Chapter 3 The zygapophysial joints – detailed structure
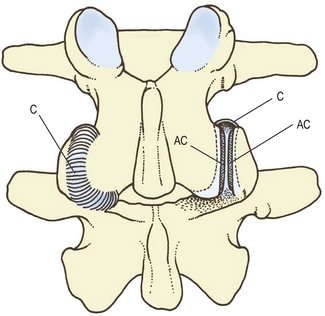
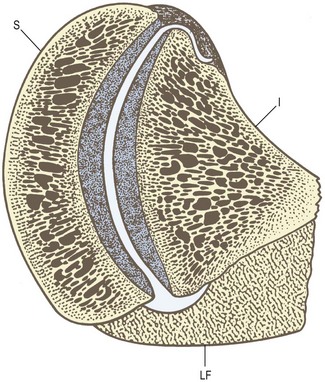
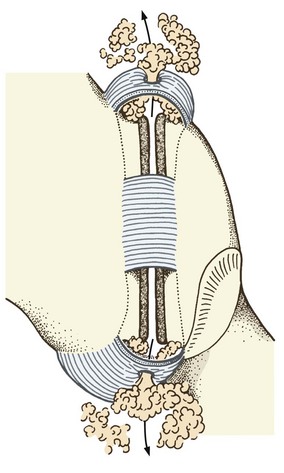
The lumbar zygapophysial joints are formed by the articulation of the inferior articular processes of one lumbar vertebra with the superior articular processes of the next vertebra. The joints exhibit the features typical of synovial joints. The articular facets are covered by articular cartilage, and a synovial membrane bridges the margins of the articular cartilages of the two facets in each joint. Surrounding the synovial membrane is a joint capsule which attaches to the articular processes a short distance beyond the margin of the articular cartilage (Fig. 3.1).
Articular facets
The articular facets of the lumbar vertebrae are ovoid in shape, measuring some 16 mm in height and 14 mm in width, and having a surface area of about 160 mm2. The facets of upper vertebrae are slightly smaller than these values indicate; those of the lower vertebrae are slightly smaller.1
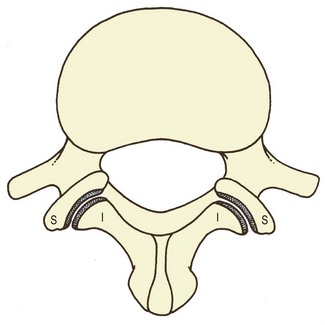
Viewed from behind (see Fig. 3.1), the articular facets of the lumbar zygapophysial joints appear as straight surfaces, suggesting that the joints are planar. However, viewed from above (Fig. 3.2), the articular facets vary both in the shape of their articular surfaces and in the general direction they face. Both of these features have significant ramifications in the biomechanics of these joints and, consequently, of the lumbar spine, and should be understood and appreciated.
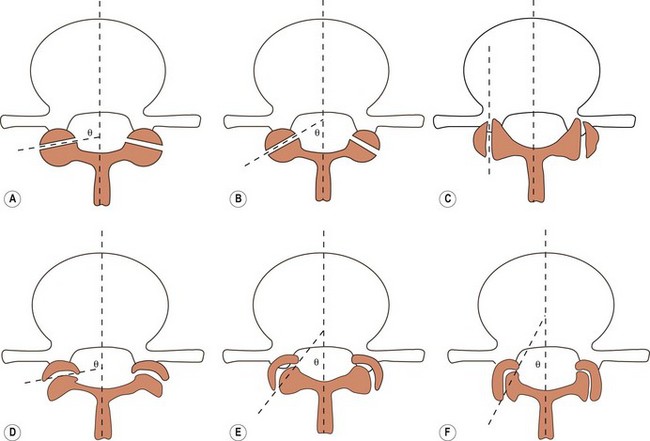
In the transverse plane, the articular facets may be flat or planar, or may be curved to varying extents (Fig. 3.3).2 The curvature may be little different from a flat plane (Fig. 3.3D) or may be more pronounced, with the superior articular facets depicting a C shape (Fig. 3.3E) or a J shape (Fig. 3.3F). The relative incidence of flat and curved facets at various vertebral levels is shown in Table 3.1.
