Chapter 47 Thermotherapy
(Includes Hot Packs, Paraffin Wax, Infrared Lamps)
OVERVIEW.
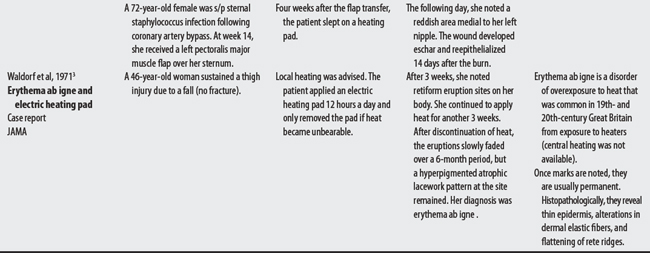
Thermotherapy comprises a number of physical agents that use superficial heat to increase soft tissue extensibility, reduce pain, improve circulation, and accelerate healing. Thermal therapy is believed to accomplish these goals by increasing blood flow (vasodilation), reducing alpha motor neuron firing rate, increasing pain threshold (gating effect; reduced ischemia), and increasing metabolic activity (increasing the availability of oxygen to tissue).1 Note: Because thermotherapy produces heat, the tissue needs to be capable to dissipating the heat via adequate blood circulation, and the patient must be capable of informing the clinician (or escaping) if the modality gets too hot.
OTHER ISSUES: POSSIBLE PROCEDURAL IRREGULARITIES CONTRIBUTING TO COMPLICATIONS.
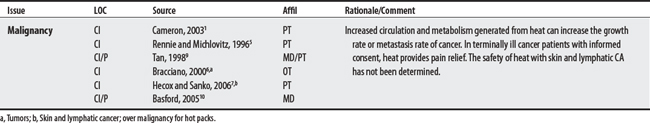
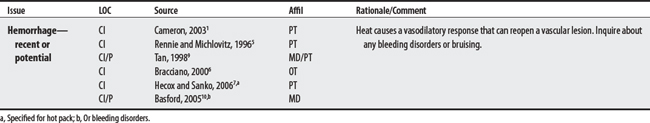
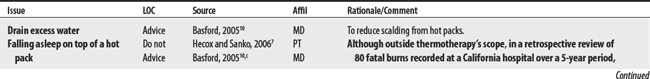
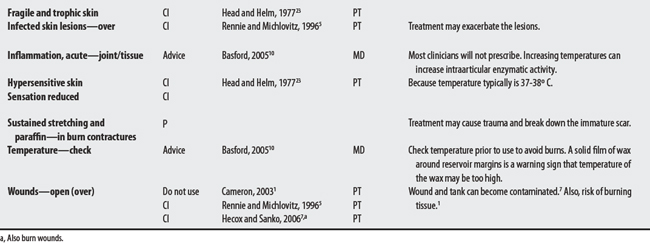
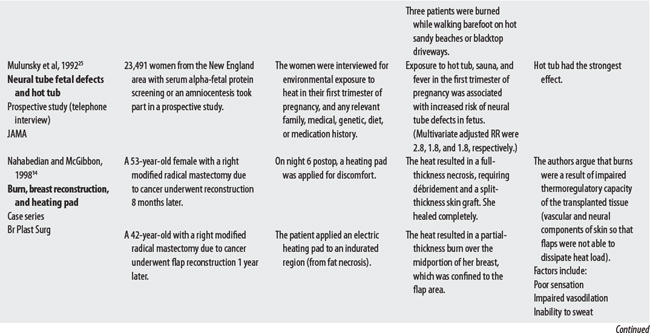
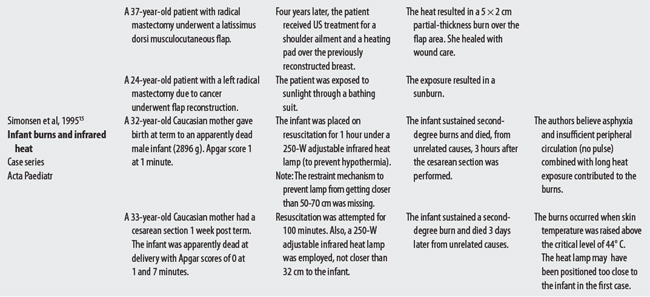
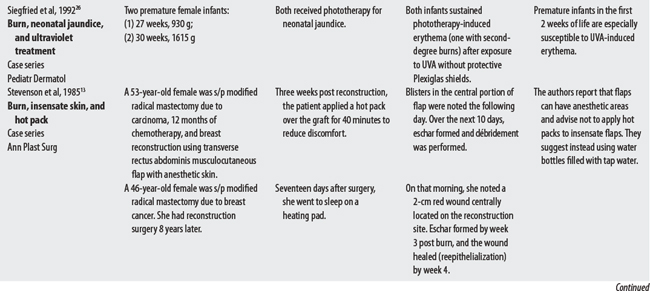
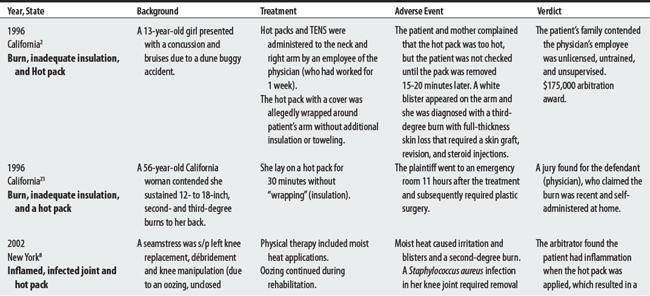
(1) Monitoring insulation: In a 1996 California lawsuit,2 a 13-year-old girl received a $175,000 arbitration award after she sustained a third-degree arm burn from a hot pack that was inadequately insulated and not periodically monitored. (2) Monitoring excessive treatment: Waldorf et al3 reported on a 46-year-old woman