Chapter 9. The thoracic spine
CHAPTER CONTENTS
Summary225
SUMMARY
This chapter sets out to explain the anatomy of the thoracic spine and highlights the somatic structures which are a common cause of pain. Pain patterns are discussed and the non-mechanical causes of thoracic back pain are presented to aid diagnosis and appropriate management.
The clinical examination procedure is outlined and interpreted, the contraindications are emphasized and the treatments used in orthopaedic medicine are described, with notes on the indications for their use.
ANATOMY
There are 12 thoracic vertebrae which gradually increase in size from above down, marking a transition between cervical and lumbar vertebrae. A typical thoracic vertebra is easily recognized by its costal facets, its heart-shaped superior surface and waisted vertebral body (Fig. 9.1). The vertebral canal in the thoracic region is round and smaller than that found in either the cervical or lumbar spine. Short pedicles pass almost directly backwards and thick, broad laminae overlap each other from above down.
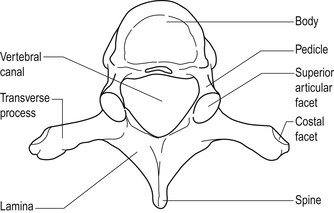 |
| Figure 9.1
Typical thoracic vertebra.
From Anatomy and Human Movement by Palastanga N, Field D and Soames R. Reprinted by permission of Elsevier Ltd.
|
The slope of the long spinous processes gradually increases downwards with the 5th to 8th spinous processes overlapping each other. The 8th spinous process is the longest, while the 12th is shorter, horizontal and similar to the lumbar spinous processes.
Long, rounded, club-like transverse processes are directed posterolaterally and slightly superiorly. Except for the 11th and 12th vertebrae, oval, anterior facets lie at the tips of all transverse processes. These facets articulate with the tubercles of the corresponding ribs.
Flat articular processes project superiorly and inferiorly to form the thoracic zygapophyseal joints. Their direction facilitates the movement of rotation, which is coupled with side flexion, while also permitting a range of flexion and extension. Rotation is a particular feature of the thoracic spine and is facilitated by the direction of the articular facets and rotation of the fibres in the intervertebral discs. The shearing movement common to lumbar discs does not occur so readily in the thoracic spine (Kapandji 1974). The 12th thoracic vertebra is a transitional vertebra with the upper surface being typical of a thoracic vertebra but the lower surface having lumbar characteristics for articulation with L1. A dramatic change of direction of the plane of the zygapophyseal joints occurs over one level at the thoracolumbar junction permitting rotational stresses between T11 and T12 which are disallowed between T12 and L1. This makes the 12th thoracic vertebra susceptible to fracture (Agur & Dalley 2009).
The thoracic intervertebral joints consist of the vertebral body above and below and the intervertebral disc. These joints are supported by anterior and posterior longitudinal ligaments, supraspinous, interspinous and intertransverse ligaments and the ligamentum flavum that connects adjacent laminae internally. Further support is gained by the costovertebral joints and ligaments which directly involve the intervertebral disc.
Nakayama et al (1990), Maiman & Pintar (1992), Oppenheim et al (1993), Bogduk & Valencia (1994) and Boriani et al (1994) all share the opinion that disc lesions are relatively uncommon in the thoracic spine, in contrast to the claim that disc lesions account for a higher proportion of thoracic pain than is often realized (Cyriax & Cyriax 1993, Mellion & Ladeira 2001). The bony anatomy, including the primary kyphotic curve, and the surrounding ligamentous structures related to the costovertebral joints may have a stabilizing effect on the intervertebral disc, making displacement less likely in this region. The rib cage also exerts a stabilizing effect by restricting movement, particularly in the upper segment where the ribs are firmly attached anteriorly and posteriorly.
Movement in the thoracic spine is limited. This is due in part to the thoracic disc height relative to vertebral body height being less than in the cervical or lumbar spines with the ratio of disc diameter to height 2–3 times greater than in the lumbar spine. The acute angle of orientation of the annular fibres and the relatively small nucleus in the thoracic spine contribute to this lack of mobility. The angle of the zygapophyseal joints in the thoracic spine facilitates rotation while limiting flexion and anterior translation and having little influence on side flexion (Edmondston & Singer 1997). Little has been written about the structure and function of the thoracic disc, so it is not covered in depth here.
Twelve pairs of ribs normally attach posteriorly to the thoracic spine. The upper seven pairs are termed true ribs and attach anteriorly to the sternum. The lower five pairs consist of false and floating ribs, the false ribs attaching to the costal cartilage above.
A typical rib consists of a shaft and anterior and posterior ends. It is the posterior end that concerns us here. The posterior end of the rib typically has a head, neck and tubercle and articulates with the thoracic vertebrae, forming the posterior rib joints. The head of the rib is divided into two demifacets by a horizontal ridge that is attached to the disc via an intra-articular ligament. The lower facet articulates with its corresponding vertebra; the upper facet articulates with the vertebra above.
The tubercle of the rib is at the junction of the neck with the shaft and articulates with the transverse process of the corresponding vertebra. Just lateral to the tubercle the rib turns to run inferiorly forwards; this point is the angle of the rib.
A cervical rib may be present as an extension of the costal elements of the seventh cervical vertebra. It generally passes forwards and laterally into the posterior triangle of the neck where it is crossed by the lower trunk of the brachial plexus and the subclavian vessels. Compression of these structures may produce motor and sensory signs and symptoms.
Posterior rib joints
Two joints, the costovertebral and costotransverse joints, attach the rib firmly to the vertebral column (Fig. 9.2). These assist stabilization of the intervertebral joint while being relatively unstable themselves. Minor subluxations of these joints may be responsible for the mechanical pattern of signs and symptoms associated with a thoracic pain. This minor instability may also account for the ease with which subluxations occur and can be reduced in this region.
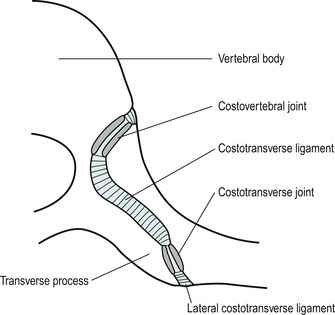 |
| Figure 9.2
Posterior rib joints. Costovertebral and costotransverse joints, horizontal section.
From Anatomy and Human Movement by Palastanga N, Field D and Soames R. Reprinted by permission of Elsevier Ltd.
|
The costovertebral joint is a synovial joint formed between the head of the rib and two adjacent vertebral bodies, except at the first, 11th and 12th ribs, where a joint is formed with a single vertebral body. The joint surfaces are covered by articular cartilage and surrounded by a fibrous capsule. The capsule is thickened anteriorly by the radiate ligament while the posterior aspect of the capsule blends with the nearby denticulation of the posterior longitudinal ligament. An intra-articular ligament divides the joint and attaches the transverse ridge of the rib head to the intervertebral disc.
