CHAPTER 72 Thoracic Spinal Pain
INTRODUCTION
Disorders of the thoracic spine are as disabling as those in the cervical and lumbar spine and therefore deserve wider recognition than they often receive. As a consequence of having a low incidence, diagnosis and treatment often remain a challenge. Thoracic pain accounts for less than 2% of spinal pain.1 Pain may be due to soft tissue, visceral, disc or structural etiologies.2,3 Pain from thoracic spine lesions may present as pain in the anterior and/or posterior thorax, lumbar spine, and extremities.4 In a study by Acre and Dohramm, 57% were found to present with non-specific pain, 24% present with sensory changes, and 17% present with motor changes.5 The thoracic spine is relatively immobile due to the unique anatomy6 and is stabilized and strengthened by the rib cage.7,8
ETIOLOGY
There are numerous etiologies for thoracic spinal pain as outlined in Table 72.1. One cause of thoracic pain is thoracic disc disease. The incidence of thoracic disc disease is less than 2%.5,9,10 This low incidence may be due to the orientation of the thoracic facet joints in the coronal plane, restraint of the thoracic spine by the ribs and sternum, and the small size of the thoracic discs. Thoracic spine disc herniations account for only 0.2–5% of all disc herniations and have a male predominance. The lower, more mobile segments (T11–12) are affected with greater frequency.5,11–13 The youngest reported case of thoracic disc herniation was in a child 12 years of age.5 Although trauma may contribute to thoracic disc herniation,12 degenerative changes are the most common cause of thoracic disc herniation.5
Most major thoracic disc lesions occur in the lower thoracic spine, but minor thoracic disc lesions occur in the upper and middle regions. Thoracic disc disease usually affects adults in the fourth through sixth decades of life,5,10 in some cases following spinal trauma. The intervertebral discs of the thoracic spine increase in height and width from cranial to caudal. The spinal canal is relatively small, and the epidural space is narrow. The narrowest point is between T4 and T9. The intradiscal pressure is very high in the ventral segment of the thoracic spine, while dorsally the support is mainly by the vertebral joints. Nevertheless, parts of the intervertebral discs can displace towards the spinal canal.14 Seventy percent of these herniations occur in a posterolateral direction. Onset can be acute, subacute, or chronic.10 Ninety percent of patients have signs of spinal cord compression at the time of diagnosis.5
Another cause of thoracic spinal pain is canal stenosis, often stemming from osteoarthritis with facet hypertrophy combined with hypertrophy of the posterior longitudinal ligament and/or ligamentum flavum with or without facet joint hypertrophy.15–17 Thoracic facet joint disease is most common at the T3–5 segment.4 The incidence of thoracic canal stenosis is approximately 2%.18 Infectious causes of thoracic spinal pain include tuberculosis (Pott’s disease), discitis, or osteomyelitis.
This etiology is of particular relevance in the immunocompetent and immunocompromised patient. A retrospective review of 33 patients with tuberculosis of the spine revealed that the majority of the lesions involved the thoracic spine (30%), followed by lumbar spine (27%). Skip lesions were seen in 12% of the patients. Neurological involvement was seen in 50% of patients. The concomitant pulmonary tuberculous rate was 67%.19 In those who are immunocompromised, such as patients with HIV, steroid use, organ transplant, i.v. drug use, or cancer, there may be a delay in diagnosis due to the fact that they may not present with signs and symptoms as evident as in immunocompetent patients.20 Back pain accompanied by fever may be the presenting symptoms of discitis. Septic discitis is inflammation of the intervertebral disc and discovertebral junction. The inflammatory process may extend in to the epidural space, posterior vertebral elements, and paraspinal musculature21 Spondylodiscitis accounts for 2% of all cases of osteomyelitis.22 In a study done by Hopkinson et al., the spectrum of septic discitis was studied. They found that the incidence was 2 per 100 000. Seventy-three percent were 65 years or older; 91% had back pain, with lumbar, thoracic, and then cervical as the most common areas affected. Predisposing factors included cancer, diabetes, and invasive spinal procedures.23
Thoracic spine fractures of various causes may also lead to significant thoracic spinal pain. Thoracic spine fractures are unique due to the anatomy of the thoracic spine and its biomechanics. Fractures can cause neurological compromise because of the small size of the thoracic spinal canal relative to the spinal cord.7,8 Fractures may be due to compression of the vertebral body compounded with or without compression of neural elements as seen in Figure 72.1. Disorders known to contribute to fractures include osteoporosis, tumor such as primary spinal cord lesions, systemic disease such as multiple myeloma, metastatic disease such as those most commonly found from breast, lung, or prostate cancer, or from trauma itself. Not only do the etiologies differ, they may also have varying physical findings, treatments, and functional outcomes.24
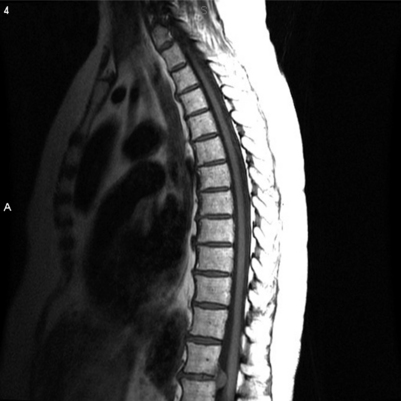
Fig. 72.1 Sagittal magnetic resonance image revealing large disc herniation at T11–T12.
(Courtesy of MD Anderson Cancer Center.)
Osteoporosis can lead to significant back pain, kyphosis, impaired respiratory function, and quality of life, as well as morbidity. Fractures due to osteoporosis occur in the spine (especially thoracolumbar), hip, and distal forearm. The lifetime risk of clinically diagnosed vertebral fractures is approximately 15% in Caucasian women.25 Vertebral fractures are the most common skeletal injury from osteoporosis, with an incidence of 700 000 per year in the United States.26 Vertebral body height reduction by 20% or 4 mm can be considered a vertebral compression fracture (Fig. 72.2).27 Three types of vertebral fractures in osteoporosis are described: wedge, crush, and biconcave. Most common are wedge fractures (collapsed anterior border with almost intact posterior border), which occur mostly in the midthoracic and thoracolumbar regions.28 In crush fractures, the entire vertebral body is collapsed. Crush fractures are also usually located in the midthoracic or thoracolumbar areas. Biconcave fractures collapse in the central portion of the vertebral body and are more commonly seen in the lumbar region. Those who have wedge fractures tend to experience severe, sharp pain, which usually gradually decreases over 4–8 weeks, although chronic pain is common in this patient group. Patients with superior endplate discontinuity have progression to complete collapse of the vertebral body and have dull, less severe pain. Those with more severe pain initially and a well-defined wedge fracture may have better functional outcomes with pain management and early mobilization.29 Pain due to vertebral fractures is due to a combination of a reduction in body weight, decreased compressive spinal loading, and decreased bone mass.30 Risk factors include lack of hormonal replacement in the perimenopausal period, chronic illnesses, smoking, and alcohol use.31,32
Thoracic-region pain in the adolescent or athlete may be due to muscle strain, stress fractures, or costochondritis. Stress fractures occur when there is overloading of the bone. Common areas of stress fractures include the ribs, especially the first rib. Patients usually complain of pain and shoulder discomfort with radiation into the sternum. Costochondritis is an inflammation (without swelling) and Tietze’s syndrome (with swelling) at the costochondral junction where two different tissue types merge, especially in an area stressed by repetitive movement. Costochondritis usually occurs in ribs two through five and is provoked by movement.33 Scoliosis is another abnormality that may also contribute to thoracic pain. Adult scoliosis usually patterns with more rigid deformity than adolescent idiopathic scoliosis.34
