8 THE SPINE
Applied Anatomy and Biomechanics of the Spine
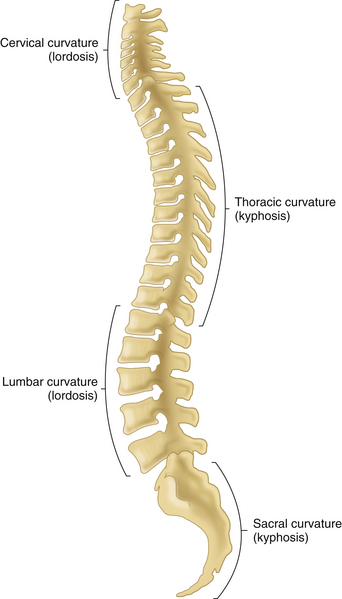
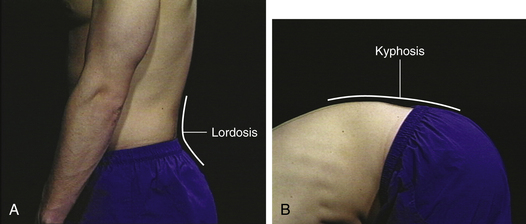
The vertebral column consists of 33 vertebrae—7 cervical (C), 12 thoracic (T), 5 lumbar (L), 5 sacral (S), and 4 coccygeal vertebrae—and 23 intervertebral disks. Its structure provides a remarkable combination of rigidity, stability, and flexibility. Rigidity provides an essential vertical bony axis, stability provides strong scaffolding for cavities and extremities, and flexibility permits complex movements of the neck and low back. The spinal column is composed of four balanced curves: a cervical lordosis, a thoracic kyphosis, a lumbar lordosis, and a sacrococcygeal kyphosis (Figure 8-1). The compensatory nature of the balanced spinal curves allows the normal resting, erect posture to be maintained with minimal muscular effort.
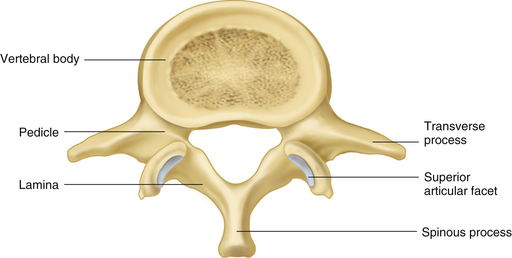
The neural arch is made up of two pedicles attached to the vertebral body and two laminae, which fuse in the midline to form the spinous process. Three pairs of bony processes project from the arch close to the junction of the pedicles and laminae: two transverse processes, two superior articular processes, and two inferior articular processes. The paired articular processes at each level form the facet (apophyseal) joints (Figure 8-2). In the cervical spine, these joints bear about half of the weight of the head. In the lumbar spine, they accept less than a fifth of the load. This fact accounts for the relative difference in size between the facet joints and the vertebral bodies in the neck and low back. In the cervical spine, the joints are flat and slide easily. In the lumbar spine, they are curved to lock together and provide stability. In both areas the superior joints face backward.
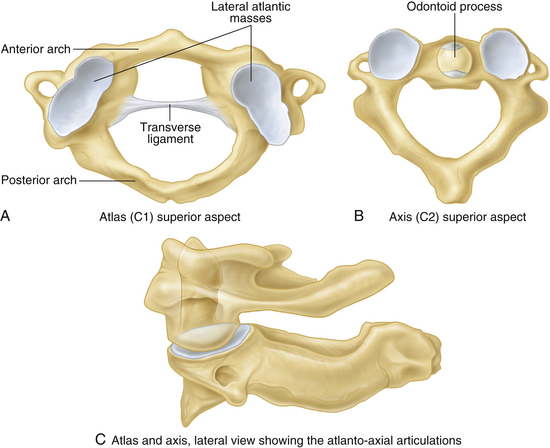
Several vertebrae deserve special comment, because they have unique features. The first cervical vertebra, C1, also called the atlas, lacks a vertebral body and consists of anterior and posterior arches and two cup-shaped lateral masses (Figure 8-3). Just as Atlas in Greek mythology was forced to bear the world on his shoulders, so the cervical atlas (C1) bears the skull on its “shoulders” (lateral masses), each articulating with the occipital condyles on either side of the foramen magnum at the atlantooccipital joints. These joints allow nearly 40° of flexion–extension, for nodding the head, and 10° of lateral flexion. The second cervical vertebra, C2 or the axis, has a vertebral body anteriorly; from it a fingerlike peg projects superiorly. This bony process, called the odontoid or dens (den and dont from the Latin “tooth”), fits snugly against the anterior arch of the atlas, forming the atlantoaxial joint. The two are held together by the fibrous transverse ligament, which runs behind the odontoid process (see Figure 8-3). Rotation of the cervical spine, such as when shaking the head “no,” occurs mainly at the atlantoaxial joints (about 50°). There are no intervertebral disks between the atlas and occiput or between the atlas and the axis.
