The spinal cord and spinal reflexes
Basic anatomy and function of the spinal cord
Gross anatomy
The spinal cord begins superiorly at the foramen magnum where it is continuous with the medulla oblongata (S2.10). It continues inferiorly within the vertebral column protected in the vertebral canal by the meninges and cerebrospinal fluid (S2.8). The lowest part of the spinal cord lies at the first lumbar vertebra (level L1/2). Along the length of the spinal cord, there are two swollen regions: the cervical and lumbar enlargements, which represent the origins of the brachial and lumbosacral plexus, respectively.
Grey and white matter
In cross-section (Fig. 13.1), the spinal cord can be seen to consist of the inner grey matter (H shaped) and the remaining area termed the white matter. These are so named because of their microscopic appearance and a consequence of the cells located within the area. The white matter consists of myelinated axons and represents the existence of the ascending and descending tracts (S2.14, 15). The grey matter is formed by the cell bodies of the same neurons and includes motor neurons and many interneurons which make connections within segments and between segments of the spinal cord. The grey matter is described in terms of the anterior/ventral horn and posterior/dorsal horn (Fig. 13.1). In the thoracic and upper lumbar region there is also a lateral horn, which represents the sympathetic trunk, part of the autonomic nervous system.
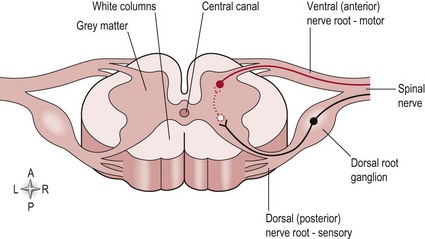
Figure 13.1 A cross-section of the spinal cord.
Spinal nerves
At each spinal level there are a pair (left and right) of spinal nerves which exit the vertebral canal via the intervertebral foramen. There are 31 pairs of spinal nerves in total (8 cervical, 12 thoracic, 5 lumbar and 5 sacral). The spinal nerve consists of a sensory root and motor root (Fig. 13.1) from the spinal cord. The sensory root transmits information into the spinal cord and its cell body is found in the dorsal root ganglion just adjacent to the spinal cord but within the vertebral canal. The motor root carries information out of the spinal cord and its cell body is located in the anterior/ventral horn of the grey matter of the spinal cord. The sensory and motor roots at one level combine to form a spinal nerve and are part of the peripheral nervous system. Spinal nerves from several levels of the spinal cord will combine to form a peripheral nerve. For example, the median nerve consists of the spinal nerves from levels C5/6/7/8 and T1, whereas the musculocutaneous nerve includes spinal nerves from levels C5/6/7.
Lower motor neuron/final common pathway and upper motor neuron
The lower motor neuron/final common pathway
The neurons indicated as nerve roots in Figure 13.1 are the starting point of the lower motor neuron division. Anything more peripheral is included in this division. In effect, damage to these neurons is interpreted as a deficit of the peripheral nervous system, for example, Guillain–Barré syndrome and motor neuron disease. However, different clinical presentations can occur within this division depending upon the location of the lesion. For example, damage to the spinal root or spinal nerve would present very differently to that of a peripheral nerve.
Spinal root or spinal nerve
Basic anatomy and function of spinal reflexes
The neural pathway involved in a simple reflex arc includes:
Sensory receptor: This detects a stimulus
Afferent neuron: This transmits information from the periphery to the spinal cord
Integrating centre: This modulates the response of the reflex
Efferent neuron: This transmits information from the spinal cord to the periphery (effector organ)
Effector organ: This carries out the reflex response and is usually a muscle or a gland.
The most important reflex arcs in relation to movement control are:
Stretch reflex
Phasic stretch reflex
This component of the stretch reflex is primarily monosynaptic:
Sensory receptor: A muscle spindle (dynamic nuclear bag), which responds to changes in length (stretch)
Afferent neuron: Type Ia afferent neurons enter the spinal cord through the dorsal horn and synapse in the grey matter directly on the efferent neuron
Efferent neuron: Alpha motor neuron (AMN)
Effector: Contraction of the same muscle from which the stretch was detected and any relevant synergist muscles required.