Back pain due to metastatic bone disease can lead to fractures, hypercalcemia, and spinal cord compression, all of which can adversely affect a patient’s functional status and quality of life. Metastatic bone disease leads to increased osteoclastic activity and impaired bone metabolism. Patients with neoplastic diseases such as breast, prostate, or lung cancer, and multiple myeloma may experience some of the sequelae of skeletal complications.35
In rare cases, spinal cord compression may be idiopathic. Saito et al. described a 68-year-old female who had chronic midback pain with slowly progressive weakness over 34 years when she became paraplegic. Magnetic resonance imaging (MRI) revealed idiopathic spinal cord herniation at T6–7. She underwent T5–8 laminectomy, and her pain improved although she continued to have some lower extremity weakness.36
Post-thoracotomy pain and postherpetic neuralgia (PHN) are both causes of thoracic pain of radicular origin. In these cases, the pain referral pattern is neuropathic in nature and not usually due to axial pain.37
Anterior and middle column injuries may contribute to thoracic spinal pain. Posterior column injuries are commonly reported; however, anterior and middle column injuries are often missed and not reported. Katz and Scerpella reviewed seven gymnasts’ reports of back injuries, finding a relatively high incidence of thoracic anterior column pathology in a young patient population. All subjects had tenderness to palpation and were neurologically intact. Two had pain with provocative tests (straight-leg raise or single-leg hyperextension test). Each subject had plain roentgenograms. Three of them were normal. Four subjects had MRIs with findings consistent with disc herniation or degeneration. Of those with abnormal MRI findings, two subjects had vertebral body compression fractures. One subject had a compression fracture of T12 with a 30% loss of height, multiple Schmorl’s nodes, and fractures at L4 and L5. The other one had T11 anterior wedging and T11–12 disc space narrowing. All subjects were treated by physical therapy; two had interventional epidural or facet blocks, and none had surgery. In all cases, practice time was lost. Only one continued to remain competitive. Therefore, anterior and middle column abnormalities from injuries should be included in the differential diagnosis of the thoracic back in athletes.38
Another cause of thoracic back pain may be myofascial pain syndrome. This syndrome is characterized by regional pain, usually in the neck and upper back, with presence of trigger points. The most commonly affected areas of pain and trigger points include the levator scapulae muscles and the upper and lower trapezius.39
Rare causes of thoracic pain may be associated with other pain syndromes such as complex regional pain syndrome-1 (CRPS-1),40 rheumatoid arthritis (RA),41 the T4 syndrome,3 and thoracic nerve root dysfunction (TNRD).42,43 TNRD is most often seen in diabetics who present with chest or abdominal pain, sensory polyneuropathy, or weight loss.42,43 Other causes of TNRD include herpes zoster, scoliosis or osteoarthritis of the thoracic spine, thoracic disc disease, or carcinoma of the thoracic spinal nerve roots.44,45 Rheumatoid arthritis may be associated with thoracic back pain although diffuse joint pain and neck pain may be more prevalent41 The spinal area most commonly affected is the atlantoaxial region; however, thoracic spinal pain may also be present.46 Ankylosing spondylitis (AS) may also be another cause of thoracic back pain. Back pains with sacroiliitis along with other features of spondyloarthropathy (ethesitis and uveitis) are highly suggestive of AS.47
PHYSICAL EXAM
In addition to a thorough history, a general physical exam with a focus on the thoracic spine should be performed. The thorax and back should be examined for any signs of trauma, infection, lesions, or other skin abnormalities. The inspection should also include any overt deformity of the spine such as scoliosis or kyphosis. Abnormalities in posture, biomechanics, and mobility should be noted. The axial spine and ribs should be palpated for any evidence of tenderness. Sensory deficits (hypoesthesia or allodynia) along the back and thorax should be noted. Any abnormalities in the range of motion should be documented. Manual muscle testing in the upper and lower extremities along with reflex testing should be performed.48 The chest should be auscultated to ensure that there are no other physical signs of a systemic disorder. If an infectious etiology is suspected, then examination of lymph nodes and glands may be beneficial. If an inflammatory disease is suspected, then examination of joints and overall musculature is warranted.49 If malignancy is suspected, then the exam should be centered on a systematic approach.
Symptoms of thoracic disc disease may be reported as vague and poorly defined.10,11,50,51 The location of the disc herniation may present with different physical findings. For instance, a central disc herniation may present with pyramidal tract signs, whereas lateral discs may present with radicular pain.6,10–12,52 Common symptoms include motor and sensory deficits with radicular pain or numbness. Bowel and bladder dysfunction may also be present. Examination may reveal upper motor signs such as hyperreflexia, spastic paraparesis, and Babinski signs. If sensory dysfunction is present, it is usually decreased sensation.5,10,12,50,52–54 Symptoms may not present for several years.5,10,12,53 Local pain may be due to distention of the nerve fibers in the anulus fibrosus and posterior longitudinal ligament.10,12 Small disc herniations may also produce spinal cord compression because of the anterior placement of the spinal cord with respect to the thoracic canal.55 Radicular pain may be due to impingement on the short thoracic nerve root by the disc or from traction or stretching of the root by the thecal sac.12
Neurologic symptoms from disorders of the thoracic and lumbar spine can present with upper motor or lower motor findings, cauda equina syndrome, or nerve root lesions.5 In a retrospective review of 26 symptomatic patients, Tokuhashi et al. reviewed different levels of disc herniations and the physical findings for each level. They found that for those with T10–11 and T11–12 disc herniations, the clinical presentation was consistent with upper motor neuron disorders (increased patellar tendon and ankle tendon reflexes), positive Babinski signs, and bowel and bladder dysfunction. In those patients with T12–L1 disc herniations, the physical findings were suggestive of a lower motor neuron disorder (muscle weakness/atrophy, decreased patellar and ankle tendon reflexes, and negative Babinski signs). For the L1–2 disc herniations, mild disorders of cauda equina and sensory disturbance at the anterior or lateral aspect of the thigh were noted. In the L1–3 group, most had severe thigh pain, sensory deficits, and weakness in the quadriceps and tibialis anterior, and decreased or absent patellar tendon reflexes.56
Sometimes, thoracic disc herniations may have unusual presentations or pain referral patterns. Wilke et al. reported a case of thoracic disc herniation that presented with chronic shoulder pain. In this report, a 44-year-old female with shoulder pain underwent acromioplasty. However, symptoms and pain became progressive. She then developed urinary retention. MRI of thoracic spine revealed an extradural space-occupying lesion at T10–11 (sequestered prolapsed intervertebral disc). The patient was treated with costotransversectomy and nucleotomy at T10–11, and her symptoms improved immediately.57
Thoracic disc herniation may also present like acute lumbosacral radiculopathy. Compression of the lumbosacral spinal nerve roots at the lower thoracic level after their exit from the lumbar enlargement may contribute to this physical finding. Lyu et al. reported such a case. A 49-year-old woman was found to have sudden low back pain with radiation into the left buttock and lateral aspect of the left leg and foot. MRI with contrast was consistent with T11–12 midline disc bulge and posterior osteophytes. When she was treated with a laminectomy, her symptoms resolved immediately. A 3-year follow-up revealed normal neurological function with mild low back soreness.58
Thoracic back pain may also present with paresthesias, numbness, or upper extremity pain with or without headaches. DeFranca and Levine described the T4 syndrome where patients presented with upper back stiffness, headaches, and paresthesias without gross neurological deficits. Thoracic joint dysfunction appeared to be the cause of the symptoms.3