who developed erythema ab igne (hyperpigmentation) from using an electric heating pad 12 hours a day for about 6 weeks. (3) Monitoring paraffin temperatures: The FDA4 reports14 incidences of paraffin wax device problems from September 1992 to January 2003. Of these, 10 reports were of wax becoming too hot. Five cases led to hand burns.
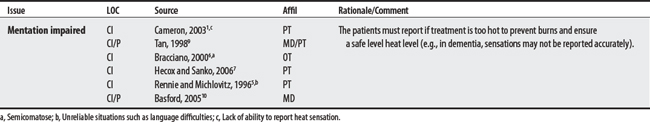
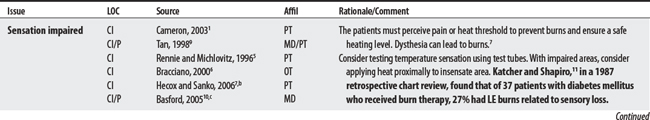
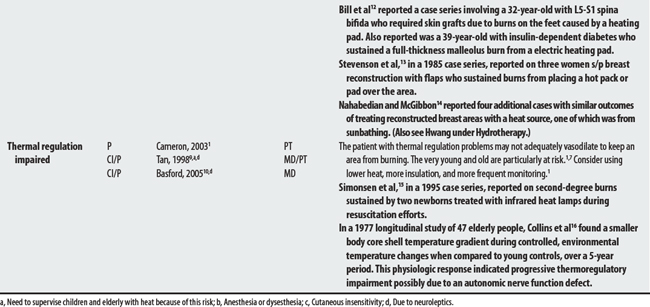
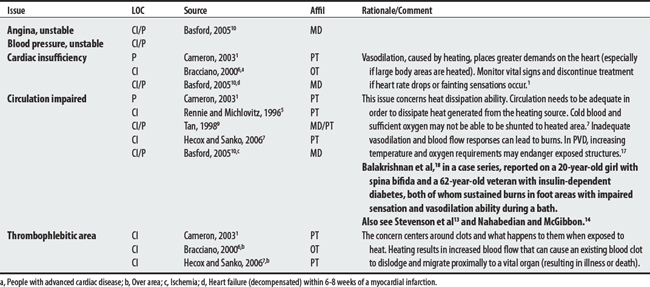
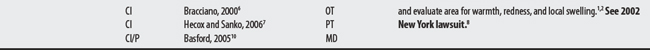
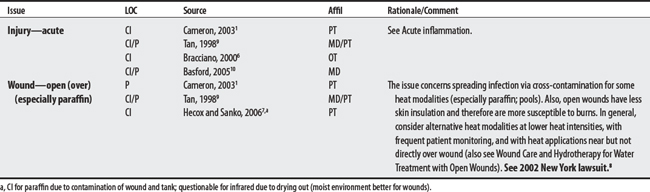
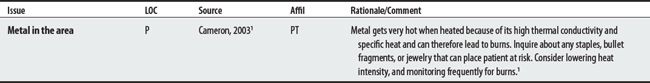
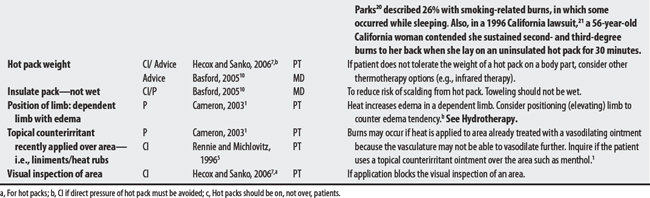
CONTRAINDICATIONS AND PRECAUTIONS FOR SUPERFICIAL HEAT
A00-B99 CERTAIN INFECTIONS AND PARASITIC DISEASES
D50-89 DISEASES OF BLOOD AND BLOOD-FORMING ORGANS, AND CERTAIN DISORDERS
F00-F99 MENTAL AND BEHAVIORAL DISORDERS
G00-99 DISEASES OF THE NERVOUS SYSTEM
I00-99 DISEASES OF THE CIRCULATORY SYSTEM
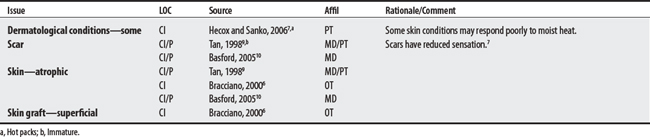
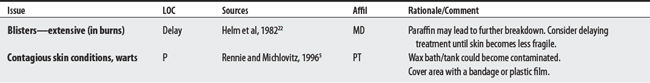
L00-99 DISEASES OF THE SKIN AND SUBCUTANEOUS TISSUE
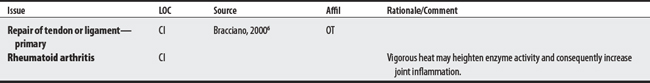
M00-99 DISEASES OF THE MUSCULOSKELETAL SYSTEM AND CONNECTIVE TISSUE
O00-99 PREGNANCY, CHILDBIRTH, AND PUERPERIUM
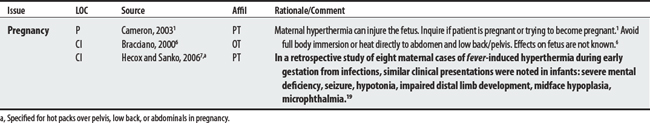
S00-98 INJURY, POISONING, AND CERTAIN OTHER CONSEQUENCES OF EXTERNAL CAUSES
ADVERSE EVENTS
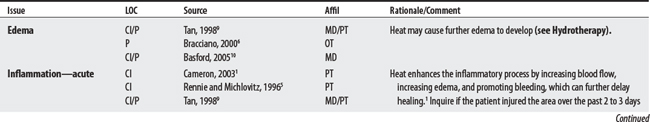
FDA4 REPORTS FOR PARAFFIN BATH
14 Reports from 9/18/92 to 1/9/03
| Date | Event |
|---|---|
| 1/9/03 | The bath overheated. |
