CHAPTER 44 Thoracic Disc Disease
Historical Background
In 1838, Key1 wrote the first report of a thoracic herniated disc causing spinal cord compression. Middleton and Teacher2 reported the second case 73 years later. The first reported surgical treatment of a thoracic herniated disc was in 1922 by Adson, who performed a laminectomy and disc removal.3 In their classic 1934 monograph on ruptured intervertebral discs, Mixter and Barr4 described four cases of thoracic disc herniation; two of three patients treated surgically via laminectomy were rendered paraplegic, emphasizing the challenge in the management of the disease. In the ensuing years, many reports helped define the disease and document that treatment by laminectomy was unpredictable and very risky.3,5–16
The costotransversectomy approach was introduced by Menard17 in 1900. Capener18 later modified the procedure for use in the treatment of Pott disease. At Alexander’s suggestion, Hulme19 was the first to use this approach in the management of a herniated thoracic disc. Hulme19 reported his experience with six patients treated by costotransversectomy and showed that it was a safer, more effective approach than laminectomy. In a later literature review of 49 surgical cases using costotransversectomy, Arce and Dohrmann20 noted 82% of patients improved, the condition was unchanged in 14% of patients, and only 4% of patients experienced worsening of their condition.
Hodgson and Stock21 popularized the anterior approach to the spine for the treatment of Pott disease. In 1958, Crafoord and colleagues22 reported the first transthoracic procedure on the spine for a herniated disc. They performed a fenestration, or windowing of the disc without any attempt at disc removal or cord decompression. The one patient described in their article did well. Simultaneous reports by Perot and Munro23 and Ransohoff and colleagues24 in 1969 established transthoracic spinal cord decompression as a viable alternative to costotransversectomy. The posterolateral approach to the thoracic disc space was described by Carson and colleagues25 in 1971 and was modified by Patterson and Arbit26 in 1978.
All the surgical approaches have undergone minor modifications, including the application of microsurgical techniques.27–29 Developments in the use of video-assisted thoracoscopic surgery (VATS) have provided an additional option in surgical treatment of a symptomatic thoracic herniated disc.30–33 Each technique has advantages and disadvantages, and all but laminectomy are currently acceptable.
The diagnostic use of MRI has had a profound influence on the treatment of thoracic disc herniation.34–42 At most centers, MRI has replaced myelography as the standard for the diagnosis of this condition. Because MRI is rapid, noninvasive, and increasingly available, its use is likely to decrease delay in diagnosis and lead to earlier treatment and perhaps improved prognosis. A new challenge is likely to be avoiding overdiagnosis and unnecessary operations on asymptomatic lesions.41,43
Epidemiology
The true incidence of thoracic herniated discs is unknown; many cases are unrecognized, or patients are asymptomatic. Most patients are in the 4th through 6th decades of life (Fig. 44–1).3,6,44,45 In a review of 288 cases reported in the literature, Arce and Dohrmann44 noted a slight male preponderance (1.5:1), although most series show an approximately even sex distribution.5,11,46,47 Cases have been reported in patients ranging in age from 11 to 75 years.25,48,49
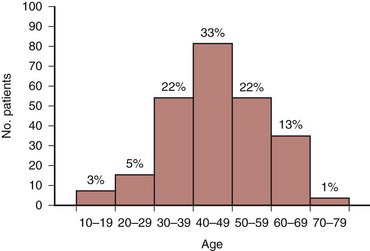
FIGURE 44–1 Distribution of 280 cases of thoracic disc herniation according to age.
(From Arce CA, Dohrmann GJ: Herniated thoracic disks. Neurol Clin 3:383-392, 1985.)
Historically, only 0.15% to 4% of all symptomatic protrusions of an intervertebral disc are in the thoracic spine.3,5,6,12,44,50–52 Surgically, thoracic disc excision accounts for 0.2% to 1.8% of all operations performed on symptomatic herniated discs.5,29,39,44,53–56 In 1950, Love and Kiefer47 reported on 17 cases seen over 26 years. Logue12 reported a thoracic herniated disc in 11 of 250 discectomies (4%). Otani and colleagues51 later reported symptomatic thoracic disc herniation in 15 of 857 discectomies (1.8%) over a 15-year period. In a cadaveric study, Haley and Perry57 showed that 11% of unselected autopsies revealed protruded thoracic discs; 2 of 99 specimens in their series had discs protruding 4 to 7 mm into the canal. The prevalence of herniated thoracic discs with an associated neurologic deficit has been estimated to be 1 per 1 million population.25,42,47,52,58
Improvements in imaging techniques have resulted in an increased detection of thoracic abnormalities and, concurrently, of herniated thoracic discs. Ryan and colleagues59 reviewed 270 patients undergoing computed tomography (CT) of the thorax for suspected malignancy and found 4 (1.5%) who had asymptomatic calcified herniated thoracic discs. In a retrospective review of combined CT and myelography in 360 patients, Awwad and colleagues60 found 54 herniations of a thoracic disc in 40 patients (11%) who were asymptomatic. In their study, 88% of the asymptomatic thoracic discs showed some deformity of the spinal cord; there was no single feature or combination of features clearly separating asymptomatic from symptomatic thoracic herniated discs.
The advent of MRI and its inherent sensitivity has increased further the reported incidence of thoracic disc herniations. Williams and colleagues41 retrospectively reviewed 48 patients who underwent MRI for oncologic evaluation and reported a thoracic herniated disc in 7 (15%). Ross and colleagues39 diagnosed 20 cases (16 confirmed) by MRI in a 2-year period compared with the initial report of Love and Kiefer47 in 1949 of 17 cases seen over a 26-year period. Wood and colleagues42 reported 66 of 90 asymptomatic individuals (73%) had positive anatomic findings at one or more thoracic levels; findings included herniation of a disc in 33 subjects (37%), bulging of a disc in 48 (53%), an annular tear in 52 (58%), and deformation of the spinal cord in 26 (29%). Wood and colleagues42 reported no association between age and the prevalence of disc herniation. Compared with the MRI findings of 18 patients treated operatively for thoracic disc herniations in their study, the overall prevalence of these findings in the group that had thoracic pain was not significantly different from the asymptomatic population.
Williams and colleagues41 suggested that thoracic disc herniation may be common enough to be considered a normal variant on MRI. More recently, Niemelainen and colleagues61 reported that degenerative thoracic MRI changes were less common than previously reported. In a cross-sectional study of men 35 to 70 years old from the Finnish Twin Cohort study, only 9.2% of subjects had posterior disc bulging. Anterior disc bulging was much more common, found in 45.2%. The presence of anterior disc bulging was positively correlated with age (r = 0.15 to 0.23, P < .005). Moderate to severe disc height narrowing ranged from 5.4% to 9.5% by level in the thoracic spine.
Etiology
Most authors favor degenerative processes as the major cause of thoracic disc herniation.3,20,57 This theory is supported by the higher incidence of herniation in the thoracolumbar spine, where greater degenerative changes occur.34,40,62 In a review of MRI findings and their relationship to thoracic and lumbar disc degeneration in a cohort of 232 subjects, Videman and colleagues40 noted that moderate and severe osteophytes were most common at the T11-12 level (20.7% of subjects); upper endplate irregularities were most common at levels T8-12, typically in the middle of the endplates in the thoracolumbar spine compared with more peripheral endplate changes in the lumbar spine. These results were later supported by Niemelainen and colleagues,61 who reported moderate to severe disc height narrowing in 21.4% of subjects.
The role of trauma as a cause of herniated thoracic discs is controversial. A history of trauma can be elicited in 14% to 63% of patients.35,45 The mean prevalence in 10 random series was 34%. In some patients, the causal relationship is undeniable; in others, trauma may have been an aggravating factor or purely coincidental. The degree of reported trauma responsible for herniation ranges from minor twisting strains and chiropractic manipulation to major falls or motor vehicle accidents.63
Several authors35,54,64 have suggested an association between Scheuermann disease and herniated thoracic discs. The primary pathogenic process of the disease or secondary disc degeneration may be the factors promoting herniation. Wood and colleagues42 noted that endplate changes consistent with Scheuermann disease were more prevalent in their symptomatic patient group than in the asymptomatic population.
Pathogenesis
The pathogenesis of neurologic compromise secondary to herniated thoracic discs is believed to be a combination of direct neural compression and vascular insufficiency.2,3,6,12,26 Middleton and Teacher2 suggested this in a case reported in 1911. Severe back pain developed while this patient was lifting a heavy object. Approximately 20 hours later, he felt a sudden severe pain shoot from his chest to his feet and he became almost completely paraplegic. The patient died 16 days later of urosepsis. The autopsy revealed a herniated thoracic disc opposite a section of cord that was compressed, degenerated, and hemorrhagic. A thrombosed vessel was found in the section of cord showing the most hemorrhage.
