CHAPTER 4 The white lung field
4.1 Collapse
Check the position of the oblique and horizontal fissures (pp. 13 and 14). Any displacement from their normal position suggests collapse. Collapse of any of the lobes of the lung gives a distinct appearance on the X-ray.


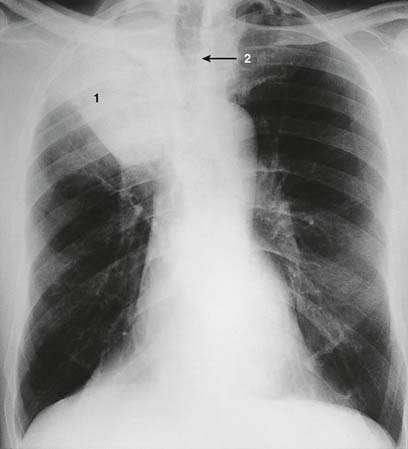
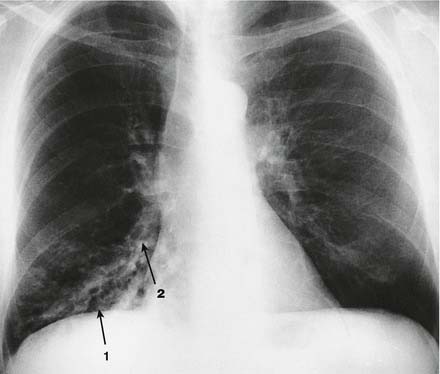
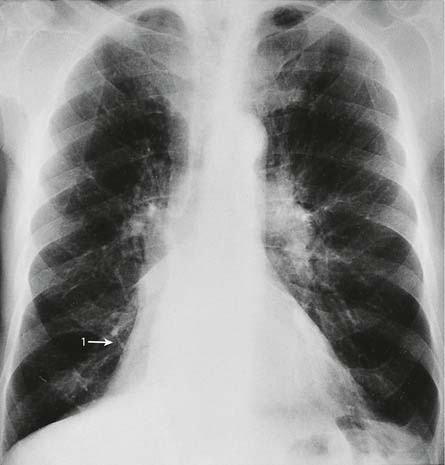
1. Right upper lobe collapse. There is an area of whiteness in the upper zone of the right lung (1). The horizontal fissure is elevated, there is an apparent right upper hilar ‘mass’, the trachea is deviated to the right (2) and the ribs over the area of whiteness are closer together than is normal. On the lateral film the increased whiteness in the uppermost part of the chest may be seen.

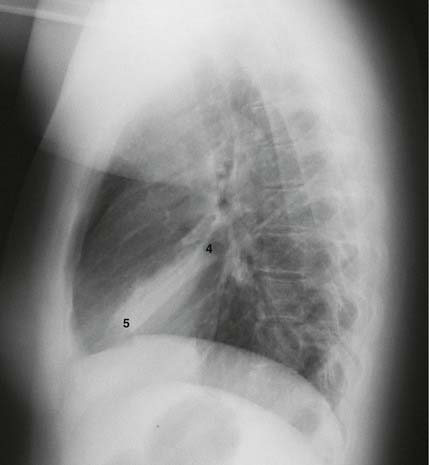
2. Right middle lobe collapse. This can be difficult to spot. The right diaphragm may be slightly raised (1) and the horizontal fissure (2) may be lower than usual. The upper part of the lower zone may have a hazy white appearance (3) and the heart border is sometimes indistinct. It is easier to detect in the lateral film. There is a triangular area of whiteness with its apex at the hilum (4) and its base running between the sternum and the diaphragm (5).
3. Right lower lobe collapse. There is a whiteness immediately above the diaphragm (1) causing a loss of its outline. On the lateral film there is a white triangle at the lower posterior part of the lung field (2). Note how the outline of the right heart border is maintained.