| 12/13/02 | The drain heater coil overheated and the unit smoked. |
| 4/18/02 | The bath temperature was not regulated; a replacement thermostat corrected the problem. |
| 4/3/02 | Paraffin wax leaked onto the carpet. |
| 1/13/98 | The bath had a faulty thermostat; the wax reached a flash point and then caught fire. The incident was replicated by a biomedical department. |
| 3/14/97 | The bath provided insufficient heat. |
| 4/02/02 | The bath’s temperature fluctuated from low to high. |
| 2/28/01 | The paraffin wax surface was too hot. |
| 2/13/01 | A wax burn was reported (minor hand burn). |
| 2/6/01 | A patient complained the wax was too hot and sustained a second-degree burn to the fingers. The device temperature read 155°. The PTA noticed that the machine switch had been switched to Start instead of Operate. |
| 7/29/98 | An individual sustained a second-degree burn on the left hand after using the device in hospital. The wound took 3 to 4 weeks to heal. |
| 12/29/95 | During therapy, a patient’s right hand was dipped in paraffin and wrapped for 15 minutes. The next day, the patient returned with a dime-size blister that appeared to be a burn on the right finger. |
| 2/15/95 | The unit got too hot, and then not hot enough. |
| 9/18/92 | The temperature of the wax varied from one area of the unit to another. |
Note: FDA reports do not necessarily establish cause-effect relationships between equipment and injury. Incidences may be due to equipment or user error. Also, some reports are alleged by attorneys.
