Skin is considered to be the largest organ. It covers the whole surface of the body and is continuous at entry and exits points of the body with the mucous membranes lining the nose, mouth and anus, and the reproductive and urinary openings. Skin on the eyelids is replaced on the inner surfaces of the lids by the moist epithelium of the conjunctiva. At the ear the skin continues into the external acoustic meatus and is continuous with the tympanic membrane which separates the outer ear from the middle ear.
All four types of primary tissue (epithelial, connective, muscle and nerve) are present in the skin and its functions are related to its structure. The skin has roles in protection against microbes, physical and chemical damage and UV radiation; it also prevents excess water loss. Skin plays an important role in regulating body temperature by the ability of sweat glands to secrete sweat onto the surface of the skin which cools the body as it evaporates. In addition, the amount of blood flowing in vessels in the skin varies and this too helps in regulating heat loss and thus body temperature. Skin also has important roles as a sense organ detecting stimuli through specific sensory nerve receptors. In addition, cells in the surface of skin exposed to sunlight are involved in the production of vitamin D.
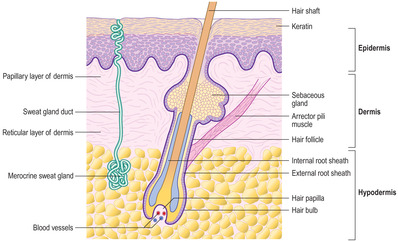
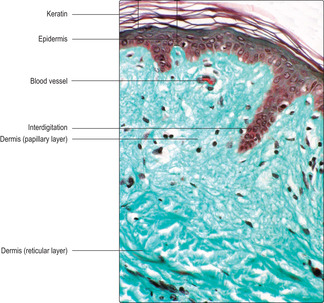
The skin consists of two layers: the superficial epidermis (the epithelium of skin) and the deeper dermis consisting mainly of connective tissue (Figs 7.1 and 7.2). The dermis is superficial to the hypodermis and the latter is not considered to be part of the skin. The hypodermis is composed mainly of connective tissue, which may contain large numbers of adipose cells; the hypodermis is also known as superficial fascia or subcutaneous tissue.
Epidermis
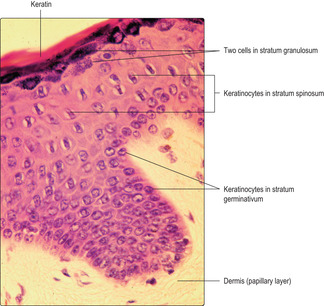
The epidermis is derived from the ectoderm germ layer of the embryo and is composed of a stratified, squamous, keratinised epithelium (Figs 7.2 and 7.3). It is made up of keratinocytes, the protein keratin and other specialised cell types (see below). Extending through the epidermis in many regions of the body are hairs (see below) and spiral channels which end as pores and allow for the passage of sweat (Fig. 7.3).
The epidermis may be described in five layers, though all layers are present only in thick skin, such as on the palms of the hand and soles of the feet.
■ Stratum corneum. This is the most superficial layer and consists of the protein keratin; no cells are present. In thick skin (Fig. 7.3) the keratin is in numerous layers; there is less keratin in thin skin (Fig. 7.2). Keratin is a filamentous protein produced by keratinocytes in deeper layers of the epidermis. It confers toughness and protection on the epidermis and helps to prevent water loss and dehydration of cells in the epidermis (and deeper). Some keratinocytes in deeper layers produce lipids which are added to the stratum corneum, and this increases the ability of skin to resist water absorption. The surface of the stratum corneum is constantly being shed, particularly if it is subjected to abrasion.
Importantly, the stratum corneum is constantly being added to as cells in the deeper layers move towards the surface at a rate which equals the rate at which the keratin is shed.
■ Stratum granulosum. This layer may be up to five cells deep, but in thin skin it may be absent. It is characterised by the presence of cytoplasmic granules of keratohyalin (Fig. 7.4). Other cytoplasmic granules contain lipids and these are released into extracellular spaces and confer waterproofing on the superficial layers of the epidermis. Upper cells in this stratum die and then become part of the stratum lucidum.