The costotransverse joint joins the upper 10 ribs to the transverse processes of their corresponding vertebra. The joint is surrounded by a fibrous capsule that is reinforced posteriorly by the lateral costotransverse ligament. The joint is further stabilized by the costotransverse ligament which joins the transverse process to the neck of the rib, and the superior costotransverse ligament which connects the rib to the transverse process of the vertebra above. Movements occur concurrently at the costovertebral and costotransverse joints and are determined by the shape and direction of the articular facets. This amounts to small rotary and gliding movements in association with the ‘bucket handle’ action of the ribs during respiration.
Three thin musculotendinous layers occupy the intercostal space between adjacent ribs and may become symptomatic due to strain (Fig. 9.3). The external intercostal muscle is the most superficial, with fibres running in an oblique direction downwards and forwards. The internal intercostal muscle lies beneath with fibres running in the opposite direction, and the thinnest and deepest layer is formed by the innermost (intimi) intercostal muscle, which is thin and possibly absent, with fibres running in the same direction as the internal intercostal muscle.
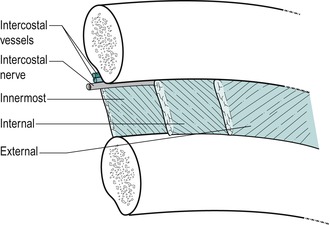 |
| Figure 9.3
Layers of intercostal muscles.
From Anatomy and Human Movement by Palastanga N, Field D and Soames R. Reprinted by permission of Elsevier Ltd.
|
Differential diagnosis at the thoracic spine
Orthopaedic medicine treatment techniques for the thoracic spine are aimed at reducing a mechanical lesion, i.e. subluxation of a posterior rib joint or herniations of the intervertebral disc.
Minor subluxation of the posterior rib joints
Subluxation of one or other of the posterior rib joints is a common cause of thoracic pain. The articulating surfaces of these joints are relatively shallow and unstable, rendering them susceptible to minor subluxations. The relatively trivial incidents that provoke thoracic mechanical pain and the relative ease with which it is reduced leads us to this hypothesis. Differential diagnosis of thoracic pain is difficult because of the numerous conditions that refer pain to the area and the lesions that mimic mechanical pain.
Patients present with a sudden onset of pain; the precipitating event is usually trivial and they often feel a pop or click. More gradual onset can be associated with working in rotated postures. The pain presents a typical mechanical picture of pain aggravated by movement and posture and eased by rest. In common with a thoracic disc lesion, a deep breath often provokes the pain, presumably because the ‘bucket handle’ action of the ribs during respiration translates aggravating movements to the rib joints at the spine.
On examination there is a non-capsular pattern of limited movement involving one rotation more than the other and these simple mechanical lesions usually respond rapidly to manipulation. Provided that there are no contraindications present (see below), the manipulative techniques described in this chapter can be applied. The usual postural and management advice should also be given to prevent recurrence, which is also a typical feature.
Thoracic disc lesions
It is important to reduce a thoracic disc displacement because of the potential for the displaced fragment to compromise the spinal cord. The thoracic vertebral canal is relatively small; therefore central prolapse poses the most threat.
In a review of the literature, Oppenheim et al (1993) reported an estimated annual incidence of one case of thoracic disc herniation per 1 million population. However, Mellion & Ladeira (2001) present a more current review of the literature which suggests that thoracic disc herniations are more common than previously thought and that in many cases these may be asymptomatic. It is primarily a condition of middle age, occurring between the third and fifth decade, and affects the lower thoracic levels more frequently. This is probably because the lower thoracic spine is free of the restriction of the rib cage, making it more mobile, and the transition to the non-rotational lumbar spine produces greater torsional stresses here. The most common level reported was T11, 12, and 75% of thoracic disc lesions occurred below T8.
Positive diagnosis of a thoracic disc lesion is difficult. There is no regular pattern to the history, signs and symptoms, as found at the cervical and lumbar spine, and it is not possible to produce a clinical model on which to base differential diagnosis. Wilke et al (2000) reported a case of shoulder pain associated with a lower thoracic disc herniation.
Central disc prolapse is most likely to compress the spinal cord and produce signs of myelopathy which include progressive paraparesis, increased reflexes, decreased sensation and bladder dysfunction. Although thoracic disc herniations are rare, Ozturk et al (2006) highlight the potential danger of their being missed as they could possibly result in the progressive myelopathy and paralysis mentioned above. A posterolateral prolapse produces segmental signs and symptoms.
To support the possible confusion arising from thoracic referred pain, Ozturk et al (2006) presented a case study of a patient with left flank pain, compatible with urinary system disorder. The cause of the pain could not be identified until magnetic resonance imaging (MRI) revealed a left T10–T11 lateral disc herniation with associated nerve root compression. They warn that thoracic disc herniation should be considered in the differential diagnosis of patients with pain more likely to be associated with visceral disorders, especially if basic diagnostic studies do not reveal the cause.
A further example is provided by Whitcomb et al (1995) who describe a patient with a 7-year history of severe disabling chronic epigastric abdominal pain attributed to chronic pancreatitis for which a 95% pancreatectomy was performed for pain control. Previous attempts to identify and treat the pain led to extensive radiographic, pharmacological, endoscopic and surgical interventions. Pain control was poor despite implantation of a continuous intrathecal morphine infusion pump. A focused physical examination eventually raised the suspicion of thoracic disc disease, which was confirmed with computed tomography. Disruption of the T7–T8 disc with protrusion into the vertebral canal and displacement of the spinal cord was identified. A microsurgicaI thoracic discectomy was performed and immediately the pain began resolving with the patient being pain-free and off all medication within several weeks.
In a review of the literature, Mellion & Ladeira (2001) highlight degenerative change, traumatic incidents, lifting, rotation, falls, exercise, rugby tackles and road traffic accidents as precipitating factors for thoracic disc lesions. The onset may be sudden and severe or insidious and slowly progressive. Mellion & Ladeira mention that Cyriax was the first author to describe the clinical presentation of a thoracic disc lesion. They suggest it may give four classical presentations: intermittent thoracic back pain which may be aggravated by sitting and relieved by standing; acute thoracic ‘lumbago’ with the thoracic spine fixed in flexion following a bending or twisting motion; thoracic root pain and paraesthesia; and symptoms of spinal cord compression. Chest pain may be constant or intermittent and may be central, localized or diffuse. A band-like dermatomal chest pain is not uncommon and abdominal referral may occur. If accompanied by cord compression, complaints of bladder involvement, lower limb paraesthesia and gait disturbance can be reported and findings may include spastic muscle weakness, hyperreflexia and a positive Babinski sign.
