Chapter 34 The uvulopalatal flap
1 INTRODUCTION
This book includes a number of chapters which describe a variety of palatal surgical procedures for sleep disordered breathing, including traditional uvulopalatopharyngoplasty (UPPP) techniques, Z-palatoplasty (ZPPP), transpalatal advancement pharyngoplasty, laser-assisted uvulopalatoplasy (LAUP), pillar implantation, etc. Most of these procedures can be divided into two mutually exclusive groups based upon several different criteria: by their action on the palate, the setting in which they are performed, and how the surgeon is reimbursed. First, these various procedures usually work by one of two different ways: by either shortening the soft palate or by stiffening it. They also differ in where they are performed: those that are more invasive and which are used for more significant obstructive sleep apnea (OSA) are generally done in the operating room under general anesthesia, and those that are less invasive and which are advocated for less severe forms of sleep disordered breathing (such as primary snoring) are done in the office under local anesthesia. Furthermore, the insurance industry makes a distinction between these two groups of procedures in regards to reimbursement: those done in the OR for OSA are generally reimbursed by insurance, while those done in the office for primary snoring and mild OSA are relegated to self-pay status.
2 THE PROCEDURE
The UPF procedure was first described by Powell et al.2 in 1996 as a UPPP variation for the operating room. A similar technique was described in 1993 by Bresalier and Brandes,3 referred to as the imbrication technique of UPPP in 1999. In 2000, I described the use of this technique in the office under local anesthetic,4 which was presented in more detail in 2003 by Neruntarat.5 The procedure can also be expanded under general anesthesia to include greater effects in the laterally, by including concurrent tonsillectomy with tonsillar pillar closure4,6 or by extending incisions superolaterally from the apices of the tonsillar fossas toward the third molar region;4 Li et al.7 call this modification an extended uvulopalatal flap. The principles of the UPF have been further extended by Friedman with the Z-palatoplasty,8 which is the subject of Chapter 33. The Z-palatoplasty is essentially a UPF procedure in which the uvula and distal soft palate are split in the midline. This creates two flaps which are advanced not only anteriorly but laterally to further augment the retropalatal airway in its lateral dimensions. Because of the versatility of the procedure, therefore, the UPF is a useful tool which should be part of the armamentarium of all surgeons who treat sleep disordered breathing.
3 TECHNIQUE
3.1 AWAKE, LOCAL ANESTHESIA, OFFICE PROCEDURE
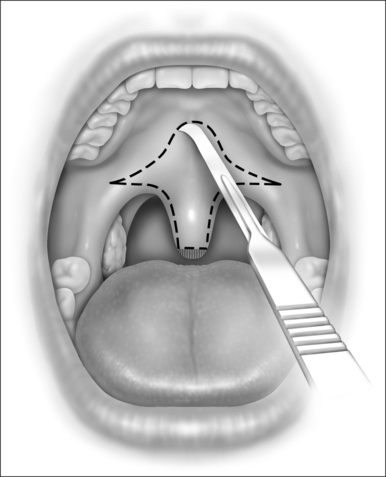
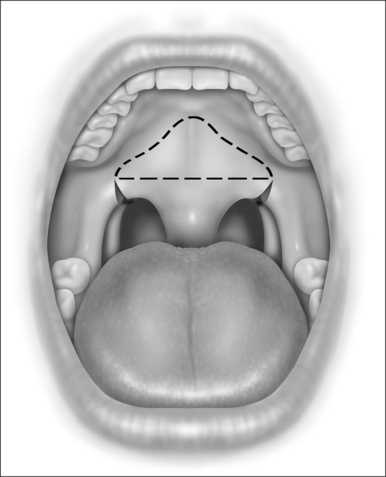
While still grasping the uvula in its new position, the planned incision is outlined with a marker or with a number 12 blade, as shown in Figure 34.1. This gothic arch-shaped incision generally has its apex within 5–10 mm of the hard–soft palate junction and flares laterally to allow for advancement of the lateral palate. The farther laterally these incisions extend, the greater the elevation of the lateral aspects of the palate. The incision will be carried caudally onto the uvula in a mirror image of the palatal incision. Unless vertical relaxing incisions are necessary, as described previously, it is recommended that the incisions be kept away from the free edge of the palate, to lessen the chance of scar contracture.
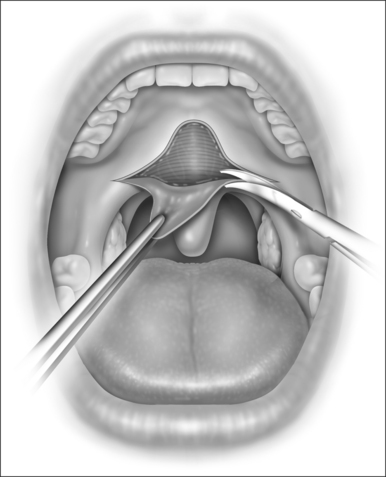
The dissection can be performed entirely with a scalpel and with scissors; Metzenbaum or long Iris scissors are adequate. Though the procedure could also be performed acceptably with a needle point cautery unit, the additional expense, tissue destruction, and postoperative pain do not warrant its use, particularly since electrocautery should rarely be necessary for hemostasis if local anesthetic injection and surgical dissection have been meticulous. It is easiest to begin with the scalpel at the apex of the palatal incision and extend inferolaterally on each side. The mucosa within this outlined area is then carefully removed with sharp pointed scissors, as shown in Figure 34.2. As the dissection reaches the tip of the uvula, the tip is usually amputated to reduce the length of tissue brought up to the palate.
