10 The wrist and hand
History and examination
Much of what has already been written about the history-taking for the shoulder and elbow also holds true for the wrist and hand: it is part of a kinematic chain and clinical thinking must be directed to the other components of that chain, which may be responsible both for disrupting distal biomechanics and perpetuating symptoms and for referring proximal pathology.1 It is also necessary to be alert for ‘double crush’ mechanisms of neural entrapment: the nerves that pass through the wrist are also subject to entrapment in the elbow, arm and thoracic outlet, which can refer pain or be comorbid with local entrapment.2
Examination of the wrist and hand, perhaps unsurprisingly, reflects that of the ankle and foot, with emphasis on observation; active and passive ranges of motion; neurological assessment; digital palpation; and muscle testing. There is, again, a paucity of meaningful special orthopaedic tests; the one exception to this is Finkelstein’s test for stenosing tenosynovitis of the tendons of extensor pollicis brevis and abductor pollicis longus.3 This test involves the patient opposing their thumb so that it lies across the palm, then grasping it with the fingers so that it lies within a clenched fist. The examiner then forcibly adducts the thumb to recreate the patient’s symptoms. The examination should also include evaluation of the elbow, shoulder, thoracic outlet and cervical spine.4
The presence of obvious and persistent neurological signs and symptoms would, in the first instance, be likely to precipitate referral for nerve conduction studies; otherwise, diagnostic imaging is the next step for the inconclusive examination or unresponsive patient.5,6
Protocols
The MR imaging study will normally consist of all three imaging planes: coronal, axial and sagittal, which are normally planned from the axial scout view. T1-weighted and T2-weighted sequences are usually performed in one or more imaging planes, with a slice thickness of 1 to 3 mm being adopted. However, depending on the clinical indication for MR imaging of the wrist and hand, particular sequences or even planes may be selected. In the wrist, the imaging study includes the distal radius and ulna up to the bases of the metacarpal bones. In the hand, the imaging study will normally include the distal carpal row to just beyond the distal aspects of the fingers.7