Mellion & Ladeira (2001) suggest that upper thoracic disc lesions are less common. Radiculopathies involving T1 share similarities with those occurring at C8, with numbness and weakness in the hand and pain in the arm and medial forearm. Weakness of the intrinsic hand muscles may be involved with T1, but this is an uncommon finding and the clinician must exclude non-mechanical causes such as Pancoast’s tumour. Horner’s syndrome (miosis and ptosis of the eye) is associated with T1 involvement but not C8. Presence of Horner’s syndrome is therefore contraindicated in manipulation or mobilization of the thoracic joints until the cause of the symptoms has been determined.
Disc lesions at the T2 and 3 levels are even less common and there are few reports in the literature of the features of involvement of T3–T8; symptoms of nerve root involvement at these levels may produce intercostal neuralgia. If there is involvement of the dura mater or dural nerve root sleeve, their mobility will be impaired and signs provoked on flexion of the cervical spine and scapular approximation. T9–T11 may produce a dermatomal pattern of pain and can include the abdomen and groin, often being confused with visceral symptoms. These lower levels may also mimic lumbar presentations including low back and leg pain.
In summary, small uncomplicated thoracic disc lesions may present with sudden or gradual onset of pain that may be felt posteriorly, anteriorly or radiating laterally. Pressure on the dura mater produces multisegmental reference of pain. The pain should have a typical mechanical behaviour, i.e. aggravated by movement and posture and eased by rest. Dural symptoms of increased pain on a cough, sneeze or deep breath may be present.
On examination, a non-capsular pattern of limited movement will be found, with one rotation being significantly more painful or limited than the other. Dural signs of pain on neck flexion and/or scapular approximation may be present if the dura mater is compromised. If there are no neurological signs and signs of cord compression are absent, the treatment techniques described in this chapter may be used. Alternatively, since lower thoracic displacements are more common, they may be treated using the techniques described for the lumbar spine.
Urgent surgical intervention is necessary for patients showing signs of spinal cord compression. Otherwise, uncomplicated thoracic disc lesions follow a path of recovery similar to that seen in cervical and lumbar disc lesions, responding to physical treatments and eventually stabilizing with time (Brown et al 1992).
Other causes of thoracic pain and associated signs and symptoms
Cervical disc lesions commonly refer pain into the thoracic region and this is particularly indicative of dural reference producing unilateral or bilateral scapular pain. The patient has a typical mechanical picture, with cervical movements increasing the pain felt in the thoracic region. Pain is not reproduced by thoracic movements. Minor chest wall pain may frequently be recognized as referred from the cervical spine, and Yeung & Hagen (1993) reported two cases of herniated C6–C7 disc producing major neuropathic chest wall pain which were treated surgically.
Subluxations of the posterior rib joints are a common cause of thoracic pain. They tend to present with unilateral central pain and tenderness and a non-capsular pattern of pain and limitation of movement. They respond quickly to the manipulative techniques described below.
Arthritis presents with the capsular pattern of limited movement.
• Equal limitation of rotations.
• Equal limitation of side flexions.
• Some limitation of extension.
• Usually full flexion.
• Degenerative osteoarthrosis can affect the spinal joints, causing secondary signs and symptoms. Gross degenerative changes may produce central osteophytes that may cause gradual cord compression. Anterior and lateral lipping of the vertebral body, as well as wedging of mid-thoracic vertebrae, has been associated with degenerative osteoarthrosis of the thoracic spine (Osman et al 1994).
• Inflammatory arthritis can involve the thoracic spine. Rheumatoid arthritis commonly affects the costovertebral, costotransverse and zygapophyseal joints. Reiter’s disease can affect the spinal joints, although it is more frequently seen in the lower limb joints. Ankylosing spondylitis, when it involves the thoracic cage, causes a reduction in chest expansion. Thoracic pain and stiffness may be its presenting symptoms.
Serious non-mechanical conditions can affect the thoracic area and suspicions are alerted when the patient appears unwell, has a fever, night pain with or without night sweats, or reports an unexpected weight loss. The pain is not affected by movement or postures and is often unrelenting.
• Malignant disease, both primary and secondary, may be a cause of pain in the thoracic spine. Bronchial carcinoma accounts for 95% of all primary tumours of the lung and may present with a cough and chest pain (Kumar & Clark 2002). Tumours in the bronchus, breast, kidney, prostate and thyroid commonly metastasize to bone. Intradural and extradural neoplasm, although relatively rare, may produce symptoms similar to nerve root irritation. Watanabe et al (1992) reported a case of benign osteoblastoma in the sixth thoracic vertebra presenting with thoracodorsal pain in a 19-year-old woman, increased by coughing and shifting sleeping positions. Hodges et al (1994) reported a case of intraspinal, extradural synovial cyst at the level of T4–T5 in a 51-year-old woman experiencing intermittent mid-thoracic and lumbar pain after lifting.
• Spinal infections may include osteomyelitis or epidural abscess. The organism responsible may be Staphylococcus aureus, Mycobacterium tuberculosis or, rarely, Brucella (Kumar & Clark 2002).
Bone conditions can include acquired conditions or congenital abnormalities. These conditions may be asymptomatic and a chance finding on X-ray.
• Scheuermann’s disease is vertebral osteochondritis, most commonly seen in males aged 12–18 years. It usually involves the lower thoracic vertebrae, often T9. The disc may move forwards between the cartilage end-plate and the anterior longitudinal ligament, producing wedging. It may produce minor thoracic backache and a local dorsal kyphosis may be evident on spinal flexion (Corrigan & Maitland 1989). Scheuermann’s disease has been associated with Schmorl’s nodes and degenerative lumbar disc disease in relatively young patients (Heithoff et al 1994).
• Schmorl’s nodes are protrusions of the intervertebral disc into the cancellous bone of the vertebral body. This may produce an anterior prolapse, causing separation of a small fragment of bone, seen on X-ray as a limbus vertebra (Taylor & Twomey 1985).
• Osteoporosis is a reduction in bone mass that may present a problem in postmenopausal women, who lose bone density faster than men. It is common in the sixth and seventh decades of life. Pain is not due to the condition itself, but usually to secondary wedge compression fractures of the vertebral body (Turner 1991). The patient presents with moderate to severe episodes of thoracic back pain that gradually resolve over the course of approximately 6 weeks. Fracture produces wedging of the vertebral body on X-ray and a characteristic increase in thoracic kyphosis is seen.