For the immunocompromised patient with spinal disease, the most common presenting symptom is back pain (thoracic or lumbar) with radiculopathy, myelopathy, or sensory deficits.20 If discitis is suspected, the patient may have focal back pain, with possible radicular involvement, as well as neurological compromise. The presentation of symptoms may be acute or chronic.21 In the study of septic discitis in the immunocompetent patient by Hopkinson et al., 45 had neurological symptoms such as weakness, urinary retention, diminished reflexes, and sensory deficits. Therefore, focal back pain in a patient with constitutional symptoms and/or neurological sequelae may be indicative of discitis.23 Although many cases of spondylodiscitis may present acutely, some present after years with the disease. In a case report by Finsterer et al., a 65-year-old female had recurrent, localized thoracic back pain for over 2 years. Approximately 9 months after pain onset, she developed sensory deficit of the left lower extremity. Fourteen months prior to admission, she had recurrent fever, mild weakness, and numbness of the lower extremities.59
In patients with osteoporotic vertebral fractures, the spine may appear kyphotic. These patients become shorter as a consequence of vertebral compression and flexed posture. An exaggerated thoracic kyphosis and a protuberant abdomen may compromise and reduce lung capacity.60 Pain is exacerbated by standing erect or with a change of position or movement. Pain may also be reproduced by palpation of the spinous process at the involved level. Neurological deficits are rare, but should be ruled out by a thorough examination of motor and sensory function.61
Patients who have post-thoracotomy pain syndrome have a history of chest and/or spine surgery several weeks or months prior to development of pain. Examination can reveal muscular tenderness, sensitivity to touch, with either decreased or increased sensation. Tenderness is usually along a dermatome near the incision. Upper extremity range of motion may be decreased due to pain.37 Postherpetic neuralgia (PHN) may have similar physical findings. Pain is usually unilateral. Pain in PHN is a common presenting symptom. Pain from acute herpes zoster may last a few weeks or persist longer.62 Pain in a dermatomal pattern usually presents 7–10 days prior to the rash. Nerves commonly affected include T4–6, cervical, and trigeminal. Pain is produced by inflammation associated with movement of the virus from sensory nerves to skin and subcutaneous tissues.63 Pain may present in 90% of the patients with allodynia (pain evoked by nonpainful stimuli) or with deafferentation (sensory loss without allodynia).64 Management and treatment should begin immediately after symptoms begin.63
In those patients suspected of having an inflammatory disease such as RA, physical findings in addition to those related to back pain may be beneficial in assisting with the diagnosis. For instance, most patients with RA have symmetrical swelling of small joints and have morning stiffness of at least 1 hour. Extra-articular synovitis along with malaise, fatigue, fever, and weight loss may be seen.41 In patients with AS or suspected AS, there is loss of spinal mobility, especially with restrictions of flexion and extension of the thoracic and lumbar spine, as well as restrictions of chest expansion. Ankylosis along with muscular spasms and limitation of motion may contribute to pain. The spine may be stiff or fused and there may be sacroiliac joint dysfunction along with limitations of bilateral hip involvement, peripheral arthritis, and extra-articular manifestations. Postural abnormalities also contribute to pain. In severe cases, lumbar lordosis is destroyed, the buttocks atrophy, thoracic kyphosis is exaggerated, and the neck is flexed. Thoracic kyphosis may contribute to restricted chest wall motion with concomitant decreased vital capacity.47 If a stress fracture or costochondritis is suspected, patients will experience tenderness with pressure over the affected ribs, especially since the painful area tends to be focal.33
In the myofascial pain syndrome, diagnosis is made by clinical presentation of regional pain, referred pain, taut bands in muscles, tenderness, and restricted range of motion as described by Simons. On examination, pain is due to muscle tension within or over muscles or their attachments. Trigger points are also elicited.65
DIAGNOSIS
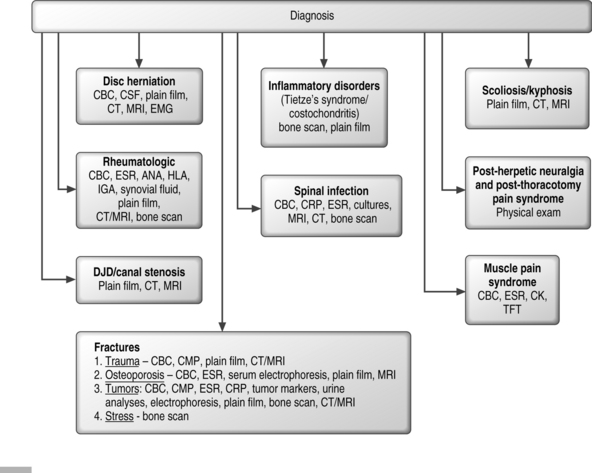
Laboratory work-up
The laboratory work-up for a patient with thoracic back pain can vary based on the history and physical findings. Figure 72.3 summarizes the diagnostic evaluation of thoracic spinal pain. For instance, if thoracic disc herniation is suspected, complete blood count (CBC) may be normal and cerebrospinal fluid (CSF) analyses usually reveal a normal cell count and clear fluid.12 If tumor or malignancy is suspected, then CBC, complete metabolic profile (CMP), tumor markers, urine analysis, electrophoresis (SPEP, UPEP), and erythrocyte sedimentation rate (ESR) may be beneficial in assisting with the diagnosis. If a rheumatological disorder or connective tissue disorder is suspected, then ESR, ANA, HLA, RF, calcium, alkaline phosphatase, and cultures may be of value. To rule out a source of infection, ESR, C-reactive protein (CRP), CBC, and cultures should be performed.
For a spinal infection in an immunocompromised patient, the diagnosis is made by identification of the pathogen since MRI, computer tomography (CT), and bone scan do not aid in the diagnosis unless tuberculosis is suspected.20 In an immunocompetent patient with suspected discitis, MRI is the best imaging study to assist with the diagnosis.21 Hopkinson et al. found that CRP and ESR were elevated in 68% of the patients, and MRI made the diagnosis. The most common pathogen identified was Staphylococcus aureus.23 Findings on imaging studies may also be seen when the symptoms are chronic. For instance, Finsterer et al. found that even after a 2-year presentation of back pain, MRI imaging revealed T11 vertebral body destruction with spondylodiscitis of adjacent discs and epidural abscess from T4–9.59 If a patient is suspected of having back pain and there are other systemic signs, an inflammatory disorder such as RA must be considered in the work-up. Diagnosis may be made with elevated ESR and CRP along with anemia and specific rheumatologic indicators.41 In patients with AS, the HLA-B27 gene is present in 90–95% of patients. Other markers include increased CRP, ESR, raised alkaline phosphatase levels, above normal serum IgA levels, and a mild normochromic normocytic anemia. Synovial fluid analyses are similar to that of other joint diseases.47 In patients suspected of having myofascial pain syndrome, suggested evaluation includes ESR, serum creatine kinase, CBC, and thyroid function tests. These are all normal in myofascial pain syndrome, which is a diagnosis of exclusion.65
Osteoporotic fractures in the upper thoracic spine may be suggestive of an underlying malignancy and a thorough evaluation should be performed. Evaluation with CBC, ESR, and serum electrophoresis can help in identifying an underlying malignancy (including multiple myeloma) in a patient with a high thoracic fracture.66
Radiological work-up
In general, the radiological evaluation of patients with thoracic pain includes plain films, CT, and/or MRIs. Plain radiographs may be helpful in determining flexibility of the spine. Techniques commonly used to evaluate flexibility include side bending, fulcrum bending, push-prone, and traction radiographs.67–69
Deviren et al. evaluated potential predictors of flexibility in patients with thoracolumbar and lumbar scoliosis by side-bending radiographs. In this retrospective study of 75 patients with idiopathic thoracolumbar and lumbar scoliosis, preoperative side bending and standing X-rays of thoracolumbar and lumbar curves were taken. Cobb angles, curve flexibility, and axial and radicular pain were noted. Axial and radicular pain were more commonly associated with adult deformity than adolescent idiopathic deformity. Findings revealed that 75 patients had average major curve magnitude of 56° and flexibility of 55%. Both axial and radicular pain was correlated with age but not curve magnitude. Curve magnitude and age are main predictors of structural flexibility. Every 10° increase in curve magnitude over 40° resulted in 10% decrease in flexibility and every 10-year increase in age decreased flexibility of structural curve by 5%. Progressive loss of flexibility with age and curve progression can make surgical correction more challenging.34