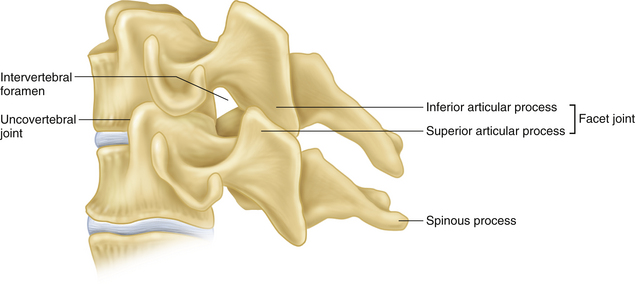
The third through the seventh cervical vertebrae possess more typical vertebral bodies and posterior elements, as well as intervertebral disks, and a foramen in each transverse process for the vertebral arteries. In addition, C3 through C7 vertebrae frequently form bony projections posteriorly and laterally from the superior end plate of each vertebra, which articulate with the beveled inferolateral surface of the vertebra above to form the uncovertebral joints or joints of Luschka. They also provide lateral stability to the discovertebral complex and form a barrier to extrusion of disk material posterolaterally (Figure 8-4). The C3 through C7 vertebrae allow cervical spine flexion, extension, lateral inclination, and rotation.
The lumbar vertebrae are remarkable for their size. The larger cross-sectional area of the lumbar vertebral end plates facilitates load bearing by the intervertebral disks. The larger surface area of the lumbar facet joints provides increased torsional and sheer stability to these spinal segments, limiting rotation but allowing side bending. The superior facet joints face medially and backward (see Figure 8-2). The lumbar spine allows a greater range of motion (ROM) than the thoracic spine, including flexion, extension, lateral flexion, and rotation.
SPINAL JOINTS
Discovertebral Joints
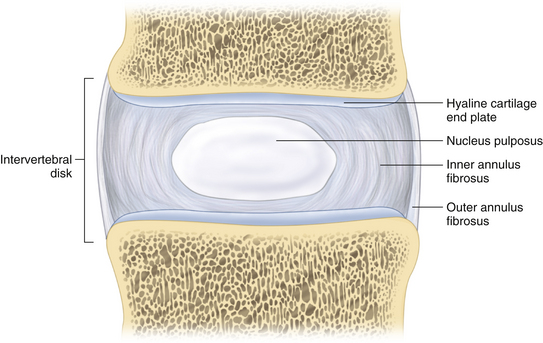
Each vertebral end plate is coated with a layer of hyaline articular cartilage (cartilaginous end plate). Adjacent vertebrae are united by a fibrocartilaginous intervertebral disk. Concentric, crossing layers of tough fibrous tissue, the annulus fibrosus, make up the outer circumference of the disk, enclosing a central, shock-absorbing gelatinous core, the nucleus pulposus (Figure 8-5). The intervertebral disks account for about one fourth of the height of the vertebral column above the sacrum. The sacrococcygeal vertebrae are fused and have no intervertebral disks. The disks are thickest in the lumbar spine and thinnest in the thoracic spine, and the cervical disks are intermediate in size. The intervertebral disks distribute the weight over the surface of the vertebral body and act as shock absorbers during loading, converting vertical load into horizontal thrust, which is absorbed by the elastic mechanism of the annulus. The disks provide a strong tie between the vertebrae yet allow a greater range of spinal movements compared with a solid column.
LIGAMENTS
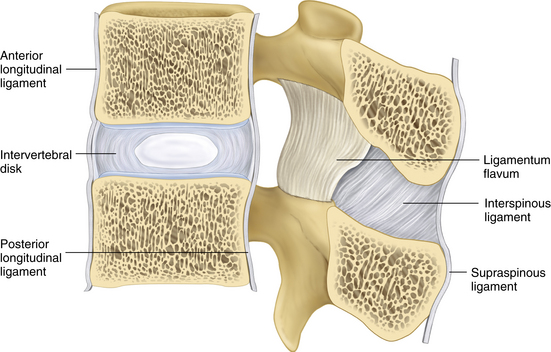
Numerous ligaments stabilize the anterior and posterior elements of the spinal column. The anterior longitudinal ligament is a strong, broad fibrous band that runs from the occiput to the sacrum, where it anchors the anterior vertebral surfaces and intervertebral disks (Figure 8-6); it prevents excessive extension of the spine. The posterior longitudinal ligament also runs the length of the spinal column. It is a weak and narrow band but broadens where it attaches to the posterior intervertebral disks. Multiple ligaments also stabilize the posterior elements. The ligamentum flavum interconnects the vertebral laminae at the posterior roof of the spinal canal, and the weak interspinous ligaments and the stronger supraspinous ligaments interconnect the spinous processes. The latter two sets of ligaments partially limit forward and lateral flexion of the spine (see Figure 8-6). The intertransverse ligaments interconnect the transverse processes.