■ Stratum spinosum. This is the thickest layer of the epidermis, and is characterised by the presence of ‘prickle’ cells (Fig. 7.4). The angular appearance of these keratinocytes in sectioned material is due to the large number of desmosomes between adjacent keratinocytes, which are important in holding the cells together and resisting shearing forces. Increasing amounts of cytoplasmic keratin filaments are produced by keratinocytes in this layer. The uppermost cells in this layer develop keratohyalin granules, move towards the surface and become part of the stratum granulosum.
■ Stratum germinativum. This is the deepest layer of the epidermis and consists of cuboidal epithelial cells (Fig. 7.4). The basal cells in the stratum germinativum are attached to the basement membrane of the epidermis, which, in turn, is adjacent to the dermis. The cells in this stratum undergo mitosis and are the stem cells of the epidermis. Some offspring cells remain in this layer, undergo further mitotic activity, and thus continue as stem cells. Other offspring cells begin to produce keratin filaments and migrate towards the surface of the epidermis; this initially replaces the keratinocytes in the stratum spinosum. Over a period of about 30days, keratinocytes produced by mitosis in the stratum germinativum migrate towards the surface of skin, die and the keratin they have formed is shed.
Within the epidermis there are various cell types in addition to keratinocytes.
■ Merkel cells. These cells are scattered throughout the stratum germinativum and are thought to act as mechanoreceptors.
■ Langerhans cells. These cells are derived from bone marrow cells and they have an immunological function (Chapter 8). They are mainly located in the stratum spinosum.
■ Melanocytes. These cells produce pigment and are present in the stratum germinativum between the mitotically active cells. Melanin is responsible for giving skin a brownish colour and carotene for giving it a yellowish colour. The type and amount of pigment present is affected by the genetic make-up of the individual and, in the case of melanin, the amount of exposure to ultraviolet light (sunlight stimulates the synthesis and spread of melanin). Melanocytes have long cytoplasmic processes in which the melanin granules are present. They also pass melanin to keratinocytes. The melanin is often located in the cytoplasm of keratinocytes between the nucleus and the surface of the skin (Fig. 7.5); there, it helps protect DNA from damage by UV light.
Dermis
The dermis is derived from the mesoderm layer of the embryo and consists largely of connective tissue fibres and cells. Also present in the dermis are structures which may extend between the hypodermis and the epidermis, e.g. parts of developing hairs in hair follicles, sebaceous glands and sweat glands (see below). The dermis is divided into two layers, the papillary and the reticular layer.
■ Papillary layer. This is the most superficial layer and it interdigitates with the epidermis through a series of dermal ridges and papillae (Figs 7.2 and 7.3). In this way, the attachment of the epidermis and the dermis is strengthened. The papillary layer is characterised by loose connective tissue, including collagen, reticulin and elastin fibres and fibroblasts. There are also the transient cell types typical of connective tissue, e.g. white blood cells (Chapters 4 and 8). In the papillary region there are blood vessels that supply oxygen and nutrients to nearby cells, including epidermal cells, and that are also involved in temperature regulation. Some sensory nerve endings are present in the papillary region of the dermis.
■ Reticular layer. The reticular layer is deep to the papillary layer but the border between them is a gradual transition: it connects the skin to the underlying hypodermis. Dense, irregular connective tissue (Figs 7.2 and 7.3) containing many collagen fibres is predominant in the reticular layer. The transient cell population is less abundant in the reticular layer than in the papillary layer.
Glands of skin
Exocrine glands are present in skin. Some secrete sweat and are involved in temperature regulation. Others, sebaceous glands, secrete lipids and most are associated with hairs. In females, modified glands in the skin (mammary glands) are able to secrete milk in response to the hormones present during and after pregnancy (Chapter 16).