Function
The phasic component is evident in the intact nervous system at rest and is the component that is assessed during reflex testing (S3.22). An imposed stretch on the muscle by the clinician gives information on nerve integrity and the reflexic properties of muscle. This technique is referred to as a tendon jerk.
Tonic stretch reflex (TSR)
This component is primarily polysynaptic:
Sensory receptor: A muscle spindle (nuclear chain or static nuclear bag), which responds to changes in length (stretch)
Afferent neuron: Type II afferent neurons enter the spinal cord through the dorsal horn and synapse in the grey matter on interneurons
Integrating centre: Excitatory interneurons within the grey matter of the spinal cord which synapse upon the AMN
Efferent neuron: Alpha motor neuron
Effector: Contraction of the same muscle from which the stretch was detected and any relevant synergist muscles required.
Function
The tonic component is not apparent in an intact nervous system unless the muscle is already contracting. The TSR serves to set resting muscle tone (S3.21), the base level of muscle activity. The reflex arc also responds to changes in the environment adjusting the level of activity as appropriate to functional needs, e.g. lowering muscle activity when we lie down and raising it in preparation to stand up against gravity.
Golgi tendon organ (GTO)
This reflex arc is polysynaptic:
Sensory receptor: Golgi tendon organ, which responds to changes in tension at the musculotendinous junction
Afferent neuron: Type Ib afferent neurons enter the spinal cord through the dorsal horn and synapse in the grey matter on an interneuron
Integrating centre: Inhibitory interneurons within the grey matter of the spinal cord
Efferent neuron: Alpha motor neuron
Effector: Reduced contraction of the same muscle from which the tension was detected.
Flexor withdrawal and crossed extensor reflex
This reflex is polysynaptic and initiated from the flexor withdrawal arc:
Sensory receptor: Free nerve endings (pain) in the plantar aspect of the foot
Afferent neuron: Type A delta afferent neurons enter the spinal cord through the dorsal horn and synapse in the grey matter on an interneuron
Integrating centre: Excitatory interneuron
Efferent neuron: Alpha motor neuron
Effector: Contraction of the flexor muscles of the ipsilateral lower limb.
Additional neuronal activity associated with the reflex arc
First, the afferent neuron within the circuit includes the following branches which synapse upon:
• An inhibitory interneuron within the spinal cord, which inhibits the AMN of the antagonist muscle so that the effector muscle is not contested. This is termed reciprocal innervation.
• A second order neuron of the ascending tract (dorsal columns) (S2.15), which transmits information to the higher centres in relation to the state of the muscle (proprioception).
• An interneuron, which affects a gamma motor neuron. This latter neuron innervates the contractile ends of the muscle spindle itself making it shorten simultaneously with the muscle fibres of the effector muscle and so ensuring that it can remain responsive to stretch. This occurs concurrently with the AMN recruitment and is termed alpha gamma co-activation.
Second, the efferent neuron output from the reflex arc can be modulated by neurons from higher centres. This occurs via the descending tracts (S2.14), which synapse upon the alpha motor neuron directly or indirectly via interneurons. This descending control involves altering the level of output from the AMN to the muscle by enhancing either the inhibitory or excitatory synapses as required.
References and Further Reading
Hooper, SL. Central pattern generators. www.elsnet/elsonline/figpage/10000202html, 1999.
Kandel, ER, Schwartz, JH, Jessell, TM. Principles of neural science, ed 4. New York: McGraw-Hill Health Professions Division; 2000.
Kiehn, O, Butt, SJ. Physiological anatomical and genetic identification of CPG neurons in the developing mammalian spinal cord. Progress in Neurobiology. 2003; 70:347–361.





