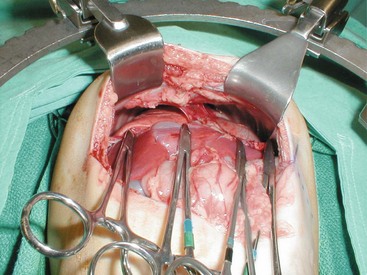
FIGURE 15-2 Bilateral diaphragmatic rupture after blunt abdominal trauma. The hemostats have been placed on the lower rim of the diaphragmatic rupture.
On imaging studies, an abnormal diaphragm contour, a high-riding diaphragm, or a questionable overlap of abdominal visceral shadows may suggest injury. Visceral herniation or the abnormal placement of a nasogastric tube into the left hemithorax should be considered diagnostic. Many diaphragmatic ruptures are not identified in the first few days after injury, and may not be detected for a considerable period of time (Fig. 15-3).60 CXR findings may be obscured by associated contusion or atelectasis in the lung bases. In patients requiring intubation, herniation of abdominal viscera through the injury may not occur until after the patient is off positive-pressure ventilation.61 CT has been used to establish the diagnosis, but the CT may appear normal in some patients. A heightened awareness of this injury should be present to avoid the late complications of visceral herniation or bowel complications.
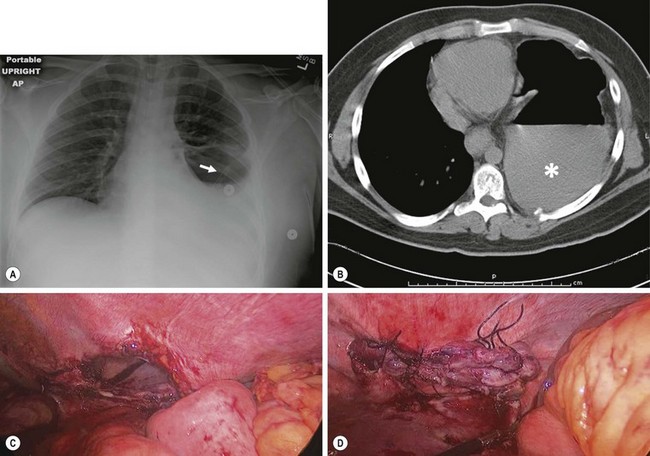
FIGURE 15-3 This 16-year-old was initially admitted to another hospital following a motor vehicle accident that necessitated insertion of a left chest tube. Six weeks later, he began to develop left-sided chest discomfort and vomiting. (A) The patient’s chest radiograph. Note the tip of the nasogastric tube in the left thoracic cavity (arrow). (B) A CT scan was performed at the outlying hospital which shows an air-fluid level in the stomach which is located in the left side chest cavity. The solid contents in the stomach are marked with an asterisk. (C) At laparoscopic exploration, the diaphragmatic defect is seen. (D) This defect was able to be closed laparoscopically and he was discharged two days later. He has recovered uneventfully and has not developed any postoperative problems with more than a one year follow-up.
When penetrating trauma is sustained below the nipple line, a diaphragmatic injury needs to be considered. Imaging evaluation is often unreliable in this setting. Therefore after determining whether other life-threatening injuries to the heart, lung, liver, spleen, or gastrointestinal tract exist, operative exploration and repair may be needed.59 If exploration is undertaken, laparoscopy, thoracoscopy, thoracotomy, or laparotomy have all been used with success (see Fig. 15-3C,D).
Mediastinum
Airway Injury
Injuries to the tracheobronchial tree are infrequent in children. Airway disruption may occur with penetrating injury or with blunt injury such as high-energy acceleration or deceleration. Up to three-quarters of these injuries are noted within 2 cm of the carina and almost half occur within the first 2 cm of the right main-stem bronchus.62 Most patients with tracheal injuries have mediastinal air on CXR. More distal injuries may rupture into the pleural space and present as a tension pneumothorax. Other findings associated with a major airway injury include a persistent large air leak from a chest tube, mediastinal air, cervical subcutaneous emphysema without pneumothorax, or florid respiratory compromise. Rarely, complete transection of a distal main-stem bronchus will appear on CXR with total lung collapse and mediastinal displacement.63 Persistent pneumomediastinum and pneumothoraces on CXR after adequate tube thoracostomy should alert the clinician to consider an injury to the tracheobronchial tree (Fig. 15-4).