4. Left upper lobe collapse. This is difficult to spot. Remember that most of the left upper lobe lies in front of, as opposed to above, the left lower lobe. When it collapses it causes a haze to appear over the whole of the left lung field.

5. Left lower lobe collapse. This is easy to miss. The left lower lobe collapses down behind the heart. The left lung field appears much darker than normal and the heart shadow will appear much whiter than normal. If you look carefully you can see a white triangle behind the heart (1). On the lateral film you may see a white triangle at the bottom posterior corner of the lung fields (2) and the vertebral bodies will appear whiter.
4.2 Volume loss
A pneumonectomy is another cause of a white lung. You should know from the history and your examination that the patient has had a pneumonectomy. Look at the X-ray for the following features:
A very rare cause of a similar appearance is extensive hypoplasia or congenital absence of one lung.

This patient had right upper lobectomy and postoperative radiotherapy. Both of these have led to volume loss in the remaining right lung. The trachea has been pulled to the right as a result. The lung is of increased blackness on the right compared to the left because the remaining lung is hyperinflated.

Tracheal deviation can be the result of it being pushed by a mass lesion in the mediastinum, most often an enlarged thyroid gland, as in the case shown here. The lung volumes in this case are normal, and the ribs and diaphragms are in their normal positions. In the elderly a very tortuous aorta may also lead to tracheal shift.
4.3 Consolidation

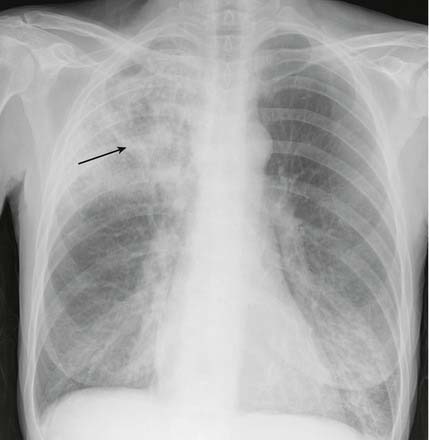
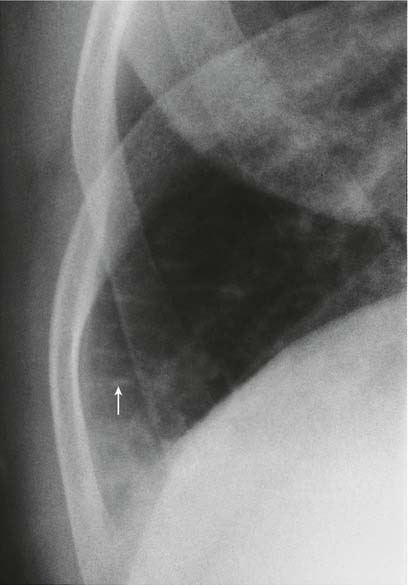
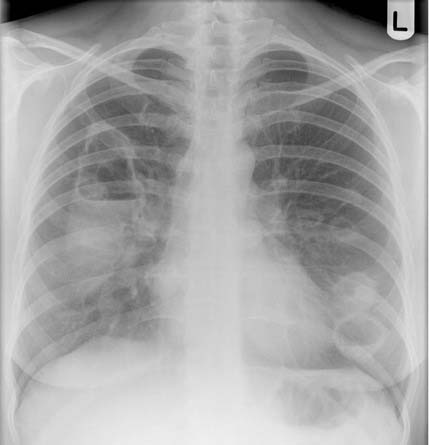
This is the appearance of a lobar pneumonia. Notice how the inferior margin of the consolidation is quite straight. This appearance indicates a right upper lobe pneumonia. An air bronchogram (arrow) is visible.