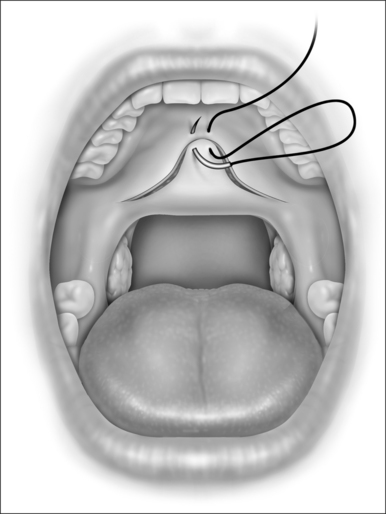
The initial suture is a mattress suture that first passes through the mucosa and underlying muscle at the apex of the palatal incision and then passes through the tip of the uvular muscle and adjacent mucosa from the nasopharyngeal side of the uvula. This is shown in Figure 34.3. Tension of this mattress suture can be adjusted to allow for proper positioning of the soft palate edge. Additional mucosa on the palate or flap may now be trimmed, if necessary. The closure is then completed in a two layered interrupted surgical technique. It is highly recommended that this closure be done in layers to minimize the chance of postoperative dehiscence.
Note that the advanced uvula and distal palate are a different color than the rest of the palate. This tissue, which originated on the nasopharyngeal surface of the palate, is brighter red than the oral palatal mucosa. This is explained to the patient preoperatively, as is the fact that the folded-over central palate may be somewhat thicker for some time postoperatively. This seems to thin out somewhat postoperatively, and should not require subsequent thinning or revision. Note that patients who have excessively thick and beefy palates may not be optimal candidates for this procedure, however.
3.2 GENERAL ANESTHESIA, WITH CONCURRENT TONSILLECTOMY
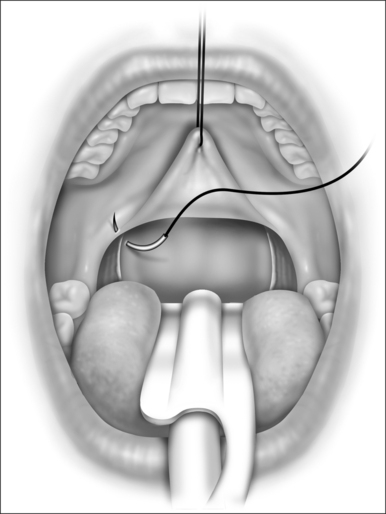
It is recommended that the tonsillectomy be performed first with care taken to spare as much tonsillar pillar mucosa as possible. Hemostasis is improved by injecting the tonsillar fossas with a total of 5–10 ml of the same local anesthetic with adrenalin as was used to inject the palate previously. This also helps with initial postoperative analgesia. The tonsillar pillar sutures are then placed before the palate is dissected, as illustrated in Figure 34.4. This closure is preferably performed in two layers to obliterate any dead space and to minimize the chance for postoperative dehiscence.
A stay suture held by a hemostat can be placed through the tip of the uvula to retract the distal palate cephalad during the tonsillar fossa closure to help align the tissues properly and aid in correct suture placement. This can also help in determining if relaxing incisions extending cephalad from the apices of the tonsillar fossas are necessary (Fig. 34.5), which would be performed next.
4 POSTOPERATIVE MANAGEMENT
When performed in the outpatient setting in the office, patients are sent home with prescriptions for an appropriate antibiotic for several days and a narcotic pain medication. If edema is thought to be problematic, a short course of steroids may be offered. Anxiolytics, sleep aids, or other sedating medications are not recommended in the immediate postoperative period. A regular diet is resumed as soon as the patient is comfortable. Residual sutures may be safely removed after 2 weeks.
6 SUMMARY
The original procedure as described by Powell et al.2 has been modified by extending incisions into the lateral distal soft palate4,7 to allow for augmented flap elevation laterally; when an incision is placed in the midline of the uvula to create two flaps (the Z-palatoplasty) as discussed by Friedman,8 the lateral dimensions of the oropharyngeal inlet at this level can be augmented even more. This latter modification is thought to provide significant benefit in many cases.
1. Huntley T. Uvulopalatal flap (UPF) vs. LAUP in the treatment of snoring. Presented at the AAO-HNS annual meeting, Washington, DC, 2000 (unpublished data).
2. Powell N, Riley R, Guilleminault C, et al. A reversible uvulopalatal flap for snoring and sleep apnea syndrome. Sleep. 1996;19:593-599.
3. Bresalier H, Brandes W. Uvulopalatopharyngoplasty: prevention of complications with the imbrication technique. Ear Nose Throat J. 1999;78:920-922.
4. Huntley T. The uvulopalatal flap. Op Tech Otolaryngol Head Neck Surg. 2000;11(1):30-35.
5. Neruntarat C. Uvulopalatal flap for snoring on an outpatient basis. Otolaryngol Head Neck Surg. 2003;129:353-359.
6. Hormann K, Erhardt T, Hirth K, et al. [Modified uvula flap in therapy of sleep-related breathing disorders]. HNO. 2001;49(5):361-366. (article in German).
7. Li H-Y, Li K, Chen N-H, et al. Modified uvulopalatopharyngoplasty: the extended uvulopalatal flap. Am J Otolaryngol. 2003;24(5):311-316.