For either area, contrast may be added, depending on the nature of the clinical situation being investigated. The contrast may be added via the intravenous route, to attempt to differentiate a soft tissue mass or active inflammation8 or, in some institutions, injected directly in to the joint to perform MR arthrography9; however, due to the inherent contrast from the fluid in the wrist, these procedures are not usually necessary. Some institutions have advocated imaging with varying positions of the wrist, placing the patient in pronation and supination in order to further study the ligamentous relationships in these positions10; however, this has not been adopted as standard protocol in most imaging institutions.
Normal and abnormal imaging appearances of the wrist and hand
Osseous structures
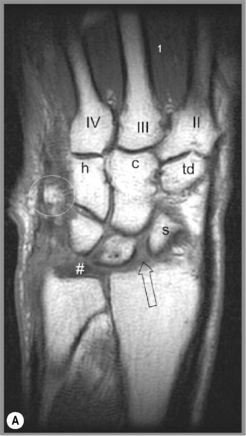
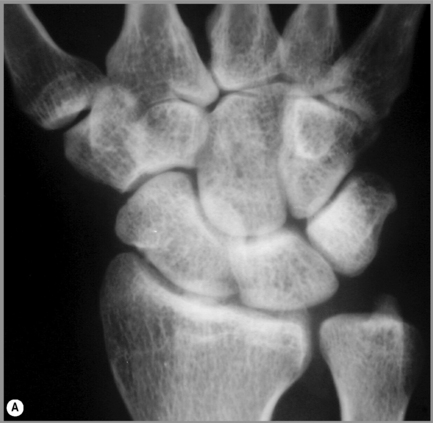
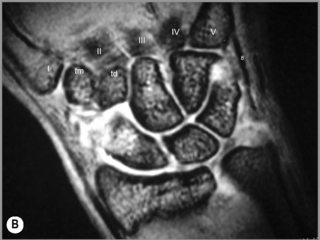
The coronal imaging study will provide information regarding a number of areas, including the overall gross alignment (Figure 10.01, Box 10.01). On these images, the convex head of the ulna and the articular surface of the distal radius should be at the same level; any variance from this can indicate abnormal stresses being placed on the wrist, and is associated with a number of syndromes (Table 10.01).11–15
Table 10.01 Syndromes associated with distal radioulnar misalignment
| Ulna proximal to radius > 2 mm | Radius proximal to ulna > 2 mm |
|---|---|
It is also essential to determine that all the carpal bones are present in the proximal and distal carpal rows (Figure 10.01). Carpal coalition is a condition whereby incomplete segmentation has occurred, resulting in two or more of the carpal bones appearing fused; most commonly, the lunate and triquetrum or the capitate and hamate,16–18 although any adjacent bones may seemingly be involved.19–25 The distal carpals may also be congenitally fused with the metacarpals, the most common coalition being between the second metacarpal and trapezoid.26 Accessory ossicles may be present, which represent a normal variation, usually without clinical consequence to either the patient or physician; one exception to this is the presence of an os styloideum, a common bony protuberance located on the dorsal surface of the base of the second and third metacarpals, which may be associated with degenerative changes, bursitis or ganglia.26,27 In patients with a history of trauma, ossification may occur in and around tendons, resulting in the appearance of osseous lesions about the wrist and hand, a form of myositis ossificans (Figure 10.02).28
Triangular fibrocartilage complex
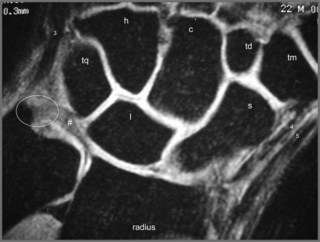
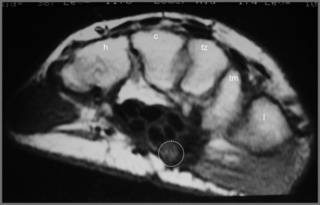