Several anatomic features make the thoracic cord vulnerable to manipulation and trauma.26 The thoracic spinal canal is small, and most of its available space is occupied by the cord. The blood supply to the cord is tenuous in this region, especially in the “critical zone” of T4-9.65 In addition, thoracic disc protrusions are more common centrally than laterally, are often calcified, and may adhere to or penetrate the dura.*
The theory of direct compression causing neural compromise is supported by the report by Logue12 of a patient who died after a 14-month course of progressive paraplegia. The autopsy showed extreme distortion of the cord, but the anterior spinal artery and vein were patent and showed no evidence of damage. Kahn68 suggested that, in addition to direct anterior compression by the herniated disc, the dentate ligaments may resist posterior displacement of the cord, leading to traction and distortion of neural structures.
Vascular insufficiency has been the explanation for unusual cases, such as cases with transitory paresis and instances in which the segmental level of involvement was higher than expected from the location of the herniated disc.3,6 Significant neural deficits may be caused by herniations that appear too small to cause significant compression. This theory also helps explain patients who show no improvement after complete decompression and patients who had an abrupt onset of paraplegia in the presence of a chronic calcified disc. The theory is supported by patients in whom the disc herniation has been shown to cause anterior spinal artery thrombosis.12
Doppman and Girton69 performed an angiographic study on the effect of laminectomy in the presence of acute anterior epidural masses. They found that when decompression restored normal arteriovenous hemodynamics, the animals were neurologically intact despite significant cord distortion. When either the artery or the vein remained obstructed, however, the animals remained paraplegic.
Clinical Presentation
In symptomatic cases, the condition is dynamic and can progress.9 Tovi and Strang16 outlined the usual chronologic progression, which begins with thoracic pain followed by sensory disturbances, weakness, and finally bowel and bladder dysfunction. Arce and Dohrmann20 confirmed this pattern in their review of the literature: Of 179 patients who described their initial symptoms, 57% described pain, 24% described sensory disturbance, 17% described motor weakness, and 2% described bladder dysfunction (Table 44–1). By the time of presentation, 90% of the patients had signs and symptoms of cord compression, 61% had motor and sensory complaints, and 30% had bowel or bladder dysfunction (Table 44–2). The duration of symptoms before presentation ranged from hours to 16 years in one series.3 In a report of 55 patients initially treated conservatively, Brown and colleagues70 reported anterior bandlike chest pain as the most common early symptom in 67% of patients; lower extremity complaints were present in 20% of patients and ranged from paresthesia (4%) to frank muscle weakness (16%). Additional symptoms included intrascapular pain (8%) and epigastric pain (4%).
| Symptom | No. Patients (%) |
|---|---|
| Pain | 102 (57) |
| Sensory | 42 (24) |
| Motor | 31 (17) |
| Bladder | 4 (2) |
From Arce CA, Dohrmann GJ: Herniated thoracic disks. Neurol Clin 3:383-392, 1985.
TABLE 44–2 Presenting Features of Thoracic Disc Herniation
| Feature | No. Patients (%) |
|---|---|
| Motor and sensory signs and symptoms | 131 (61) |
| Brown-Séquard syndrome | 18 (9) |
| Sensory signs and symptoms only | 33 (15) |
| Motor signs and symptoms only | 13 (6) |
| Radicular pain only | 20 (9) |
| Bladder or sphincter features | 65 (30) |
From Arce CA, Dohrmann GJ: Herniated thoracic disks. Neurol Clin 3:383-392, 1985.
Thoracic pain can be midline, unilateral, or bilateral, depending on the location of the herniation. In some cases, there may be no pain. Coughing and sneezing may aggravate pain, as with herniated discs in the cervical and lumbar regions. With herniation of the T1 disc, the pain may be in the neck and upper extremity and simulate a cervical disc problem, causing upper extremity numbness, intrinsic muscle weakness, and Horner syndrome.5,26,71
When the herniation is in the mid-thoracic spine, radiation of pain into the chest or abdomen can simulate cardiac or abdominal disease, clouding an already complex clinical picture. In the four cases reported by Epstein,7 one patient underwent an unnecessary thoracotomy for excision of a pericardial cyst, hysterectomy and salpingo-oophorectomy were performed in another patient, and a third patient almost underwent an abdominal exploration for endometriosis before the true cause of her symptoms was identified. Pain from a lower thoracic disc herniation may radiate to the groin or flank and simulate ureteral calculi or renal disease.62,72,73 Abdominal wall paresis and abdominal hernia have also been presenting signs for thoracic disc herniations.74,75 Herniated discs at the lowest thoracic levels can impinge on the cauda equina and on the distal spinal cord causing lower extremity pain or weakness and mimic a herniated lumbar disc.76,77 On physical examination, flexion of the neck may induce back or root pain with lesions below the mid-thoracic level.25 A thorough neurologic examination is mandatory, and the examiner should pay close attention to long tract signs and other evidence of myelopathy.
Some investigators believe that the occurrence of pronounced sensory changes with relatively minor motor deficits is highly suggestive of a herniated thoracic disc.25,78 Sensory disturbances, motor weakness, sphincter dysfunction, and gait abnormalities should direct the examiner’s attention to the nervous system as the source of the problem.
Level and Classification of Herniation
Three fourths of cases occur between T8 and L1; the peak is at T11-12, where 26% to 50% of herniations occur (Fig. 44–2).20,40 Herniations are uncommon in the upper thoracic spine.20,26,71 Haley and Perry57 found a similar distribution in their cadaveric study of 99 spines and theorized that the increased incidence in the thoracolumbar area is due to the greater degree of motion in this region. The reason that the incidence at T11-12 is greater than that at T12-L1 (9%) may be the facet orientation. Malmivaara and colleagues79 believed that the coronally oriented facets in the upper thoracolumbar region have less torsional resistance than the sagittally oriented facets at T12-L1, so the T11-12 disc is exposed to greater stress and has a high likelihood of degeneration.
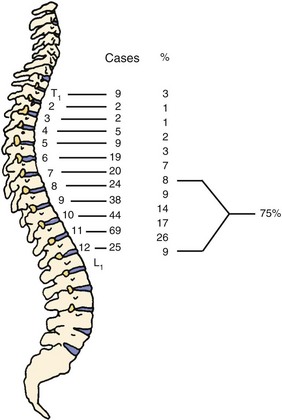
FIGURE 44–2 Levels of thoracic disc protrusion in 280 cases.
(From Arce CA, Dohrmann GJ: Herniated thoracic disks. Neurol Clin 3:383-392, 1985.)
Herniated thoracic discs can be classified by location or by symptoms. Most authors describe the location of the herniation as central, centrolateral, or lateral, and roughly 70% of the cases are either central or centrolateral.20,60 In a comparison of characteristics on CT myelography of asymptomatic and symptomatic herniated thoracic discs, Awwad and colleagues60 reported that 90% of herniations were central or parasagittal versus lateral in asymptomatic patients, whereas 80% were central or parasagittal in symptomatic patients. No identifiable radiographic features could reliably classify a herniated disc as symptomatic or asymptomatic. Abbott and Retter5 classified cases by symptoms and reported that lateral protrusions cause root compression and that patients have radicular pain and minimal or no signs of cord compression. Patients with central disc herniation in the upper and middle thoracic spine can have myelopathy. Protrusions at T11 and T12 compress the conus and cauda equina and may cause pain referred to the lower limbs and sphincter disturbance.
Few cases of intradural herniation of thoracic discs have been reported, suggesting that the incidence is low.3,8,16,26,80–84 Love and Schorn3 reported a series of 61 cases in which 7 (11%) showed disc erosion through the anterior dura. In a review of the literature, Epstein and colleagues81 noted that 5% of all intradural disc herniations were found in the thoracic spine. Similar to the cervical spine, the low incidence was attributed to the lack of significant dural adhesions of the thoracic dura to the posterior longitudinal ligament and anulus fibrosus. Patients with intradural thoracic disc herniations tended to present with a higher incidence of Brown-Séquard syndromes and paraplegia.44 In most cases, the presence of an intradural thoracic disc herniation is not identified preoperatively. CT myelography seems to have a higher sensitivity to detect this than MRI even with the addition of gadolinium.80
The exact incidence of multilevel herniations is unknown.5,14,35,85 Arseni and Nash6 reviewed the literature in 1960 and found multiple herniations in only 4 of 106 cases reported. A report by Bohlman and Zdeblick35 suggested, however, that the incidence may be much higher than previously recognized. Of their 19 patients, 3 (16%) had herniations at two levels. The sensitivity of MRI may be partially responsible for this increased frequency.37,39 Ross and colleagues39 reported that 3 of 13 patients (23%) whose herniation was diagnosed by MRI had multilevel involvement; Wood and colleagues42 reported multiple disc herniations in 39% of asymptomatic volunteers that were diagnosed by MRI. These rates are similar to the findings in the autopsy study by Haley and Perry,57 in which two of seven patients had more than one protruded disc.
Van Landingham64 suggested an association between Scheuermann disease and multilevel herniation. Wood and colleagues42 noted that endplate changes consistent with Scheuermann disease were more prevalent in the group with thoracic pain and disc herniation than in the asymptomatic population. Conversely, Lesoin and colleagues54 reported six cases of single-level herniations only in patients with Scheuermann disease, suggesting a lack of significant association with multiple herniations.