1 Cameron MH. Physical agents in rehabilitation: from research to practice. St Louis: Saunders, 2003.
2 Medical malpractice verdicts, settlements and experts, Feb 1996, p 27, loc 1.
3 Waldorf DS, Rast MF, Garofalo VJ. Heating-pad erythematous dermatitis “erythema ab igne,”. JAMA. 1971;218(11):1704.
4 U.S. Food and Drug Administration. Web page Available at: http://www.FDA.gov.cdrh/mdr. Accessed: November 7, 2005
5 Rennie GA, Michlovitz SL. Biophysical principles of heating and superficial heating agents. In Michlovitz SL, editor: Thermal agents in rehabilitation, ed 3, Philadelphia: FA Davis, 1996.
6 Bracciano AG. Physical agent modalities: theory and application for the occupational therapist. Thorofare (NJ): Slack, 2000.
7 Hecox B, Sanko JP. Superficial thermotherapy. In: Hecox B, Mehreteab TA, Weisberg J, editors. Integrating physical agents in rehabilitation. Upper Saddle River (NJ): Pearson Prentice Hall, 2006.
8 Medical malpractice verdicts, settlements and experts, Feb 2002, p 51, loc 2.
9 Tan JC. Practical manual of physical medicine and rehabilitation: diagnostics, therapeutics, and basic problems. St Louis: Mosby, 1998.
10 Basford JR. Therapeutic physical agents. Delisa JA, editor. Physical medicine and rehabilitation: principles and practices, ed 4, vol 1. Philadelphia: Lippincott Williams & Wilkins, 2005.
11 Katcher ML, Shapiro MM. Lower extremity burns related to sensory loss in diabetes mellitus. J Fam Pract. 1987;24(2):149-151.
12 Bill TJ, Edich RF, Himel HN. Electric heating pad burns. J Emerg Med. 1994;12(6):819-824.
13 Stevenson TR, Hammond DC, Keip D, et al. Heating pad burns in anesthetic skin. Ann Plast Surg. 1985;15(1):73-75.
14 Nahabedian MY, McGibbon BM. Thermal injuries in autogenous tissue breast reconstruction. Br J Plast Surg. 1998;51(8):599-602.
15 Simonsen K, Graem N, Rothman LP, Degn H. Iatrogenic radiant heat burns in severely asphyxic newborns. Acta Paediatr. 1995;84(12):1438-1440.
16 Collins KJ, Dore C, Exton-Smith AN, et al. Accidental hypothermia and impaired temperature homeostasis in the elderly. BMJ. 1977;1(6057):353-356.
17 Abramson DI. Physiologic basis for the use of physical agents in peripheral vascular disorders. Arch Phys Med Rehabil. 1965;46:216-244.
18 Balakrishnan C, Rak TP, Meininger MS. Burns of the neuropathic foot following use of therapeutic footbaths. Burns. 1995;21:622-623.
19 Smith DW, Clarren SK, Harvey MA. Hyperthermia as a possible teratogenic agent. J Pediatr. 1978;92(6):878-883.
20 Parks JG, Noguchi TT, Klatt EC. The epidemiology of fatal burn injuries. J Forens Sci. 1989;34(2):399-406.
21 Medical malpractice verdicts, settlements and experts, July 1996, p 47, loc 4.
22 Helm PA, Kevorkian CG, Lushbaugh M. Burn injury: rehabilitation management in 1982. Arch Phys Med Rehabil. 1982;63:6-16.
23 Head MD, Helm PA. Paraffin and sustained stretching in the treatment of burn contractures. Burns. 1977;4:136-139.
24 Imai Y, Nobuoka S, Sagashima J, et al. Acute myocardial infarction induced by alternating exposure to heat in a sauna and rapid cooling in cold water. Cardiology. 1998;90(4):299-301.
25 Milunsky A, Ulcickas M, Rothman KJ, et al. Maternal heat exposure and neural tube defects. JAMA. 1992;268(7):882-885.
26 Siegfried EC, Stone MS, Madison KC. Ultraviolet light burn: a cutaneous complication of visible light phototherapy of neonatal jaundice. Pediatr Dermatol. 1992;9:278-282.