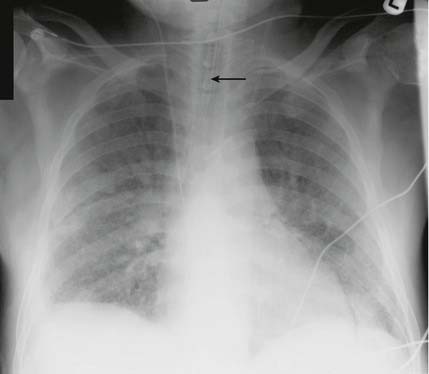
This shows much more widespread consolidation affecting both lungs, especially in the mid to lower zones, and is a bronchopneumonia. An air bronchogram (arrow) is again visible.
Again you can see an area of white lung. Look first at the nature of the whiteness and its border. If it is uniform with a well-demarcated border you are much more likely to be dealing with an area of collapse or a pleural effusion. If the shadowing is not uniform and the border is not so well demarcated the possibilities are consolidation, fibrosis or some other infiltrative condition. It can be difficult to diagnose consolidation so make your way carefully through the following steps:
If a patient is admitted with pneumonia it is not necessary to repeat the chest X-ray before discharge if they make a satisfactory recovery. For patients who fail to recover, further X-rays are necessary to look for possible complications such as the development of an empyema or pulmonary abscess. For patients ill enough to warrant admission to intensive care, early follow-up X-rays are warranted to ensure that their condition is not progressing.
4.4 Pneumocystis carinii (jiroveci) pneumonia (PCP)
Pneumocystis carinii pneumonia (PCP) can be difficult to diagnose on a chest X-ray and in 10% of patients with PCP the chest X-ray is normal. It is something to suspect if a patient presents with shortness of breath and hypoxia which are out of proportion to a relatively normal looking chest X-ray.
4.5 Pleural effusion

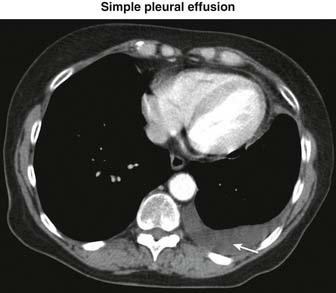
This pair of films shows the varied appearances of pleural effusions. The first film shows a small left effusion filling the costophrenic angle. It has a curved upper margin.
If you see an area of whiteness at the base of a lung then the possible causes are a pleural effusion, a raised hemidiaphragm and an area of consolidation or collapse. You need to determine which of these it is.
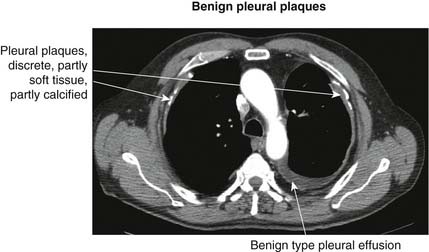
4.6 Asbestos plaques
Pleural plaques represent areas of pleural thickening caused by exposure to asbestos fibres. They may be predominantly soft tissue with small amounts of calcium or be heavily calcified. Isolated pleural thickening is a cause of a localized area of white lung and can be difficult to separate from lung shadows. If you suspect pleural plaques then:
4.7 Mesothelioma