Fracture may present with a history of trauma. The fracture may involve elements of the vertebra or the ribs. The position of the pain and local tenderness will give an indication to the site of possible fracture.
Visceral disease can produce local thoracic pain or pain referred to the thoracic region that mimics mechanical pain, making diagnosis difficult. In visceral conditions the patient is usually unwell, which will aid diagnosis, but this is not always so.
• Angina is usually felt in the chest and can be referred into the arms. If mild, it may mimic mechanical pain. The patient experiences increased pain with exertion, e.g. climbing stairs, which may also be felt in the back.
• Pulmonary embolism, pleurisy, pneumothorax, etc. all present with chest pain, but other distinguishing features will hopefully lead to diagnosis, which is often difficult.
• Acute pancreatitis produces abdominal pain localized to the epigastrium or upper abdomen, but pain may be referred to the mid or low thoracic region.
• Acute cholecystitis can cause pain in the epigastrium and right hypochondrium, but pain may also be referred to the back and shoulder.
• The testes may refer pain to the lower thoracic area as they are supplied by nerves derived from the 10th and 11th thoracic spinal segments.
Shingles (herpes zoster) is related to a chickenpox virus infection affecting one posterior nerve root. The patient presents with a dermatomal reference of pain that may be present for some days before the typical rash appears. The rash consists of vesicles following a segmental course related to the affected nerve root. Shingles can be recurrent and may provide a persistent cycle of thoracic pain.
Soft tissue conditions can produce thoracic pain.
• Muscle lesions are relatively common in the thoracic region, therefore resisted tests are included in the routine examination. Commonly the intercostal muscles are affected, particularly if there is a history of a fractured rib. Palpation determines the site of the lesion.
• Tietze’s syndrome is a condition affecting the costochondral or chondrosternal joints. It is usually unilateral, affecting one, two or three joints that are tender to palpation. The cause is not known, but the condition may follow a respiratory condition that involves prolonged coughing. The condition is self-limiting and may be treated with physiotherapeutic pain-relieving modalities, non-steroidal anti-inflammatory drugs or injection of corticosteroid and local anaesthetic (Kumar & Clark 2002).
• Epidemic myalgia (Bornholm’s disease) is due to infection by the Coxsackie B virus. The features are an upper respiratory tract illness and fever followed by pleuritic and abdominal pain and muscular tenderness. It may occur in young adults in the late summer and autumn, but resolves spontaneously within a week (Kumar & Clark 2002).
COMMENTARY ON THE EXAMINATION
Observation
A general observation of the patient is made, assessing the face, posture and gait. Serious pathology should show in the face with the patient appearing tired and drawn. An assessment of the gait is important; the presentation of a disc lesion at the thoracic spine may present a serious threat to the spinal cord and signs of myelopathy may show in the gait pattern, which if severe will be spastic in nature.
See the Box on p. 231 listing ‘red flags’ for the possible presence of serious pathology that should be listened for and identified throughout the subjective and objective examination. In isolation, many of the flags may have limited significance but it is for the clinician to consider the general profile of the patient and to decide whether contraindications to treatment exist and/or whether onward referral is indicated.
History (subjective examination)
The age, occupation, sports, hobbies and lifestyle of the patient will indicate possible lesions and any contributing factors to the condition that may need to be addressed to prevent recurrence. Mechanical lesions tend to be found in the middle-aged group. Osteoporosis can affect postmenopausal women. Serious conditions may present in both the very young and the elderly, and caution is required if these particular age groups present with symptoms mimicking a mechanical lesion. Habitual postures may have relevance to the symptoms, as will the patient’s sports or hobbies.
The site and spread of symptoms may indicate the site of the lesion. The initial site of the symptoms may be different to the current situation and it may be helpful to know this. Mechanical lesions can produce central pain, anterior pain or both. Pain may radiate around the chest wall and this may be indicative of nerve root involvement. Progressively increasing and radiating pain is usually sinister. Symptoms may spread in a multisegmental distribution, indicating dural involvement, or separate satellite areas of pain may be related to visceral causes. Cardiac pain characteristically radiates from the chest into one or both arms. Mechanical lesions of the posterior rib joints produce relatively local pain, but movement may provoke sharp, shooting or twinging pain.
The nature of the onset and duration of the symptoms will assist differentiation of mechanical lesions from more serious pathology. Minor subluxation of the posterior rib joints usually has a sudden onset, with the patient recalling the exact time of onset. The mode of onset is usually trivial and is often associated with a popping or cracking sound. The duration is generally short; patients seek help as they realize the mechanical nature of the problem, having ‘felt it go’. Minor subluxation may present gradually following the adoption of an awkward posture for some time. A disc lesion may have a gradual or sudden onset. A history of trauma may indicate possible fracture. More serious pathology generally starts insidiously for no apparent reason and the duration of the symptoms may be many weeks or months. Recurrent episodes may be indicative of mechanical instability or inflammatory arthritis.
The behaviour of the pain is important since mechanical lesions produce a recognizable pattern of behaviour. The pain is better for rest and worse for activity. Providing the mechanical lesion does not wake the patient on turning, night pain is not a feature and the patient is usually well rested. The provoking activities are consistent and every time the patient repeats a particular aggravating movement, the pain is produced.
The 24 h pain pattern gives an indication of severity and irritability of the condition. Inflammatory symptoms are worse at night, but if the patient does get to sleep there is stiffness on waking which may take some time to wear off. This would be generally indicative of inflammatory arthritis. If night pain is a feature, the patient will look tired and this generally indicates serious pathology.
Other symptoms may indicate a mechanical lesion, be it either a minor posterior rib joint subluxation or a minor disc lesion. A deep breath may aggravate the pain, and needs to be distinguished from such conditions as pleurisy and pulmonary embolism, for example. These conditions may also produce pain on a deep breath, but the subsequent findings on the objective assessment will confirm whether the lesion is mechanical. Although movements are small at the posterior rib joints, the length of the ribs produces a greater proportion of movement at the anterior ends. This movement may also be painful in an intercostal muscle strain. A cough or sneeze increasing the pain could be indicative of minor subluxation or, more commonly, dural irritation, and symptoms are generally increased with activity and relieved by rest.
As the vertebral canal in the thoracic spine is small, disc displacement can threaten the spinal cord and produce symptoms of myelopathy; these must be ruled out. The patient is asked about the presence of paraesthesia in the feet, weakness in the legs and difficulty in walking. A specific question must be asked about bladder and bowel function, to rule out myelopathy (Oppenheim et al 1993). If any impairment is noted, the patient should be referred for neurosurgical opinion.