Common radiographic findings in thoracic disc herniation include disc space narrowing, osteophyte formation, kyphosis, and calcification.13,52,54
MR can detect spinal cord compression and disc degeneration on T2-weighted sequences.70
Gadolinium enhancement may also detect small and large herniations as seen in Figure 72.1.55 In patients with thoracic canal stenosis, there may be hypertrophy of the facets manifested by increased density overlying the zygapophyseal joints on frontal or lateral radiographs.71–73 Arana et al. found that there may be a relationship between upper thoracic and cervical spine degenerative disc disease. They studied the incidence and evaluated upper thoracic degenerative disc changes on MRI in patients with neck pain. In this study, 156 patients, 19–83 years old, with cervical pain had MRI imaging including thoracic spine. Findings revealed that 13.4% of the patients with cervicalgia had degenerative disc changes in the thoracic spine. The most commonly affected area was in the T2–3 disc.74
Electromyography may also be beneficial in diagnosing patients with thoracic nerve root dysfunction (TNRD). Electromyography may reveal findings suggestive of radiculopathy.75 Such findings include normal nerve conduction studies, decreased recruitment in motor unit action potentials, and the presence of fibrillations or positive sharp waves.76
If a vertebral compression fracture is suspected, radiographs may show osteopenia and a fracture with loss of height, with possible wedging and occasionally retropulsion of osseous fragments into the spinal canal. Most fractures are located in the thoracolumbar area.28 MRI of the spine is most useful in determining fracture age, excluding malignant tumor, and for selecting appropriate treatment. In an acute fracture, MRI shows a geographic pattern of low-intensity signal changes on T1-weighted images and high-intensity signal changes on T2-weighted images, indicating more bone edema in the acute fracture. As the fracture becomes chronic, a linear area of low-intensity signal change replaces the geographic area on T1-weighted images.77 The MRI findings of osteoporotic and metastatic spine fractures are decreased signal intensity on T1-weighted images and increased signal intensity on T2-weighted images. Pedicle involvement or involvement of other posterior elements and presence of lesions in the epidural space or paraspinal regions are suggestive of malignancy rather than osteoporosis.78 Bone scans are sensitive and can be used to identify and discriminate acute from chronic fractures; however, they have low specificity for the diagnosis of the underlying process.79
If a traumatic fracture of the thoracic spine is suspected, it should be treated appropriately. However, many fractures may be occult and missed if no radiological studies are taken. The absence of pain and tenderness does not necessarily exclude significant thoracolumbar trauma.80 For instance, Cooper et al. found that 31% (34 patients) out of 183 patients who had GCS 13–15 in the Maryland Shock Trauma Center had no pain or tenderness, yet all had fractures.81 Thoracolumbar spinal fractures are not uncommon and may be missed. Kirkpatrick and McKevitt recommend clinical clearance (of trauma patients) if patients are clinically responsive, nonintoxicated, and neurologically intact without another spinal injury. Otherwise, they advocate full imaging evaluation to assess for thoracolumbar fractures.80
Patients with inflammatory diseases such as RA and AS may have distinct radiographic presentations. For instance, in RA, radiographic images show juxta-articular osteoporosis.41 In AS, radiological changes reflect the disease process, and sacroiliitis is usually detectable in the early stages of AS. MRI and CT can detect AS lesions earlier than plain radiography. Plain films and MRI also reveal thoracic kyphosis and fused spine in severe cases.47 Reactive changes affect the discovertebral junctions in the thoracolumbar area. On MRI images, inflammatory osteitis of the vertebrae is visualized.82 In patients with stress fractures, the definitive diagnosis may be made by a bone scan. Bone scans are also helpful in diagnosing Tietze’s syndrome. Plain films may be normal leading to delay in diagnosis with further evaluation only when there is concern that a large bony callus may represent a bone tumor or other pathology.33 Plain films, bone scan, CT, or MRI may evaluate infectious etiologies of the spine.
Differential diagnosis
Some patients with thoracic disc disease or pain are thought to have cardiovascular, pulmonary, gastrointestinal, genitourinary, or psychiatric disorders.10,11,50,51 Disc herniation can be confused with esophagitis, nephritis, gastrointestinal ulcers and cholecystitis.83 Some patients with T1 herniation may present with Horner’s syndrome51,84 and T11 herniation with testicular pain.85 Thoracic nerve root dysfunction may be diagnosed as abdominal pain unless a careful history and physical examination are performed.86
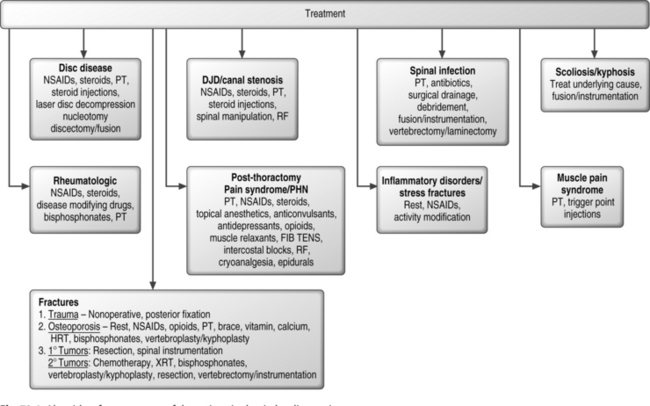
TREATMENT
In treatment of thoracic disc disease, numerous management strategies, from conservative through aggressive surgical options are available as shown in Figure 72.4.14 The goal of physical therapy is to improve posture, joint and spinal mobility and flexibility, to strengthen musculature such as the trapezius, rhomboids, and latissmus dorsi, and to prevent deconditioning.65
For pain which persists despite conservative treatment, steroid injections can be used in the treatment of pain of spinal origin. These injections can be performed relatively quickly and conveniently with or without radiological guidance, although fluoroscopic guidance may allow more accurate injections to the appropriate anatomic level. The therapeutic effects of corticosteroids are mostly due to their antiinflammatory effects. They may also have local anesthetic-like actions on peripheral nerves. The antiinflammatory effect is through modification of protein synthesis at a nuclear level. At therapeutic doses corticosteroids up-regulate the production of lipocortin, a protein that inhibits phospholipase A2. This enzyme converts membrane-bound phospholipids into arachidonic acid derivatives, including leukotrienes and prostaglandins that are potent inflammatory mediators. To this date, there are no existing data for epidural steroid injections for the treatment of radicular pain of thoracic origin. Thoracic zygapophyseal joints can be a source of pain and, although steroids and denveration procedures are routinely performed, data currently available do not allow for conclusions to be reached.87
Spinal manipulative therapy is commonly used for treatment of joint dysfunction and pain. Thoracic zygapophyseal joints can be a source of pain.88 A single-blind, randomized, controlled pilot study to investigate the effectiveness of spinal manipulative therapy in the treatment of mechanical thoracic spine pain was performed. Thirty subjects (16–60 years) were split into two groups. All had thoracic spine range of motion tested with BROM II goniometers and pain threshold with algometers. All completed Oswestry Back Pain Disability Index, short-form McGill Pain Questionnaire, and Numerical Pain Rating Scale – 101 Questionnaires. The treatment group received thoracic spinal manipulation, and the placebo group received nonfunctional ultrasound application. The spinal manipulative therapy group showed improvements in both subjective and objective measurements. The ultrasound group, however, showed improvements in subjective measurement only.89
Radiofrequency (RF) ablation of the zygapophyseal joints is a minimally invasive technique used to treat mechanical pain of spinal origin. In a study by Pevsner et al., 122 patients underwent RF of the medial branch nerve for mechanical back pain. The levels included cervical, thoracic, and lumbar segments. Patients were followed at 1, 3, 6, and 12 months after RF. Seventy-five percent of patients had significant pain relief after 1 month; 71% had significant pain relief after 3 months. At 6 months, 66% had pain relief and 34% had no effect. At 12 months, 63% still had good pain relief while 37% had no effect. Complications included transient discomfort and burning pain in 27 patients.90
