Chapter 5. The shoulder
CHAPTER CONTENTS
Summary87
SUMMARY
Knowledge of anatomy and the use of selective tension aid the incrimination of the causative structure. Palpation then identifies the specific site of the lesion to which effective treatment can be applied. The orthopaedic medicine treatment techniques discussed below should be integrated into clinical practice alongside techniques drawn from other modalities; the importance of addressing the cause as well as the symptoms cannot be stressed enough.
This chapter outlines the relevant anatomy of the shoulder region with guidelines for palpation. The assessment procedure follows, incorporating the pertinent elements of thesubjective and objective examination towards the identification of shoulder lesions. The lesions are discussed and treatments are suggested, based on the principles of theory and practice.
ANATOMY
Inert structures
In the shoulder region, simultaneous coordinated movements occur at four articulations between the scapula, clavicle, humerus and sternum: the glenohumeral joint, acromioclavicular joint, sternoclavicular joint and scapulothoracic joint. The glenohumeral joint (shoulder joint) is the most mobile joint in the body and is the first link in a mechanical chain of levers that allows the arm to be positioned in space. The joint is inherently unstable and it relies more on its surrounding muscles for stability than on the shape of its joint surfaces and ligamentous constraints. Movement at the spinal joints increases the range of movement available to the glenohumeral joint (Nordin & Frankel 2001).
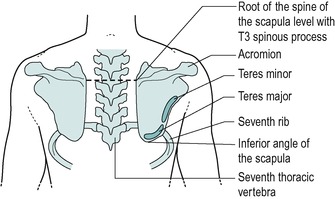
The large, flat scapula is suspended by its muscles against the posterolateral thoracic wall and overlies the second to seventh ribs in the neutral position. It is attached to the strut-like clavicle by the acromioclavicular joint and together they position, steady and brace the shoulder laterally, so that the arm can clear the trunk. The clavicle transmits the weight of the upper limb to the axial skeleton via the coracoclavicular and costoclavicular ligaments, and the glenohumeral joint provides the upper limb with its wide range of movement.
The inferior junction of the medial and lateral borders of the scapula forms the inferior angle, which lies over the seventh rib and is crossed by latissimus dorsi. The lateral border provides the origins of teres major below and teres minor above. The medial border is long, providing attachment for the levator scapulae and the rhomboid muscles; it joins the short superior border at the superior angle. The suprascapular notch lies at the junction of the superior border with the coracoid process. This notch is converted by the superior transverse scapular ligament into a foramen for the passage of the suprascapular nerve. The suprascapular vessels pass above it.
The dorsal surface of the scapula is divided by the spine of the scapula into fossae above and below. The smaller upper supraspinous fossa gives origin to the supraspinatus muscle and the lower, larger infraspinous fossa gives origin to infraspinatus. The two fossae communicate laterally at the spinoglenoid notch through which runs the suprascapular nerve. The costal surface shows a slight hollowing for the origin of subscapularis and its medial border is roughened for the insertion of serratus anterior.
The lateral angle of the scapula is broadened to form the pear-shaped glenoid fossa that articulates with the head of the humerus at the glenohumeral joint. A roughened supraglenoid tubercle gives origin to the long head of biceps and a roughened infraglenoid tubercle gives origin to the long head of triceps.
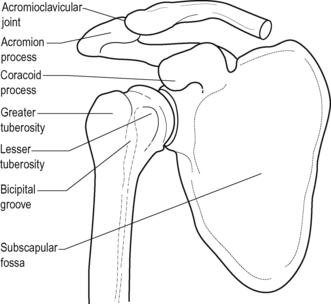
The spine of the scapula is subcutaneous and, having arisen from the upper dorsal surface of the scapula, it widens laterally, projecting forwards to form the distinctive acromion process. When the acromion is viewed laterally it may be observed to be flat, slightly curved or to have an anterior hook-like process. The last two may predispose to rotator cuff pathology since they reduce the vertical dimensions of the subacromial space (Flatow et al 1994, Pratt 1994, Hulstyn & Fadale 1995).
The lower border of the crest of the spine of the scapula is continuous with the lateral border of the acromion and forms a useful palpable bony landmark: the posterior angle of the acromion. The anteromedial border of the acromion shows an oval facet for articulation with the clavicle at the acromioclavicular joint.