Sweat glands
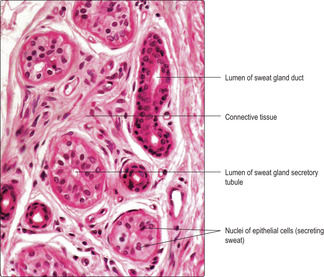
■ Merocrine sweat glands. These are present in skin (Figs 7.1 and 7.6) all over the body and they are simple, coiled tubular glands (Chapter 3). The secretory cells are located deep in the dermis, and even in the underlying hypodermis. An epithelial lined duct (Fig. 7.3) drains each gland and it passes to the superficial layer of the epidermis (stratum corneum). The duct is replaced by a spiral channel through the stratum corneum (Fig. 7.3) and opens at a pore on the surface of the skin. Merocrine sweat glands are innervated by sympathetic nerves and may be stimulated to secrete under conditions of stress, as well as in order to cool the body.
Myoepithelial cells surrounding the gland cells contract and assist in the expulsion of sweat.
■ Apocrine sweat glands. This type of sweat gland is present in the axilla, around nipples and in the anal region. The glands are larger than merocrine sweat glands, and they are located more deeply in the dermis and underlying hypodermis. Unlike merocrine glands, apocrine sweat glands do not secrete onto the surface of the skin; instead, they secrete around developing hairs in hair follicles. Secretion by apocrine sweat glands is influenced by sex hormones, and, after bacterial action, their secretions have a characteristic odour. It is thought that this odour may impart pheromone-like qualities to the secretion.
Sebaceous glands
■ Sebaceous glands (Figs 7.1 and 7.7) secrete a lipid-based substance known as sebum. They release their secretions by the holocrine method and as the cells die the sebum is released from the cytoplasm and empty spaces may be apparent in the gland. The activity of sebaceous glands is influenced by sex hormones and their secretory activity increases substantially after puberty. In areas where there are hairs, sebaceous glands secrete into the follicle of each hair (see below) and the sebum ‘conditions’ the hair. In locations where there are no hairs (e.g. the palms and soles) sebaceous glands open directly onto the surface of the skin and help maintain its texture and condition.
Hair follicles
Hair is formed largely of a compact, dense form of keratin. Each hair is produced in a structure known as a hair follicle (Fig. 7.1). Hairs are widespread over the body surface though they are absent from the palms, soles, parts of the genitalia, tips of fingers and toes, and lips. Hairs are of two types: vellus hairs, which are the short, fine, soft hairs on the skin, and terminal hairs, which are the long hairs such as on the scalp. Hairs may be coloured, e.g. by the presence of a pigment such as melanin.
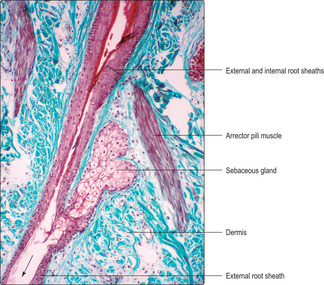
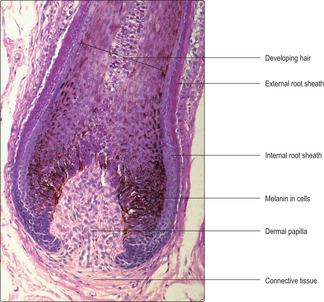
Hair follicles develop as cylindrical invaginations of the epidermis and they extend into the dermis and, in some instances, also into the hypodermis. Straight hair grows from straight follicles, and spiralling follicles give rise to curly hairs. Hair follicles are surrounded by connective tissue (Fig. 7.8). During the growing phase of a hair the base of its follicle is expanded into a bulbous portion (Figs 7.8 and 7.9). Cell proliferation in the epidermal-like cells of the bulb produces a variety of cells. Some of these cells form part of the follicle and move towards the surface and others, centrally placed, form the hair which grows out from the follicle. Pigment such as melanin in cells in this region (Fig. 7.9) affect the colour of the hair. Each hair bulb is invaginated by a dermal papilla of connective tissue (Fig. 7.9) containing blood vessels which are essential for hair growth.