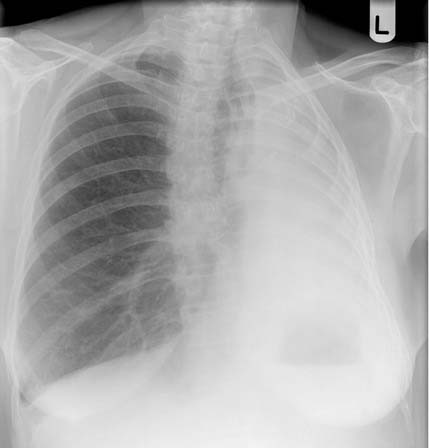
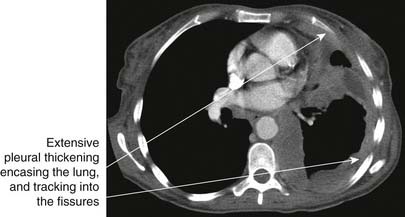
This is the chest X-ray of a 68-year-old man with a history of asbestos exposure. He presented with right lateral chest wall pains. The film demonstrates lobulated pleural thickening around the upper, mid and basal right lung, with further pleural thickening evident next to the right side of the mediastinum. CT of a mesothelioma in a different patient is shown on page 71.
Mesothelioma is a malignant tumour of the pleura. The shadowing it causes will have the characteristics of pleural shadowing and some of the characteristics of malignant shadows. If you suspect the whiteness to be mesothelioma then:
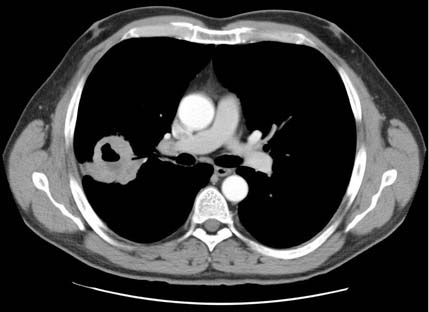
4.8 Pleural disease on a CT scan
If you see increased density around the inner chest wall:
4.9 Lung nodule
The term ‘lung nodule’ is used to describe a discrete area of whiteness situated within a lung field. It is less than 3 cm in diameter. It is not necessarily strictly circular. The main worry is that it may represent a carcinoma. Other possibilities are a localized area of consolidation, an abscess or a pleural abnormality. Go through the following steps in assessing the abnormality:
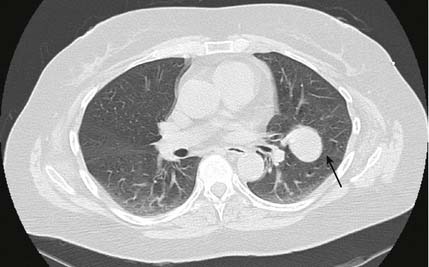
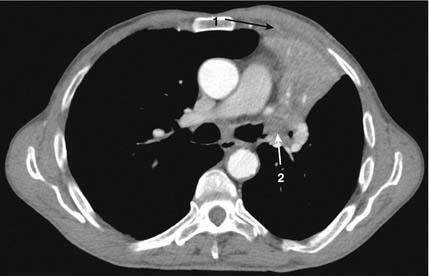
The arrow marks the location of the left oblique fissure. The coin lesion seen on the plain film lies on the oblique fissure and in front of it. The remainder of the CT scan showed no evidence of metastatic disease and no hilar or mediastinal lymph nodes were involved. The patient was referred for a PET scan and subsequently underwent a left upper lobectomy.
4.10 Cavitating lung lesion

These two films both demonstrate cavitating lung lesions. In the first study there are bilateral thin-walled cavities, some with air–fluid levels. This was due to Wegener’s granulomatosis.
Some coin lesions may cavitate, and if you have identified a coin lesion, it is important to look for the features of cavitation. Therefore:
If you diagnose a cavitating lesion:
4.11 Left ventricular failure (LVF)