FIGURE 15-4 Chest radiograph of a 2-year-old patient who was run over by an automobile. Note the persistent large right pneumothorax despite the adequate placement of a chest tube. This patient was found to have a complete disruption of the right main-stem bronchus at the orifice of the right upper lobe bronchus.
Once recognized, these injuries require prompt diagnosis and treatment. Pleural air or fluid collections should be drained until an accurate evaluation and diagnosis of the airway injury is made. Mechanical ventilation may be necessary because of respiratory failure in this setting. Fiberoptic bronchoscopy allows for evaluation of the airway and may improve the probability of successful intubation. Many airway injuries are diagnosed by rigid or flexible bronchoscopy. Chest CT with a multiple-array scanner may have a role in visualizing tracheal or bronchial injuries, especially if three-dimensional reconstructions of the airway are used (virtual bronchoscopy) (Fig. 15-5).64,65

FIGURE 15-5 CT scan of the chest in a child who sustained penetrating trauma. This image was taken from the upper thoracic region. Note the air in the subcutaneous tissue and mediastinum. This child was found to have a tracheal and an esophageal injury.
A delay in diagnosis is not uncommon in children. A retrospective review found that 75% of cases with a delayed diagnosis of tracheobronchial injury occurred in children younger than age 15.66 This was thought to be related to the probability that incomplete tears in children cause minimal symptoms and the possibility that children involved in a severe accident with the loss of a family member may be reluctant to express physical complaints.
In general, when a tracheobronchial injury is identified, operative repair is usually needed. Repair may be delayed if the symptoms can be managed without significant morbidity. Repair of some bronchial injuries can be successful even a year after injury.62 Occasionally, more distal bronchial injuries may heal with nonoperative management.67 Distal bronchial injuries are generally well managed by pulmonary resection, whereas more proximal airway trauma is best treated by direct repair. Nonoperative management of a tracheobronchial injury may result in a high incidence of airway stenosis. When the diagnosis of a tracheobronchial injury is substantially delayed, scarring may obliterate the airway lumen and cause chronic collapse of the lung segment or lobe. The degree of injury may also play a role in determining whether a repair, as opposed to a resection, is needed. Complete transections are commonly associated with an obliterated distal bronchus, which may spare the pulmonary parenchyma from infection, thus making repair possible. Incomplete tears, on the other hand, form granulation tissue and scar that result in a patent, but narrowed lumen, predisposing the supplied lung to recurrent infection and retained secretions. This usually necessitates resection at some point. Three-dimensional reconstructions of the trachea and bronchi, taken from spiral CT images, have been found to be useful in planning operative therapy treatment. If the esophagus and the airway are injured near one another, a traumatic tracheoesophageal fistula can occur.68
Great Vessel Injuries
Injuries to the heart and great vessels are rare in young children. The National Trauma Data Bank reports the incidence of blunt aortic injury to be 0.1%, but with a mortality rate of over 40%.69 Traumatic thoracic aortic disruptions can occur in children as young as 4 years of age.70,71 However, these injuries are more likely in the older child. Most (80%) children who sustain a thoracic aortic tear will have significant associated injuries to the lung, heart, skeletal system, abdominal organs, or central nervous system.72 Only half of these patients will have external evidence of a thoracic injury. Most aortic injuries in children are related to falls or motor vehicle collisions, especially when children are unrestrained.