Other joint involvement may give an indication of any polyarthritic condition.
Past medical history will give information concerning conditions that may be relevant to the patient’s current complaint or reveal possible alternative diagnoses and contraindications to treatment. An indication of the patient’s general health will indicate any systemic illness. It may be pertinent to take the patient’s temperature. The patient should be asked about any recent unexplained weight loss. As well as past medical history, establish any ongoing conditions and treatment. Explore other previous or current musculoskeletal problems with previous episodes of the current complaint, any treatment given and the outcome of treatment.
On considering medications, the patient should be specifically asked about anticoagulants, long-term oral steroids, antidepressant medication and the current intake of analgesics, as an objective measure of pain control requirement.
• Young: Under 20
• Elderly: First episode over 55
• Recent trauma
• Past medical history of malignancy
• Constant progressive pain
• Unremitting night pain
• Systemically unwell
• Unexplained weight loss
• Drug abuse and HIV
• Long-term systemic steroid use
• Upper motor neuron signs and symptoms
• T1 weakness
• Horner’s syndrome
• Inflammatory arthritis
• Visceral pathology
• Osteopenic/osteoporotic
Inspection
The patient should undress to underwear and an inspection carried out in a good light. A general inspection of the posture is made assessing bony deformity. Note the position of the head and neck, cervical, thoracic and lumbar curves. Is there any evidence of cervical protraction or dowager’s hump, excessive or local thoracic kyphosis? Note the position of the scapulae and any evidence of scoliosis.
Colour changes or swelling would not be expected unless associated with a history of recent trauma. The typical appearance of shingles may be seen or the mottled reddening (erythema ab igne) produced following prolonged application of excessive heat, giving an indication of the severity of the pain.
Muscle wasting may be seen in the scapular area associated with neuritis.
State at rest
Before any movements are performed, the state at rest is established to provide a baseline for comparison.
Examination by selective tension (objective examination)
The suggested sequence for the objective examination will now be given, followed by a commentary including the reasoning in performing the movements and the significance of the possible findings.
Eliminate the cervical spine
• Active cervical extension (Fig. 9.4a)
 |
| Figure 9.4
Six active cervical movements to eliminate the cervical spine as a cause of pain. (a) Extension; (b, c) rotations; (d, e) side flexions; (f) flexion.
|
• Active right cervical rotation (Fig. 9.4b)
• Active left cervical rotation (Fig. 9.4c)
• Active right cervical side flexion (Fig. 9.4d)
• Active left cervical side flexion (Fig. 9.4e)
• Active cervical flexion (a dural sign due to the upward migration of the dura mater in this area during cervical flexion) (Fig. 9.4f)
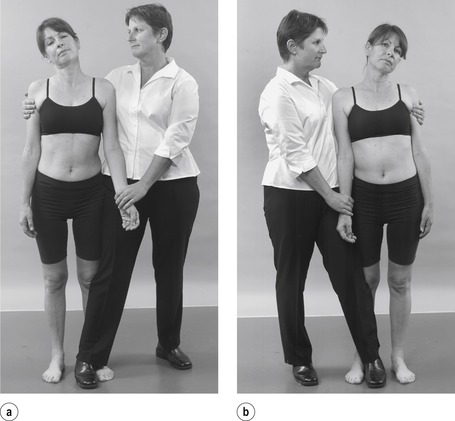
Dural test
• Scapular approximation (Fig. 9.5)
 |
| Figure 9.5
Dural test: scapular approximation.
|
Articular and muscle signs
Standing
• Active thoracic extension (Fig. 9.6)
 |
| Figure 9.6
Active extension.
|
• Active right thoracic side flexion (Fig. 9.7a)
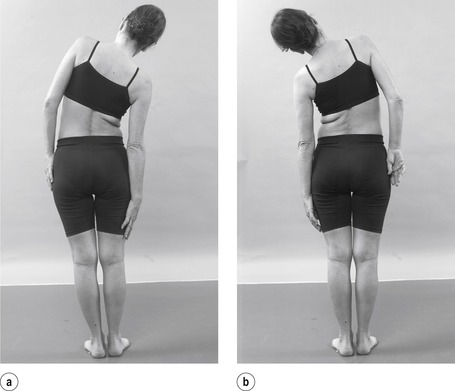 |
| Figure 9.7
Active side flexions.
|
• Active left thoracic side flexion (Fig. 9.7b)
• Active thoracic flexion (Fig. 9.8)
 |
| Figure 9.8
Active flexion.
|
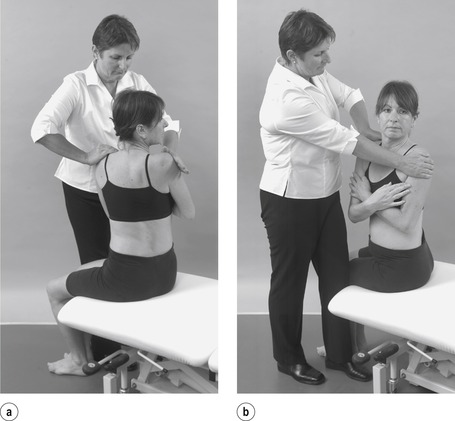
• Resisted thoracic side flexions (Fig. 9.9a,b)
 |
| Figure 9.9
Resisted side flexions.
|
Sitting
• Active thoracic right rotation (Fig. 9.10a)
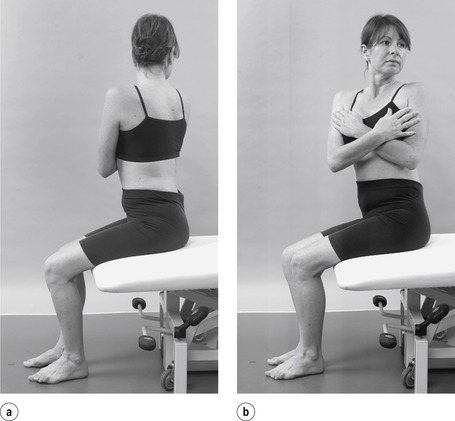 |
| Figure 9.10
Active rotations.
|
• Active thoracic left rotation (Fig. 9.10b)
• Passive thoracic right rotation (Fig. 9.11a)
 |
| Figure 9.11
Passive rotations.
|
• Passive thoracic left rotation (Fig. 9.11b)
• Resisted thoracic right rotation (Fig. 9.12a)
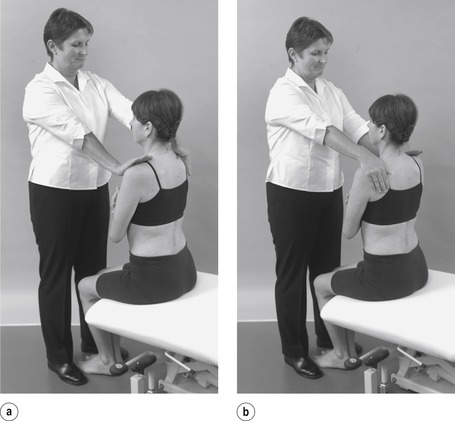 |
| Figure 9.12
Resisted rotations.
|
• Resisted thoracic left rotation (Fig. 9.12b)
• Resisted thoracic flexion (Fig. 9.13)
 |
| Figure 9.13
Resisted flexion.
|
Supine lying
• Plantar response (Fig. 9.14)
 |
| Figure 9.14
Plantar response.
|
Prone lying
• Resisted thoracic extension (Fig. 9.15)
 |
| Figure 9.15
Resisted extension.
|
Palpation
• Spinous processes for pain, range and end-feel (Fig. 9.16)
 |
| Figure 9.16
Palpation.
|
The cervical spine is a possible source of pain felt in the thoracic region and it must first be eliminated. If cervical flexion is the only movement to reproduce the thoracic pain, it is considered to be a dural sign for the thoracic spine since neck flexion draws the dura upwards (Fig. 9.4f). Scapular approximation is conducted as a dural test since it pulls on the dura via the T1 and 2 nerve roots and may be positive in a disc lesion at these levels (Fig. 9.5) (Cyriax & Cyriax 1993).
In common with other regions of the spine, the thoracic spine is considered to be an ‘emotional’ area and the movements are assessed actively to observe willingness to perform the movements, as well as assessing the articular signs for pain and limited range of movement. The capsular or non-capsular pattern will become evident through these movements.
Resisted side flexion is assessed looking for evidence of a muscle lesion. Resisted tests may also be applied if serious pathology or psychological factors are suspected.
The patient sits to fix the pelvis while the rotations are assessed for pain, range of movement, end-feel and the capsular pattern. End-feel, which is normally elastic, is particularly pertinent to the rotations since these movements may show minimal limitation and pain in minor subluxations of the posterior rib joints. Passive overpressure can be applied to any of the other movements if appropriate. Resisted flexion may also be assessed in this position.
The non-capsular pattern involves pain and/or limitation of at least one of the rotations.
A convenient shorthand for recording the findings of the objective examination can be found in Appendix 3 where the ‘star diagram’ is explained.
The patient is positioned in supine lying to test for the Babinski reflex, the extensor plantar response, by stroking up the lateral border of the sole of the foot and across the metatarsal heads. If the response is extensor, i.e. upgoing, it is indicative of an upper motor neuron lesion; the normal response is flexor.
The patient is positioned in prone lying to complete the examination. Resisted extension is applied and the spinous processes are palpated assessing pain, range of movement and end-feel at each segmental level.
Any other tests can be added to this basic routine examination of the thoracic spine, including repeated, combined and accessory movements and neural tension testing as appropriate.
TREATMENT OF THORACIC LESIONS
Manipulation is the treatment of choice for thoracic mechanical lesions, either minor subluxation of the posterior rib joints or an uncomplicated thoracic intervertebral disc lesion. Central displacement can endanger the spinal cord and, if present, the history and objective examination should reveal signs of spinal cord compression.
Contraindications to thoracic manipulation
It is impossible to be definitive about all contraindications to thoracic manipulation and nothing can substitute for a rigorous assessment of the presenting signs and symptoms and an accurate diagnosis.
‘Red flags’ are signs and symptoms found in the patient’s subjective and objective examination that may indicate serious pathology and provide contraindications to thoracic manipulation (Greenhalgh & Selfe 2006, Sizer et al 2007) (see Red flags p. 231).
The absolute contraindications are highlighted in the discussion below but there are several relative contraindications that should be considered as well. It may be useful to use the mnemonic ‘ COINS’ (a contraction of ‘contraindications’), as an aide-mémoire to be able to create mental categories for the absolute contraindications: Circulatory, Osseous, Inflammatory, Neurological and suspicious features indicating Serious pathology. If the first and last two letters are pushed together as ‘ CONS’, the crucial need for consent is emphasized.
The treatment regime discussed below is absolutely contraindicated in the absence of informed patient consent. The patient should be given all details of their diagnosis together with the proposed treatment regime and a discussion of the risks and benefits should ensue to enable them to give their informed consent. Consent is the patient’s agreement, written or oral, for a health professional to provide care. It may range from an active request by the patient for a particular treatment regime, to the passive acceptance of the health professional’s advice. The process of consent, within the context of the orthopaedic medicine, is ‘fluid’ rather than one instance in time when the patient gives their consent. The patient is constantly monitored and feedback is actively requested. The treatment procedures can be progressed or stopped at the patient’s request or in response to adverse reactions. Reassessment is conducted after each technique and a judgment made about proceeding. The patient has a right to refuse consent and this should be respected and alternative treatment options discussed. For further information on consent, the reader is referred to the Department of Health website: www.dh.gov.uk/consent.
Signs and symptoms of spinal cord compression require urgent neurosurgical referral. Inflammatory arthritis affecting the thoracic synovial joints is not appropriate for manipulation but is a relative contraindication to treatment.
Suspicious features indicative of non-mechanical lesions would be an absolute contraindication to the orthopaedic medicine treatment regime. These symptoms should not be considered in isolation but in the general context of the whole examination procedure and may include unexplained weight loss, poor general health, pain unaffected by posture or activity, constant pain of which night pain is a feature and cord signs such as spastic gait and/or abnormal plantar response. Secondary tumour needs to be eliminated as a cause of pain in patients with a past history of primary tumour but the patient with a past history of primary tumour is not strictly contraindicated. Diagnosis of a mechanical lesion must be certain before proceeding with the treatment regime since bony metastases can form in the thoracic cage and may mimic mechanical pain.
The ill patient should be investigated for the cause of the systemic illness. As mentioned above, Horner’s syndrome is a contraindication to manipulation or mobilization of the thoracic joints until the cause of the symptoms has been determined, due to its association with more serious pathology. Anticoagulation therapy and blood clotting disorders are absolute contraindications unless medical advice is sought. Known osteoporosis with prolonged corticosteroid therapy is an absolute contraindication to manipulation and a sensible selection of less aggressive techniques is advised in mechanical lesions; however, pathological fracture will need to be excluded.
Safety recommendations for spinal manipulative techniques are included in Appendix 2.