Another minimally invasive procedure recommended for patients who have no relief with conservative treatment includes nonendoscopic percutaneous laser disc decompression and nucleotomy (PLDN) with Nd-YAG laser 1064 nm.91 Following diagnosis by MRI, this technique may be employed for thoracic discogenic pain. Hellinger et al. recommends Nd-YAG laser 1064 nm with a maximal dose of 15 watts, 1 second per single shot with a total dose of 1000 joules per intervertebral disc. In their practice, regional anesthesia is used and motor function is observed. The procedure is performed with fluoroscopic guidance, as are most minimally invasive procedures. Patients are prescribed a brace for 6 weeks after treatment. In the prospective study by Hellinger et al., aimed at treating 42 patients with thoracic disc protrusions and extrusions, monitored parameters were VAS, subjective condition, neurological findings, and peripheral EMG. At 6 weeks after treatment, success rate was 90%. Complications include one case of spondylodiscitis, one pneumothorax, and one case of pleuritis. Pain relief and decompression of spinal structures was effective and immediate by disc vaporization, shrinkage, and nociceptor destruction.14
When a spinal infection is suspected in an immunocompromised patient based on the appropriate clinical and lab findings, the treatment involves medical management, physical therapy to prevent deconditioning, and immobilization of the affected area. If tuberculosis of the spine is suspected, the mainstay of treatment is antituberculosis chemotherapy, which is highly effective. Additional treatment includes radical anterior debridement and fusion along with anterior or posterior instrumentation.19 Epidural abscesses require surgical drainage if there is neurological compromise. Vertebrectomy may also be indicated if there is evidence of spinal cord impingement or osteomyelitis.20
In the treatment of immunocompetent patients with septic discitis, most without neurological compromise can be treated with i.v. antibiotics. Those with neurological deficits require surgical drainage and laminectomy.23 Even after a 2-year history of back pain and symptoms of epidural abscess, treatment is equivalent to treatment for symptoms that present acutely. For instance, in case study by Finsterer et al. with the diagnosis of an epidural abscess 2 years after the patient had developed symptoms, the abscess was drained and laminectomy was performed. The patient was treated with i.v. antibiotics for S. aureus infection and had full neurological recovery after 10 weeks.59
Patients with thoracic spine fractures due to various causes may present with physical findings and be treated according to their clinical presentation. Dai reviewed thoracic spine fractures in 77 patients. Thirty-seven were compression fractures, 34 were fracture-dislocations, 3 burst fractures and 3 burst-dislocations. Twenty-six had complete spinal cord lesions, 14 had incomplete injuries, and 37 were neurologically intact. Approximately 70% were treated nonoperatively and 30% operatively. Those with complete spinal cord lesions had no neurological improvement. One-third of the neurologically intact patients continued to have pain although they retained normal function. Fifty percent of those with incomplete lesions had neurological recovery.24
Thoracic spinal pain due to fractures in the neurologically intact patient may be managed either nonoperatively or with posterior fixation. Surgical treatment usually includes decompression of neural elements and posterior fixation with pedicle screws. This technique provides spinal stability, pain relief, and partial correction of kyphosis. In a prospective study of 80 patients with burst fractures without neurological deficit, patients were randomized into a nonoperative treatment group or a posterior fixation group. All patients were neurologically intact, with burst fractures at T1–L2, had no fracture dislocations or pedicle fractures, had nonpathological cause of fractures, and had no other musculoskeletal or major organ system injuries. The nonoperative group were allowed activity to pain tolerance while wearing a hyperextension brace. The operative group had a three-level fixation. A 2-year follow-up revealed that the surgical group had less pain only up to 3 months. In the nonoperative group, the kyphosis angle worsened by 4° and retropulsion decreased from 34% to 15%. Therefore, posterior fixation provided partial kyphosis correction and earlier pain relief, but functional outcomes were similar.92
Symptomatic conservative management of osteoporotic fractures includes a short period of bed rest, modification of activity, opioids, antiinflammatory agents, and a brace.26 Appropriate nutrition, calcium and vitamin D, along with cessation of smoking and alcohol plus moderate exercise and physical therapy focused on weight-bearing exercises are recommended. Hormonal replacement in those without contraindications may also be beneficial.93 Other agents commonly prescribed include bisphosphonates and calcitonin.94 The physical therapy regimen includes spinal extension exercises to reduce lumbar lordosis, correction of poor posture, strengthening of abdominal musculature with a focus on weight bearing, and progressive, resistive, and chest expansion exercises. Thoracolumbar orthoses may also be helpful to relieve pain and to promote extension of the spine.65
If an osteoporotic fracture is suspected and patients do not respond to conservative treatment, minimally invasive procedures such as nerve root injections for pain control may be attempted. In a study by Kim et al., 58 patients with osteoporotic vertebral fractures received a nerve root injection with lidocaine, bupivacaine, and DepoMedrol. Pain scores were obtained before treatment, at 1 month and 6 months after treatment (mean of 14 months postfracture follow-up). Six patients reported excellent pain results, 42 reported good results, and 10 reported fair results. Therefore, this study suggests a trial of nerve root injections for reducing symptoms of back pain prior to more invasive procedures.95
Although nerve root injections may help relieve back pain due to osteoporotic vertebral compression fractures, they do not modify the vertebral body causing the pain. Balloon kyphoplasty has been shown to safely reduce and repair vertebral compression fractures and increase independence and quality of life. A retrospective chart review of 96 patients with 133 fractures evaluated functional outcomes of patients at 1 week, 1 month, 3 months, 6 months, and 1 year after balloon kyphoplasty. This procedure increased vertebral body height, decreased acute and chronic back pain, and led to increased independence.96 Both vertebroplasty and kyphoplasty are procedures which percutaneously inject methylmethacrylate into the vertebral body. With kyphoplasty, a balloon ‘tamp’ is inserted into the vertebral body to increase the vertebral body height prior to methylmethacrylate injection. This procedure can correct kyphotic deformity.97 There are no studies directly comparing vertebroplasty and kyphoplasty, but both procedures reduce pain effectively and have low complication rates in numerous cases series.98–100
Benign tumors of the spine that present with back pain are rare and often misdiagnosed. Symptoms can be alleviated with the appropriate management such as excision and debridement of the lesion along with spinal instrumentation and fusion.101
If bony metastases from cancer are suspected, nonsurgical management includes external beam radiotherapy, chemotherapy, as well as bisphosphonates such as zoledronic acid or pamidronate. Bisphosphonates may relieve symptoms of pain from bony metastasis, but the ultimate goal is to prevent and teat osteoporosis in those with cancer.35 Vertebroplasty and kyphoplasty can also be beneficial to patients with painful compression fractures due to metastasis.94