Natural History
There are few long-term reports of untreated adults with herniated thoracic discs. In 1992, Brown and colleagues70 reported a 2-year follow-up on 55 patients found to have thoracic disc herniation on MRI and concurrent pain; 11 (20%) initially had lower extremity complaints. Initial treatment in 54 patients included bed rest; nonsteroidal anti-inflammatory drugs; and controlled physical therapy involving hyperextension strengthening, postural training, and body mechanics education. Ultimately, 15 patients (27%) underwent operation. Of the remaining 40 patients treated nonoperatively, 31 (78%) returned to their prior level of activity. Nine of the 11 patients presenting with lower extremity complaints of pain or weakness underwent operation; 55% of herniated discs in the operative group were at or below T9. In contrast, 48% of the discs in the nonoperative group were at T6-9.
In patients with lower extremity complaints, the natural history of the disorder is typically one of progression, and nearly all patients eventually undergo operation for progressive neurologic deficit or unremitting pain.3,11 The most characteristic chronologic progression of symptoms is pain followed by sensory disturbance, weakness, and bowel and bladder dysfunction.16 The course can be extremely variable, however, and it is unknown whether neurologic signs or symptoms ever would have developed in patients operated on for pain alone. Some patients might have improved spontaneously if not subjected to surgical treatment. Haro and colleagues86 reported on two patients with acute onset of symptomatic thoracic disc herniation with signs of myelopathy that resolved without surgery. Both patients had lower extremity signs of myelopathy, but neither developed bladder dysfunction or progressive motor weakness. Treatment with steroids and prostaglandin E1 led to resolution of symptoms and resorption of thoracic disc herniation on follow-up MRI scans.
Arseni and Nash6 described two general patterns for the time course of symptoms. The first, which occurs in younger patients with a history of trauma, is backache that can be followed by a rapidly evolving myelopathy. In the second pattern, which typically occurs in patients past middle age who have degenerative disc disease without any significant trauma, signs and symptoms of cord compression develop slowly and progressively. Tovi and Strang16 found that when the first symptom to develop was unilateral, the course tended to be one of slow progression with periods of stabilization and occasional slight remission. Rapid, irreversible progression generally was noted in cases with a bilateral onset.
Calcification of the disc in children is considered to be a painful but self-limited process, with eventual resolution of the pain and resorption of the calcified deposit. It generally occurs in the cervical spine. About half of cases are preceded by a history of trauma (30%) or upper respiratory tract infection.87,88 The natural history of herniated calcified thoracic discs in children was reviewed by Nicolau and colleagues.89 The course was similar to cases without herniation; the patients improved spontaneously, and the calcified fragment resorbed. The progression is not always benign, however. Two cases in children have been reported in which myelopathy developed from cord compression and required operation.13,67
Disc calcification in adults differs from that in children. The thoracolumbar spine is the most frequent site of calcification, and the condition is generally asymptomatic unless herniation of the disc occurs.87 The deposits may accelerate degeneration by interfering in the biomechanics and nutrition of the disc.87,90 Disc calcification is found on routine radiographs in 4% to 6% of patients without disc herniation compared with up to 70% of patients with disc prolapse.12,87 The natural history of disc herniation in adults has not been conclusively shown to be altered by disc calcification.
Differential Diagnosis
Love and Schorn3 reported that before myelography the correct diagnosis was made in 13 of 61 patients and was considered in the differential diagnosis in only 7 others; even after myelography, the correct diagnosis was made preoperatively in only 56% of patients. With greater awareness of the diagnosis and improved imaging techniques now available, the correct diagnosis should be made before operation in almost all cases.
The differential diagnosis of back pain includes spinal tumors and infections, ankylosing spondylitis, fractures, intercostal neuralgia, herpes zoster, and cervical and lumbar herniated discs. Diseases of the thoracic and abdominal viscera may have a similar presentation. Neurosis is another possibility. The differential diagnosis of myelopathy includes demyelinating and degenerative processes of the central nervous system, such as multiple sclerosis and amyotrophic lateral sclerosis.91,92 Intraspinal tumors, brain tumors, and cerebrovascular accidents also should be considered.20,63
In patients who have a neurologic deficit and radiographic evidence of Scheuermann disease, the differential diagnosis includes an extradural cyst or compression from an angular kyphosis.54,93 In the series by Lesoin and colleagues,54 the mean age of the patients who had a herniated thoracic disc in association with Scheuermann disease was 44 years, similar to the population without Scheuermann disease. This is in contrast to a mean age of 17 years in three patients in whom neurologic compromise developed secondary to bony cord compression at the apex of the kyphosis.93
Diagnostic Evaluation
Spine Radiographs
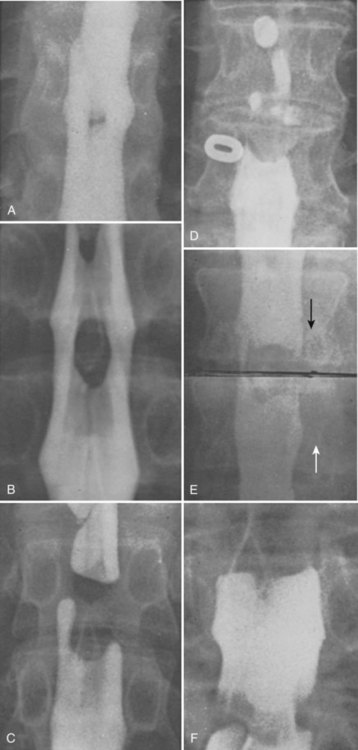
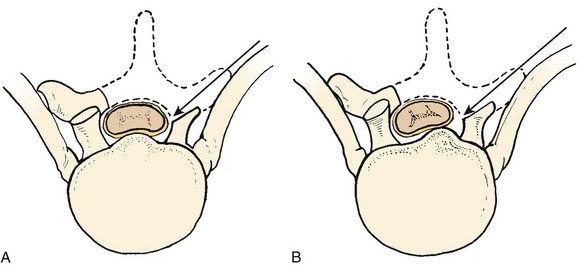
Plain radiographs of the spine generally are diagnostic only if they show disc calcification. The calcified disc is not always the one that is herniated, but the association at least suggests the diagnosis.3,94 A calcified disc in the canal is pathognomonic of disc herniation.12,27,28,94 Baker and colleagues94 identified two radiographic patterns of calcification (Fig. 44–3). One consisted of extensive calcification posteriorly in the interspace and bulging into the canal. The other pattern, which is subtle and often overlooked initially, is a small nidus just posterior to the narrowed interspace. Studies35,59 of adult lumbar discs have shown that the deposits may be calcium pyrophosphate dihydrate or calcium hydroxyapatite. The clinical significance of the different radiographic patterns or chemical compositions has not been determined.

FIGURE 44–3 Plain radiographs can be used to diagnose herniated discs only when calcification is seen within spinal canal. A, Large calcified disc within canal (arrows) is nearly obscured by overlying ribs (see Figs. 44-7 and 44-8 for CT and MRI scans from same patient). B, Tiny nidus of calcium is visible in canal posterior to narrowed 11th interspace (arrow).