Indications for thoracic manipulation
• Mechanical thoracic lesion, either a minor disc herniation or a minor subluxation of posterior rib joint
• A sudden or gradual onset of pain
• Central, unilateral, local or referred pain
• Non-capsular pattern, usually limitation and/or pain of at least one thoracic rotation
• No neurological signs
• No contraindications.
THORACIC MANIPULATION TECHNIQUES
It is recommended that a course in orthopaedic medicine is attended before the treatment techniques described are applied in clinical practice (see Appendix 1).
As with the cervical spine, the treatment techniques in this section will be described carefully in a step-by-step fashion to enable their application. However, the professional judgment and existing skill of the operator will allow each technique to be adapted. The techniques described have been adapted from those originally described by Cyriax (1984) and Cyriax & Cyriax (1993). Clinically, minor subluxation of a posterior rib joint has been judged to be a more common lesion than thoracic disc lesion and hence the techniques are not carried out under traction. As with all manipulations, the comparable signs are reassessed after each manoeuvre and a decision made about the next. If the techniques fail to produce a reduction in signs and symptoms, they can be applied under traction (see below) (Cyriax 1984, Cyriax & Cyriax 1993).
The position of the bed for each manoeuvre is a matter of personal choice. The extension thrust techniques are best conducted with the bed as low as possible.
Straight extension thrust
Position the patient comfortably in prone lying, preferably with the head in neutral, with the face positioned in the nose hole and the arms resting over the edge of the couch or at the patient’s side. Palpate for the tender thoracic level. Apply the ulnar border of your hand, reinforced with the other hand, to the most tender spinous process, which will indicate the level of the lesion (Fig. 9.17). With the patient relaxed, apply downward pressure to test the end of range of the tissues. Remove all pressure and ask the patient to take a small breath in. Apply pressure downwards with straight arms, following the breath out. Apply a minimal amplitude, high velocity thrust once all the slack is taken up.
 |
| Figure 9.17
Straight extension thrust.
|
This technique can be uncomfortable for the patient as the thrust is applied to the tender bony spinous process. The following manoeuvre is much more comfortable for the patient. Both techniques may have to be applied at one or two levels. It is common to find one, two or even three tender levels, in which case the most tender level is chosen first.
Extension with a rotational component
Position the patient as for the above manoeuvre and again locate the most tender spinous process by palpation. The technique can be applied in one of two ways but it may be necessary to do both if, on reassessment, the first manoeuvre is unsuccessful.
Position your hands as follows on either side of the spinous processes over the paraspinal muscle bulk, approximately over the underlying transverse processes.
1. Take the pisiform of your hand which is nearest to the patient’s head and place it adjacent to the spinous process and on the side nearest to yourself at the painful level (fingers pointing caudally). The pisiform will now be resting over the transverse process (Figure 9.18, Figure 9.19 and Figure 9.20). Place the trapeziofirst-metacarpal joint of your other hand adjacent to the spinous process on the level above, resting on the transverse process on the opposite side. With the patient relaxed, apply downward pressure to test the end of range of the tissues. Remove all pressure and ask the patient to take a small breath in. Follow the movement down as the patient breathes out; the position of your hands will automatically apply the rotation/extension thrust and rotation of the hands is unnecessary. Apply a minimal amplitude, high velocity thrust through straight arms once all of the slack is taken up.
 |
| Figure 9.18
Extension with a rotational component.
|
 |
| Figure 9.19
Extension with a rotational component showing hand position.
|
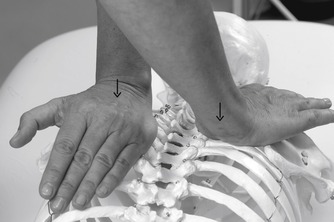 |
| Figure 9.20
Extension with a rotational component, hand position demonstrated on spine.
|
2. This technique is the reverse of that described above, or a similar effect will be achieved by perfoming the technique as described above, but from the other side of the bed. Take the trapeziofirst-metacarpal joint of your hand which is nearest to the patient’s head and place it adjacent to the spinous process at the painful level (fingers pointing caudally). The trapeziofirst-metacarpal joint will now be resting over the transverse process on the side opposite to yourself (Figure 9.21, Figure 9.22 and Figure 9.23). Place the pisiform of your other hand on the level above, over the transverse process on the side nearest to yourself. With the patient relaxed, apply downward pressure to test the end of range of the tissues. Remove all pressure and ask the patient to take a small breath in. Follow the movement down as the patient breathes out; the position of your hands will automatically apply the rotation/extension thrust and rotation of the hands is unnecessary. Apply a minimal amplitude, high velocity thrust through straight arms once all of the slack is taken up.
 |
| Figure 9.21
Extension with a rotational component; alternative position.
|
 |
| Figure 9.22
Extension with a rotational component showing alternative hand position.
|
 |
| Figure 9.23
Extension with a rotational component, alternative hand position demonstrated on spine.
|
Sitting rotation
Position the patient astride the end of a narrow couch to fix the pelvis, with the patient’s back towards you and the patient’s arms folded across the chest. Stand close to the patient and bend your knees. Hug the patient so that the patient’s shoulder fits into the front of your axilla (Fig. 9.24). Keep the patient as close as possible, while the heel of your other hand rests adjacent to the spinous process just above the painful level (Fig. 9.25). Ask the patient to rotate actively as far as possible. Rotate the spine a little further passively and straighten your knees to apply some traction to the patient’s upper trunk (Fig. 9.26). Rotate a little further and apply a minimal amplitude, high velocity thrust towards rotation once all of the slack is taken up, by smartly rotating your body and pushing through the heel of your hand.
 |
| Figure 9.24
Sitting rotation, starting position.
|
 |
| Figure 9.25
Sitting rotation, showing hand position just above painful level.
|
 |
| Figure 9.26
Sitting rotation, traction applied by straightening knees, before application of the Grade C manipulation.
|
Sitting extension thrust with a degree of traction
This technique is useful if the patient is large and the practitioner small, as body weight can be used more effectively to apply the traction.
Position the patient in sitting on the end of the couch with the patient’s hands, overlapping each other, behind his or her head. Stand on the couch behind the patient and place one knee at the painful level, with a pillow or padding placed between your knee and the patient’s back. Wrap your hands over and below the patient’s upper arms, with your thumbs on the side chest wall and your fingers resting over the patient’s scapulae (Fig. 9.27). Apply traction by moving your body weight upwards and backwards onto your other leg (Fig. 9.28); be careful not to bend the patient backwards over the fulcrum of your knee, as this is very uncomfortable for the patient. Once the patient has relaxed, extend the thoracic spine by applying a small amplitude, high velocity upward jerk of your knee against the spine.
 |
| Figure 9.27
Sitting extension thrust, starting position.
|
 |
| Figure 9.28
Sitting extension thrust with a degree of traction.
|
Thoracic traction
Thoracic traction is difficult to apply and is not as effective as in the cervical and lumbar joints, probably due to the comparative rigidity of the spine and to the sternal and vertebral attachments of the ribs.