Short-course radiotherapy may lead to significant improvements in symptom control (back pain, weakness) and to improvements in functional status in patients with metastatic spinal cord compression. In a study by Maranzano et al., they found that early treatment with a short course of radiotherapy for patients had positive clinical outcomes in those with spinal cord compression due to metastatic disease. They studied 53 patients with less radio-responsive primary tumors (non small cell lung, kidney, head and neck, melanoma, sarcomas), and more radio-responsive ones (breast, prostate, lymphoma, and multiple myeloma). All patients received a single fraction of 8 Gy, repeated after 1 week in responders, for a total dose of 16 Gy. All patients also received dexamethasone along with antiemetics. Response was assessed according to back pain, motor function, and bladder function before and after radiotherapy. Findings revealed pain relief in 67% of patients, 63% for motor function, and 98% for improved or preserved bladder function.102
If pain is due to post-thoracotomy pain, which is caused by incisional pain or muscular pain, pleural irritation due to chest tubes, effective analgesia may contribute to improved respiratory function and prevent complications such as infections and atelectasis.38 Treatment of post-thoracotomy pain syndrome includes NSAIDs, steroids, topical local anesthetics, anticonvulsants, opioids, and muscle relaxants. Epidural infusions are frequently used for postoperative pain control.103 Noninvasive and nonpharmacological approaches in the treatment of post-thoracotomy pain include electrical nerve stimulation104 and cryoanalgesia.105 A small preliminary case series showed favorable, short-duration analgesia with the use of focal intense brief transcutaneous electric nerve stimulation (FIBTENS) for the treatment of radicular and post-thoracotomy pain.104
Cryoanalgesia or freezing of intercostal nerves may also offer short- and long-term analgesia.105 In a clinical trial of patients undergoing thoracotomy, 200 patients were randomized to cryoanalgesia versus conventional (parenteral opiates) analgesia groups. Findings revealed that compared to the conventional analgesia group, cryoanalgesia of intercostal nerves led to improvement in postoperative pain scores, decreased opiate analgesia usage, and improvement in respiratory function. Cutaneous sensory changes resolved within 6 months with complete restoration of function.106
If PHN is suspected, there are many treatment options. A few such options include antivirals, antidepressants, corticosteroids, opioids, anticonvulsants, topical agents, nerve blockade (sympathetic nerve blockade, epidural), and spinal cord stimulation.64 In a retrospective study by Rowbotham et al., sympathetic blockade was performed to prevent PHN. Ninety percent of patients were pain free when treatment began within 2 months of zoster onset.107
For treatment of inflammatory disorders such as RA and AS, many options are available. NSAIDs are effective and considered to be first-line treatment although they only provide symptomatic relief without modifying the disease course. Other agents include corticosteroids,47 disease-modifying drugs such as sulfasalazine, methotrexate, thalidomide, and TNF-α.108 Other agents include intravenous bisphosphonates such as pamidronate.109 Nonpharmacological management of AS includes exercises to maintain erect posture, spinal and joint mobility, and chest expansion as well as aerobic exercises.65 However, the spine is susceptible to fractures and dislocation, atlantoaxial and spinal deformity, hip disease, and spinal stenosis, for which surgery may be required.109 Treatment of stress fractures, costochondritis, and Tietze’s syndrome is supportive with NSAIDs, relative rest, and modification of activity.33
For patients with the T4 syndrome as described by DeFranca and Levine, patients were treated with joint manipulation, stretching, and strengthening exercises. The symptoms then resolved.3 If myofascial pain syndrome is suspected based on physical findings, treatment includes correcting poor posture and body mechanics, along with stress management. In addition, prolonged stretching exercises with neuromuscular re-education may be beneficial.65 Localized treatments include spray and stretch technique with vapocoolant spray. Other treatments include trigger point injections with local anesthetics and dry needling.39
Sellman and Mayer studied six patients who had chronic thoracic back pain and were suspected of having TNRD. All patients had pain referred to the abdomen. The main causes of TNRD were osteoarthritis and diabetes. Electromyography revealed acute radiculopathy. All of the patients received treatment with antiinflammatory agents, along with anticonvulsants, tricyclic antidepressants, or local nerve blocks. Symptoms resolved within 6 months of treatment.75
For impairments in posture, joint mobility, muscle performance, and range of motion, along with thoracic intervertebral derangement, an intense physical therapy regimen may lead to more effective thoracic pain control. For example, Austin and Benesky described the biomechanics and alleviation of thoracic pain in a collegiate runner. Examination revealed moderate forward head posture, increased thoracic kyphosis, decreased lumbar lordosis, shoulder depression, decreased thoracic range of motion, and painful trunk rotation. Three weeks of mobilization, high-velocity, low-amplitude manipulation (HVLA), along with multiplanar therapeutic exercise and postural education drastically improved symptoms and function.110 Other muscular causes of thoracic pain such as myofascial pain syndromes may be treated with some similar techniques such as therapeutic exercise, prolonged stretch, and postural and neuromuscular education. In severe cases, additional use of muscle relaxants, trigger point injections, or acupuncture may be helpful.65
1 Kramer J. Intervertebral disc disease: causes, diagnosis, treatment, and prophylaxis. Georg Stuttgart: Thieme-Verlag, 1981.
2 Decina PA, Vallee DM, Nueray D. Acute pancreatitis presenting as back pain: a case report. J Can Chiropract Assoc. 1992;36:75-83.
3 DeFranca GG, Levine LJ. The T4 syndrome. Jf Manip Physiolol Ther. 1995;18(1):34-37.
4 Skubic JW, Kostuik JP. Thoracic pain syndromes and thoracic disc herniation. The adult spine: principles and practice. Philadelphia: Lippincott, Williams & Wilkins, 1991;1443-1461.
5 Arce CA, Dorhmann GJ. Thoracic disc herniation: Improved diagnosis with computed tomographic scanning and a review of the literature. Surg Neurol. 1985;23:356-361.
6 Blumenkopf B. Thoracic intervertebral disc herniations: Diagnostic value of magnetic resonance imaging. Neurosurgery. 1988;23:36-40.
7 Brandser EA, El-Khoury GY. Thoracic and lumbar spine trauma. Radiol Clin North Am. 1997;35:533-557.
8 Saboe LA, Reid DC, Davis LA, et al. Spine trauma and associated injuries. J Trauma. 1991;31:43-48.
9 Alvarez O, Roque CT, Pampati M. Multilevel thoracic disk herniations: CT and MR studies. J Comput Assist Tomogr. 1988;12:649-652.
10 Arseni C, Nash F. Protrusion of the thoracic intervertebral discs. Acta Neurochir. 1963;11:3-33.
11 Abbott KH, Retter RH. Protrusions of thoracic intervertebral disks. Neuorology. 1956;6:1-10.
12 Love JG, Schorn VG. Thoracic-disk protrusions. JAMA. 1965;191:627-631.
13 Otani K, Yosida M, Fujii E, et al. Thoracic disc herniation: Surgical treatment in 23 patients. Spine. 1988;13:1262-1267.
14 Hellinger J, Stern S, Hellinger S. Nonendoscopic Nd-YAG 1064 nm PLDN in the treatment of thoracic discogenic pain syndromes. J Clinl Laser Med Surg. 2003;21(2):61-66.
15 Barnett Gh, Hardy RW, Little JR, et al. Thoracic spinal canal stenosis. J Neuosurg. 1987;66:338-344.
16 Chintapalli K. Progressive myelopathy in a 32-year-old man. JAMA. 1985;253:2255-2257.
17 Miyasaka K, Kaneda K, Ito T, et al. Ossification of spinal ligaments causing thoracic radiculomyelopathy. Radiology. 1982;143:463-468.
18 Ungersbrock K, Perneczky A, Korn A. Thoracic vertebral stenosis combined with thoracic disc herniation. Spine. 1987;12:612-615.
19 Dharmalingam M. Tuberculosis of the spine – the Sabah experience. Epidemiology, treatment and results. Tuberculosis. 2004;84(1–2):24-28.
20 Broner FA, Garland DE, Zigler JE. Spinal infections of the immunocompromised host. Orthoped Clin N Am. 1996;27(1):37-46.
21 Kapeller P, Fazekas F, Krametter D, et al. Pyogenic infectious spondylitis: clinical, laboratory and MRI features. Eur Neurol. 1997;38:94-98.