The proposed association between Scheuermann disease and herniated thoracic discs has been discussed previously. A patient found to have kyphosis with vertebral body wedging and endplate irregularity in association with back pain or a neurologic deficit should undergo other studies to eliminate the possibility of a herniated disc. Other radiographic findings, such as narrowing and hypertrophic changes, are nonspecific and are not helpful in the diagnosis.3,12,94
Myelography
The thoracic spine is difficult to image by myelography because of the thoracic kyphosis and superimposition of mediastinal structures. Myelography alone is diagnostic in only 56% of cases and has a false-negative rate of 8%.3 A complete block is found in 10% to 15% of cases.16,94 Myelography is performed by injecting water-soluble contrast agent in the lumbosacral canal, removing the spinal needle, and placing the patient supine so that the contrast agent pools in the dependent thoracic kyphosis.36 Anteroposterior and lateral films are essential. A herniated disc appears as a central filling defect at the level of the disc space (Fig. 44–4). Central protrusions produce discrete oval or round filling defects. In large protrusions, a complete block occurs with a blunt, convex leading edge.12,94 Lateral discs produce triangular or semicircular indentations with displacement of the cord to the opposite side (Fig. 44–5).94 Evaluation of cerebrospinal fluid at the time of myelography is nonspecific.9 The protein content is increased in less than 50% of patients and helps only to focus attention on the central nervous system. It generally is in the range of 50 to 100 mg/dL but may be greater than 400 mg/dL.53 Currently, myelography is most helpful in localizing lesions to allow directed CT and in preparation for operation.35,95
Computed Tomography
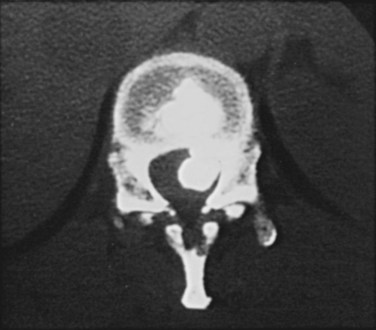
Enhanced CT after myelography with a water-soluble contrast agent is an extremely valuable technique and has been the diagnostic standard (Fig. 44–6).35,36,39,44,50,60 When combined with standard myelography, CT not only improves sensitivity and accuracy, but also detects intradural penetration of the disc.44,81
CT alone may be helpful when the disc is calcified (Fig. 44–7), but it is impractical to image the entire thoracic spine and it is not as sensitive as CT with intrathecal injection of a contrast agent.65 The criterion for diagnosis of a herniated disc by CT is a focal extension of the disc beyond the posterior aspect of the vertebral body with spinal cord compression or displacement.39
Magnetic Resonance Imaging
MRI has revolutionized the diagnostic evaluation of thoracic disc disease. Some centers rely on MRI almost exclusively, but others still perform myelography and CT when operative treatment is being considered.35–37 MRI is a rapid, noninvasive outpatient procedure that does not use ionizing radiation and causes no morbidity. It is a sensitive and specific technique that makes it easy to obtain sagittal sections of the entire thoracic spine.36,37,39 Findings on MRI are similar to findings of myelography and CT, but it is necessary to use information from sagittal T1-weighted and T2-weighted and axial T1-weighted images to achieve similar sensitivity (Fig. 44–8).39
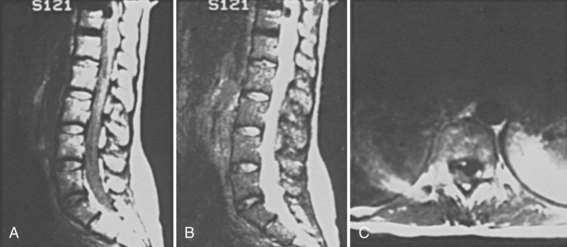
FIGURE 44–8 MRI of the patient in Figure 44–7 showing large, calcified, herniated thoracic disc at T11-12. A, T1-weighted sagittal image. B, T2-weighted sagittal image. C, T1-weighted axial image.
MRI is a highly technical procedure; the expertise of the radiologist and the design of the scanner determine the accuracy of the test to a great degree. There are pitfalls of MRI, such as partial volume averaging (owing to the relatively large section thickness), the cerebrospinal fluid flow void sign (regions of low signal intensity within the fluid owing to its pulsatile motion), signal dropout from calcified discs, chemical shift artifacts from marrow fat, and mismapped signal from cardiac motion.36,39,96 Addition of gadolinium as a contrast agent has been reported to help in differentiating between thoracic disc herniations and small meningiomas; herniated disc material does not enhance, whereas spinal meningiomas show a very early, homogeneous, and intense uptake of contrast agent.38
Despite improved imaging and increased sensitivity, findings of thoracic disc herniation on MRI must be interpreted with caution and closely correlated with clinical findings. Several reports noted significant disc protrusion and spinal cord deformation in 30% of asymptomatic individuals.42,60 In their large MRI series, Wood and colleagues42 noted that the overall prevalence of thoracic disc herniation in the group with thoracic pain was not significantly different from the asymptomatic population.
Discography
The general sensitivity but lack of specificity of thoracic MRI in diagnosing painful thoracic disc disease sometimes may require the supplemental use of provocative discography to identify a specific thoracic disc pain source. In a retrospective review, Schellhas and colleagues97 showed thoracic discography as a safe and reliable technique.
In a controlled prospective study, Wood and colleagues98 compared MRI and discography in asymptomatic and symptomatic individuals. In asymptomatic volunteers, the mean pain response with discography was 2.4 out of 10. On discography, 27 of 40 discs were abnormal, with endplate irregularities, annular tears, or herniations. Ten discs read as initially normal on MRI showed annular pathology on discography. In symptomatic patients with chronic thoracic pain, the pain response with discography was 6.3 out of 10. Of the 49 discs studied in this group, 55% had a concordant pain response, 39% had a discordant pain response, and 6% had no pain. On MRI, 21 of 49 discs appeared normal; however, on discography, only 10 were judged as normal. The only correlative pathology seemed to be Scheuermann endplate pathology as seen on MRI and Schmorl nodes as seen on discography.
In a systematic review of the literature, Buenaventura and colleagues99 reported there is limited evidence to support the role of discography for the diagnosis of chronic thoracic discogenic pain. Given the general prevalence of degenerative thoracic disc pathology in asymptomatic individuals, discography apparently should be reserved for individuals with interdiscal pathology on MRI and thoracic axial pain unresponsive to an appropriate duration of nonsurgical treatment.
Treatment
Indications for surgery include (1) progressive myelopathy, (2) lower extremity weakness or paralysis, (3) bowel or bladder dysfunction, and (4) radicular pain refractory to conservative measures. Brown and colleagues70 reported that 77% of patients with radicular pain as the primary presentation improved after a course of physical therapy. In cases of radicular presentation only, some authors believe that if the protrusion is far lateral with nerve root compression only, the situation is not urgent, and the decision to operate should be based on the degree of pain.7 Conversely, there have been reports of lateral lesions causing severe neurologic deficits from compression of a major medullary feeder vessel.55 Small herniations also should be respected because abrupt, severe, and irreversible deficits can occur; some investigators have concluded that there is no relationship between the size of the herniation and the gravity of the clinical picture.11,27
In cases of myelopathy and lower extremity involvement, most authors recommend early decompression. In cases of late treatment, favorable results are still possible despite significant delays and the presence of major neurologic deficits.35 A less aggressive approach may be taken in children because the natural history of the disorder seems to be different.89
The surgical management of this disorder has evolved in recent years. Laminectomy with disc excision was the benchmark approach 30 years ago but has been abandoned because of the risk of neurologic deterioration (Fig. 44–9). After the introduction of alternative techniques of decompression, Ravichandran and Frankel100 noted a significant decrease in admission to spinal cord injury centers of patients with paralysis after treatment of herniated thoracic discs. In a review of 135 cases, Arce and Dohrmann20 found that after laminectomy 58% of the patients were improved, 10% were unchanged, 28% were worse, and 4% had died. There is also evidence that patients who do not improve or who are made worse by laminectomy are less likely to be helped by later anterior decompression.91 The best results are achieved in patients who have lateral lesions above T11, who have minimal neurologic deficits, who have a soft disc, and who are operated on early after the onset of symptoms.* Patients with myelopathy caused by ossification of the posterior longitudinal ligament have worse rates of recovery.101 Although laminectomy is still occasionally advocated for lateral lesions, most authors think that the procedure is contraindicated.28,103
Singounas and Karvounis104 described good results in patients treated by decompressive laminectomy alone without attempted disc removal. Several studies8,12 described disastrous results with this technique, however. Studies in animals found consistent neurologic deterioration after decompressive laminectomy alone for anterior epidural masses.69,105
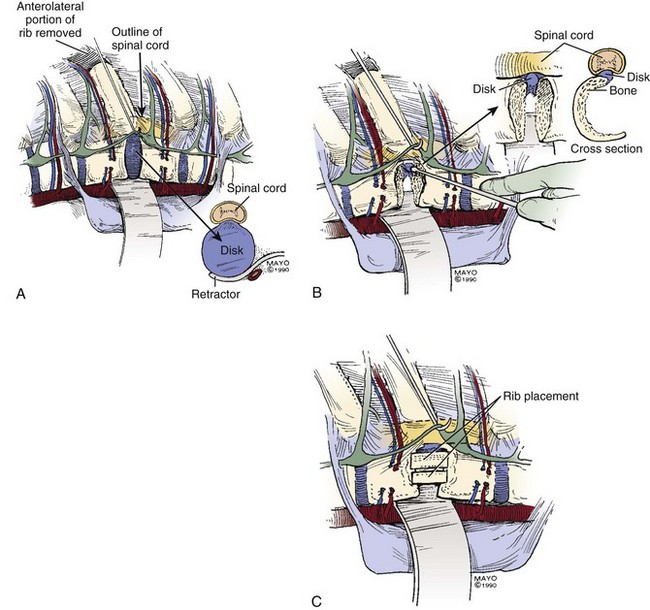
Costotransversectomy is an effective technique for managing herniated thoracic discs (Fig. 44–10).10,45,106 Disc excision is performed through a paramedian incision with the patient prone10 or in a modified lateral decubitus position.106 The paraspinal muscles are either retracted medially or split transversely.10,45 The posterior portion of each rib on the side of the herniated disc is excised, and the pleura is mobilized and reflected anterolaterally. The transverse processes and remaining head and neck of each excised rib are removed. The intervertebral foramen is located by tracing the intercostal nerve medially. The foramen is enlarged by partial removal of the corresponding pedicles, and the dural sac is exposed. A cavity is created in the posterior aspect of the bodies and disc, allowing gentle removal of disc fragments through the defect without manipulation of the spinal cord.10,45,107,108
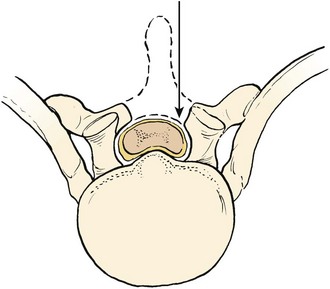
Transthoracic spinal cord decompression has been shown to be a viable alternative to costotransversectomy (Fig. 44–11).23,24 Advantages include a more direct approach to the lesion and better visualization, facilitating excision of central herniations and herniations with intradural penetration. Disadvantages of the procedure include the potential complications associated with a thoracotomy.