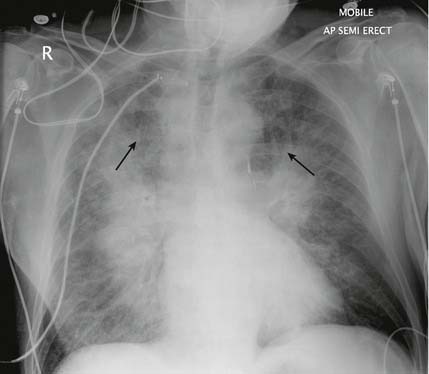
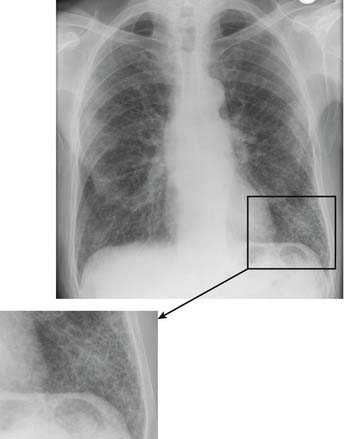
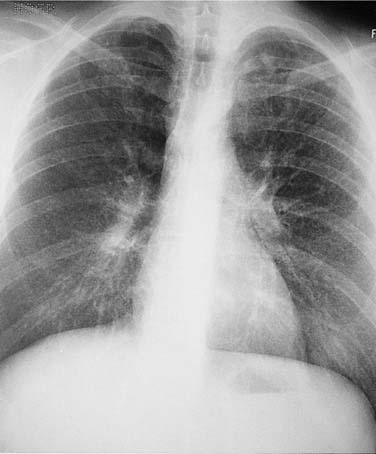
This patient presented with an acute cardiac event. At present the pleural spaces are clear but it is common in pulmonary oedema to develop pleural effusions. These are often larger on the right than on the left. Pulmonary upper zone blood vessels are also often dilated, as is shown in this film (arrows). This patient’s film clearly shows ‘bat’s wing’ hilar shadows characteristic of pulmonary oedema. The magnified image of the right lower zone (opposite) shows the horizontal septal lines more clearly (arrowed).
If you suspect heart failure as a cause of a generalized, or localized, area of shadowing then:
4.12 Acute respiratory distress syndrome
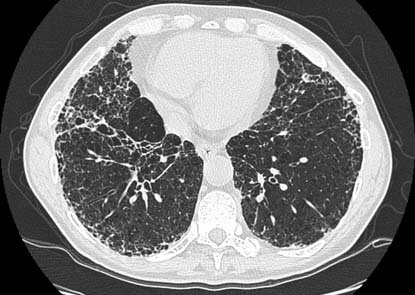
Acute respiratory distress syndrome (ARDS) is defined as respiratory failure in association with a chest X-ray that shows confluent alveolar opacification (whitening) of the lungs that looks like pulmonary oedema.
If you are certain that the chest X-ray suggests a diagnosis of ARDS then look for clues as to the cause. There are many causes of ARDS (see Box on p. 89) and most can only be picked up by history and examination. However, an asymmetrical distribution of the shadowing, i.e. significantly more shadowing in one lung than the other, may point to lung injury as a cause. Chest X-rays taken just before the development of ARDS may show an obvious pneumonia.
4.13 Bronchiectasis
Bronchiectasis can be difficult to diagnose on a plain chest X-ray. If you suspect it as a cause of increased shadowing then look for the following features:
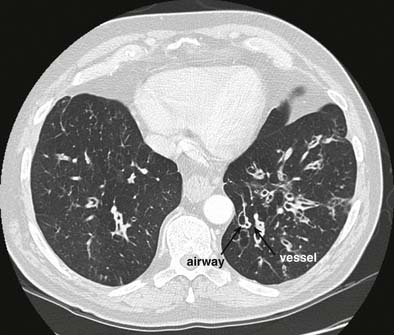
The HRCT scan and bronchiectasis
4.14 Fibrosis
Fibrosis is one of the rarer causes of white lung and you need to differentiate it from consolidation or oedema which is far more common. If you suspect fibrosis:
The HRCT scan and pulmonary fibrosis
You will be ordering the scan to give you details of any lung parenchymal changes. Therefore you will need to order a high-resolution scan so that you can see the fine detail of the lung architecture.
Confirming fibrosis
Determining aetiology
4.15 Chickenpox pneumonia
Chickenpox pneumonia in adulthood can cause the development of numerous calcified nodules. To determine whether this is a likely diagnosis:
4.16 Miliary shadowing
The lungs have a spotted appearance. This may be due to miliary shadowing. The normal lung can sometimes have a mottled appearance. This can be especially so in obese patients. To distinguish between miliary shadowing and normal lung: