Chapter 16. The unconscious patient
The unconscious patient is unable to ensure their own safety and in deeper levels of coma may be unable to protect their own airway.
Assessment of the unconscious patient
The first priority is to ensure safety before approaching the patient. Use the SAFE approach and evaluate the ABCs.
If there is any suspicion that the patient may have been a victim of trauma, the neck is immobilised in a rigid cervical collar while the airway is being assessed.
Give high-concentration oxygen, open the airway, check breathing and circulation status.
If there is no cardiac output, then immediately start CPR.
The next stage is to perform the rapid neurological checks – AVPU and assessment of pupillary responses.
DEFG: Don’t Ever Forget Glucose – a capillary glucose level (BM stix) MUST be checked in all unconscious patients.
Take a baseline set of observations and transfer the patient to hospital with monitoring on.
The assessment must be repeated regularly. A change in conscious level is the most important single sign in the assessment of the unconscious patient with a head injury.
AVPU
A – is the patient Alert?
V – is the patient responding to Verbal stimuli?
P – is the patient responding to Painful stimuli?
U – is the patient Unresponsive?
A response by speech or movement scores ‘V’. If there is no response, a painful stimulus is applied. The best stimulus to use is pressure over the supraorbital ridge, above one of the eyes: a response to this stimulus scores ‘P’, no response scores ‘U’.
Signs to look for in the unconscious patient
• Any sign of head injury (protect the C-spine)
• ‘Raccoon eyes’ (base of skull fracture)
• A bitten tongue and urinary incontinence (epileptic fit)
• Pyrexia and rash (meningococcal septicaemia)
• Pinpoint pupils, needle marks and slow, shallow respiration (signs of an opiate overdose. Give naloxone (Narcan) and assess response)
• Empty medication packaging (possible overdose)
• Medi-alert bracelet
• Insulin, needles, glucose monitor (diabetic patient).
Bilateral pinpoint pupils virtually always indicate opiate overdosage (although a brainstem stroke can produce the same appearance). Bilateral dilated pupils are less helpful because there are many potential causes.
A dilated pupil on one side may indicate an expanding intracranial haematoma on the same side.
Further neurological examination
Two other useful neurological checks can be performed: a more detailed assessment of the conscious level of the patient using the Glasgow Coma Scale, and a brief neurological examination to determine if the patient has any areas of localized weakness or paralysis (focal neurological deficit).
Glasgow Coma Scale
The Glasgow Coma Scale uses three areas of patient response to determine a score that indicates coma level: these are eye opening, speech and best motor response.
The highest score (the alert patient) is 15 and the lowest (in deep coma or dead) is 3.
‘Coma’ is defined as a GCS score of 8 or less.
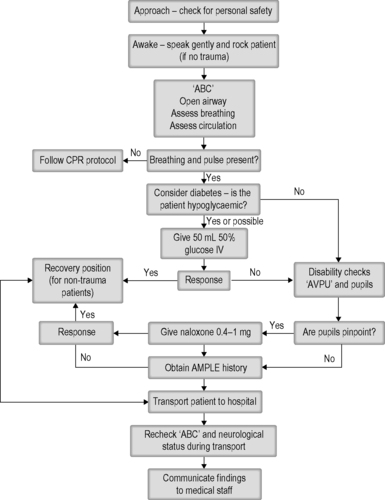 |
| Figure 16.1. |
| Management of the unconscious patient. |
| Component | Response | Score |
|---|---|---|
| Best motor response | Obeys commands | 6 |
| Localises to paina | 5 | |
| Withdraws from painb | 4 | |
| Flexor response to painc | 3 | |
| Extensor response to paind | 2 | |
| No motor response to pain | 1 | |
| Best verbal response (speech) | Oriented | 5 |
| Confused conversatione | 4 | |
| Inappropriate speechf | 3 | |
| Incomprehensible speechg | 2 | |
| No speech | 1 | |
| Eye opening | Spontaneous | 4 |
| In response to speech | 3 | |
| In response to pain | 2 | |
| No eye opening | 1 | |
| aMoves hand towards pain. |
||
| bMoves away from pain. |
||
| cBends arm at elbow and wrist in response to a painful stimulus. |
||
| dStraightens at elbow and knee in response to a painful stimulus. |
||
| eDisorientated in time, person and place. |
||
| fInappropriate response to question. |
||
| gMoans and groans. |
||
Focal neurological deficit
On close examination of the face, note should be made of a drooping of the smile on one side, indicating a facial paralysis, common in patients who have had a cerebrovascular accident (stroke).