Familiarity with the soft tissue structures of the wrist and hand is particularly important, owing to their role in maintaining the stability of the wrist. In the coronal plane, the triangular fibrocartilage complex (TFCC) is well demonstrated with its contributing structures, including the meniscus and ulnar collateral ligament (Figure 10.01). The TFCC is a biconcave structure located in the region of the wrist between the ulna and the proximal carpal row, with attachments to the ulnar styloid process by bands of tissue and similarly attached to the radius (Figure 10.03). It stabilizes the ulnocarpal and radioulnar joints, facilitates complex movements at the wrist and distributes loads from the carpus to the ulna.29,30 Between the TFCC and the radius is a region of intermediate signal on MR images, which represents hyaline cartilage.
Tendons
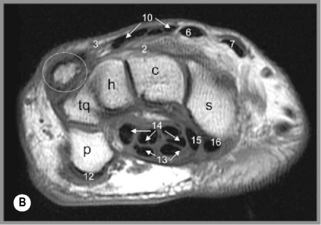
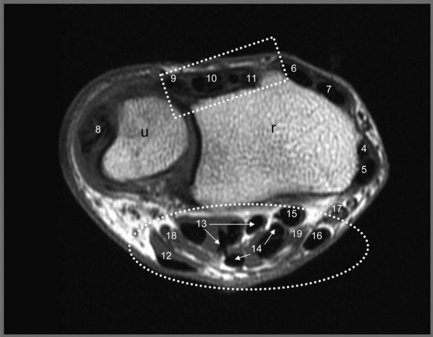
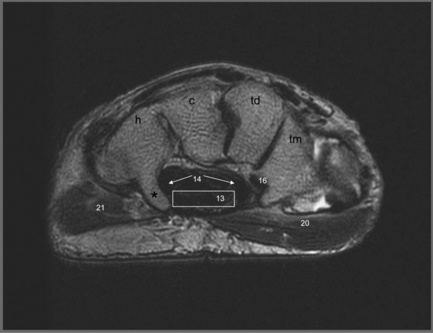
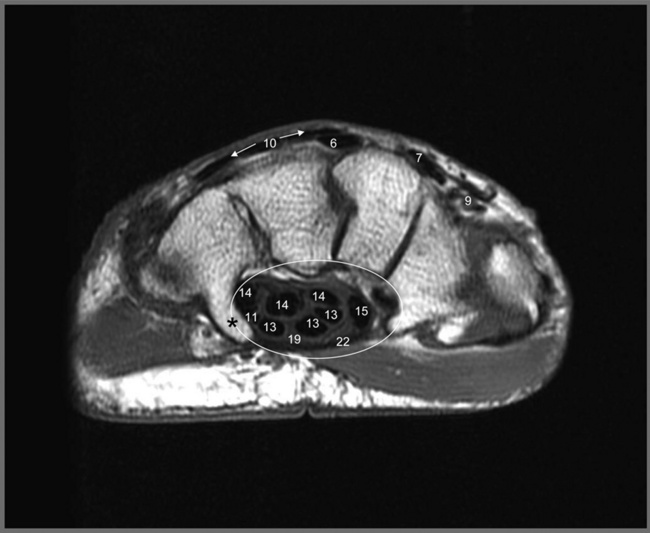
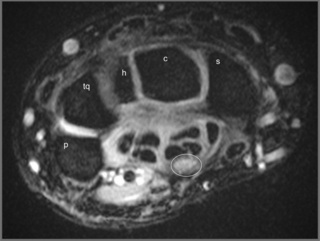
The tendons of the wrist can be best evaluated in the axial plane; in the hand, the sagittal plane is, initially, the primary plane for diagnostic information. The normal appearance of a tendon in the wrist and hand is that of a low signal intensity structure that is both linear and continuous. About the wrist, the tendons are divided into compartments for both anatomical and imaging description. The two main regions for the tendons of the wrist are the extensor and flexor groups (Figure 10.04). The median nerve lies amongst the flexor tendons as they travel through the wrist and may be involved in the development of symptoms and signs of carpal tunnel syndrome (Figure 10.05).31 The extensor tendons run along the dorsal aspect of the wrist towards the hand and may cross over each other, leading to friction syndromes. These tendons may vary in their shape, with the extensor carpi radialis brevis appearing rather elongated in the axial plane (Figure 10.06). The tendons are normally surrounded by a small degree of fluid, which can accumulate in conditions such as tenosynovitis. This can be caused by direct trauma or by systemic disorders that promote a generalized inflammatory process, such as rheumatoid arthritis (Figure 10.07) and are often accompanied by osseous involvement such as erosions.
Nerves
Median nerve
Neural structures can be assessed well with MR imaging. When a patient presents with symptoms and signs of carpal tunnel syndrome, differentiation from proximal neuropathies can be challenging and the MR image may be useful to determine the presence and extent of any local irritation to the median nerve.32 The median nerve should normally be of a slightly grey or higher signal intensity as compared with the surrounding tendons in the carpal tunnel of normal dimension.31 In the proximal carpal tunnel, the nerve is slightly flatter than the surrounding tube-like flexor tendons. As it travels more distally through the carpal tunnel, it becomes even flatter in shape.
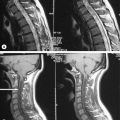
Carpal tunnel syndrome may arise due to a number of conditions, but is primarily considered a compressive neuropathy.33 Such compression may occur due to a simple local lesion, such as a ganglion within the carpal tunnel, or from a tenosynovitis of the flexor tendons, causing a decrease in the space that the median nerve occupies within the tunnel.34–36 Relevant imaging findings from carpal tunnel syndrome may therefore include the presence of tenosynovitis of the flexor tendons, which will appear as areas of increased signal intensity about the tendons on the T2-weighted sequences. The addition of intravenous contrast may enhance a T1 sequence. The nerve may demonstrate an increase in its size and signal intensity on the fluid-sensitive sequences (Figure 10.08). MR imaging is not used routinely in the primary diagnosis of carpal tunnel syndrome,6 but is best employed to determine the cause of symptoms and signs in persistent cases or to evaluate scar tissue formation following surgery, which can itself be a cause of median nerve irritation (Figure 10.09).37,38
Because of the potential complications of surgical intervention, conservative care is recommended; steroid injections and splinting can often be effective and both manual therapy and acupuncture have shown some benefit to patients.39–42
Ulnar nerve
The ulnar nerve may be compressed in the tunnel of Guyon, which lies between the pisiform and hamate and under their interconnecting ligament. Common causes of compression include ganglia, trauma and the presence of accessory muscles, all of which can be easily identified on MR imaging.43 The site of compression needs to be differentiated from cubital tunnel syndrome (Chapter 9), which will affect the extensor carpi ulnaris in addition to distally innervated structures; however, it is also possible to differentiate between compression of the deep and superficial branches (Box 10.02).
Ligaments
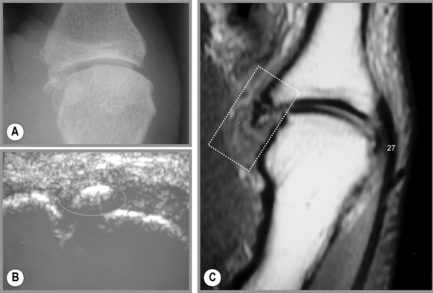
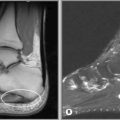
Game-keeper’s thumb is an avulsion injury of the base of the proximal phalanx, commonly related to a forced abduction movement in sports such as skiing or from the recoil of a gun (hence the eponymic name) whereby the ulnar collateral ligament is disrupted along with a small fragment of bone from its insertion into the proximal phalanx. This ligament is important for conferring stability to the thumb, and, although basic imaging may be used to demonstrate the bony lesion, MR imaging depicts the bony and soft tissue injury with exquisite detail, which is important in the prognosis and most appropriate clinical management of the patient (Figure 10.10).
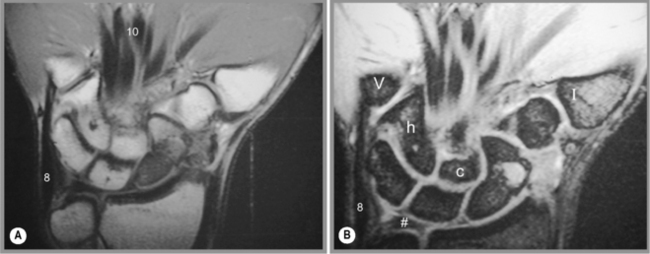
MR imaging may also be used to determine the presence of radiographically occult fractures (Figure 10.11). The scaphoid is the most commonly fractured bone in the wrist, and, if initial radiographs are negative, options may consist of immobilizing the patient and re-radiographing 10 days later, or, if such facilities exist, performing MR imaging to determine the presence of any fracture and also to follow the development of potential complications such as avascular necrosis. This condition can also develop spontaneously in the paediatric lunate (Kienböck’s disease) (Figure 10.12).44,45
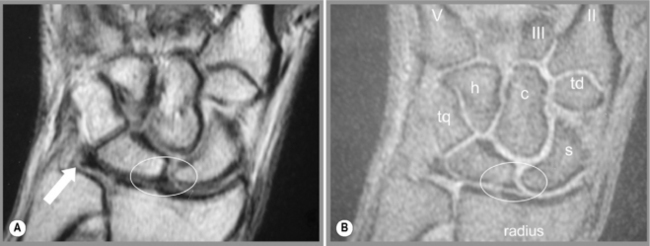
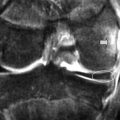