Table 3.1 The incidence of flat and curved lumbar zygapophysial joints at different segmental levels. (Based on Horwitz and Smith 1940.3)
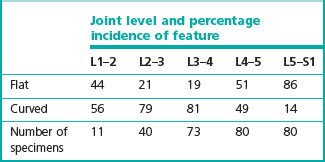
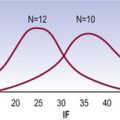
The orientation of a lumbar zygapophysial joint is, by convention, defined by the angle made by the average plane of the joint with respect to the sagittal plane (see Fig. 3.3). In the case of joints with flat articular facets, the plane of the joint is readily depicted as a line parallel to the facets. The average plane of joints with curved facets is usually depicted as a line passing through the anteromedial and posterolateral ends of the joint cavity (see Fig. 3.3). The incidence of various orientations at different levels is shown in Figure 3.4.
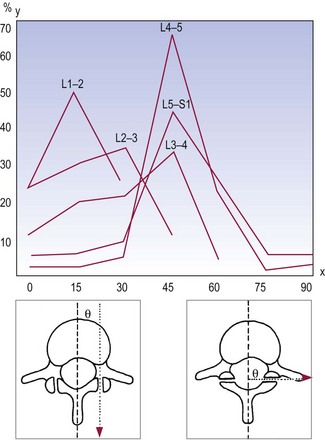
Figure 3.4 The orientation of lumbar zygapophysial joints with respect to the sagittal plane: incidence by level. (Based on Horwitz and Smith 1940.3) x-axis, orientation (degrees from sagittal plane); y-axis, proportion of specimens showing particular orientation.
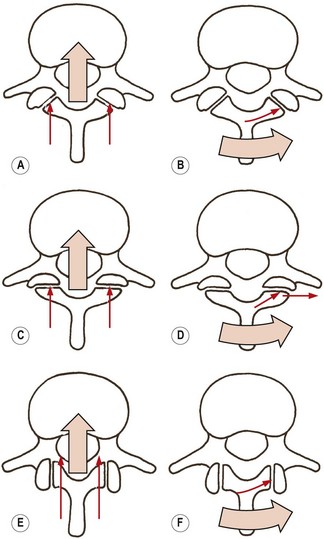
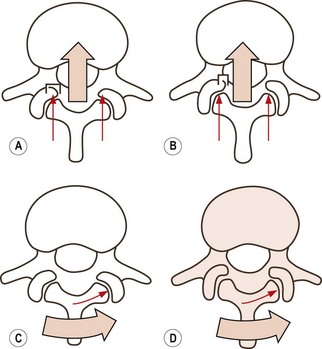
In the case of planar zygapophysial joints, the analysis is straightforward. In a joint with an oblique orientation, the superior articular facets face backwards and medially (Fig. 3.5A). Because of their backward orientation, these facets can resist forward displacement. If the upper vertebra in a joint attempts to move forwards, its inferior articular processes will impact against the superior articular facets of the lower vertebra, and this impaction will prevent further forward movement (see Fig. 3.5A).
Similarly, the medial orientation of the superior articular facets allows them to resist rotation. As the upper vertebra attempts to rotate, say, anticlockwise as viewed from above, its right inferior articular facet will impact against the right superior articular facet of the vertebra below, and further rotation will be arrested (Fig. 3.5B).
Maximum resistance to forward displacement will be exerted by the superior articular facets that are orientated at 90° to the sagittal plane, for then the facets face fully backwards and the entire articular surface directly opposes the movement (Fig. 3.5C). Such facets, however, are less capable of resisting rotation, for during rotation the inferior articular facet impacts the superior articular facet at an angle and is able to glance off the superior articular facet (Fig. 3.5D).
Joints orientated parallel to the sagittal plane afford no resistance to forward displacement. The inferior articular facets are able simply to slide past the superior articular facets (Fig. 3.5E). However, such joints provide substantial resistance to rotation (Fig. 3.5F).
In the case of joints with curved articular surfaces, the situation is modified to the extent that particular portions of the articular surface are involved in resisting different movements. In curved joints, the anteromedial end of the superior articular facet faces backwards, and it is this portion of the facet that will resist forward displacement. As the upper vertebra attempts to move forwards, its inferior articular facets will impact against the anteromedial portion of the superior articular facets of the vertebra below (Fig. 3.6A). The degree of resistance will be proportional to the surface area of the backward-facing, anteromedial portion of the superior articular facet. Thus, C-shaped facets (Fig 3.6A) have a larger surface area facing backwards and afford greater resistance than J-shaped facets (Fig. 3.6B), which have only a small portion of their articular surface facing backwards.
Rotation is well resisted by both C- and J-shaped facets, for virtually the entire articular surface is brought into contact by this movement (Fig. 3.6C,D).
The additional significance of variations in orientation of zygapophysial joints in relation to the biomechanical requirements of joints at different levels, the age changes they suffer and their liability to injury are explored in Chapters 5, 8, 13 and 15.