After a painful stimulus, movement of the patient’s limbs should be observed and may reveal paralysis in one or more of the limbs. Weakness and paralysis are signs of focal neurological deficit and should be recorded and communicated to the receiving medical facility.
Common causes of altered conscious level
These may be remembered with the mnemonic CID CID F, see below.
CID CID F
C – Cerebral causes
I – Injury to the head
D – Diabetes and metabolic problems
C – Cardiac causes
I – Infection
D – Drugs, poisons and alcohol
F – Failure of organs and hypothermia
Cerebral causes
Common cerebral causes of unconsciousness are epilepsy, cerebrovascular accident (stroke) and subarachnoid haemorrhage.
Cerebrovascular accidents (CVAs) or strokes have two basic causes:
• Haemorrhagic stroke – from bleeding into the brain
• Cerebral infarction – a blood vessel becomes blocked.
If the features resolve completely over the space of several hours then the episode is known as a transient ischaemic attack (TIA).
Subarachnoid haemorrhage is usually caused by the sudden bursting of a small swelling (an aneurysm) of a cerebral vessel.
The characteristic history is of a patient who develops a sudden headache (often described as ‘like being hit on the back of the head with a hammer’) and who then collapses.
Epilepsy is a condition of abnormal brain activity, which presents with convulsions or ‘fits’.
The most common type of epilepsy is ‘grand mal’ epilepsy, which has the following phases:
1. The patient collapses and the whole body contracts – the tonic phase; this usually lasts for a period of up to 30 seconds
2. Then follows a period of generalised contractions and relaxations, the tonic–clonic phase (the ‘fit’), the duration of which can be very variable
3. The convulsion stops and consciousness slowly returns: this is the postictal phase. The patient may at first be confused before gradually returning to full awareness.
If the tonic–clonic phase continues for more than 15 minutes, the patient is said to be in status epilepticus which is a medical emergency.
The patient who is immediately alert after an episode of collapse is unlikely to have had a grand mal fit.
Management of the fitting patient
• Ensure that the patient comes to no further harm
• Do not attempt to put anything in the patient’s mouth
• Place an oxygen mask on or near the face of the patient
• If the convulsion shows no sign of ceasing give diazepam 10–20 mg IV or PR
• Transport the patient rapidly to the nearest available hospital with resuscitation facilities
• Ensure that the individual is protected from self-injury during the ambulance journey
• Check the patient’s blood glucose level to exclude hypoglycaemia as the underlying cause.
Head injury
The diagnosis of head injury should not be overlooked, particularly in the drunk or intoxicated patient. Signs of trauma such as a head wound or palpable depressed fracture may be present.
Signs that indicate a base of skull fracture are:
• Bruising around both eyes (‘raccoon eyes’)
• Bruising over the mastoid process (Battle’s sign, which usually takes a number of hours to develop)
• Blood or cerebrospinal fluid leaking from an ear.
Any episode of hypoxia or fall in blood pressure will significantly increase the head injured patient’s morbidity and mortality.
Diabetes and metabolic problems
A low blood glucose level is one of the most common causes of coma found in the community. It is seen most often in diabetic patients who have taken too much insulin in relation to their food intake and activity level.
Chronic alcoholics have very low sugar stores and may develop acute hypoglycaemia after a bout of drinking.
The features of hypoglycaemia develop rapidly, usually over a period of a few minutes. Give glucose urgently, orally if possible, IV if absolutely necessary.
High blood sugars cause unconsciousness less commonly.
Clinical presentation of diabetic emergencies
Hypoglycaemia
• Dizziness and light-headedness
• Sweating (may be profuse)
• Confusion
• Aggression
• Weakness and loss of coordination
• Coldness and clamminess
• Fitting.