Falls on the outstretched hand (FOOSH) may also affect the ligaments about the wrist, which need to be scrutinized, particularly on the coronal sequence. The ligaments, such as the scapholunate ligament, should be seen as a linear low-signal continuous structure connecting the scaphoid and lunate. In the case of disruption of the ligament, a slightly increased distance may be noted between the scaphoid and lunate (normal range is 2 to 4 mm) as well as disruption of the linear signal, which appears discontinuous or irregular (Figure 10.13).43,45
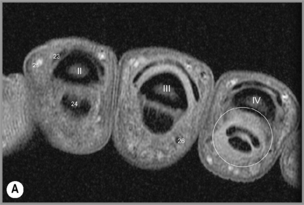
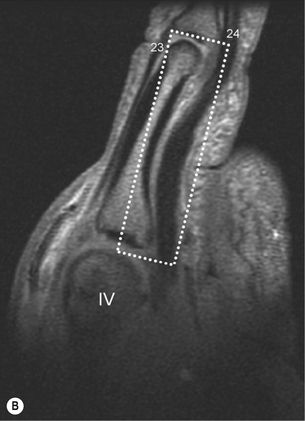
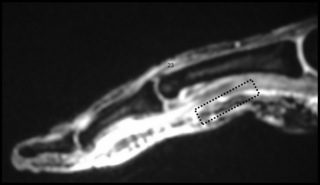
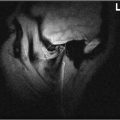
Lacerating injuries to the hand or wrist may result in damage to soft tissue or bony structures. A commonly sustained injury is laceration of the fingers, whereby the tendons of the fingers may be partially or completely ruptured (Figure 10.14). The patient usually presents with a history of acute trauma, commonly involving a sharp utensil, with clinical deformity of the finger and the inability to perform flexion or extension. Whereas ultrasound may be useful to determine the extent of injury, it is highly operator-dependent.46 MR imaging will provide superior information with respect to both bony and soft tissue damage, providing important information regarding the clinical diagnosis and management of the patient.
Tumours
The majority of neoplasms in the wrist and hand are benign; the most common cause of such growths are ganglia, fibrous-walled masses attached to ligaments, joint capsules and tendon sheaths. More commonly found in females, they only become painful when pressing against adjacent structures; their cause appears to relate to chronic irritation.47 MR imaging will reveal ganglia as low intensity structures on T1-weighted imaging; on T2-weighted imaging, the signal intensity is higher though generally diffuse with characteristic thin, low signal lines representing septa that subdivide the internal architecture of the ganglion. The most common differential is the presence of accessory, anomalous muscles, most commonly extensor digitorum manus brevis, found on the dorsum of the wrist medial to the tendon of extensor indices. The characteristic location helps to differentiate it from a ganglion.29,43
The second commonest soft tissue mass about the wrist is the giant cell tumour of the tendon sheath; a localized form of pigmented villonodular synovitis, characteristically noted on the volar digital surfaces; their differentiation is further helped by their appearance as low signal intensity structures on both T1- and T2-weighted images.43
1 Young M.F. The physics of anatomy. In: Essential Physics for Musculoskeletal Medicine. Edinburgh: Elsevier; 2009.
2 Pierre-Jerome C., Bekkelund S.I. Magnetic resonance assessment of the double-crush phenomenon in patients with carpal tunnel syndrome: a bilateral quantitative study. Scand J Plast Reconstr Surg Hand Surg. 2003;37(1):46-53.
3 Kutsumi K., Amadio P.C., Zhao C., et al. Finkelstein’s test: a biomechanical analysis. J Hand Surg Am. 2005;30(1):130-135.
4 Bates B. The musculoskeletal system. In: Bates B., editor. A Guide to Physical Examination. 3rd ed. Philadelphia: JB Lippincott; 1983:324-370.
5 Keith M.W., Masear V., Amadio P.C., et al. Treatment of carpal tunnel syndrome. J Am Acad Orthop Surg. 2009;17(6):397-405.
6 Keith M.W., Masear V., Chung K., et al. Diagnosis of carpal tunnel syndrome. J Am Acad Orthop Surg. 2009;17(6):389-396.