Articular cartilage
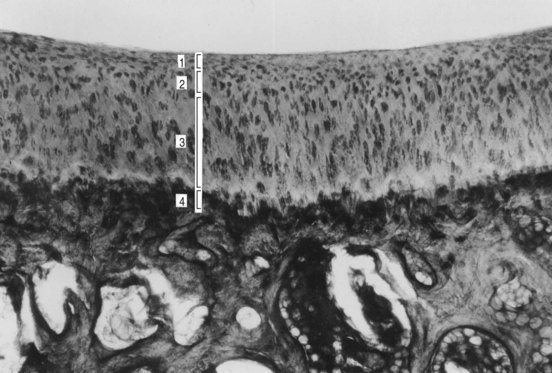
Articular cartilage covers the facets of the superior and inferior articular processes, and as a whole assumes the same concave or convex curvature as the underlying facet. In a normal joint, the cartilage is thickest over the centre of each facet, rising to a height of about 2 mm.4,5 Histologically, four zones may be recognised in the cartilage (Fig. 3.7).5 The superficial, or tangential, zone consists of three to four layers of ovoid cells whose long axes are orientated parallel to the cartilage surface. Deep to this zone is a transitional zone in which cartilage cells are arranged in small clusters of three to four cells. Next deeper is a radial zone, which constitutes most of the cartilage thickness. It consists of clusters of six to eight large cells whose long axes lie perpendicular to the cartilage surface. The deepest zone is the calcified zone, which uniformly covers the subchondral bone plate and constitutes about one-sixth of the total cartilage thickness. Conspicuously, the radial zone of cartilage is identifiable only in the central regions of the cartilage. Towards the periphery, the calcified zone is covered only by the transitional and tangential zones. As is typical of all articular cartilage, the cartilage cells of the zygapophysial joints are embedded in a matrix of glycosaminoglycans and type II collagen; however, the most superficial layers of the tangential zone, forming the surface of the cartilage, lack glycosaminoglycans and consist only of collagen fibres running parallel to the cartilage surface. This thin strip is known as the lamina slendens.6
The articular cartilage rests on a thickened layer of bone known as the subchondral bone (see Fig. 3.7). In normal joints there are no particular features of the subchondral bone. However, the age changes and degenerative changes that affect the articular cartilage also affect the subchondral bone, and these changes are described in Chapter 13.
Capsule
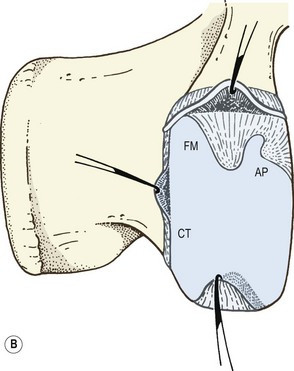
Around its dorsal, superior and inferior margins, each lumbar zygapophysial joint is enclosed by a fibrous capsule, formed by collagen fibres passing more or less transversely from one articular process to the other (Figs. 3.1, 3.8). Along the dorsal aspect of the joint, the outermost fibres of the capsule are attached about 2 mm from the edge of the articular cartilage but some of the deepest fibres attach into the margin of the articular cartilage (Figs. 3.8, 3.9).7,8 At the superior and inferior poles of the joint, the capsule attaches further from the osteochondral junctions, creating subcapsular pockets over the superior and inferior edges of both the superior and inferior articular processes, which in the intact joint are filled with fat (see Fig. 3.8).9 Anteriorly, the fibrous capsule of the joint is replaced entirely by the ligamentum flavum (see Ch. 4), which attaches close to the articular margin (Fig. 3.9).9–11
The capsule has been found to consist of two layers.12 The outer layer consists of densely packed parallel collagen fibres. This layer is 13–17 mm long in the superior and middle regions of the joint, but 15–20 mm long over the inferior pole of the joint. The inner layer consists of irregularly orientated elastic fibres; it is 6–10 mm long over the superior and middle regions of the joint and 9–16 mm long over its inferior pole.
The joint capsule is thick dorsally and is reinforced by some of the deep fibres of the multifidus muscle (see Ch. 9).5,7,12,13 At the superior and inferior poles of the joint, the capsule is abundant and loose.9 Superiorly, it balloons upwards towards the base of the next transverse process. Inferiorly, it balloons over the back of the lamina (see Fig. 3.8). In both the superior and inferior parts of the capsule, there is a tiny hole, or foramen, that permits the passage of fat from within the capsule to the extracapsular space (see Fig. 3.10).9
Intra-articular structures
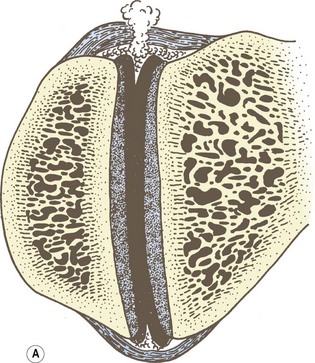
There are two principal types of intra-articular structure in the lumbar zygapophysial joints. These are fat, and what may be referred to as ‘meniscoid’, structures. The fat basically fills any leftover space underneath the capsule. It is located principally in the subcapsular pockets at the superior and inferior poles of the joint (Fig. 3.10). Externally, it is covered by the capsule, while internally it is covered by the synovium. It communicates with the fat outside the joint through the foramina in the superior and inferior capsules. Superiorly, this extracapsular fat lies lateral to the lamina and dorsal to the intervertebral foramen.5,9 Inferiorly, it lies dorsal to the upper end of the lamina of the vertebra and separates the bone from the overlying multifidus muscle.
There have been many studies and differing interpretations of the meniscoid structures of the lumbar zygapophysial joints3,9,14–28 but the most comprehensive study of these structures identifies three types.29,30
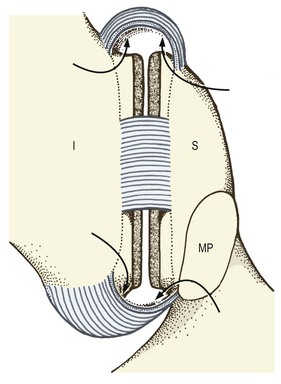
The simplest and smallest structure is the connective tissue rim. This is simply a wedge-shaped thickening of the internal surface of the capsule, which, along the dorsal and ventral margins of the joint, fills the space left by the curved margins of the articular cartilages (Fig. 3.11). The second type of structure is an adipose tissue pad. These are found principally at the superoventral and inferodorsal poles of the joint. Each consists of a fold of synovium enclosing some fat and blood vessels (see Fig. 3.11). At the base of the structure, the synovium is reflected onto the joint capsule to become continuous with the synovium of the rest of the joint, and the fat within the structure is continuous with other fat within the joint. These adipose tissue pads project into the joint cavity for a short distance (about 2 mm).
The largest of the meniscoid structures are the fibro-adipose meniscoids. These project from the inner surface of the superior and inferior capsules. They consist of a leaf-like fold of synovium which encloses fat, collagen and some blood vessels (see Fig. 3.11). The fat is located principally in the base of the structure, where it is continuous with the rest of the fat within the joint, and where it communicates with the extracapsular fat through the superior and inferior capsular foramina. The collagen is densely packed and is located towards the apex of the structure. Fibro-adipose meniscoids are long and project up to 5 mm into the joint cavity.
Differing and conflicting interpretations have marked the literature on zygapophysial intra-articular structures, and there is no conventional, universal nomenclature that can be ascribed to them. However, it is clear from their histology that none is really a meniscus which resembles the menisci of the knee joint or the temporomandibular joint. They do, nonetheless, resemble the intra-articular structures found in the small joints of the hand.31,32 The connective tissue rims described above are most easily interpreted as a thickening of the joint capsule that simply acts as a space filler, although it may be that they also serve to increase the surface area of contact when articular facets are impacted, and thereby transmit some load.9,18
The adipose tissue pads and the fibro-adipose meniscoids have been interpreted as serving a protective function.29 During flexion of an intervertebral joint, the inferior articular facet slides upwards some 5–8 mm along the superior articular facet.9,33 This movement results in cartilages of the upper portion of the inferior facet and the lower portion of the superior facet becoming exposed. The adipose tissue pads and the fibro-adipose meniscoids are suitably located to cover these exposed articular surfaces, and to afford them some degree of protection during this movement. By remaining in contact with the exposed articular cartilage, the synovium-covered pads and meniscoids can maintain a film of synovial fluid between themselves and the cartilage. This ensures that the cartilage is lubricated against friction as it moves back into its resting position against the surface of the apposing articular facet.
There is also another form of intra-articular structure derived from the articular cartilage but it is apparently formed artificially by traction on the cartilage. This structure is described in Chapter 13, and the clinical relevance of all intra-articular structures is considered in Chapter 15.
1 Benini A. Das klein Gelenk der lenden Wirbelsaule. Fortschr Med. 1979;97:2103-2106.
2 Bogduk N, Engel R. The menisci of the lumbar zygapophysial joints. A review of their anatomy and clinical significance. Spine. 1984;9:454-460.
3 Horwitz T, Smith RM. An anatomical, pathological and roentgenological study of the intervertebral joints of the lumbar spine and of the sacroiliac joints. Am J Roentgenol. 1940;43:173-186.