Hyperglycaemia
• Slow onset
• Thirst
• Weight loss
• Passing large amounts of urine
• Dehydration (dry skin, sunken eyes)
• Smell of ketones (not every one can smell these)
• Deep sighing breathing (Kussmaul’s respiration).
Cardiac causes of unconsciousness
Cardiac arrhythmias
Major cardiac arrhythmias such as ventricular fibrillation result in collapse and should be treated using the cardiac arrest protocols.
Non-arrest arrhythmias may only cause transitory upset in cardiac output and result in a brief loss of consciousness.
A Stokes–Adams attack is when a patient (who is usually elderly) has a short run of a haemodynamically compromising arrhythmia. Patients have no warning symptoms of the collapse and recover quickly.
The patient should be transported to hospital with ECG monitoring.
Simple faint
Clinical features
• Sudden transient loss of consciousness.
Precipitating causes
• Emotional triggers include fright, sexual desire and the sight of blood
• Physical triggers such as pain
• Drugs (such as glyceryl trinitrate)
• Standing up too quickly or for prolonged periods (especially in hot weather)
• Anaemia (rarely).
Management
• The patient should be laid flat with the feet raised or in a head-down position
• If rapid recovery does not occur, consider an alternative diagnosis
• When the patient awakens, they should be asked about any possible precipitating causes of the faint
• If the patient does not fully recover or is unsafe at home, transfer to the ED.
Infection
Infection is a rare but serious cause of collapse. It is most commonly encountered in the young child or adolescent who develops meningococcal septicaemia.
These children or young people should be administered benzyl penicillin without delay and transported to hospital as rapidly as possible.
Other infections of the brain such as encephalitis and cerebral abscess can also cause collapse.
Overwhelming septicaemia, whatever the organism, may cause unconsciousness.
The diagnosis should be considered in an unconscious patient who is tachycardic with a low blood pressure and no signs of blood loss.
Intravenous fluids should be started and the patient transferred to hospital as soon as possible.
Drugs, poisons and alcohol
Alcohol
A drunk patient is not necessarily unconscious because of the alcohol; the cause may be a head injury, hypoglycaemia or an overdose.
Hypoglycaemia may be present and should be treated with intravenous glucose.
It is important to be wary of leaving an apparently drunk patient in police custody when other possible causes of decreased consciousness have not been excluded.
When a drunk patient is unconscious THINK:
• HEAD INJURY, HYPOGLYCAEMIA
Only then THINK:
• ALCOHOL
as the cause of the loss of consciousness.
Opiate poisoning
The features of opiate overdose are pinpoint pupils, respiratory depression and coma.
Assist respiration as necessary and consider using the opiate antagonist naloxone (Narcan).
Naloxone is given intravenously in a dose of 0.4–10 mg. Response to the drug is rapid, with wakening within 1 min, but the drug is short-acting, with a half-life of about 40 minutes.
If IV access is not possible, naloxone can be given intramuscularly (IM).
Other drugs that can cause coma
The next most common group of drugs causing coma is the antidepressants, particularly tricyclic antidepressants such as amitriptyline and mianserin.
Signs that may indicate tricyclic overdose include:
• Dilated pupils
• Convulsions
• Respiratory depression
• Cardiac arrhythmias.
The patient’s cardiac rhythm must be monitored during transport to hospital.
Diazepam, temazepam and nitrazepam can cause drowsiness and coma when taken in overdose.
Carbon monoxide poisoning from faulty gas fires or attempted suicide from car exhaust fumes can cause coma. Be aware that carbon monoxide is odourless and invisible and may pose a threat to rescuers.
Drugs commonly causing coma:
• Alcohol
• Opiates
• Tricyclic antidepressants
• Benzodiazepines
• Carbon monoxide.
Hypothermia
A core body temperature of less than 35°C can be a cause of or a result of coma. The diagnosis should be suspected in the collapsed elderly patient or in anyone who has been exposed to the environment (such as the entrapped trauma victim).
For further information, see Ch. 16 in Emergency Care: A Textbook for Paramedics.