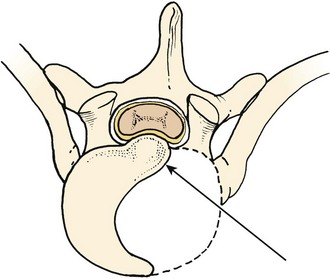
FIGURE 44–11 Transthoracic decompression allows the most direct approach to lesion without manipulation of cord.
Although many complications have been described after thoracotomy for other disorders, few have been reported after discectomy.* The results of transthoracic decompression are similar to results of costotransversectomy. In 53 cases collected from the literature, 52 patients improved, and 1 was unchanged. Bohlman and Zdeblick35 reported the outcome in 19 patients treated by costotransversectomy or transthoracic decompression. The two poor outcomes in their series were in cases treated by costotransversectomy. They concluded that the transthoracic approach with its superior exposure was the preferred procedure.
Some authors23,24,49,82,111 recommended preoperative angiography to determine the location of the artery of Adamkiewicz and other major medullary feeder vessels. If such a vessel is found at the level of the disc herniation, the spine could be approached from the opposite side. Alternatively, by carefully avoiding dissection in the neural foramina, this problem can be obviated without the need for an arteriogram. There is generally abundant collateral circulation in the region of the neural foramina that provides blood flow to the cord even with ligation of the artery of Adamkiewicz.65,112,113 The authors routinely ligate the segmental vessels adjacent to the herniated disc midway between the foramina and the aorta and have not observed any untoward effects (Fig. 44–12).91
The patient is placed in the lateral decubitus position. A lateral prolapse is best approached from the ipsilateral side; a midline herniation may be approached from either side. In the upper or middle thoracic spine, the right side has the advantage of avoiding the great vessels and the heart. There also is statistically less risk to the artery of Adamkiewicz because this vessel is on the left in approximately 80% of the patients.65 When the herniation is in the lower thoracic spine, a left thoracotomy is preferred because it is easier to mobilize the aorta than the vena cava, and the liver does not crowd the field.23,35
The level of rib resection is chosen to give the most direct access to the affected disc (see Fig. 44–12A). A horizontal line drawn on a chest radiograph from the disc space to the chest wall intersects the rib that should be resected. This is generally one to two ribs above the affected disc in the middle and lower thoracic spine.82 In the upper thoracic spine, the exposure is limited by the scapula, and it is generally necessary to excise the fifth or sixth rib and then work craniad.
The recommended extent of bone and disc removal varies from a relatively small trough in the posterior aspect of the disc to complete discectomy with partial corpectomy of the adjacent bodies (see Fig. 44–12B).23,28,35,82,91 The authors believe that the latter approach is safer because it provides the greatest degree of visualization and allows complete discectomy without disturbing the foraminal vessels. In either case, great care is taken to perform the decompression without any manipulation or pressure to the spinal cord.
Fusion is indicated when stability is compromised by the decompression and in cases associated with Scheuermann disease.45 When only a small amount of bone and disc is excised, fusion generally is not recommended.23,28,35,82 Conversely, with complete discectomy, fusion is mandatory (see Fig. 44–12C). In addition to providing stability, fusion may limit local pain secondary to motion of the degenerated segment. Recurrence of thoracic disc herniation has not been reported, but complete discectomy and fusion theoretically is the best way to prevent this complication. At the conclusion of the procedure, a chest tube is placed and attached to water-seal suction. If fusion has been performed, a thoracolumbosacral orthosis brace should be used.
Otani and colleagues49 described a modification of the transthoracic procedure in which the pleura is dissected away from the chest wall after rib excision. This modification allows the approach to be entirely extrapleural. Their results were similar to results in other series of transthoracic decompressions. The advantage of the technique is the avoidance of a chest tube postoperatively. Claims of a lower incidence of pulmonary complications may be more theoretical than real because few such complications have been reported.
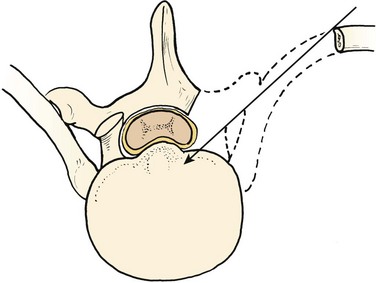
A posterolateral approach was described by Carson and colleagues25 in 1971 (Fig. 44–13). They performed a complete laminectomy of the vertebrae adjacent to the herniated disc combined with a medial facetectomy and excision of the transverse process. A T-shaped incision through the erector muscle of the spine allowed an oblique approach to the anterior epidural space. Patterson and Arbit26 modified the approach in 1978 to include the removal of the facet and pedicle of the vertebra caudal to the protruded disc through a straight midline incision. The central portion of the disc is removed by creating a cavity. The protruded material is excised by reduction of disc and bone into the cavity before removal. After anterior decompression, a complete laminectomy can be performed. Le Roux and colleagues53 reported the results of the transpedicular approach and use of the operative microscope in 20 patients; all patients symptomatically improved postoperatively, 40% became asymptomatic, and no complications were noted.
Lesoin and colleagues27 reported good results with a slightly more extensive exposure in which the transverse process, articular facets, and portions of the adjacent pedicles are removed. The extent of bone removal requires that a fusion be performed, and these authors recommended unilateral Harrington rod instrumentation. Spinal deformity has been reported to occur after posterolateral decompression without fusion.15 In the 45 cases in the literature, 40 patients noted improvement (89%), the condition was unchanged in 3 patients, and it was worse in 1 patient; 1 patient died.30 Some authors claim that intradural disc herniation can be dealt with much more easily with this approach than with any other; however, approaching anterior dural erosion by this technique requires some degree of manipulation of the cord.97
Other, less common approaches have also been described for upper thoracic disc herniations. Ulivieri and colleagues114 described a transmanubrial osteomuscular sparing approach for T1-2 disc herniations. A transvertebral herniotomy has also been reported for a T2-3 lesion.115
Video-Assisted Thoracoscopic Surgery
The continuing evolution of VATS has provided experienced surgeons an alternative approach for thoracic disc herniation decompression. The technique of VATS was first described by Mack and colleagues116 in 1993 for the drainage of thoracic paravertebral abscess. In 1994, Horowitz and colleagues117 reported the clinical application of VATS for the treatment of thoracic disc herniation. Subsequently, several authors reported larger clinical series documenting the outcome of VATS-treated thoracic disc herniation.1,19,30–32,56,118,119
Reported advantages of VATS include reduced perioperative morbidity from minimal surgical dissection and avoidance of rib resection or spreading, enhanced visualization for the operating surgeons and support team, reduced postoperative pain with improved ventilatory excursion, shorter hospitalization and rehabilitation, and consequent decreased overall medical costs.1,26 Disadvantages of VATS include the required coordination of two operative surgeons, an acquired technical skill set with a steep learning curve, specialized thoracoscopic instrumentation, and the required deflation of the ipsilateral lung for the procedure to be successful.
Indications for VATS application for thoracic disc herniation are similar to the indications for the anterior thoracic approach. The procedure can be performed in patients ranging in age from pediatric to geriatric. The minimally invasive nature of the VATS surgical approach and consequent reduced postoperative pain and inspiratory splinting make this approach applicable in patients less able to tolerate the physiologic effects of open thoracotomy, such as patients with chronic obstructive pulmonary disease or interstitial fibrosis. Patients with contraindications for VATS include patients intolerant of single-lung ventilation and patients with severe or acute respiratory insufficiency, high airway pressures with positive-pressure ventilation, and pleural scarring. Relative contraindications include previous tube thoracostomy or previous thoracotomy. For technical details of VATS technique, see Chapter 25.
In addition to numerous case reports, several authors have reported on large series of thoracic disc herniation treated by VATS.30,32,56,118,119 In 1998, Regan and colleagues32 reported their preliminary experience in 29 patients. Mean operative time was 175 minutes. The surgical complication rate was 14%, primarily from intercostal neuralgia and atelectasis. At 1-year follow-up, 76% of patients related satisfactory results; 24% of patients reported dissatisfaction or no change.
In a further extension of their series, Anand and Regan30 reported outcomes on 100 consecutive cases with minimal 2-year follow-up. In 100 patients, 117 discs were excised; 40 patients underwent fusion: 27 with autologous rib strut and 13 with a threaded interbody fusion cage. Mean operative time was 173 minutes, mean blood loss was 259 mL, and average length of stay was 4 days. The surgical complication rate was 21%; 75% of the complications were pulmonary related (pleural effusion, pneumothorax, atelectasis, and pneumonia). Intercostal neuralgia occurred in six patients (6%) early in the series and declined subsequent to use of soft flexible intercostal trocars. One patient incurred a 2500-mL blood loss; open conversion to thoracotomy was done in one patient. Five patients underwent reoperation: four for secondary fusion secondary to discogram-positive intractable axial pain and one for pseudarthrosis with a threaded interbody fusion device that was removed and replaced with rib graft strut.
Kim and colleagues118 reported on the use of VATS in 20 consecutive patients with various thoracic pathologies. These investigators found VATS to be an effective minimally invasive technique but with a steep learning curve.
McAfee and colleagues56 reported on the incidence of VATS complications in a series of 78 consecutive patients, 41 of whom underwent VATS for thoracic discectomy. Six patients showed a transient postoperative intercostal neuralgia; the incidence diminished with subsequent use of soft trocars. Atelectasis or effusion resulting in a prolonged hospital stay was seen in five patients. Blood loss greater than 2500 mL occurred in two patients. Penetration of the right hemidiaphragm occurred in one case with mild parenchymal laceration to the liver repaired thoracoscopically without postoperative sequelae. Intraoperative conversion to open thoracotomy was required in one patient secondary to scarring from a previous costotransversectomy.
Methodologic review of VATS emphasizes the necessity of initial portal placement at the midaxillary sixth or seventh intercostal space to avoid injury to vital organs. The recommended use of soft trocar portals and a meticulous technique emphasizing the constant visualization of all instrumentation tips was believed to be cardinal in the reduction of VATS-associated complications. Gille and colleagues119 reported on the results of VATS in 18 cases of hard thoracic disc herniation. In 11 of the patients, there was no definitive plane between the calcified disc and the dura. Seven patients developed a dural tear with a high risk of cerebrospinal fluid fistula. Four of these seven patients required revision surgery.
Minimally Invasive Techniques
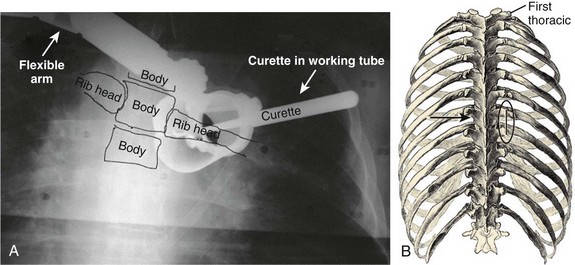
There have been several more recent reports of using minimally invasive techniques for the surgical treatment of thoracic disc herniations.120–123 In a cadaveric and initial clinical study, Lidar and colleagues122 reported the minimally invasive technique to be safe and effective. These investigators used a series of sequentially larger tubular dilators inserted on the lateral border of the rib head to allow visualization of the space between the costotransverse joint and caudal border of the costovertebral joint as shown in Figure 44–14. The joints are disarticulated, and the rib is freed and cut 2 cm distal to the costotransverse joint. The neurovascular bundle is identified and gently retracted. The transverse process is removed. The working tube is inserted deeper and medially. The pedicle is removed, starting at the foramen, allowing access to the disc.
The feasibility of this technique was first verified using four cadaveric specimens. Following that, Lidar and colleagues122 used the technique on 10 patients with myelopathy secondary to thoracic disc herniation. The mean operative time was 171 minutes (range 150 to 220 minutes), mean blood loss was 215 mL (range 60 to 350 mL), and all patients had a 1-night hospital stay and returned to work within 4 weeks. There were no documented operative or postoperative complications.
Summary
Laminectomy is no longer indicated for treatment of thoracic disc herniation because of a high risk of neurologic deterioration and the fact that it may compromise the results of later anterior decompression. Discectomy may be performed by various surgical approaches: costotransversectomy, transthoracic, posterolateral, or video-assisted. The most rational way to manage the problem may be to select the approach best suited to the disease that is present and to the surgeon’s experience. Posterolateral techniques are ideal for lateral lesions and may be the best choice for herniated discs with coexistent stenosis.124 The transthoracic approach permits the best visualization for central lesions. Upper thoracic lesions are more difficult to approach through the chest and may be managed best by costotransversectomy. Depending on the experience of the surgeon, video-assisted approaches can provide an alternative approach with reportedly less surgical morbidity. Newer minimally invasive approaches are also being developed that may offer less pain and quicker recovery.
Pearls
Key Points
1 Anand N, Regan JJ. Video-assisted thoracoscopic surgery for thoracic disc disease. Spine (Phila Pa 1976). 2002;27:871-879.
2 Arce CA, Dohrmann G. Herniated thoracic disks. Neurol Clin. 1985;3:383-392.
3 Bohlman HH, Zdeblick TA. Anterior excision of herniated thoracic discs. J Bone Joint Surg Am. 1988;70:1038-1047.
This article describes the technique of transthoracic disc decompression and clinical outcomes.
4 Brown CW, Deffer PA, Akmakjian J, et al. The natural history of thoracic disc herniation. Spine (Phila Pa 1976). 1992;17:S97-S102.
5 Currier BL, Eismont FJ, Green BA. Transthoracic disc excision and fusion for thoracic herniated discs. Spine (Phila Pa 1976). 1994;3:323-328.
6 Wood KB, Garvey TA, Gundry C, et al. Magnetic resonance imaging of the thoracic spine. J Bone Joint Surg Am. 1995;77:1631-1638.
1 Key CA. On paraplegia: Depending on disease of the ligaments of the spine. Guys Hosp Rep. 1838;3:17-24.
2 Middleton GS, Teacher JH. Injury of the spinal cord due to rupture of an intervertebral disc during muscular effort. Glasgow Med J. 1911;76:1. 1
3 Love JG, Schorn VG. Thoracic disk protrusions. JAMA. 1965;191:627-631.
4 Mixter WJ, Barr JS. Rupture of the intervertebral disc with involvement of the spinal canal. N Engl J Med. 1934;211:210-218.
5 Abbott KH, Retter RH. Protrusions of thoracic intervertebral disc. Neurology. 1956;6:1-10.
6 Arseni C, Nash F. Thoracic intervertebral disc protrusion: A clinical study. J Neurosurg. 1960;17:418-430.
7 Epstein JA. The syndrome of herniation of the lower thoracic intervertebral discs with nerve root and spinal cord compression: A presentation of four cases with a review of the literature, methods of diagnosis, and treatment. J Neurosurg. 1954;11:525-538.
8 Fisher RG. Protrusions of thoracic disc: The factor of herniation through the dura mater. J Neurosurg. 1965;22:591-593.
9 Hawk WA. Spinal compression caused by enchondrosis of the intervertebral fibrocartilage with a review of the recent literature. Brain. 1936;59:204-224.
10 Huang T, Hsu RW, Sum C, et al. Complications in thoracoscopic spinal surgery: A study of 90 consecutive patients. Surg Endosc. 1999;19:346-350.
11 Kite WCJr, Whitfield RD, Campbell E. The thoracic herniated intervertebral disc syndrome. J Neurosurg. 1957;14:61-67.
12 Logue V. Thoracic intervertebral disc prolapse with spinal cord compression. J Neurol Neurosurg Psychiatry. 1952;15:227-241.
13 Peck FCJr. A calcified thoracic intervertebral disk with herniation and spinal cord compression in a child: Case report. J Neurosurg. 1957;14:105-109.
14 Svien HJ, Karavitis AL. Multiple protrusions of intervertebral disks in the upper thoracic region: Report of case. Mayo Clin Proc. 1954;29:375-378.
15 Terry AF, McSweeney T, Jones HWF. Paraplegia as a sequela to dorsal disc prolapse. Paraplegia. 1981;19:111-117.
16 Tovi D, Strang RR. Thoracic intervertebral disk protrusions. Acta Chir Scand Suppl. 1960;267:6.
17 Menard V. Etude Pratique sur le Mal de Pott. Paris: Masson; 1900.
18 Capener N. The evolution of lateral rachiotomy. J Bone Joint Surg Br. 1954;36:173-179.
19 Hulme A. The surgical approach to thoracic intervertebral disc protrusions. J Neurol Neurosurg Psychiatry. 1960;23:133-137.
20 Arce CA, Dohrmann G. Herniated thoracic disks. Neurol Clin. 1985;3:383-392.
21 Hodgson AR, Stock FE. Anterior spinal fusion: A preliminary communication on the radical treatment of Pott’s disease and Pott’s paraplegia. Br J Surg. 1956;44:266-275.
22 Crafoord C, Hiertonn T, Lindblom K, et al. Spinal cord compression caused by a protruded thoracic disc: Report of a case treated with anterolateral fenestration of the disc. Acta Orthop Scand. 1958;28:103-107.
23 Perot PHJr, Munro DD. Transthoracic removal of midline thoracic disc protrusions causing spinal cord compression. J Neurosurg. 1969;31:452-458.
24 Ransohoff J, Spencer F, Siew F, et al. Case reports and technical notes on transthoracic removal of thoracic disc: Report of three cases. J Neurosurg. 1969;31:459-461.
25 Carson J, Gumpert J, Jefferson A. Diagnosis and treatment of thoracic intervertebral disc protrusions. J Neurol Neurosurg Psychiatry. 1971;34:67-68.
26 Patterson RHJr, Arbit E. A surgical approach through the pedicle to protruded thoracic discs. J Neurosurg. 1978;48:768-772.
27 Lesoin F, Rousseaux M, Autricque A, et al. Thoracic disc herniations: Evolution in the approach and indications. Acta Neurochir. 1986;80:30-34.
28 Safdari H, Baker RL. Microsurgical anatomy and related techniques to an anterolateral transthoracic approach to thoracic disc herniations. Surg Neurol. 1985;23:589-593.
29 Signorini G, Baldini M, Vivenza C, et al. Surgical treatment of thoracic disc protrusion. Acta Neurochir. 1979;49:245-254.
30 Anand N, Regan JJ. Video-assisted thoracoscopic surgery for thoracic disc disease: Classification and outcome study of 100 consecutive cases with a 2-year minimum follow-up period. Spine (Phila Pa 1976). 2002;27:871-879.
31 Regan JJ, Mack MJ, Picetti GD. A technical report on video-assisted thoracoscopy in thoracic spine surgery: Preliminary description. Spine (Phila Pa 1976). 1995;20:831-837.
32 Regan JJ, Ben-Yishay A, Mack MJ. Video-assisted thoracoscopic excision of herniated thoracic disc: Description of technique and preliminary experience in the first 29 cases. J Spinal Disord. 1998;11:183-191.
33 Rosenthal D, Rosenthal R, de Simone A. Removal of a protruded thoracic disc using microsurgical endoscopy: A new technique. Spine (Phila Pa 1976). 1994;19:1087-1091.
34 Blumenkopf B. Thoracic intervertebral disc herniations: Diagnostic value of magnetic resonance imaging. Neurosurgery. 1988;23:36-40.
35 Bohlman HH, Zdeblick TA. Anterior excision of herniated thoracic discs. J Bone Joint Surg Am. 1988;70:1038-1047.
36 Chambers AA. Thoracic disk herniation. Semin Roentgenol. 1988;23:111-117.
37 Francavilla TL, Powers A, Dina T, et al. MR imaging of thoracic disk herniations. J Comp Assist Tomogr. 1987;11:1062-1065.
38 Parizel PM, Rodesch G, Baleriaux D, et al. Gd-enhanced MR in thoracic disc herniations. Neuroradiology. 1989;31:75-79.
39 Ross JS, Perez-Reyes N, Masaryk TJ, et al. Thoracic disc herniation: MR imaging. Radiology. 1987;165:511-515.
40 Videman T, Battie MC, Gill K, et al. Magnetic resonance imaging findings and their relationships in the thoracic and lumbar spine: Insights into the etiopathogenesis of spinal degeneration. Spine (Phila Pa 1976). 1995;20:928-935.
41 Williams MP, Cherryman GR, Husband JE. Significance of thoracic disc herniations demonstrated by MR imaging. J Comput Tomogr. 1989;13:212-214.
42 Wood KB, Garvey TA, Gundry C, et al. Magnetic resonance imaging of the thoracic spine. J Bone Joint Surg Am. 1995;77:1631-1638.
43 Williams MP, Cherryman GR. Thoracic disc herniation: MR imaging [letter to the editor]. Radiology. 1988;167:874-875.
44 Arce CA, Dohrmann G. Thoracic disc herniation: Improved diagnosis with computed tomographic scanning and a review of the literature. Surg Neurol. 1985;23:356-361.
45 Benson MKD, Byrnes DP. The clinical syndromes and surgical treatment of thoracic intervertebral disc prolapse. J Bone Joint Surg Br. 1975;57:471-477.
46 Albrand OW, Corkill G. Thoracic disc herniation: Treatment and prognosis. Spine (Phila Pa 1976). 1979;4:41-46.
47 Love JG, Kiefer EJ. Root pain and paraplegia due to protrusions of thoracic intervertebral disks. J Neurosurg. 1950;7:62-69.
48 Brennan M, Perrin JCS, Canady A, et al. Paraparesis in a child with a herniated thoracic disc. Arch Phys Med Rehab. 1987;68:806-808.
49 Otani KI, Yoshida M, Fujii E, et al. Thoracic disc herniation: Surgical treatment in 23 patients. Spine (Phila Pa 1976). 1988;13:1262-1267.
50 Alvarez O, Roque CT, Pampati M. Multilevel thoracic disk herniations: CT and MR studies. J Comput Assist Tomogr. 1988;12:649-652.
51 Otani K, Manxoku S, Shibaski K, et al. The surgical treatment of thoracic and thoracolumbar disc lesions using the anterior approach. Spine (Phila Pa 1976). 1977;2:266-275.
52 Russell T. Thoracic intervertebral disc protrusion: Experience of 67 cases and a review of the literature. Br J Neurosurg. 1989;3:153-160.
53 Le Roux PD, Haglund MM, Harris AB. Thoracic disc disease: Experience with the transpedicular approach in twenty consecutive patients. Neurosurgery. 1993;33:58-66.
54 Lesoin F, Leys D, Rousseaux M, et al. Thoracic disk herniation and Scheuermann’s disease. Eur Neurol. 1987;26:145-152.
55 Mansour H, Hammoud F, Vlahovitch B. Brown-Séquard syndrome caused by foramen and calcified disk herniation responsible for direct compression of Adamkiewicz’s artery. Neurochirurgie. 1987;33:478-481.
56 McAfee PC, Regan JR, Zdeblick T, et al. The incidence of complications in endoscopic anterior thoracolumbar spinal reconstructive surgery: A prospective multicenter study comprising the first 100 cases. Spine (Phila Pa 1976). 1995;20:1624-1632.
57 Haley JC, Perry JH. Protrusion of intervertebral discs: Study of their distribution, characteristics and effects on the nervous system. Am J Surg. 1950;80:394-404.
58 Ridenour TR, Haddad SF, Hitchon PW, et al. Herniated thoracic disks: Treatment and outcome. J Spinal Disord. 1993;6:218-224.
59 Ryan RW, Lally JF, Kozic Z. Asymptomatic calcified herniated thoracic disks: CT recognition. AJNR Am J Neuroradiol. 1988;9:363-366.
60 Awwad EE, Martin DS, Smith KRJr, et al. Asymptomatic versus symptomatic herniated thoracic discs: Their frequency and characteristics as detected by computed tomography after myelography. Neurosurgery. 1991;28:180-186.
61 Niemelainen R, Battie MC, Gill K, et al. The prevalence and characteristics of thoracic magnetic resonance imaging findings in men. Spine (Phila Pa 1976). 2008;33:2552-2559.
62 Tahmouresie A. Herniated thoracic intervertebral disc: An unusual presentation: Case report. Neurosurgery. 1980;7:623-625.
63 Landreneau RJ, Hazelrigg SR, Mack MJ, et al. Post-operative pain-related morbidity: Video-assisted thoracic surgery versus thoracotomy. Ann Thorac Surg. 1993;56:1285-1289.
64 Van Landingham JH. Herniation of thoracic intervertebral discs with spinal cord compression in kyphosis dorsalis juvenilis (Scheuermann’s disease): Case report. J Neurosurg. 1954;11:327-329.
65 Dommisse GF. The blood supply of the spinal cord: A critical vascular zone in spinal surgery. J Bone Joint Surg Br. 1974;56:225-235.
66 Hochman MS, Pena C, Ramirez R. Calcified herniated thoracic disc diagnosed by computerized tomography. J Neurosurg. 1980;52:722-723.
67 Maccartee CCJr, Griffin PP, Byrd EB. Ruptured calcified thoracic disc in a child. J Bone Joint Surg Am. 1972;54:1271-1274.
68 Kahn EA. The role of the dentate ligaments in spinal cord compression and the syndrome of lateral sclerosis. J Neurosurg. 1944;4:191-199.
69 Doppman JL, Girton M. Angiographic study of the effect of laminectomy in the presence of acute anterior epidural masses. J Neurosurg. 1976;45:195-202.
70 Brown CW, Deffer PA, Akmakjian J, et al. The natural history of thoracic disc herniation. Spine (Phila Pa 1976). 1992;17(Suppl 6):S97-S102.
71 Gelch MM. Herniated thoracic disc at T1-2 level associated with Horner’s syndrome. J Neurosurg. 1978;48:128-130.
72 Fransen P, Collignon F, Van Den Heule B. Foraminal disc herniation Th9-Th10 mimicking abdominal pain. Acta Orthop Belg. 2008;74:881-884.
73 Ozturk C, Tezer M, Sirvanci M, et al. Far lateral thoracic disc herniation presenting with flank pain. Spine J. 2006;6:201-203.
74 LaBan MM, Gorin G. A thoracic disc herniation presenting as an abdominal hernia. Am J Phys Med Rehab. 2007;86:601.
75 Stetkarova I, Chrobok J, Ehler E, et al. Segmental abdominal wall paresis caused by lateral low thoracic disc herniation. Spine (Phila Pa 1976). 2007;32:E635-E639.
76 Deitch K, Chudnofsky C, Young M. T2-3 thoracic disc herniation with myelopathy. J Emerg Med. 2009;36:138-140.
77 Papapostolou A, Tsivgoulis G, Papadopoulou M, et al. Bilateral drop foot due to thoracic disc herniation. Eur J Neurol. 2007;14:E5.
78 Kuhlendahl H. Der Thorakale Bandscheibenprolaps als extramedullarer Spinaltumor und in seinen Beziehungen zu internen. Organsyndromen. Arztl Wochenschr. 1951;6:154-157.
79 Malmivaara A, Videman T, Kuosma E, et al. Facet joint orientation, facet and costovertebral joint osteoarthrosis, disc degeneration, vertebral body osteophytosis, and Schmorl’s nodes in the thoracolumbar junctional region of cadaveric spines. Spine (Phila Pa 1976). 1987;12:458-463.
80 Almond LM, Hamid NA, Wasserberg J. Thoracic intradural disc herniation. Br J Neurosurg. 2007;21:32-34.
81 Epstein NE, Syrquin MS, Epstein JA, et al. Intradural disc herniations in the cervical, thoracic, and lumbar spine: Report of three cases and review of the literature. J Spinal Disord. 1990;3:396-403.
82 Fidler MW, Goedhard ZD. Excision of prolapse of thoracic intervertebral disc: A transthoracic technique. J Bone Joint Surg Br. 1984;66:518-522.
83 Isla A, Roda JM, Benscome J, et al. Intradural herniated dorsal disc: Case report and review of the literature. Neurosurgery. 1988;22:737-738.
84 Jefferson A. The treatment of thoracic intervertebral disc protrusion. Clin Neurol Neurosurg. 1975;78:1.
85 Chin LS, Black KL, Hoff JT. Multiple thoracic disc herniations: Case report. J Neurosurg. 1987;66:290-292.
86 Haro H, Domoto T, Maekawa S, et al. Resorption of thoracic disc herniation: Report of 2 cases. J Neurosurg Spine. 2008;8:300-304.
87 Bullough PG, Boachie-Adjei O. Atlas of Spinal Diseases. Philadelphia: JB Lippincott; 1988.
88 Sonnabend DH, Taylor TKF, Chapman GK. Intervertebral disc calcification syndromes in children. J Bone Joint Surg Br. 1982;64:25-31.
89 Nicolau A, Diard F, Darrigade JM, et al. Posterior herniation of a calcified disc in children: A report of two cases. J Radiol. 1985;66:683-688.
90 Weinberger A, Myers AR. Intervertebral disk calcification in adults: A review. Semin Arthritis Rheum. 1978;8:69-75.
91 Currier BL, Eismont FJ, Green BA. Transthoracic disc excision and fusion for thoracic herniated discs. Spine (Phila Pa 1976). 1994;3:323-328.
92 Roosen N, Dietrich U, Nicola N, et al. Case report: MR imaging of calcified herniated thoracic disk. J Comput Assist Tomogr. 1987;11:733-735.
93 Ryan MD, Taylor TKF. Acute spinal cord compression in Scheuermann’s disease. J Bone Joint Surg Br. 1982;64:409-412.
94 Baker HLJr, Love JG, Uihlein A. Roentgenologic features of protruded thoracic intervertebral disks. Radiology. 1965;84:1059-1065.
95 Alberico A, Sahni KS, Hall JAJr, et al. High thoracic disc herniation. Neurosurgery. 1986;19:449-451.
96 Enzmann DR, Griffin C, Rubin JB. Potential false-negative MR images of the thoracic spine in disk disease with switching of phase and frequency encoding gradients. Radiology. 1987;165:635-637.
97 Schellhas KP, Pollei SR, Dorwart RH. Thoracic discography: A safe and reliable technique. Spine (Phila Pa 1976). 1994;19:2103-2109.
98 Wood KB, Schellhas KP, Garvey TA, et al. Thoracic discography in healthy individuals: A controlled prospective study of magnetic resonance imaging and discography in asymptomatic and symptomatic individuals. Spine (Phila Pa 1976). 1999;24:1548-1555.
99 Buenaventura RM, Shah RV, Patel V, et al. Systematic review of discography as a diagnostic test for spinal pain: An update. Pain Physician. 2007;20:147-164.
100 Ravichandran G, Frankel HL. Paraplegia due to intervertebral disc lesions: A review of 57 operated cases. Paraplegia. 1981;19:133-139.
101 Aizawa T, Sato T, Sasaki H, et al. Results of surgical treatment for thoracic myelopathy: Minimum 2-year follow-up study in 132 patients. J Neurosurg Spine. 2007;7:13-20.
102 Yi S, Kim H, Shin HC, et al. Outcome of surgery for a symptomatic herniated thoracic disc in relation to preoperative characteristics of the disc. Acta Neurochir (Wien). 2007;149:1139-1145.
103 Fessler RG, Sturgill M. Review: Complications of surgery for thoracic disc disease. Surg Neurol. 1998;49:609-618.
104 Singounas EG, Karvounis PC. Thoracic disc protrusion (analysis of 8 cases). Acta Neurochir. 1977;39:251-258.
105 Bennett MH, McCallum J. Experimental decompression of the spinal cord. Surg Neurol. 1977;8:63-67.
106 Simpson JM, Silveri CP, Simeone FA, et al. Thoracic disc herniation: Re-evaluation of the posterior approach using a modified costotransversectomy. Spine (Phila Pa 1976). 1993;13:1872-1877.
107 Chesterman PJ. Spastic paraplegia caused by sequestrated thoracic intervertebral disc. Proc R Soc Med. 1964;57:87-88.
108 Garrido E. Modified costotransversectomy: A surgical approach to ventrally placed lesions in the thoracic spinal canal. Surg Neurol. 1980;13:109-113.
109 Hulme A. The surgical approach to thoracic intervertebral disc protrusions. J Neurol Neurosurg Psychiatry. 1960;23:133-137.
110 Amini A, Apfelbaum RI, Schmidt MH. Chylorrhea: A rare complication of thoracoscopic discectomy of the thoracolumbar junction. J Neurosurg Spine. 2007;6:563-566.
111 Maiman DJ, Larson SJ, Luck E, et al. Lateral extracavitary approach to the spine for thoracic disc herniations: Report of 23 cases. Neurosurgery. 1984;14:178-182.
112 DiChiro G, Fried LC, Doppman JL. Experimental spinal cord angiography. Br J Radiol. 1970;43:19-20.
113 Lazorthes G, Gouzae A, Zadeh JO, et al. Arterial vascularization of the spinal cord: Recent studies of the anastomotic substitution pathways. J Neurosurg. 1971;35:253-262.
114 Ulivieri S, Oliveri G, Petrini C, et al. Transmanubrial osteomuscular sparing approach for T1-T2 thoracic disc herniation. Minerva Chir. 2008;63:421-423.
115 Kawahara N, Demura S, Marukami H, et al. Transvertebral herniotomy for T2/3 disc herniation—a case report. J Spinal Disord Tech. 2009;22:62-66.
116 Mack MJ, Regan JJ, Bobechko WP, et al. Present role of thoracoscopy for diseases of the spine. Ann Thorac Surg. 1993;56:736-738.
117 Horowitz MB, Moossy JJ, Julian T, et al. Thoracic discectomy using video assisted thoracoscopy. Spine (Phila Pa 1976). 1994;19:1082-1086.
118 Kim SJ, Sohn MJ, Ryoo JY, et al. Clinical analysis of video-assisted thoracoscopic spinal surgery in the thoracic or thoracolumbar spinal pathologies. J Korean Neurosurg Soc. 2007;42:293-299.
119 Gille O, Soderlund C, Razafimahandri HJC, et al. Analysis of hard thoracic herniated discs: Review of 18 cases operated by thoracoscopy. Eur Spine J. 2006;15:537-542.
120 Bartels RH, Peul WC. Mini-thoracotomy or thoracoscopic treatment for medially located thoracic herniated disc? Spine (Phila Pa 1976). 2007;32:E581-E584.
121 Chi JH, Dhall SS, Kanter AS, et al. The mini-open transpedicular thoracic discectomy: Surgical technique and assessment. Neurosurg Focus. 2008;25:E5.
122 Lidar Z, Lifshutz J, Bhattacharjee S, et al. Minimally invasive, extracavitary approach for thoracic disc herniation: Technical report and preliminary results. Spine J. 2006;6:157-163.
123 Sheikh H, Samartzis D, Perez-Cruet MJ. Techniques for the operative management of thoracic disc herniation: Minimally invasive thoracic microdiscectomy. Orthop Clin North Am. 2007;38:351-361.
124 Ungersbock K, Perneczky A, Korn A. Thoracic vertebrostenosis combined with thoracic disc herniation: Case report and review of the literature. Spine (Phila Pa 1976). 1987;12:612-615.