Just above the glenoid fossa, the prominent hook-like coracoid process springs up and forwards to lie below the outer clavicle. With the arm in the anatomical position, the coracoid points directly forwards to form a prominent palpable bony landmark.
The clavicle is subcutaneous, running horizontally between the acromion process of the scapula and the manubrium sterni, with which it articulates. On its lateral aspect is a small oval facet that articulates with the acromion at the acromioclavicular joint.
Inferiorly and laterally is a rounded conoid tubercle from which a roughened trapezoid line runs forwards and laterally. Both give attachment to the separate parts of the coracoclavicular ligament, which firmly fastens the clavicle to the scapula via the coracoid process.
The upper part of the humerus expands to bear a head and the greater and lesser tuberosities. The head of the humerus is approximately hemispherical and provides an articulating surface that is much greater than its scapular counterpart, the glenoid fossa. Surrounding the head of the humerus is a slight constriction that represents the anatomical neck and separates the head from the two tuberosities. The head of the humerus joins the shaft at the surgical neck, so called because it is the common site of fracture of the humerus.
The greater tuberosity is large and quadrilateral and is the most lateral palpable bony landmark at the shoulder. Projecting laterally beyond the acromion, it is covered by the deltoid muscle and is continuous with the shaft of the humerus below. Three articular facets sit on its superior and posterior surface for the attachment of supraspinatus, infraspinatus and teres minor. Supraspinatus inserts into the highest or superior facet, infraspinatus into the middle and teres minor into the lower or inferior facet. In reality these tendons are not separate, but together with subscapularis they interdigitate at their insertions to form a fibrous thickening of the capsule, the rotator cuff. The sharp medial edge of the greater tuberosity forms the lateral lip of the bicipital groove ( intertubercular sulcus) which receives the insertion of pectoralis major.
The lesser tuberosity is a bony projection that lies below and lateral to the coracoid process. It receives the insertion of subscapularis on its medial aspect and its sharp lateral edge forms the medial lip of the bicipital groove which receives the insertion of teres major.
The sternoclavicular joint is a synovial joint between the medial end of the clavicle and a notch on the supero-lateral aspect of the manubrium sterni. A fibrocartilaginous disc is positioned between the joint surfaces. It is an important joint since it is the point of attachment of the upper limb to the axial skeleton.
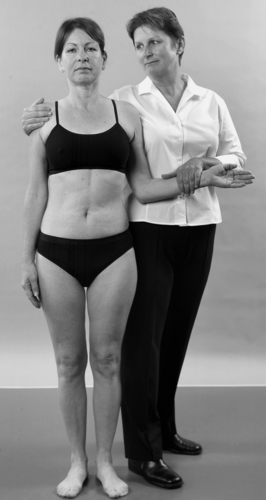
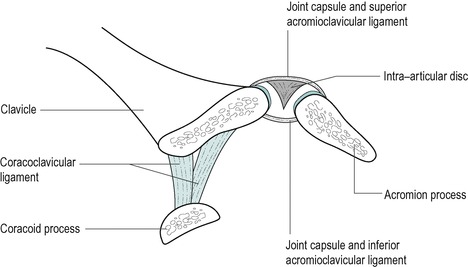
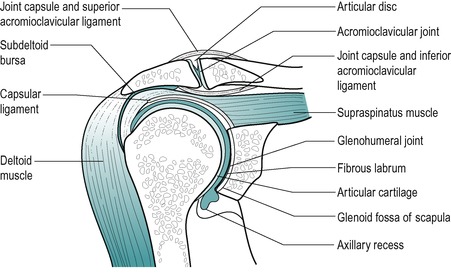
The acromioclavicular joint is a synovial plane joint with its articular surfaces covered with fibrocartilage. A wedge-shaped fibrocartilaginous disc drops down into the joint from the superior aspect of the joint capsule, producing a partial division of the joint. The articular facet on the lateral aspect of the clavicle is directed inferolaterally and the corresponding facet on the medial border of the acromion is directed superomedially, producing a tendency for the clavicle to override the acromion. The plane of the joint tends to be variable, but may run slightly obliquely, sloping medially from superior to inferior. The joint is surrounded by a fibrous capsule that is thickened superiorly and inferiorly by the parallel fibres of the capsular ligaments running between the two bones (Fig. 5.1). The stability of the acromioclavicular joint is provided by the strong accessory coracoclavicular ligament.
 |
| Figure 5.1
Acromioclavicular joint, showing intra-articular disc and ligaments.