Cyriax devised a method of applying distraction before performing the straight extension and the extension with rotational component techniques, using two assistants to pull longitudinally through the patient’s arms and legs before the technique is applied (Cyriax 1984, Cyriax & Cyriax 1993). In practice, two assistants are rarely readily available and the added benefit of the distraction is unproven. However, the added distraction may be considered for patients with symptoms that are resistant to other treatment techniques.
The higher and lower thoracic levels form part of the cervicothoracic and thoracolumbar transition levels respectively, and traction, or mobilization under traction, applied to the cervical and lumbar regions will affect these levels. For mid to lower thoracic levels the thoracic harness needs to be placed higher on the rib cage, which can lead to uncomfortable pressure in the axillae that is not well tolerated by the patient.
If the history, signs and symptoms do warrant its use, it is applied on the same lines as for the lumbar spine (see Ch. 13).
Intercostal muscle strain (Cyriax 1984)
Generally, muscle lesions at the spinal joints are rare. However, it is not uncommon to find a lesion in the intercostal muscles. The onset of pain may follow a chest infection with prolonged coughing, overexertion or as the result of a fractured rib. Pain is felt locally and reproduced on resisted testing. Palpation reveals an area of tenderness in one intercostal space.
The lesion responds well to transverse frictions. Position the patient in half-lying and locate the tender area (Fig. 9.29). Using an index or middle reinforced finger, direct the pressure up or down against the affected rib and apply transverse frictions parallel to the rib, according to the general principles.
 |
| Figure 9.29
Friction of the intercostal muscles.
|
REFERENCES
Agur, A.M.R.; Dalley, A.F., Grant’s Atlas of Anatomy. 12th edn. ( 2009)Lippincott Williams & Wilkins, Philadelphia.
Bogduk, N.; Valencia, F., Innervations and pain patterns of the thoracic spine, In: (Editor: Grant, R.) Clinics in Physical Therapy, Physical Therapy of the Cervical and Thoracic Spine2nd edn. ( 1994)Churchill Livingstone, Edinburgh, pp. 77–87.
Boriani, S.; Biagini, R.; de Lure, F.; et al., Two-level thoracic disc herniation, Spine 19 (1994) 2461–2466.
Brown, C.W.; Deffer, P.A.; Akmakjian, J.; et al., The natural history of thoracic disc herniation, Spine 17 (1992) S97–S102.
Corrigan, B.; Maitland, G.D., Practical Orthopaedic Medicine. ( 1989)Butterworths, London.
Cyriax, J., 11th edn.Textbook of Orthopaedic Medicine. vol. 2 ( 1984)Baillière Tindall, London.
Cyriax, J.; Cyriax, P., Cyriax’s Illustrated Manual of Orthopaedic Medicine. ( 1993)Butterworth Heinemann, Oxford.
Edmondston, S.J.; Singer, K.P., Thoracic spine: anatomical and biomechanical considerations for manual therapy, Man. Ther. 2 (3) ( 1997) 132–143.
Greenhalgh, S.; Selfe, J., Red Flags. ( 2006)Elsevier, Edinburgh.
Heithoff, K.B.; Gundry, C.R.; Burton, C.V.; et al., Juvenile discogenic disease, Spine 19 (1994) 335–340.
Hodges, S.D.; Fronczak, S.; Zindrick, M.R.; et al., Extradural synovial thoracic cyst, Spine 19 (1994) 2471–2473.
Kapandji, I.A., The Physiology of the Joints, Trunk and the Vertebral Column. vol. 3 ( 1974)Churchill Livingstone, Edinburgh.
Kumar, P.; Clark, M., Clinical Medicine. 5th edn. ( 2002)Baillière Tindall, London.
Maiman, D.J.; Pintar, F.A., Anatomy and clinical biomechanics of the thoracic spine, Clin. Neurosurg. 38 (1992) 296–324.
Mellion, L.R.; Ladeira, C., The herniated thoracic disc: a review of the literature, J. Man. Manip. Ther. 9 (3) ( 2001) 154–163.
Nakayama, H.; Hashimoto, H.; Hase, H.; et al., An 80 year old man with thoracic disc herniation, Spine 15 (1990) 1234–1235.
Oppenheim, J.S.; Rothman, A.S.; Sachdev, V.P., Thoracic herniated discs – review of the literature and 12 cases, Mt. Sinai. J. Med. 60 (1993) 321–326.
Osman, A.A.; Bassiouni, H.; Koutri, R.; et al., Ageing of the thoracic spine: distinction between wedging on osteoarthritis and fracture in osteoporosis – a cross-sectional and longitudinal study, Bone 15 (1994) 437–442.
Ozturk, C.; Tezer, M.; Sirvanci; et al., Far lateral thoracic disc herniation presenting with flank pain, Spine J. 6 (2006) 201–203.
Palastanga, N.; Field, D.; Soames, R., Anatomy and human movement. 5th edn. ( 2006)Butterworth-Heinemann, Edinburgh.
Sizer, P.; Brismée, J.; Cook, C., Medical screening for red flags in the diagnosis and management of musculoskeletal spine pain, Pain Pract. 7 (1) ( 2007) 53–71.
Taylor, J.R.; Twomey, L.T., Vertebral column development and its relation to adult pathology, Aust. J. Physiother. 31 (1985) 83–88.
Turner, P., Osteoporotic back pain – its prevention and treatment, Physiotherapy 77 (1991) 642–646.
Watanabe, M.; Kihara, Y.; Matsuda, Y.; et al., Benign osteoblastoma in the vertebral body of the thoracic spine – a case report, Spine 17 (1992) 1432–1434.
Whitcomb, D.C.; Martin, S.P.; Schoen, R.E.; et al., Chronic abdominal pain caused by thoracic disc herniation, Am. J. Gastroenterol. 90 (5) ( 1995) 835–837.
Wilke, A.; Wolf, U.; Lageard, P.; et al., Thoracic disc herniation: a diagnostic challenge, Man. Ther. 5 (3) ( 2000) 181–184.
Yeung, M.; Hagen, N., Cervical disc herniation presenting with chest wall pain, J. Neurol. Sci. 20 (1993) 59–61.