4 Delmas A, Ndjaga-Mba M, Vannareth T. Le cartilage articulaire de L4–L5 et L5–S1. Comptes Rendus de l’Association des Anatomistes. 1970;147:230-234.
5 Dorr WM. Uber die Anatomie der Wirbelgelenke. Arch Orthop Unfallchir. 1958;50:222-234.
6 Dorr WM. Nochmals zu den Menisci in den Wirbelbogengelenken. Z Orthop Ihre Grenzgeb. 1962;96:457-461.
7 Emminger E. Les articulations interapophysaires et leurs structures meniscoides vues sous l’angle de la pathologie. Ann Med Phys. 1972;15:219-238.
8 Engel R, Bogduk N. The menisci of the lumbar zygapophysial joints. J Anat. 1982;135:795-809.
9 Giles LGF. Human lumbar zygapophyseal joint inferior recess synovial folds: a light microscope examination. Anat Rec. 1988;220:117-124.
10 Giles LGF. The surface lamina of the articular cartilage of human zygapophyseal joints. Anat Rec. 1992;233:350-356.
11 Giles LGF, Taylor JR. Inter-articular synovial protrusions. Bull Hosp Joint Dis. 1982;42:248-255.
12 Giles LGF, Taylor JR, Cockson A. Human zygapophyseal joint synovial folds. Acta Anat. 1986;126:110-114.
13 Guntz E. Die Erkrankungen der Zwischenwirbelgelenke. Arch Orthop Unfallchir. 1933–1934;34:333-355.
14 Hadley LA. Anatomico-roentgenographic studies of the posterior spinal articulations. Am J Roentgenol. 1961;86:270-276.
15 Hadley LA. Anatomico-roentgenographic Studies of the Spine. Springfield: Thomas; 1964.
16 Hirsch C, Lewin T. Lumbosacral synovial joints in flexion-extension. Acta Orthop Scand. 1968;39:303-311.
17 Kos J. Contribution a l’étude de l’anatomie et de la vascularisation des articulations intervertébrales. Bull Ass Anat. 1969;142:1088-1105.
18 Kos J, Wolf J. Les ménisques intervertébraux et leur rôle possible dans les blocages vertébraux. Ann Med Phys. 1972;15:203-218.
19 Kos J, Wolf J. Die ‘Menisci’ der Zwischenwirbelgelenke und ihre mogliche Rolle bei Wirbelblockierung. Man Med. 1972;10:105-114.
20 Lewin T. Osteoarthritis in lumbar synovial joints: a morphologic study. Acta Orthop Scand. 1964;176(Suppl. 73):1-112.
21 Lewin T, Moffet B, Viidik A. The morphology of the lumbar synovial intervertebral joints. Acta Morphol Neerlando-Scand. 1962;4:299-319.
22 Marchi GF. Le articolazioni intervertebrali. La Clinica Ortopedica. 1963;15:26-33.
23 Panjabi MM, Oxland T, Takata K, et al. Articular facets of the human spine: quantitative three-dimensional anatomy. Spine. 1993;18:1298-1310.
24 Ramsey RH. The anatomy of the ligamenta flava. Clin Orthop. 1966;44:129-140.
25 Santo E. Zur Entwicklungdgeschichte und Histologie der Zwischenscheiben in den kleinen Gelenken. Z Anat Entwickl Gesch. 1935;104:623-634.
26 Santo E. Die Zwischenscheiben in den kleinen Gelenken. Anat Anz. 1937;83:223-229.
27 Tager KH. Wirbelmeniskus oder synovial Forsatz. Z Orthop Ihre Grenzgeb. 1965;99:439-447.
28 Taylor JR, Twomey LT. Age changes in lumbar zygapophyseal joints. Spine. 1986;11:739-745.
29 Twomey LT, Taylor JR. Age changes in the lumbar articular triad. Aust J Physio. 1985;31:106-112.
30 Wolf J. The reversible deformation of the joint cartilage surface and its possible role in joint blockage. Rehabilitacia. 1975;8(Suppl. 10–11):30-36.
31 Yamashita T, Minaki Y, Ozaktay AC, et al. A morphological study of the fibrous capsule of the human lumbar facet joint. Spine. 1996;21:538-543.
32 Yong-Hing K, Reilly J, Kirkaldy-Willis WH. The ligamentum flavum. Spine. 1976;1:226-234.
33 Zaccheo D, Reale E. Contributo alla conoscenza delle articolazioni tra i processi articolari delle vertebre dell’uomo. Archivio di Anatomia. 1956;61:1-46.