From Anatomy and Human Movement by Palastanga N, Field D and Soames R 2006. Reprinted by permission of Elsevier Ltd.
|
The clavicle acts as a strut or brace and allows the scapula to rotate and glide forwards and backwards. The movements at the acromioclavicular joint are passive, in the same way as those of the sacroiliac joint. The small amounts of movement available make it impossible to determine a capsular pattern, although as a synovial joint it can be affected by arthritis.
The coracoclavicular ligament is separate from the acromioclavicular joint, but in strongly binding the scapula to the clavicle via the coracoid process it provides a stabilizing component to the joint. The ligament has two parts, the trapezoid and conoid ligaments, which are separate anatomically and functionally. The more horizontal trapezoid ligament acts as a hinge for scapular motion, while the more vertical conoid ligament acts as a longitudinal axis for scapular rotation. Together, the ligaments prevent medial displacement of the acromion under the clavicle.
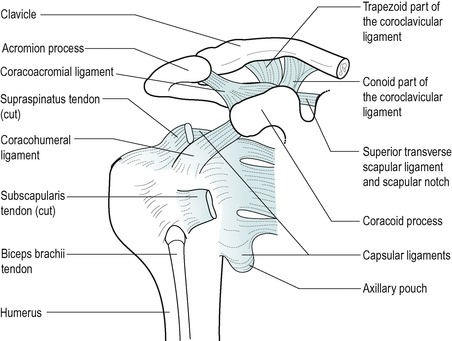
The glenohumeral joint is a synovial ball-and-socket joint between the head of the humerus and the glenoid fossa of the scapula, deepened by the fibrocartilaginous glenoid labrum (Fig. 5.2). The two articular surfaces are incongruent, with the relatively large head of the humerus providing a surface area three to four times that of the glenoid fossa (Hulstyn & Fadale 1995). The enormous range of movement is therefore at the expense of joint stability. With no inherent bony stability available, stability is dependent primarily upon the static effects of the capsuloligamentous structures and the dynamic effects of the surrounding muscles. The limited joint volume and a negative intra-articular pressure provide a form of static stability. The action of muscle forces, mainly the rotator cuff, produces compression of the head of the humerus into the glenoid labrum, providing important dynamic stability and steering the joint surfaces during movement (Speer 1995).
 |
| Figure 5.2
Cross-section of glenohumeral joint showing internal structure.
From Anatomy and Human Movement by Palastanga N, Field D and Soames R 2006. Reprinted by permission of Elsevier Ltd.
|
The joint capsule, lined with synovium, is thin and spacious, with a large volume, normally of between 15 and 30 mL (Cailliet 1991, Halder & An 2000). It attaches to the edge of the glenoid medially and surrounds the anatomical neck of the humerus laterally, except for its inferomedial part that descends to attach to the shaft of the humerus, approximately 1 cm below the articular margin. The inferomedial portion forms a loose axillary pouch or fold and consists of randomly organized collagen fibres (Hulstyn & Fadale 1995). Although this arrangement facilitates movement, this part of the capsule is relatively weak, as it is not supported by muscles, and is often subject to strain.
The capsular fibres are mainly horizontal and are reinforced anteriorly by three capsular ligaments, the superior, middle and inferior glenohumeral ligaments, which are evident only on the interior aspect of the capsule (Fig. 5.3). The three bands together form a Z-shape reinforcement to the anterior capsule (Kapandji 1982). The inferior glenohumeral ligament complex plays a major stabilizing role in supporting the humeral head in a hammock or broad sling, particularly during abduction (Hulstyn & Fadale 1995, Speer 1995). All three bands of the glenohumeral ligaments are taut in lateral rotation, and abduction stresses the middle and inferior bands. This may be significant in the development of the capsular pattern of the shoulder joint.
 |
| Figure 5.3
External aspect of glenohumeral joint showing axillary pouch and capsular ligaments.
|
The rotator cuff muscles (supraspinatus, infraspinatus, teres minor and subscapularis) act as extensible ligaments to support the capsule, assisted by the long heads of triceps and biceps. Much of the capsule is less than 1 mm thick, but it is thickened to between 1 and 2 mm near its humeral attachment where it receives the rotator cuff tendon fibres (Hulstyn & Fadale 1995). The rotator interval is a fibrous gap between the supraspinatus and subscapularis tendons and is therefore part of the rotator cuff. It is composed of fibres from supraspinatus and subscapularis together with the coracohumeral ligament, the superior glenohumeral ligament and parts of the capsule.