The diagnosis of an aortic injury in a child can be difficult. Findings on a chest film can include a left apical cap, pulmonary contusion, mediastinal widening, shift of the trachea to the right, downward depression of the left main-stem bronchus, and an indistinct aorta.71 However, none of these findings is sensitive or specific enough to make the diagnosis. A normal CXR, however, is highly predictive for the absence of an aortic injury.73 A CT scan may reveal a mediastinal hematoma or the aortic injury. Transesophageal echocardiography has also been useful for making the diagnosis.74 Whereas thoracic CT and transesophageal echocardiography can diagnose aortic injuries, aortic angiography gives excellent anatomic detail (Fig. 15-6). The most common finding with a traumatic aortic injury is a pseudoaneurysm located at the proximal descending aorta. This is thought to occur secondary to tethering of the aorta by the ligamentum arteriosum, resulting in a tear in the aortic intima and media.75
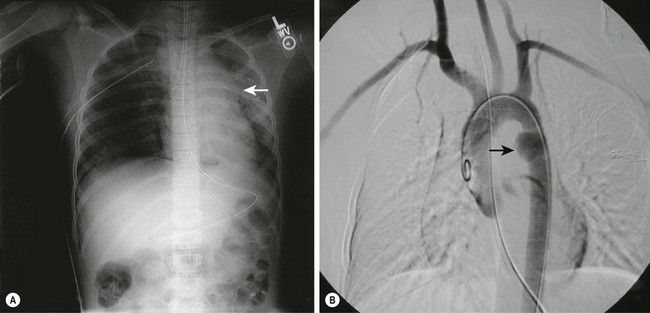
FIGURE 15-6 An 8-year-old patient presented with injuries from being an unrestrained passenger in a motor vehicle accident. (A) On the chest radiograph, note the widened mediastinum and loss of definition of the aortic knob (arrow). There is also a right pneumothorax that was treated with tube thoracostomy. (B) An aortogram shows a pseudoaneurysm (arrow) at the location of the ligamentum arteriosum just distal to the left subclavian artery, representing the partial transection of the descending aorta at this point.
There are no large collective studies of children with aortic injuries. However, of those who survive until diagnosis, more than 70% will live to discharge.71,72 Spinal cord ischemia is a complication that can occur and may be associated with preoperative cardiovascular instability.76 Although urgent operative repair is thought to be the best treatment option in most patients, recent experience has demonstrated the ability to delay operative intervention by using beta-adrenergic blockers while other injuries are managed.70,76,77 This trend in management has raised the possibility of using a less invasive endovascular approach when dealing with these injuries. In adults, studies have demonstrated that it is feasible to treat aortic injuries with endovascular stents.78 Extrapolation of this approach to children has shown that endovascular treatment in children from the ages 12 to 14 years has been successful; however, the endovascular grafts were constructed from smaller adult stent grafts.77,79,80 In the elective setting, such as endovascular treatment of aortic coarctation, infants and teenagers alike have been managed with larger adult stents.81–83 Currently, the youngest reported person with a traumatic aortic disruption treated with an endovascular stent is an 11-year-old child.84 The long-term sequelae of permanent stents in children with ‘growing’ aortas has not been evaluated. However, newer expandable stents may allow for multiple interventions in a given patient.85
Cardiac Contusion
Blunt cardiac injury such as myocardial contusion, cardiac laceration, or cardiac rupture is rare, occurring in less than 5% of children with blunt thoracic trauma.86,87 Penetrating trauma is more often a cause of cardiac and aortic injury in this age group. Cardiac contusion accounts for 95% of blunt cardiac injuries in the child, followed by valvular dysfunction and ventricular septal defect.87 Clinical manifestations of cardiac injury after blunt thoracic trauma include arrhythmia, new-onset murmur, and heart failure. However, these findings may be absent in children, and CXR and electrocardiographic findings are generally nonspecific.87
The management of a cardiac contusion is supportive. Children with a cardiac contusion who are hemodynamically stable on presentation rarely have deterioration in their cardiac rhythm. Patients should be monitored with continuous electrocardiography and frequent blood pressure determinations. Echocardiography should be performed early in the evaluation of children with a significant cardiac contusion. In patients with a suspected cardiac contusion, serum cardiac troponin I levels may be useful to confirm the diagnosis.88
Inotropic agents are occasionally needed to provide cardiac support in the presence of a cardiac contusion. Although blunt cardiac injury with heart rupture and cardiac tamponade is very rare, only immediate diagnosis and treatment will be life-saving. This is also true for penetrating cardiac trauma. A delayed diagnosis of cardiac rupture in children has been described.89,90 Immediate ultrasound in the emergency department may provide the clinical information necessary to identify this injury.91 Pericardiocentesis in this setting may provide a temporary solution while operative intervention is organized. If urgent pericardiocentesis is required in a child, it should be remembered that the distance from the skin to the pericardium is significantly reduced in younger patients relative to adults. Undercompensating or overcompensating for chest wall thickness may lead to inadequate decompression or iatrogenic cardiac injury. Once stabilized, children with a blunt cardiac injury should be followed closely and monitored for sequelae such as valvular insufficiency or a ventricular septal defect.87 Rarely, extracorporeal life support may be needed to manage a child with a severe blunt cardiac injury.
Commotio cordis has become a widely recognized problem in pediatric thoracic trauma.92 Typically, a young baseball player is struck in the chest with a hit or thrown ball and collapses suddenly. Commotio cordis is characterized by the absence of cardiac contusion, coronary artery abnormalities, structural abnormalities, or conduction system pathology. It is thought that a sudden blow to the chest will result in a disorganized cardiac rhythm followed by rapid cardiovascular collapse. Although chest protective devices seem useful, they do not provide total protection against asystole.93 Automatic electrical defibrillators may be life-saving for this rare sports-related injury.
Esophagus
Pediatric esophageal injuries are uncommon, occurring in less than 1% of children sustaining either blunt or penetrating thoracic trauma.12,94,95 The esophagus is a relatively elastic, mediastinal structure that is largely protected by the bony thorax. This mobility is helpful when blunt force is applied as the esophagus can move, which limits the likelihood of rupture. Penetrating injuries are more likely to cause esophageal trauma. Esophageal disruption may manifest as dyspnea, dysphagia, cyanosis, mediastinal air, subcutaneous emphysema, pleural effusion, chest or epigastric pain, fever, or sepsis.96 Initial symptoms, however, may be vague and nonspecific. Esophagography with a water-soluble contrast agent and esophagoscopy are typically the studies that will best identify an esophageal injury.
If the esophagus is ruptured or perforated, conventional management is operative repair. This is performed for the purpose of drainage and/or repair. Treatment is initiated with fluid resuscitation and parenteral antibiotics.97 Operative repair consists of direct suture closure of the injury. If possible, pleural flap coverage and tube thoracostomy are performed. If an operation is undertaken early after injury, this treatment strategy, along with no oral intake and total parenteral nutrition (TPN), has good success. If the perforation is not identified early, treatment becomes more difficult. In perforations of more than 24 hours duration, operative closure becomes technically much more demanding owing to the degree of inflammation and the amount of contamination. Techniques used in this circumstance include attempted suture repair, esophageal isolation, multiple drain placement, gastrostomy, and TPN.
In selected cases of esophageal perforation, nonoperative management may be successful.96 This may be the case with certain types of blunt trauma and with iatrogenic injury such as a perforation at the time of endoscopy. Nonoperative management is based on the clinical status of the patient and the injury seen on imaging studies. For example, a patient might have a small leak identified, manifested by mediastinal air or pneumothorax. If there is no fever, no effusion, and the patient looks well, nonoperative treatment with TPN and intravenous antibiotics, along with serial examinations, may be reasonable. See Chapter 26 for more information about esophageal injuries.
References
1. Peclet, MH, Newman, KD, Eichelberger, MR, et al. Thoracic trauma in children: An indicator of increased mortality. J Pediatr Surg. 1990; 25:961–966.
2. Peterson, RJ, Tepas, JJ, Edwards, FH, et al. Pediatric and adult thoracic trauma: Age-related impact on presentation and outcome. Ann Thorac Surg. 1994; 58:14–18.
3. Stafford, PW, Harmon, CM. Thoracic trauma in children. Curr Opin Pediatr. 1993; 5:325–332.
4. Holmes, JF, Sokolove, PE, Brant, WE, et al. A clinical decision rule for identifying children with thoracic injuries after blunt torso trauma. Ann Emerg Med. 2002; 39:492–499.
5. Black, TL, Snyder, CL, Miller, JP, et al. Significance of chest trauma in children. South Med J. 1996; 89:494–496.
6. Mayer, T, Matlak, ME, Johnson, DG, et al. The modified injury severity scale in pediatric multiple trauma patients. J Pediatr Surg. 1980; 15:719–726.
7. Reynolds, M. Pulmonary, esophageal and diaphragmatic injuries. In: Buntain WL, ed. Management of Paediatric Trauma. Philadelphia, PA: WB Saunders; 1995:238–247.
8. Woosley, CR, Mayes, TC. The pediatric patient and thoracic trauma. Semin Thorac Cardiovasc Surg. 2008; 20:58–63.
9. Smyth, BT. Chest trauma in children. J Pediatr Surg. 1979; 14:41–47.
10. Nakayama, DK, Ramenofsky, ML, Rowe, MI. Chest injuries in childhood. Ann Surg. 1989; 210:770–775.
11. Roux, P, Fisher, RM. Chest injuries in children: An analysis of 100 cases of blunt chest trauma from motor vehicle accidents. J Pediatr Surg. 1992; 27:551–555.
12. Cooper, A, Barlow, B, DiScala, C, et al. Mortality and truncal injury: The pediatric perspective. J Pediatr Surg. 1994; 29:33–38.
13. Allen, GS, Cox, CS, Jr. Pulmonary contusion in children: Diagnosis and management. South Med J. 1998; 91:1099–1106.
14. Balci, AE, Kazez, A, Eren, S, et al. Blunt thoracic trauma in children: Review of 137 cases. Eur J Cardiothorac Surg. 2004; 26:387–392.
15. Haxhija, EQ, Nöres, H, Schober, P, et al. Lung contusion-lacerations after blunt thoracic trauma in children. Pediatr Surg Int. 2004; 20:412–414.
16. Bliss, D, Silen, M. Pediatric thoracic trauma. Crit Care Med. 2002; 30:S409–S415.
17. Cadzow, SP, Armstrong, KL. Rib fractures in infants: Red alert! The clinical features, investigations and child protection outcomes. J Paediatr Child Health. 2000; 36:322–326.
18. Bulloch, B, Schubert, CJ, Brophy, PD, et al. Cause and clinical characteristics of rib fractures in infants. Pediatrics. 2000; 105:E48.
19. Kleinman, PK, Nimkin, K, Spevak, MR, et al. Follow-up skeletal surveys in suspected child abuse. AJR Am J Roentgenol. 1996; 167:893–896.
20. Harris, GJ, Soper, RT. Pediatric first rib fractures. J Trauma. 1990; 30:343–345.
21. Garcia, VF, Gotschall, CS, Eichelberger, MR, et al. Rib fractures in children: A marker of severe trauma. J Trauma. 1990; 30:695–700.
22. Lee, RB, Bass, SM, Morris, JA, Jr., et al. Three or more rib fractures as an indicator for transfer to a Level I trauma center: A population-based study. J Trauma. 1990; 30:689–694.
23. Gipson, CL, Tobias, JD. Flail chest in a neonate resulting from nonaccidental trauma. South Med J. 2006; 99:536–538.
24. Cannon, RM, Smith, JW, Franklin, GA, et al. Flail chest injury: Are we making any progress? Am Surg. 2012; 78:398–402.
25. Tanaka, H, Yukioka, T, Yamaguti, Y, et al. Surgical stabilization of internal pneumatic stabilization? A prospective randomized study of management of severe flail chest patients. J Trauma. 2002; 52:727–732.
26. Pettiford, BL, Luketich, JD, Landreneau, RJ. The management of flail chest. Thorac Surg Clin. 2007; 17:25–33.
27. Voggenreiter, G, Neudeck, F, Aufmkolk, M, et al. Operative chest wall stabilization in flail chest–outcomes of patients with or without pulmonary contusion. J Am Coll Surg. 1998; 187:130–138.
28. Slater, MS, Mayberry, JC, Trunkey, DD. Operative stabilization of a flail chest six years after injury. Ann Thorac Surg. 2001; 72:600–601.
29. Fitzpatrick, DC, Denard, PJ, Phelan, D, et al. Operative stabilization of flail chest injuries: Review of literature and fixation options. Eur J Trauma Emerg Surg. 2010; 36:427–433.
30. Mayberry, JC, Terhes, JT, Ellis, TJ, et al. Absorbable plates for rib fracture repair: Preliminary experience. J Trauma. 2003; 55:835–839.
31. Thompson, A, Jr., Illescas, FF, Chiu, RC. Why is the lower torso protected in traumatic asphyxia? A new hypothesis. Ann Thorac Surg. 1989; 47:247–249.
32. Gorenstein, L, Blair, GK, Shandling, B. The prognosis of traumatic asphyxia in childhood. J Pediatr Surg. 1986; 21:753–756.