Each hair follicle is lined by layers of cells similar to epidermal cells, and by cells produced by mitosis of cells in the hair bulb. The outer layers of epidermal-like cells are known as the external root sheath (Figs 7.1 and 7.9). An inner sheath, formed by cells produced in the hair bulb, extends only part way along the follicle. It is the innermost cells within the inner sheath which undergo keratinisation and form the hair shaft. At the region where the inner sheath stops, secretions from sebaceous glands drain into the follicle (Fig. 7.7) and coat the hair as it grows out of the follicle.
Hair growth is cyclical. Growth in length usually occurs for several years and then the follicle enters a rest phase when mitosis in the bulb region stops and the bulb shrinks in size. In the rest phase, the hair eventually falls out of the follicle and, after several weeks, mitosis in the bulb begins and this new growth phase produces another hair.
Muscles, nerves and blood vessels in the dermis and hypodermis
Smooth muscle cells, known as arrectores pilorum, are associated with hair follicles and their sebaceous glands (Figs 7.1 and 7.7). The muscle cells lie obliquely and attach the hair follicle to connective tissue in the dermis. Sympathetic nerves stimulate contraction of these smooth muscle cells and this causes hairs to ‘stand on end’. Sympathetic nerves also supply sweat glands and the smooth muscle cells in the walls of blood vessels in the skin. The flow of blood through vessels in skin and the amount of sweat secreted varies, particularly as a means of maintaining body temperature by varying heat loss from the body. Other nerves in skin transmit sensory information to the CNS. There are several types of nerve ending in skin that may be distinguished by their morphology and these include free nerve endings, Pacinian corpuscles, Meissner’s corpuscles and Merkel cells. The free nerve endings detect pain and temperature changes. Pacinian corpuscles (Chapter 6, Fig. 6.11) have a characteristic lamellated appearance enclosing a central nerve ending and they detect pressure changes. Meissner’s corpuscles are located in dermal papillae and detect touch. Merkel cells also detect touch and are located in the epidermis.
Age With age, numerous changes occur in skin. In particular, elastin fibres disappear so the skin loses the ability to recoil after being stretched. The epidermis becomes thinner with age and less able to withstand trauma.
Tumours Tumours of the skin may be benign or malignant. Of the benign tumours, warts (papillomata) are common. Warts occur at any site, and are simple proliferations of epidermal cells resulting from infection of the keratinocytes with a papilloma virus. Basal cell carcinomas of skin are common neoplasms which rarely spread to distant sites. However, they spread into the dermis and can cause damage in the local region. Of all the skin tumours the most malignant are malignant melanomas (neoplasms of melanocytes) and they often have fatal consequences.
Skin:
■ is an organ covering the body and consists of epidermis and dermis
■ is involved in protection against physical trauma, dehydration, ultraviolet light, harmful molecules and microorganisms
■ aids control of body temperature
■ by secretion of sweat and variation in blood flow through blood vessels near the surface of the skin
■ has sensory nerve receptors
■ is involved in producing vitamin D.
The epidermis is a stratified, squamous, keratinised epithelium:
■ the basal layer of cells (keratinocytes) act as stem cells
■ keratinocytes move from the basal layer, differentiate, make keratin and die, and keratin is shed
■ other cells in the epithelium make pigment, others are involved in immune responses.
The dermis consists mainly of connective tissue cells and fibres:
■ it has a papillary layer adjacent to the epidermis and a denser, reticular layer adjacent to the hypodermis.
Sweat glands (in most regions of the body):
■ consist of secretory cells lining coiled tubes in the dermis or hypodermis
■ secrete sweat by the merocrine method under the influence of sympathetic nerves and aid the regulation of body temperature.
Sebaceous glands synthesise and secrete lipids forming sebum:
■ secretion occurs by the holocrine method and is affected by sex hormones
■ most secretions coat developing hairs.
Hair:
■ is a compact, dense form of keratin and develops in a hair follicle
■ follicles extend between the surface of skin and the dermis or hypodermis
■ actively growing hair follicles have mitotically active cells at the base
■ cells move from the base towards the skin surface, some form the hair
■ smooth muscle attached to hair follicles, under control of sympathetic nerves, can make hairs ‘stand on end’.