Therapeutic Injection
Two major categories of vulvar injections for the alleviation of debilitating symptoms associated with dystrophic disorders are as follows: (1) alcohol injection for the relief of pruritus (not pain), and (2) dexamethasone (Decadron) injection for the relief of chronic inflammatory conditions (e.g., lichen sclerosus) and for the relief of chronic pain (pudendal neuralgia).
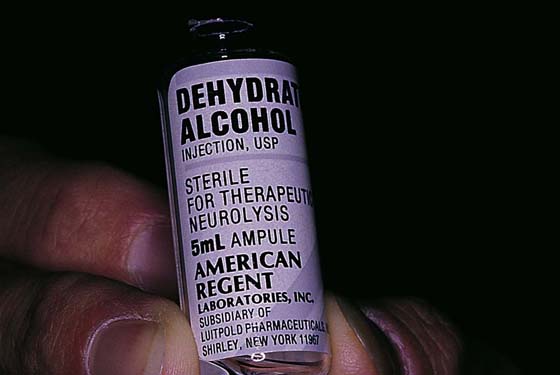
Alcohol Injection
Chronic pruritus that is unresponsive to topical medication (e.g., steroids) or retinoids is an indication for alcohol injection (Fig. 79–1). The criterion for injection to deaden the nerves is essentially the failure of conservative therapeutic measures to control vulvar itching. Patients should be warned that a complication of this type of treatment is neuropathy manifested by burning pain. Injection of an excessive volume of alcohol, as well as subcuticular injection, can and will cause tissue slough and possibly necrotizing fasciitis.
The patient is placed in the dorsal lithotomy position under general anesthesia. The area to be injected is divided into a grid, with all intersections 1 cm apart. The entire area may be large (i.e., encompassing the whole vulva) or limited to a single side. The grid is drawn after the vulva is prepared with hexachlorophene (Phisohex) or povidone-iodine (Betadine). A sterile surgical marking pen is the most convenient device for this task (Fig. 79–2). A 1-mL tuberculin syringe fitted with a 27-gauge needle is utilized for injection. Absolute alcohol is drawn up into the syringe. At each intersecting line, 0.1 mL of alcohol is injected into the subcutaneous fat (Fig. 79–3). The injection destroys the fine cutaneous branches of the perineal nerves, resulting in anesthesia to the vulva. The vulva is perceived by the patient as numb.
Dexamethasone Injection
The current treatment of choice for the relief of pruritus associated with lichen sclerosus is 2 mg of dexamethasone diluted to 10 mL with 0.25% bupivacaine. Serial injections also appear to arrest the progress of the inflammatory reaction and subsequent scar formation associated with lichen sclerosus. Injections are given in the office weekly, then biweekly, then monthly.
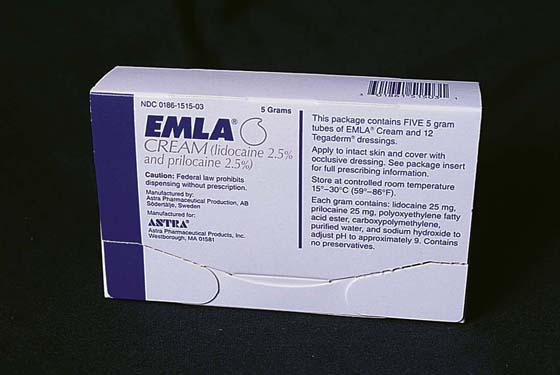
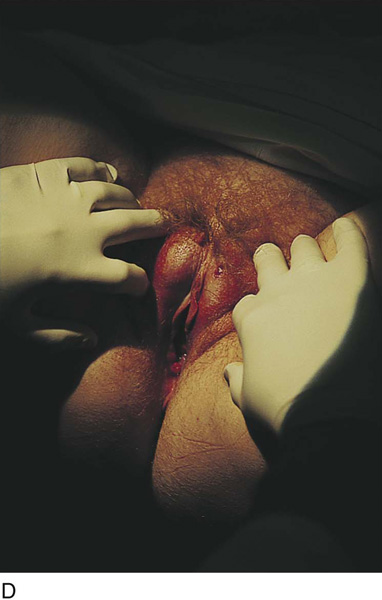
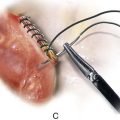
All patients are prepared with the application of EMLA cream 30 minutes before injection (Fig. 79–4). This effectively numbs the skin and greatly reduces the discomfort of needle entry. A 10-mL syringe is fitted with a 1½-inch, 27-gauge needle or a short, 30-gauge needle. Needle selection depends on the relative distribution of disease. After the skin is prepared with Betadine, the needle is directed along the interlabial sulcus subdermally (in contrast with the alcohol injection, which is subcutaneous). Two milligrams of the dexamethasone mixture is injected on each side of the vulva (Fig. 79–5A, B). The needle is inserted into the tissue to its hub, and the injection is performed during slow withdrawal of the needle (Fig. 79–6A through D).