7 Kaplan P., Helms C., Dussault R., Anderson M. Musculoskeletal MRI. Philadelphia: WB Saunders, 2001.
8 Eshed I., Althoff C.E., Schink T., et al. Low-field MRI for assessing synovitis in patients with rheumatoid arthritis. Impact of Gd-DTPA dose on synovitis scoring. Scand J Rheumatol. 2006;35(4):277-282.
9 Theumann N.H., Etechami G., Duvoisin B., et al. Association between extrinsic and intrinsic carpal ligament injuries at MR arthrography and carpal instability at radiography: initial observations. Radiology. 2006;238(3):950-957.
10 Pfirrmann C.W., Theumann N.H., Chung C.B., et al. What happens to the triangular fibrocartilage complex during pronation and supination of the forearm? Analysis of its morphology and diagnostic assessment with MR arthrography. Skeletal Radiol. 2001;30(12):677-685.
11 Singh A., Singh O.P. A rare injury of distal radial and ulnar epiphysis. J Indian Med Assoc. 2007;105(8):466. 468
12 Glasson E.J., Bower C., Thomson M.R., et al. Diagnosis of Rett syndrome: can a radiograph help? Dev Med Child Neurol. 1998;40(11):737-742.
13 Darrow J.C.Jr, Linscheid R.L., Dobyns J.H., et al. Distal ulnar recession for disorders of the distal radioulnar joint. J Hand Surg Am. 1985;10(4):482-491.
14 DiFiori J.P., Puffer J.C., Aish B., Dorey F. Wrist pain, distal radial physeal injury, and ulnar variance in young gymnasts: does a relationship exist? Am J Sports Med. 2002;30(6):879-885.
15 Caine D., Howe W., Ross W., Bergman G. Does repetitive physical loading inhibit radial growth in female gymnasts? Clin J Sport Med. 1997;7(4):302-308.
16 Mellado J.M., Calmet J., Domenech S., Sauri A. Clinically significant skeletal variations of the shoulder and the wrist: role of MR imaging. Eur Radiol. 2003;13(7):1735-1743.
17 Marburger R., Burgess R.C. Symptomatic lunate-triquetral coalition. J South Orthop Assoc. 1995;4(4):307-310.
18 Delaney T.J., Eswar S. Carpal coalitions. J Hand Surg Am. 1992;17(1):28-31.
19 Terrence J.J.J. Congenital fusion of the trapezium and trapezoid. Rom J Morphol Embryol. 2008;49(3):417-419.
20 Silverman A.T., Shin S.S., Paksima N. Asymptomatic pisiform-hamate coalition: a case report. Am J Orthop. 2007;36(6):E88-E90.
21 Louaste J., Amhajji L., Rachid K. [Pisiform-hamate synostosis with ulnar neuropathy. Case report]. Chir Main. 2007;26(3):170-172.
22 Kawamura K., Yajima H., Takakura Y. Pisiform and hamate coalition: case report and review of literature. Hand Surg. 2005;10(1):101-104.
23 Boya H., Ozcan O., Arac S., Tandogan R. Incomplete scapholunate and trapeziotrapezoid coalitions with an accessory carpal bone. J Orthop Sci. 2005;10(1):99-102.
24 Ingram C., Hall R.F., Gonzalez M. Congenital fusion of the scaphoid, trapezium, trapezoid and capitate. J Hand Surg Br. 1997;22(2):167-168.
25 Oner F.C., de Vries H.R. Isolated capitatolunate coalition: a case report. J Bone Joint Surg Br. 1994;76(5):845-856.
26 Alemohammad A.M., Nakamura K., El-Sheneway M., Viegas S.F. Incidence of carpal boss and osseous coalition: an anatomic study. J Hand Surg Am. 2009;34(1):1-6.