33. Hurtado, TR, Della-Giustina, DA. Traumatic asphyxia in a 6-year-old boy. Pediatr Emerg Care. 2003; 19:167–168.
34. Holmes, JF, Brant, WE, Bogren, HG, et al. Prevalence and importance of pneumothoraces visualized on abdominal computed tomographic scan in children with blunt trauma. J Trauma. 2001; 50:516–520.
35. Renton, J, Kincaid, S, Ehrlich, PF. Should helical CT scanning of the thoracic cavity replace the conventional chest x-ray as a primary assessment tool in pediatric trauma? An efficacy and cost analysis. J Pediatr Surg. 2003; 38:793–797.
36. Dente, CJ, Ustin, J, Feliciano, DV, et al. The accuracy of thoracic ultrasound for detection of pneumothorax is not sustained over time: A preliminary study. J Trauma. 2007; 62:1384–1389.
37. Soldati, G, Testa, A, Sher, S, et al. Occult traumatic pneumothorax: Diagnostic accuracy of lung ultrasonography in the emergency department. Chest. 2008; 133:204–211.
38. Weissberg, D, Refaely, Y. Pneumothorax: Experience with 1,199 patients. Chest. 2000; 117:1279–1285.
39. Dull, KE, Fleisher, GR. Pigtail catheters versus large-bore chest tubes for pneumothoraces in children treated in the emergency department. Pediatr Emerg Care. 2002; 18:265–267.
40. Barton, ED, Rhee, P, Hutton, KC, et al. The pathophysiology of tension pneumothorax in ventilated swine. J Emerg Med. 1997; 15:147–153.
41. Ozlu, O, Kilic, A, Cengizlier, R. Bilateral re-expansion pulmonary edema in a child: A reminder. Acta Anaesthesiol Scand. 2000; 44:884–885.
42. Rawlins, R, Momin, A, Platts, D, et al. Traumatic cardiogenic shock due to massive air embolism. A possible role for cardiopulmonary bypass. Eur J Cardiothorac Surg. 2002; 22:845–846.
43. Rivas, LA, Fishman, JE, Múnera, F, et al. Multislice CT in thoracic trauma. Radiol Clin North Am. 2003; 41:599–616.
44. Grisoni, ER, Volsko, TA. Thoracic injuries in children. Respir Care Clin N Am. 2001; 7:25–38.
45. Rielly, JP, Brandt, ML, Mattox, KL, et al. Thoracic trauma in children. J Trauma. 1993; 34:329–331.
46. Peterson, RJ, Tiwary, AD, Kissoon, N, et al. Pediatric penetrating thoracic trauma: A five-year experience. Pediatr Emerg Care. 1994; 10:129–131.
47. Kimbrell, BJ, Yamzon, J, Petrone, P, et al. Intrapleural thrombolysis for the management of undrained traumatic hemothorax: A prospective observational study. J Trauma. 2007; 62:1175–1179.
48. Uribe, RA, Pachon, CE, Frame, SB, et al. A prospective evaluation of thoracoscopy for the diagnosis of penetrating thoracoabdominal trauma. J Trauma. 1994; 37:650–654.
49. Fabbrucci, P, Nocentini, L, Secci, S, et al. Video-assisted thoracoscopy in the early diagnosis and management of post-traumatic pneumothorax and hemothorax. Surg Endosc. 2008; 22:1227–1231.
50. Skeete, DA, Rutherford, EJ, Schlidt, SA, et al. Intrapleural tissue plasminogen activator for complicated pleural effusions. J Trauma. 2004; 57:1178–1183.
51. St. Peter, SD, Tsao, K, Harrison, C, et al. Thoracoscopic decortication vs. tube thoracostomy with fibrinolysis for empyema in children: A prospective, randomized trial. J Pediatr Surg. 2009; 44:106–111.
52. Allen, GS, Cox, CS, Moore, FA, et al. Pulmonary contusion in children: Are children different? J Am Coll Surg. 1997; 185:229–233.
53. Mizushima, Y, Hiraide, A, Shimazu, T, et al. Changes in contused lung volume and oxygenation in patients with pulmonary parenchymal injury after blunt chest trauma. Am J Emerg Med. 2000; 18:385–389.
54. Kwon, A, Sorrells, DL, Kurkchubasche, AG, et al. Isolated computed tomography diagnosis of pulmonary contusion does not correlate with increased morbidity. J Pediatr Surg. 2006; 41:78–82.