22 Maiuri F, Iaconetta G, Gallicchio B, et al. Spondylodiscitis: clinical and magnetic resonance diagnosis. Spine. 1997;22:1741-1746.
23 Hopkinson N, Stevenson J, Benjamin S. A case ascertainment study of septic discitis: clinical, microbiological and radiological features. Q J Med. 2001;94(9):465-470.
24 Dai L. Thoracic spine fractures. Chin Med Sci J Drc. 2001;16(4):227-230.
25 Dennison E, Cooper C. Epidemiology of osteoporotic fractures. Hormone Res. 2000;54(Suppl 1):58-63.
26 Riggs BI, Melton LJ. Involutional osteoporosis. N Engl J Med. 1986;314:1676-1686.
27 Black DM, Palermo L, Nevitt MC, et al. Defining incident vertebral deformity: a prospective comparison of several approaches. The Study of Osteoporotic Fractures Research Group. J Bone Miner Res. 1999;14:90-101.
28 Ismali AA, Cooper C, Felsenberg D, et al. Number and type of vertebral deformities: epidemiological characteristics and relation to back pain and height loss. European Vertebral Osteoporosis Study Group. Osteoporosis Int. 1999;9:206-213.
29 Lyritis GP, Mayasis B, Tsakalakos N, et al. The natural history of the osteoporotic vertebral fracture. Clin Rheumatol. 1989;8(Suppl 2):66-69.
30 Mellish RW, Garrahan NJ, Compston JE. Age-related changes in trabecular width and spacing in human iliac crest biopsies. Bone Miner. 1989;6:331-338.
31 Santavirta S, Konttinen YT, Heliovaara M, et al. Determinant of osteoporotic thoracic vertebral fracture. Screening of 1000 Finnish women and men. Acta Ortho Scand. 1992;63:198-202.
32 Huopio J, Kroger H, Honkanen R, et al. Risk factors for perimenopausal fractures: a prospective study. Osteoporos Int. 2000;11:219-227.
33 Karlson KA. Thoracic region pain in athletes. Curr Sports Med Rep. 2004;3(1):53-57.
34 Deviren V, Berven S, Kleinstueck F, et al. Predictors of flexibility and pain patterns in thoracolumbar and lumbar idiopathic scoliosis. Spine. 2002;27(21):2346-2349.
35 Coleman RE. Metastatic bone disease: clinical features, pathophysiology and treatment strategies. Cancer Treat Rev. 2001;27(3):165-176.
36 Saito T, Anamizu Y, Nakamura K, et al. Case of idiopathic thoracic spinal cord herniation with a chronic history: a case report and review of the literature. J Orthoped Sci. 2004;9(1):94-98.
37 Katz J. Cryoanalgesia for postthoracotomy pain. Ann Thorac Surg. 1989;48:5.
38 Katz D, Scerpella T. Anterior and middle column thoracolumbar spine injuries in young female gymnasts. Am J Sports Med. 2003;31(4):611-616.
39 Travell JG, Simons DG. Myofascial pain and dysfunction: the trigger point manual. Baltimore: Williams & Wilkins, 1983.
40 Menck JY, Frquejo SM, Kulig K. Thoracic spine dysfunction in upper extremity complex regional pain syndrome type 1. J Orthop Sports Phys Ther. 2000;30(7):401-409.
41 Grassi W, De Angelis R, Lamanna G, et al. The clinical features of rheumatoid arthritis. Eur J Radiol. 1998;27(Suppl 1):S18-S24.
42 Longstreth GF, Newcomer AD. Abdominal pain caused by diabetic radiculopathy. Ann Intern Med. 1977;86:166-168.
43 Kitka DG, Breur AC, Wilbourn AJ. Thoracic root pain in diabetes: the spectrum of clinical and electromyographic findings. Ann Neurol. 1981;11:80-85.
44 Liveson JA. Thoracic radiculopathy related to collapsed thoracic vertebral bodies. J Neurol Neurosurg Psychiatr. 1984;47:404-406.
45 Marinacci AA, Courville CB. Radicular syndromes simulating intraabdominal surgical conditions. Am Surg. 1962;28:59-63.
46 Neva MH, Kotaniemi A, Kaarela K, et al. Atlantoaxial disorders in rheumatoid arthritis associated with the destruction of peripheral and shoulder joints, and decreased bone mineral density. Clin Exp Rheumatol. 2003;21(2):179-184.
47 Sieper J, Braun J, Rudwaleit M, et al. Ankylosing spondylitis: an overview. Ann Rheum Dis. 2002;61(Suppl 3):iii8-ii18.
48 Hoppenfeld S. Orthopaedic neurology, a diagnostic guide to neurological levels. Philadelphia: Lippincott, Williams & Wilkins, 1997.
49 American Pain Society. Guideline for the management of pain in osteoarthritis, rhuematoid arthritis, and juvenile chronic arthritis, 2nd edn. Glenview, IL: American Pain Society, 2002.
50 Benson MKD, Byrnes DP. The clinical syndromes and surgical treatment of thoracic intervertebral disc prolapse. J Bone Joint Surg [Br]. 1975;57B:471-477.
51 Svien HJ, Karavitis AL. Multiple protrusions of intervertebral disks in the upper thoracic region: Report of case. Staff Meetings of the Mayo Clinic. 1954;29:375-378.
52 O’Leary P, Camins MB, Polifroni NV, et al. Thoracic disc disease – clinical manifestations and surgical treatment. Bulletin of the Hospital for Joint Diseases Orthopedic Institute. 1984;44:27-40.
53 Epstein JA. The syndrome of herniation of the lower thoracic intervertebral discs with nerve root and spinal cord compression. J Neurosurg. 1954;11:525-538.
54 McAllister Vl, Sage MR. The radiology of thoracic disc protrusion. Clin Radiol. 1976;27:291-299.
55 Parizel PM, Rodesch G, Baleriaux D, et al. Gd-DTPA-enhanced MR in thoracic disc herniations. Neuroradiology. 1989;31(1):75-79.
56 Tokuhashi Y, Matsuzaki H, Uematsu Y, et al. Symptoms of thoracolumbar junction disc herniation. Spine. 2001;26(22):E512-E518.
57 Wilke A, Wolf U, Lageard P, et al. Thoracic disc herniation: a diagnostic challenge. Man Ther. 2000;5(3):181-184.
58 Lyu RK, Chang HS, Tang LM, et al. Thoracic disc herniation mimicking acute lumbar disc disease. Spine. 1999;24(4):416-418.
59 Finsterer J, Mahr K, Paral V. Favorable outcome of long-lasting thoracic spondylodiscitis with spinal epidural abscess induced by Staphylococcus aureus. South Med J. 2003;96(1):70-73.
60 Schlaich C, Minne HW, Bruckner T, et al. Reduced pulmonary function in patients with spinal osteoporotic fractures. Osteoporosis Int. 1998;8:261-267.
61 Lee YL, Yip KM. The osteoporotic spine. Clin Orthop. 1996;323:91-97.
62 Dworkin RH, Portenoy RK. Pain and its persistence in herpes zoster. Pain. 1996;67(2–3):241-251.
63 Bowsher D. Pathophysiology of postherpetic neuralgia: Towards a rational treatment. Neurology. 1995;45(suppl 8):S56.
64 Bajwa ZH, Ho CC. Herpetic neuralgia. Use of combination therapy for pain relief in acute and chronic herpes zoster. Geriatrics. 2001;56(12):18-24.
65 Braddom R. Physical medicine and rehabilitation, 2nd edn., Philadelphia: WB Saunders; 2000:942-954.
66 De Smet AA, Robinson RG, Johnson BE, et al. Spinal compression fractures in osteoporotic women: patterns and relationship to hyperkyphosis. Radiology. 1988;166:497-500.