27 Hazlett J.W. The third metacarpal boss. Int Orthop. 1992;16(4):369-371.
28 Berquist T. MRI of the Musculoskeletal System, 4th ed. Philadelphia: Lippincott Williams and Wilkins, 2000.
29 Standring S., editor. Gray’s Anatomy – Pectoral girdle and upper limb: Wrist and hand (Section 53). Edinburgh: Elsevier, 2009.
30 Moore K. The upper limb. In Clinically Oriented Anatomy, 2nd ed, Baltimore: Williams and Wilkins; 1985:626-793.
31 Bower J.A., Stanisz G.J., Keir P.J. An MRI evaluation of carpal tunnel dimensions in healthy wrists: Implications for carpal tunnel syndrome. Clin Biomech (Bristol, Avon). 2006;21(8):816-825.
32 Kim S., Choi J.Y., Huh Y.M., et al. Role of magnetic resonance imaging in entrapment and compressive neuropathy – what, where, and how to see the peripheral nerves on the musculoskeletal magnetic resonance image: part 1. Overview and lower extremity. Eur Radiol. 2007;17(1):139-149.
33 Lindsay K., Bone I., Callander R. Localised neurological disease and its management. In: Neurology and Neurosurgery Illustrated. Edinburgh: Elsevier; 1991:213-466.
34 Crowley B., Gschwind C.R., Storey C. Selective motor neuropathy of the median nerve caused by a ganglion in the carpal tunnel. J Hand Surg Br. 1998;23(5):611-612.
35 Nourissat G., Fournier E., Werther J.R., et al. Acute carpal tunnel syndrome secondary to pyogenic tenosynovitis. J Hand Surg Br. 2006;31(6):687-688.
36 Rashid M., Sarwar S.U., Haq E.U., et al. Tuberculous tenosynovitis: a cause of carpal tunnel syndrome. J Pak Med Assoc. 2006;56(3):116-118.
37 Stutz N.M., Gohritz A., Novotny A., et al. Clinical and electrophysiological comparison of different methods of soft tissue coverage of the median nerve in recurrent carpal tunnel syndrome. Neurosurgery. 2008;62(3 suppl 1):194-199. discussion 199–200
38 Stutz N., Gohritz A., van Schoonhoven J., Lanz U. Revision surgery after carpal tunnel release—analysis of the pathology in 200 cases during a 2 year period. J Hand Surg Br. 2006;31(1):68-71.
39 Napadow V., Kettner N., Liu J., et al. Hypothalamus and amygdala response to acupuncture stimuli in carpal tunnel syndrome. Pain. 2007;130(3):254-266.
40 Napadow V., Liu J., Li M., et al. Somatosensory cortical plasticity in carpal tunnel syndrome treated by acupuncture. Hum Brain Mapp. 2007;28(3):159-171.
41 Burke J., Buchberger D.J., Carey-Loghmani M.T., et al. A pilot study comparing two manual therapy interventions for carpal tunnel syndrome. J Manipulative Physiol Ther. 2007;30(1):50-61.
42 Claes F., Verhagen W.I., Meulstee J. Current practice in the use of nerve conduction studies in carpal tunnel syndrome by surgeons in The Netherlands. J Hand Surg Eur Vol. 2007;32(6):663-667.
43 Helms C., Major N., Anderson M.W., et al. Wrist and hand. In Musculoskeletal MRI, 2nd ed, Philadelphia: Elsevier Saunders; 2009:244-272.
44 Memarsadeghi M., Breitenseher M.J., Schaefer-Prokop C., et al. Occult scaphoid fractures: comparison of multidetector CT and MR imaging—initial experience. Radiology. 2006;240(1):169-176.
45 Rowe L., Yochum T., editors. Essentials of Skeletal Radiology, 2nd ed, Baltimore: Williams and Wilkins, 2004.
46 Rasmussen O.S. Sonography of tendons. Scand J Med Sci Sports. 2000;10(6):360-364.
47 Bogumill G.P., Sullivan D.J., Baker G.I. Tumors of the hand. Clin Orthop Relat Res. 1975;108:214-222.