Pudendal neuralgia is associated with burning, sticking, or sharp pain that is more or less continuous and not restricted to the vestibule. The pain is aggravated most consistently by sitting. The disorder is more common in women 50 years of age or older but may occur as the result of surgery for vulvar vestibulitis syndrome. Injection of dexamethasone into the area of the specific pudendal nerve branch is analogous to injection of an anti-inflammatory drug into the foot for relief of Morton’s neuroma. Most patients with pudendal neuralgia can pinpoint the area of hyperesthesia and pain instigation. A similar mixture of dexamethasone and 0.25% bupivacaine is utilized for these injections, as was described earlier for the treatment of lichen sclerosus. A 10-mL injection is made into a specific site (e.g., for clitoral pain, the injection is aimed at the clitoral crus). A finger into the vagina helps direct the needle to the specific site for injection. After the injection, which contains a long-acting local anesthetic, the patient should experience (on the table) immediate relief of her pain. These injections may be repeated at 1-, 2-, or 3-month intervals as required for pain relief.
FIGURE 79–1 Chronic pruritus of the vulva that is unresponsive to topical and systemic medications may be relieved by alcohol injection. Absolute alcohol is the only appropriate agent for this therapy.
FIGURE 79–2 A grid is marked on the vulva with a sterile pen after the site has been surgically prepared and draped. The intersecting lines are 1 cm apart.
FIGURE 79–3 The alcohol, which has been drawn into a tuberculin syringe fitted with a 27-gauge needle, is injected at each intersecting point. Only 0.1 mL is injected into the subcutaneous tissue at each point. Care should be taken not to inject intradermally because this will produce tissue slough.
FIGURE 79–4 EMLA cream is applied liberally to the vulvar skin 30 minutes before the anticipated injection. This preparation is by far the most effective topical anesthetic available. The discomfort of a vulvar needle stick is ameliorated by 80% to 90% via the application of EMLA.
FIGURE 79–5 A. Dexamethasone is a very effective and potent anti-inflammatory agent. It is the drug of choice for the treatment of lichen sclerosus and pudendal neuralgia. Two milligrams is serially injected into each side of the vulva. B. Bupivacaine (Sensorcaine) 0.25% is an excellent agent to couple with dexamethasone. Typically, 10 mL of bupivacaine serves to dilute the dexamethasone. It simultaneously provides pain relief for 4 to 5 hours at the injection site.
FIGURE 79–6 A. For the management of lichen sclerosus, the needle (27-gauge) is aimed at the affected location, typically the interlabial sulcus, clitoral frenulum, and hood. B. The needle is advanced subdermally to its hub. C. The solution is slowly injected while the needle is withdrawn. The procedure is repeated identically on the opposite side. D. The injection has been completed bilaterally. The labial swelling disappears as the injected solution is absorbed.