67 Cheung KMC, Luk KDK. Prediction of correction of scoliosis with use of the fulocrum-bending radiograph. J Bone Joint Surg [Am]. 1997;79:1144-1150.
68 King HA, Moe JH, Bradford DS, et al. The selection of fusion levels in thoracic idiopathic scoliosis. J Bone Joint Surg [Am]. 1983;65:1302-1313.
69 Kleinman RG, Csongradi JJ, Rinksy LA, et al. Radiographic assessment of spinal flexibility in scoliosis: a study of the efficacy of the prone push film. Clin Orthop. 1982;162:47-53.
70 Paajanen H, Alanen A, Erkintalo M, et al. Disc degeneration in Scheuermann disease. Skeletal Radiol. 1989;18:523-526.
71 Omojola MF, Cardoso ER, Fox AJ, et al. Thoracic myelopathy secondary to ossified ligamentum flavum. J Neurosurg. 1982;56:448-450.
72 Reisner A, Stiles RG, Tindall SC. Diffuse idiopathic skeletal hyperostosis causing acute thoracic myelopathy: A case report and discussion. Neurosurgery. 1990;26(3):507-511.
73 Smith DE, Godersky JC. Thoracic spondylosis: An unusual cause of myelopathy. Neurosurgery. 1987;20:589-593.
74 Arana E, Marti-Bonmati L, Molla E, et al. Upper thoracic-spine disc degeneration in patients with cervical pain. Skeletal Radiol. 2004;33(1):29-33.
75 Sellman MS, Mayer RF. Thoracoabdominal radiculopathy. South Med J. 1988;81(2):199-201.
76 Preston D, Shapiro B. Electromyography and neuromuscular disorders. Boston: Butterworth-Heinemann, 1998;413-423.
77 Yamato M, Nishimura G, Kuramochi E, et al. MR appearance at different ages of osteoporotic compression fractures of the vertebrae. Radiat Med. 1998;16:329-334.
78 Baur A, Stabler A, Bruning R, et al. Diffusion-weighted MR imaging of bone marrow: differentiation of benign versus pathological compression fractures. Radiology. 1998;207:349-356.
79 Cook G, Hannaford E, See M, et al. The value of bone scintigraphy in the evaluation of osteoporotic patients with back pain. Scand J Rheumatol. 2002;31:245-248.
80 Kirkpatric A, McKevitt E. Thoracolumbar spine fractures: Is there a problem? Can J Surg. 2002;45:1.
81 Cooper C, Dunham CM, Rodriguez A. Falls and major injuries are risk factors for thoracolumbar fractures: cognitive impairment and multiple injuries impede the detection of back pain and tenderness. J Trauma. 1995;38:692-696.
82 Kurugoglu S, Kanberoglu A, Mihmanli I, et al. MRI appearances of inflammatory vertebral osteitis in early ankylosing spondylitis. Pediatr Radiol. 2002;32(3):191-194.
83 Shaw NE. The syndrome of the prolapsed thoracic intervertebral disc. J Bone Joint Surg. 1975;57:412.
84 Gelch MM. Herniated thoracic disc at T1–2 level associated with Horner’s syndrome. J Neurosurg. 1978;48:128-130.
85 Tahmouresie A. Herniated thoracic intervertebral disc – an unusual presentation: Case report. Neurosurgery. 1980;7:623-625.
86 Child DL, Yates DAH. Radicular pain in diabetes. Rheumatol Rehabil. 1978;17:195-196.
87 Barnsley L. Steroid injections: effect on pain of spinal origin. Best Pract Res Clin Anesthesiol. 2002;16(4):579-596.
88 Herzog W, Conway PJ, Kawchuk GN, et al. Forces exerted during spinal manipulative therapy. Spine. 1993;18:1206-1212.
89 Schiller L. Effectiveness of spinal manipulative therapy in the treatment of mechanical thoracic spine pain: a pilot randomized clinical trial. J Manipulative Physio Ther. 2001;24(6):394-401.
90 Pevsner Y, Shabat S, Catz A, et al. The role of radiofrequency in the treatment of mechanical pain of spinal origin. Eur Spine J. 2003;12(6):602-605.
91 Grumme T, Kolodzieyczyk D. Komplikationen in der Neurochirurgie. Berlin: Blackwell, 1994;121-202.
92 Shen WJ, Liu TJ, Shen YS. Nonoperative treatment versus posterior fixation for thoracolumbar junction burst fractures without neurologic deficit. Spine. 2001;26(9):1038-1045.
93 Rossouw JE, Anderson GL, Prentice RL, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA. 2002;288:321-333.
94 Rao RD, Singrakhia MD. Painful osteoporotic vertebral fracture. Pathogenesis, evaluation, and roles of vertebroplasty and kyphoplasty in its management. J Bone Joint Surg. 2003;85A(10):2010-2022.
95 Kim DJ, Yun YH, Wang JM. Nerve root injections for the relief if pain in patients with osteoporotic vertebral fractures. J Bone Joint Surg [Br]. 2003;85(2):250-253.
96 Ledlie JT, Renfro M. Balloon kyphoplasty: one-year outcomes in vertebral body height restoration, chronic pain, and activity levels. J Neurosurg. 2003;98(1 Suppl):36-42.
97 Lieberman IH, Dudeney S, Reinhardt MK, et al. Initial outcome and efficacy of ‘kyphoplasty’ in the treatment of painful osteoporotic vertebral compression fractures. Spine. 2001;26:1631-1638.
98 Perez-Higueras A, Alvarez L, Rossi RE, et al. Percutaneous vertebroplasty: long-term clinical and radiological outcome. Neuroradiology. 2002;44(11):950-954.
99 Fourney DR, Schomer DF, Nader R, et al. Percutaneous vertebroplasty and kyphoplasty for painful vertebral body fractures in cancer patients. J Neurosurgery. 2003;98:21-30.
100 Burton AW, Rhines LC, Mendel E. Vertebroplasty and kyphoplasty: a review. Neurosurg Focus. In Press.
101 Kostas JP, Dailianna Z, Xenakis T, et al. Back pain caused by benign tumors and tumor-like lesions of the thoracolumbar spine. Am J Orthoped. 2001;30(1):50-56.
102 Maranzano E, Latini P, Perrucci E, et al. Short-course radiotherapy (8Gy ×2) in metastatic spinal cord compression: an effective and feasible treatment. Int J Radiat Oncol Biol Phys. 1997;38(5):1037-1044.
103 Simpson BR, Parkhouse J, Marshall R, et al. Extradural analgesia and the prevention of postoperative respiratory complications. Br J Anaesth. 1961;33:628-641.
104 Carrol E, Badura A. Focal intense brief transcutaneous electric nerve stimulation for treatment of radicular and postthoracotomy pain. Arch Phys Med Rehabil. 2001;82:262-264.
105 Evans PJD, Lloyd JW, Green CJ. Cryoanalgesia: the response to alterations in freeze cycle and temperature. Br J Anaesth. 1981;53:1121-1127.
106 Moorjani N, Zhao F, Tian, et al. Effects of cryoanalgesia on post-thoracotomy pain and on the structure of intercostal nerves: a human prospective randomized trial and a histological study. Eur J Cardio-Thorac Surg. 2001;20(3):502-507.
107 Rowbotham MC, Reinser-Keller LA, Fields H. Both intravenous lidocaine and morphine reduce the pain of postherpetic neuralgia. Neurology. 1991;41(7):1024-1028.
108 Toussirot E, Wendling D. Therapeutic advances in ankylosing spondylitis. Expert Opin Investig Drugs. 2001;10(1):21-29.
109 Dougados M, Dijkmans B, Khan M, et al. Conventional treatments for ankylosing spondylitis. Ann Rheumat Dis. 2002;61:3.
110 Austin GP, Benesky WT. Thoracic pain in a collegiate runner. Man Ther. 2002;7(3):168-172.