55. Weber, TR, Kountzman, B. Extracorporeal membrane oxygenation for nonneonatal pulmonary and multiple-organ failure. J Pediatr Surg. 1998; 33:1605–1609.
56. Davis, SL, Furman, DP, Costarino, AT, Jr. Adult respiratory distress syndrome in children: Associated disease, clinical course, and predictors of death. J Pediatr. 1993; 123:35–45.
57. Karnak, I, Senocak, ME, Tanyel, FC, et al. Diaphragmatic injuries in childhood. Surg Today. 2001; 31:5–11.
58. Koplewitz, BZ, Ramos, C, Manson, DE, et al. Traumatic diaphragmatic injuries in infants and children: Imaging findings. Pediatr Radiol. 2000; 30:471–479.
59. Brandt, ML, Luks, FI, Spigland, NA, et al. Diaphragmatic injury in children. J Trauma. 1992; 32:298–301.
60. Guth, AA, Pachter, HL, Kim, U. Pitfalls in the diagnosis of blunt diaphragmatic injury. Am J Surg. 1995; 170:5–9.
61. Westra, SJ, Wallace, EC. Imaging evaluation of pediatric chest trauma. Radiol Clin North Am. 2005; 43:267–281.
62. Kiser, AC, O’Brien, SM, Detterbeck, FC. Blunt tracheobronchial injuries: Treatment and outcomes. Ann Thorac Surg. 2001; 71:2059–2065.
63. Nishiumi, N, Maitani, F, Yamada, S, et al. Chest radiography assessment of tracheobronchial disruption associated with blunt chest trauma. J Trauma. 2002; 53:372–377.
64. Lomoschitz, FM, Eisenhuber, E, Linnau, KF, et al. Imaging of chest trauma: Radiological patterns of injury and diagnostic algorithms. Eur J Radiol. 2003; 48:61–70.
65. Wan, YL, Tsai, KT, Yeow, KM, et al. CT findings of bronchial transection. Am J Emerg Med. 1997; 15:176–177.
66. Ozdulger, A, Cetin, G, Erkmen Gulhan, S, et al. A review of 24 patients with bronchial ruptures: Is delay in diagnosis more common in children? Eur J Cardiothorac Surg. 2003; 23:379–383.
67. Slimane, MA, Becmeur, F, Aubert, D, et al. Tracheobronchial ruptures from blunt thoracic trauma in children. J Pediatr Surg. 1999; 34:1847–1850.
68. Reed, WJ, Doyle, SE, Aprahamian, C. Tracheoesophageal fistula after blunt chest trauma. Ann Thorac Surg. 1995; 59:1251–1256.
69. Heckman, SR, Trooskin, SZ, Burd, RS. Risk factors for blunt thoracic aortic injury in children. J Pediatr Surg. 2005; 40:98–102.
70. Dornhofer, T, Dinkel, HP, Carrel, T, et al. Complex, traumatic rupture of the thoracic aorta in a child: Diagnostic findings and delayed surgery. Eur Radiol. 2002; 12:1459–1462.
71. Lowe, LH, Bulas, DI, Eichelberger, MD, et al. Traumatic aortic injuries in children: Radiologic evaluation. AJR Am J Roentgenol. 1998; 170:39–42.
72. Eddy, AC, Rusch, VW, Fligner, CL, et al. The epidemiology of traumatic rupture of the thoracic aorta in children: A 13-year review. J Trauma. 1990; 30:989–991.
73. Hall, A, Johnson, K. The imaging of paediatric thoracic trauma. Paediatr Respir Rev. 2002; 3:241–247.
74. Pearson, GD, Karr, SS, Trachiotis, GD, et al. A retrospective review of the role of transesophageal echocardiography in aortic and cardiac trauma in a level I Pediatric Trauma Center. J Am Soc Echocardiogr. 1997; 10:946–955.
75. Mirvis, SE, Shanmuganathan, K. Diagnosis of blunt traumatic aortic injury 2007: Still a nemesis. Eur J Radiol. 2007; 64:27–40.
76. Karmy-Jones, R, Carter, YM, Nathens, A, et al. Impact of presenting physiology and associated injuries on outcome following traumatic rupture of the thoracic aorta. Am Surg. 2001; 67:61–66.
77. Karmy-Jones, R, Hoffer, E, Meissner, M, et al. Management of traumatic rupture of the thoracic aorta in pediatric patients. Ann Thorac Surg. 2003; 75:1513–1517.
78. Wellons, ED, Milner, R, Solis, M, et al. Stent-graft repair of traumatic thoracic aortic disruptions. J Vasc Surg. 2004; 40:1095–1100.
79. Hoffer, EK, Karmy-Jones, R, Bloch, RD, et al. Treatment of acute thoracic aortic injury with commercially available abdominal aortic stent-grafts. J Vasc Interv Radiol. 2002; 13:1037–1041.
80. Milas, ZL, Milner, R, Chaikoff, E, et al. Endograft stenting in the adolescent population for traumatic aortic injuries. J Pediatr Surg. 2006; 41:e27–e30.
81. Lee, ML. Endovascular stent for the aortic coarctation in a 1.7-kg premie presenting intractable heart failure. Int J Cardiol. 2006; 113:236–238.
82. Takawira, FF, Sinyangwe, G, Mooloo, R. Endovascular covered stent treatment for descending aorta pseudoaneurysm following coarctation of the aorta repair in an infant. Heart Lung Circ. 2010; 19:745–748.
83. Patnaik, AN, Srinivas, B, Rao, DS. Endovascular stenting for native coarctation in older children and adolescents using adult self-expanding (Nitinol) iliac stents. Indian Heart J. 2009; 61:353–357.
84. Gunabushanam, V, Mishra, N, Calderin, J, et al. Endovascular stenting of blunt thoracic aortic injury in an 11-year-old. J Pediatr Surg. 2010; 45:E15–E18.
85. Chakrabarti, S, Kenny, D, Morgan, G, et al. Balloon expandable stent implantation for native and recurrent coarctation of the aorta–prospective computed tomography assessment of stent integrity, aneurysm formation and stenosis relief. Heart. 2010; 96:1212–1216.
86. Tiao, GM, Griffith, PM, Szmuszkovicz, JR, et al. Cardiac and great vessel injuries in children after blunt trauma: An institutional review. J Pediatr Surg. 2000; 35:1656–1660.
87. Dowd, MD, Krug, S. Pediatric blunt cardiac injury: Epidemiology, clinical features, and diagnosis. Pediatric Emergency Medicine Collaborative Research Committee: Working Group on Blunt Cardiac Injury. J Trauma. 1996; 40:61–67.
88. Hirsch, R, Landt, Y, Porter, S, et al. Cardiac troponin I in pediatrics: Normal values and potential use in the assessment of cardiac injury. J Pediatr. 1997; 130:872–877.
89. Murillo, CA, Owens-Stovall, SK, Kim, S, et al. Delayed cardiac tamponade after blunt chest trauma in a child. J Trauma. 2002; 52:573–575.
90. Rezende Neto, JB, Diniz, HO, Filho, CS, et al. Blunt traumatic rupture of the heart in a child: Case report and review of the literature. J Trauma. 2001; 50:746–749.
91. Symbas, NP, Bongiorno, PF, Symbas, PN. Blunt cardiac rupture: The utility of emergency department ultrasound. Ann Thorac Surg. 1999; 67:1274–1276.
92. Perron, AD, Brady, WJ, Erling, BF. Commodio cordis: An underappreciated cause of sudden cardiac death in young patients: Assessment and management in the ED. Am J Emerg Med. 2001; 19:406–409.
93. Maron, BJ, Gohman, TE, Kyle, SB. Clinical profile and spectrum of commotio cordis. JAMA. 2002; 287:1142–1146.
94. Sartorelli, KH, McBride, WJ, Vane, DW. Perforation of the intrathoracic esophagus from blunt trauma in a child: Case report and review of the literature. J Pediatr Surg. 1999; 34:495–497.
95. Cotton, BA, Nance, ML. Penetrating trauma in children. Semin Pediatr Surg. 2004; 13:87–97.
96. Engum, SA, Grosfeld, JL, West, KW, et al. Improved survival in children with esophageal perforation. Arch Surg. 1996; 131:604–611.
97. Asensio, JA, Chahwan, S, Forno, W, et al. Penetrating esophageal injuries: Multicenter study of the American Association for the Surgery of Trauma. J Trauma. 2001; 50:289–296.