MUSCLES
A number of muscles span multiple spinal segments and provide both mobility and considerable stability to the spine. The cervical and lumbosacral spines are endowed with muscles anteriorly, laterally, and posteriorly, whereas the thoracic spinal muscles are exclusively posterior. Abdominal, trunk, and limb muscles assist the intrinsic muscles of the spine in achieving a wide range of movements.
SURFACE ANATOMY
Several landmarks can facilitate localizing specific spinal segments. The T2 vertebra is at the level of the top of the manubrium sterni. The apex of the spine of the scapula is even with the spine of T3, and the lower pole of the scapula is in line with the spine of T8. Although the position of the umbilicus varies with age, sex, obesity, and posture, it is generally on the same plane as the bottom of L3. A line connecting the upper border of the iliac crests crosses the midline at the level of L4, and a line drawn between the posterior superior iliac spines—beneath the sacral dimples, or “dimples of Venus”—crosses the second sacral segment.
History and Physical Examination
FOCUS OF INITIAL HISTORY IS CRITICAL
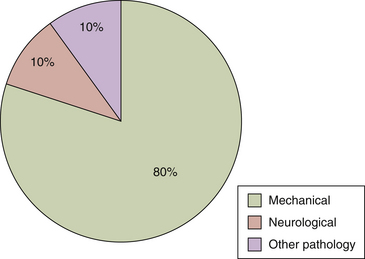
It is crucial to focus the initial history on the one problem that accounts for more than 80% of neck and back symptoms: mechanical, spine-predominant (neck or low back) pain (Figure 8-7). Mechanical pain can be defined as symptoms arising from the irritation of a physical element or elements within the spine, predictably aggravated and relieved by specific movements and positions. It is the result of an anatomic malfunction unrelated to infection, neoplastic disease, systemic illness, or major trauma. An additional 10% of patients may present with symptoms of nerve root irritation with neurological, extremity-predominant radicular (arm or leg) pain.
History
NECESSARY INFORMATION
Taking a history of spinal pain should be directed yet comprehensive. Appropriate evaluation requires a careful delineation of pain characteristics and associated features. A helpful mnemonic for characterizing spinal pain is OPQRSTU: O = onset; P = precipitating/ameliorating factors or prior episodes/treatment; Q = quality; R = radiation; S = severity; T = timing; and U = urinary or upper motor neuron symptoms.
Physical Examination
CERVICAL SPINE (Table 8-1)
| Basic Examination |
| Observation |
| Observe posture, movement, and behaviors |
| Inspection |
| Note resting posture and alignment, both sitting and standing |
| Inspect skin anteriorly and posteriorly |
| Palpation |
| Palpate occiput and spinous processes |
| Check for fibromyalgia tender points (suboccipital muscle insertions, medial upper border of trapezius, supraspinatus, and medial scapular borders) |
| Range of Motion |
| Cervical spine flexion, extension, right and left rotation, and right and left lateral flexion |
| Special Testing: Suspected Shoulder Pathology (Neck and Proximal Arm Pain) |
| Examination of shoulders |
| Special Testing: Suspected Nerve Root Compression |
| Reflexes: biceps (C5), brachioradialis (C6), and triceps (C7) |
| Muscle strength: deltoid, resisted shoulder abduction (C5); biceps, resisted elbow flexion (C6); triceps, resisted elbow extension (C7); interosseous, resisted finger abduction (C8) |
| Sensation: over lateral deltoid (C5), at thumb and index finger (C6), at middle finger (C7), and at ring and little fingers (C8) |
| Spurling sign: reproduction of radicular pain by applying gentle, firm pressure to occiput during combined rotation and extension to the affected side |
| Abduction relief sign: relief of radicular pain with placing distal forearm/wrist of affected upper extremity on occiput |
| Special Testing: Suspected Myelopathy |
| Hoffman sign: flick tip of middle finger; note involuntary flexion of thumb and index finger together |
| Knee and ankle reflexes and ankle clonus |
| Babinski sign |
| Gait: note broad base or unsteadiness, check |
Neurologic Examination
Irritative tests. Because of the mobility and multiple branches of the brachial plexus, the validity of irritative tests in the cervical spine to identify nerve root irritation is less certain than for those in the lower back. Rotating the head toward the painful side while forcing the neck into extension (Spurling maneuver, Figure 8-8) may reproduce the patient’s described arm pain, but a negative test does not rule out direct root involvement. Extending, abducting, and externally rotating the arm while extending the wrist and tilting the head to the contralateral side may also reproduce radicular symptoms. The intervening brachial plexus significantly diminishes the test’s sensitivity. Patients who experience a reduction in their arm pain by sitting with the hand on the affected side on top of their head (abduction relief sign, Figure 8-9) may be diminishing nerve root irritation by reducing tension on the lower plexus or lower cervical roots.
Conductive tests. Motor testing is the most reliable physical measure of nerve conduction. In order, the most commonly involved nerve roots in the cervical spine are C6, C7, and C5. The examiner should gauge the strength of elbow flexion (C6, biceps), forward elevation of the arm (C6, anterior deltoid), elbow extension (C7, triceps), finger extension at the MCP joints (C7, extensor digitorum), and abduction of the arm (C5, central deltoid).
THORACIC SPINE
Neurological Examination
Upper motor tests. The only possible neurological impairment that requires routine examination in the thoracic spine is spinal cord impingement. Individual root irritation produces focal pain around the chest that can be recognized on history but for which there is no corresponding physical test. Patients with suspected pathology in the thoracic spine should have their legs examined for increased reflex activity, clonus, and an abnormal plantar response.
LUMBAR SPINE (Table 8-2)
Inspection
| Basic Examination |
| Observation |
| Observe posture, movement, and behaviors |
| Inspection |
| Observe gait and heel and toe walking |
| Observe resting posture, alignment, and curvature |
| Inspect skin |
| Palpation |
| Assess skin tenderness to light touch or “skin rolling” |
| Palpate spinous processes (upper thoracic spine to sacrum) |
| Range of Motion |
| Lumbar spine flexion, extension, and right and left lateral bending |
| Special Testing: Suspected Hip Pathology (Low Back, Buttock, and Proximal Leg Pain) |
| Examination of hips |
| Special Testing: Suspected Nerve Root Compression |
| Lying: SLR |
| Sitting: Patellar (L4) and Achilles (S1) reflexes |
| Foot inversion and ankle dorsiflexion (L4), great toe dorsiflexion (L5), and foot eversion (S1) |
| “Quadriceps strength” (distracted SLR in sitting position) |
| Medial foot and ankle (L4), dorsum of foot (L5), lateral foot and ankle (S1) sensation |
| Perianal sensation, anal reflex, and sphincter tone (cauda equina syndrome) |
| Special Testing: Suspected Psychological Distress—Waddell’s Behavioral Signs |
| Superficial or nonanatomic tenderness |
| Simulated rotation (pelvis) or compression (head) |
| Discrepant SLR (lying and seated) |
| Nonanatomic regional sensory or motor disturbances |
| Overreaction |
| Special Testing: Suspected Visceral or Vascular Disease |
| Abdominal, pelvic, and rectal examinations |
| Examination for abdominal aortic aneurysm and peripheral leg pulses |
Range of Motion
Assess lumbar flexion by instructing the patient to bend forward at the waist and attempt to touch the toes. Normal lumbar flexion should involve progressive reversal of the lumbar curvature from lumbar lordosis in the standing position to flattening of the lordosis in mid flexion to flattening or even slight lumbar kyphosis at the end of full flexion (Figure 8-10). Assess lumbosacral extension by asking the patient to bend backward. Simultaneously supporting the low back with one hand and one shoulder with the other hand provides stability and permits you to help the patient into full extension. Assess lumbar lateral flexion (lateral bending) by asking the patient to bend to the right and to the left. Place your hands on both shoulders and, if necessary, provide gentle pressure to help the patient into lateral flexion and assess the patient’s response.
Neurological Examination
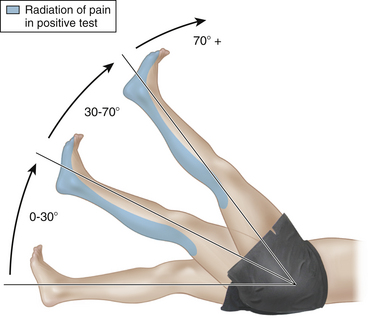
Irritative tests. A passive straight leg raise (SLR) should reproduce the patient’s typical leg-predominant pain resulting from irritation of the roots of the sciatic nerve (L4, L5, S1, S2). With the patient lying supine, support the heel of the foot on the patient’s painful leg in the palm of your hand. With the patient’s knee extended, lift the leg. An increase in the patient’s reported leg pain constitutes a positive test (Figure 8-11). The location of the leg pain should be the same as that described in the history. The production of back pain is not a positive test and does not indicate nerve root irritation.
Many patients with severe sciatica cannot fully extend the knee on the affected side, and any attempt to do so will aggravate the characteristic leg pain. This constitutes a positive test. Patients demonstrating less nerve root irritability will allow increasing amounts of elevation. The higher the leg can be lifted, the less acute the radiculitis and therefore the less clinically significant the finding. But regardless of the point in the SLR at which the typical pain is produced, reproduction of the patient’s specific complaint is a positive finding. Variations on the technique—such as dorsiflexing the ankle, applying pressure to the popliteal fossa, or passively extending the knee with the hip already flexed at 90°—are all intended to create the same leg pain. Once the examiner has exacerbated the patient’s leg symptoms with one method, hurting the patient again in a different fashion seems unnecessary and unkind.
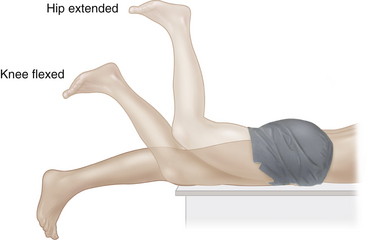
The femoral stretch test is comparable to the SLR but involves the roots of the femoral nerve (L2, L3, L4). With the patient lying prone, the examiner lifts the affected leg into extension at the hip (Figure 8-12). A positive response replicates the patient’s typical anterior thigh pain. The maneuver must aggravate the leg symptoms described in the patient’s history. Causing back pain is not a positive test.
Upper motor tests. The spinal cord and the conus medullaris end at L2. No problem below that point can produce signs of upper motor damage. Some spinal cord lesions are capable of mimicking a single lumbar root lesion and can be completely missed without an upper motor examination. Finding sustained clonus or an extensor plantar response places the pathology at the cord level, above the lower lumbar spine.
Nonmechanical and Nonradicular Spinal Pain and Other Etiologies
When the clinical picture is not a clearly defined mechanical or neurological syndrome, the focus must shift to identifying risk factors that suggest spinal pain associated with a possible serious underlying disease. A number of risk factors, or “red flags,” have been shown to be associated with an increased risk of underlying serious disease—cancer, infection, or fracture—as a cause of spinal pain. These risk factors have been studied primarily in patients with low back pain, however they likely apply to spinal pain in general. These risk factors are listed in Table 8-3. Each serious disease is matched with several associated risk factors.
TABLE 8-3 RISK FACTORS FOR POTENTIALLY SERIOUS DISEASE IN SPINAL PAIN
| Possible Cause | Key History and Examination Findings |
|---|---|
| Cancer |
CANCER, INFECTION, AND VERTEBRAL COMPRESSION
A history of cancer, especially diagnosed within the past 10 years, appears to be the most important risk factor. The presence of this risk factor increases the probability of cancer as a cause of low back pain from 0.7%—the probability of any individual having cancer-related low back pain—to 9.0%, the probability of this individual having cancer-related low back pain, now knowing there is a history of cancer. In the absence of a history of cancer, the presence of any one of the other risk factors in Table 8-1 only increases the probability of cancer to 1.2%.
The absence of any risk factors listed in Table 8-3 for cancer, infection, or vertebral compression fracture provides the clinician with extremely high reassurance that these conditions are not likely the cause of the patient’s low back pain.
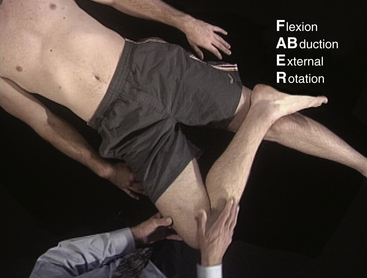
INFLAMMATORY SPINAL PAIN: ANKYLOSING SPONDYLITIS AND OTHERS
If the clinical history suggests possible inflammatory low back pain, a more focused assessment of the sacroiliac joints and spine is appropriate (Table 8-4). Ask the patient to lie supine. Bring one hip and knee into flexion as you cross the leg over the opposite leg and rest the patient’s lateral malleolus on the opposite distal thigh (crossing the legs). Now, gently but firmly apply pressure to the medial aspect of the flexed knee, pushing it toward the exam table. This maneuver is called the FABER test, and it refers to the position of the hip in Flexion, ABduction, and External Rotation, stressing the ipsilateral sacroiliac joint (Figure 8-13). A positive FABER test requires reproduction of sacroiliac pain on the same side, felt in the upper inner buttock region rather than the lumbosacral junction, trochanter, or groin. This test may be difficult to interpret in patients with intrinsic hip disease, who may feel discomfort in the groin or gluteal region rather than the SI joint. Perform the FABER maneuver on the opposite side and compare.
| Special Testing: Suspected Sacroiliitis/Spondyloarthropathy |
| Lying |
| FABER test (hip flexion, abduction, and external rotation) |
| Compress iliac crests |
| Standing |
| Schober test of lumbosacral spinal mobility |
| Longitudinal Follow-up |
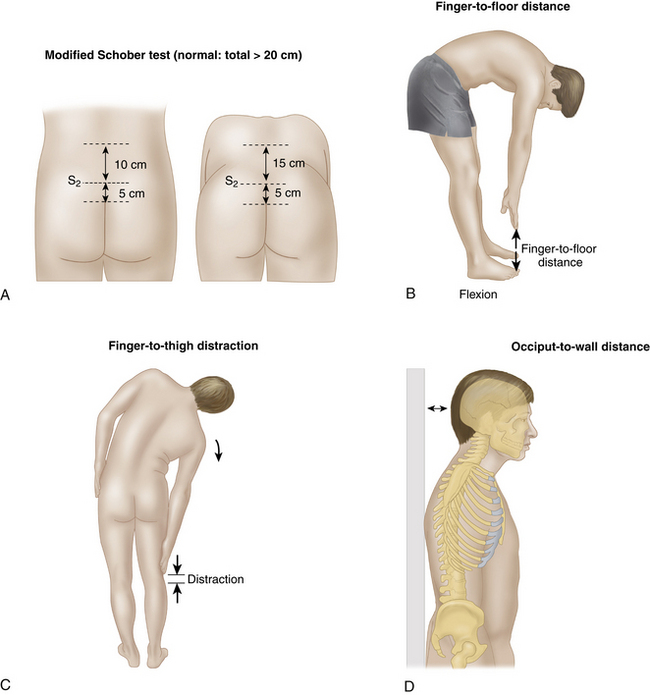
| Schober test of lumbosacral spinal mobility: modified Schober (15 cm → ___cm) |
| Finger-to-floor distance in maximal forward flexion (___cm) |
| Finger-to-thigh distraction in maximal lateral flexion, right and left (___cm) |
| Chest expansion measured at level of fourth intercostal space (___cm) |
| Occiput-to-wall distance (___cm) |
In patients whose history, examination, and imaging confirm the suspicion of a spondyloarthropathy, several spondylitis-specific measurements (Figure 8-14) are important to document initially, and in subsequent exams, to monitor disease progression and response to therapy:
PSYCHOSOCIAL DISTRESS
When spinal pain persists, and serious disease has been ruled out, risk factors for underlying psychosocial barriers to recovery should be investigated. These include personal, social, and environmental factors (Table 8-5). Personal factors include attitudes, beliefs, emotions, and behaviors that the patient exhibits in response to spinal pain that are maladaptive and may prolong disability. Social and environmental factors pertain to how the patient interacts with his or her family, friends, and the workplace. Negative social relationships can impact pain perception and recovery. Psychological distress, the belief and fear that movement or activity will worsen the pain, and social isolation are other examples of psychosocial barriers that can delay recovery from spinal pain.
TABLE 8-5 PSYCHOSOCIAL RISK FACTORS FOR PERSISTENT SPINAL PAIN
The presence of significant superficial or nonanatomic tenderness, back pain in response to simulated axial loading or pelvic rotation, marked differences in response to supine and seated straight leg raising, nonphysiologic regional disturbances in motor or sensory function, and the presence of significant overreaction manifested by inappropriate guarding, limping, bracing, rubbing, grimacing, or sighing during the examination are important clinical signs and should not be ignored. The assessment of Waddell’s categories can be readily integrated into a rapid, organized, and sequential examination of the low back.
Waddell unequivocally states that the presence of signs in three or more categories “simply shows the health care provider that abnormal illness behavior may be present as a coping strategy and that other learned cognitive and behavioral patterns and psychological influences may need to be addressed to improve treatment outcome (Waddell et al., 1980).”
Imaging and Electrodiagnostic Tests for Spinal Pain
IMAGING
The use of imaging in patients with spinal pain should be judicious and discriminating. Decisions should be based on the presence of clinical features (risk factors) in the history and physical examination that significantly raise the suspicion of underlying serious conditions. Specific causes of spinal pain that justify imaging include cancer, infection, fracture, spondyloarthropathies, and visceral disease (see Table 8-3).
Common Painful Disorders of the Spine
ACUTE, UNCOMPLICATED, MECHANICAL NECK AND LOW BACK PAIN
Acute, Mechanical Low Back Pain
This is commonly referred to as lumbosacral sprain, although there may be no evidence of ligamentous injury. Acute low back pain is a common, usually self-limiting but frequently recurrent problem. The pain may be precipitated by lifting or bending, although in the majority of cases, there is no specific triggering event. It can be felt in the lumbar spine, lumbosacral junction, buttock, and posterior thighs and may occasionally radiate below the knees. Physical examination reveals diffuse lumbar spine tenderness, muscle spasm, and diminished ROM without radicular symptoms or signs. Whether the pain originates in the paraspinal muscles, ligaments, disks (annular tears), facet joints, or other structures is not clear and usually is not clinically relevant. Although up to 85% of patients may return to normal activities within 2 months, recurrences may occur in up to 75% of patients within 12 months.
CHRONIC NECK AND LOW BACK PAIN
Neck and low back pain persisting beyond 3 months despite conservative management develops in a minority of patients and represents a significant clinical and economic problem. Chronic neck and back pain patients consume the majority of all expenditures for spine-related pain. Important historical features may relate to the patient’s work, home, personal, and psychosocial history. Occupational risk factors associated with chronic neck and low back pain include physical stresses involved in manual labor, mental stress in both manual and office workers, and job-related stress due to lack of autonomy, lack of variation in workload, and lack of cooperation among workers. Pending litigation or disability determinations, marriage and family stress, drug or alcohol problems, and a history of anxiety, depression, or somatization are important contributing factors. These risk factors of chronic neck and low back pain identify patients who are at higher risk for persistent, disabling symptoms and permit earlier referral to multidisciplinary specialized centers (see Table 8-5).
LUMBOSACRAL RADICULOPATHY
Low back pain combined with neurogenic lower extremity pain (sciatica) strongly suggests lumbosacral nerve root irritation. Pain may be abrupt or gradual in onset, and it typically radiates from the buttock to the posterior or posterolateral thigh or to the ankle or foot. There may be accompanying lower-extremity numbness, tingling, or weakness. The knee-flexed position, either supine or side-lying, often affords relief. Physical examination is remarkable for abnormal posture (list to one side), variable lumbosacral tenderness and muscle spasm, and reduced lumbosacral ROM. Nerve stretch signs (e.g., SLR, femoral stretch sign) indicating lumbosacral root irritation are frequently present. Neurologic testing may indicate diminished reflexes, strength, or sensation in the affected root distribution. Almost 85% of lumbosacral disk herniations involve the L4/L5 (L5 nerve root) or L5/S1 (S1 nerve root) level. In most cases symptoms resolve without the need for surgery, although symptoms persist longer than typical mechanical low back pain.
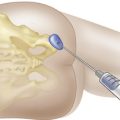
DEGENERATIVE LUMBAR SPINAL STENOSIS
Degenerative lumbar spinal stenosis is a relatively common cause of neurogenic lower-extremity pain in older individuals. Varying combinations of degenerative disk disease with loss of disk height, redundancy and hypertrophy of the ligamentum flavum, and occasionally degenerative spondylolisthesis lead to narrowing of the spinal canal with lateral recess or foraminal stenosis at multiple levels (Figure 8-15). Increased mechanical load on the facet joints combine with osteoarthritic changes and osteophyte formation. The onset of symptoms is typically insidious. The principal symptom is pain with tingling or numbness in one or both legs with standing, ambulation or spinal extension that is relieved by sitting or forward spinal flexion, but there may also be associated low back pain. Freedom from or improvement of symptoms during exercise in a flexed position (leaning on a grocery cart, walking uphill, bicycling) helps differentiate degenerative spinal stenosis from vascular claudication. Physical findings can include posterior thigh pain and transient motor weakness after 90 seconds of forced spinal extension, a wide-based gait, abnormal motor or sensory testing, and normal lower-extremity pulses. The physical examination is typically normal with the patient at rest, and the diagnosis is made primarily on the patient’s history. Differential diagnosis includes hip disease, trochanteric bursitis, and peripheral neuropathy.
INFLAMMATORY SPINAL PAIN
Spinal involvement in the spondyloarthropathies (e.g., ankylosing spondylitis, reactive arthritis, and spondylitis of inflammatory bowel disease) may involve the low back, thoracic spine, or neck and tends to occur early in the course of the disease. Initial symptoms are frequently vague and often overlooked. Characteristic features of inflammatory spondyloarthropathies include age less than 40 years, an insidious onset, significant morning stiffness, improvement of spinal pain with exercise and worsening with prolonged rest, awakening in the second half of the night with spinal pain, and a symptom duration of longer than 3 months. Although not specific, these features strongly suggest inflammatory back pain and are quite different from mechanical low back pain. The presence of SI joint pain and tenderness, limited spinal movements, and reduced chest expansion should prompt further investigation, most importantly an anteroposterior pelvic radiograph (Ferguson view) to check for radiographic sacroiliitis (Figure 8-16).
Accident Compensation Corporation (ACC). New Zealand Acute Low Back Pain Guide. Wellington: New Zealand, New Zealand Guidelines Group; 2004.
Barnsley L. Neck pain. In: Hochberg M.C., Silman A.J., Smolen J.S., et al, editors. Rheumatology. third ed. Edinburgh, UK: Mosby; 2003:567-581.
Bigos S.J., Bowyer O.R., Braen G.R. Acute Low Back Problems in Adults. Clinical Practice Guidelines No. 14. Rockville, MD: Agency for Health Care Policy and Research, Public Health Service, US Dept. of Health and Health Services; 1994. Publication No. 95-0642
Carroll L.J., Hogg-Johnson S., van der Velde G. Course and prognostic factors for neck pain in the general population: results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. Spine. 2008;33(4 Suppl):S75-S82. Review
Chou R., Fu R., Carrino J.A., Deyo R.A. Imaging strategies for low-back pain: systematic review and meta-analysis. Lancet. 2009;373(9662):463-472. Review
Chou R., Qaseem A., Snow V. Clinical Efficacy Assessment Subcommittee of the American College of Physicians; American College of Physicians; American Pain Society Low Back Pain Guidelines Panel. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann. Intern. Med.. 2007;147(7):478-491.
Croft P.R., Macfarlane G.J., Papageorgiou A.C. Outcome of low back pain in general practice: a prospective study. Br. Med. J.. 1998;316(7141):1356-1359.
Dagenais S., Caro J., Haldeman S. A systematic review of low back pain cost of illness studies in the United States and internationally. The Spine Journal. 2008;8(1):8-20.
Deyo R.A., Diehl A.K. Cancer as a Cause of Back Pain. J. Gen. Intern. Med.. 1988;3:230-238.
Deyo R.A., Weinstein J.N. Low back pain. N. Engl. J. Med.. 2001;344:363-370.
Deyo R.A. Diagnostic evaluation of LBP: Reaching a specific diagnosis is often impossible. Arch. Intern. Med.. 2002;162:1444-1447.
Guzmán J., Esmail R., Karjalainen K. Multidisciplinary rehabilitation for chronic low back pain: systematic review. Br. Med. J.. 2001;322(7301):1511-1516. Review
Guzman J., Haldeman S., Carroll L.J. Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. Clinical practice implications of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders: from concepts and findings to recommendations. Spine. 2008;33(4 Suppl):S199-S213. Review
Hall H., McIntosh G., Wilson L., Melles T. The spontaneous onset of back pain. Clin. J. Pain. 1998;14(2):129-133.
Hall H., McIntosh G., Boyle C. Effectiveness of a low back pain classification system. The Spine Journal. 2009;9(8):648-657.
Hart L.G., Deyo R.A., Cherkin D.C. Physician office visits for low back pain: Frequency, clinical evaluation and treatment patterns from a US national survey. Spine. 1995;20:11-19.
Jarvik J.G., Deyo R.A. Diagnostic evaluation of low back pain with emphasis on imaging. Ann. Intern. Med.. 2002;137(7):586-597.
Katz J.N., Harris M.B. Clinical practice. Lumbar spinal stenosis. N. Engl. J. Med.. 2008;358(8):818-825. Review
Kendrick D., Fielding K., Bentley E. The role of radiography in primary care patients with low back pain of at least 6 weeks duration: a randomised (unblinded) controlled trial. Health Technol Assess. 2001;5(30):1-69.
Kerry S., Hilton S., Dundas D. Radiography for low back pain: a randomised controlled trial and observational study in primary care. Br. J. Gen. Prac.. 2002;52(479):469-474.
Koes B., van Tulder M., Ostelo R. Clinical guidelines for the management of low back pain in primary care. Spine. 2001;26(22):2504-2514.
McCombe P.F., Fairbank J.C.T., Cockersole B.C., et al. Reproducibility of physical signs in low back pain. Spine. 1989;14:908-918.
Nordin M., Carragee E.J., Hogg-Johnson S. Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. Assessment of neck pain and its associated disorders: results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. Spine. 2008;33(4 Suppl):S101-S122. Review
Suarez-Almazor M.E., Belseck E., Russell A.S., Mackel J.V. Use of Lumbar Radiographs for the Early Diagnosis of Low Back Pain. J. Am. Med. Assoc.. 1997;277(22):1782-1786.
van den Hoogen H.J., Koes B.W., van Eijk J.T. On the course of low back pain in general practice: a one-year follow up study. Ann. Rheum. Dis.. 1998;57(1):13-19.
Viikaru-Juntura E., Porras M., Laasonen E.M. Validity of clinical tests in the diagnosis of root compression in cervical disc disease. Spine. 1989;14:253-257.
Vroomen P.C., deKrom M.C., Knottnerus J.A. Diagnostic value of history and physical examination in patients suspected of sciatica due to disc herniation: A systemic review. J. Neurol.. 1999;246:899-906.
Waddell G., McCullogh J.A., Kummel E., et al. Non-organic physical signs in low back pain. Spine. 1980;5:117-125.