The key structure of the interval is the coracohumeral ligament, which attaches between the dorsolateral aspect of the base of the coracoid and the greater, and to some extent the lesser, tuberosities. It would seem to be important for inferior stability of the glenohumeral joint and in limiting lateral rotation (Jost et al 2000), possibly contributing to the capsular pattern if the interval becomes reduced.
The wide range of movement available at the glenohumeral joint consists of flexion, extension, abduction, adduction, medial and lateral rotation that all combine to allow circumduction. The range of elevation may be up to 180° and may occur through flexion in the sagittal plane, or abduction through the coronal plane. The most functional movement is abduction in the plane of the scapula, known as scaption. This is not a fixed plane but occurs 30–40° anterior to the coronal plane of the humerus (Frame 1991). It places deltoid and supraspinatus in an optimal position to elevate the arm (Nordin & Frankel 2001). Abduction is accompanied by lateral rotation in the coronal plane which allows the greater tuberosity to clear the acromion; scaption does not involve this element of concomitant lateral rotation (Frame 1991).
Active elevation consists of abduction from 0–60° occurring at the glenohumeral joint, 60–120° occurring at the scapulothoracic joint and 120–180° occurring at the glenohumeral and scapulothoracic joints together with side flexion of the trunk to the opposite side (Kapandji 1982). Approximately 90° of passive glenohumeral abduction is achieved with the inferior angle of the scapula fixed. The range of lateral rotation is 80–90° and medial rotation 100–110°, with full range achieved only by taking the arm behind the back.
Rolling and translational (gliding) movements also occur and the glenohumeral joint surfaces can be separated by distraction. Muscle forces acting on the joint stabilize it and produce a combination of shearing and compression forces, maintaining the humeral head in the glenoid fossa.
The nerve supply to the glenohumeral joint is mainly from the C5 segment.
Cameron (1995) looked at the shoulder as a weight-bearing joint. Although this joint is traditionally considered to be non-weight-bearing in character, he applied simple physical principles showing this not to be the case. With the weight of the adult arm estimated to be approximately 5 kg, forces equivalent to three times body weight are transmitted through the shoulder during simple daily activities.
The coracoacromial ligament is an accessory ligament of the shoulder joint, forming an osseoligamentous arch over the superior aspect of the shoulder joint and the subacromial bursa. It is triangular in shape and approximately 1 cm wide. Its apex attaches to the anterior aspect of the acromion and its base to the lateral aspect of the coracoid process. The coracoacromial arch is separated from the underlying tendons by the subacromial bursa. The coracoacromial ligament is unusual in that it attaches to two parts of the same bone, probably functioning as a buffer; it provides stability for the head of the humerus against upwards displacement and protects it from direct vertical trauma (Petersilge et al 1997).
Numerous small bursae are associated with the shoulder joint. An anterior subscapular bursa lies between the tendon of subscapularis and the anterior capsule, consistently communicating with the joint. The synovial lining of the joint extends to form a sheath around the long head of biceps in the bicipital groove. A bursa, which communicates with the joint, may be present between the tendon of infraspinatus and the posterior capsule.
The subacromial bursa is independent of the shoulder joint and normally does not communicate with it. It was described by Codman in 1934 as the largest and most complicated bursa in the body forming a secondary scapulohumeral joint (Beals et al 1998). It therefore has a special role in the biomechanics of the shoulder joint and is frequently a cause of pain. It is a smooth synovial sac containing variable thin bands or plicae and is surrounded by fatty areolar tissue (Hulstyn & Fadale 1995). Beals et al (1998) identified by cadaver studies that only the anterior half of the under-surface of the acromion is contained within the subacromial bursal cavity, which may have implications for injection of the subacromial bursa, particularly if a posterior approach is used. Its deep layer lies over the rotator cuff tendons and the head of the humerus (Cooper et al 1993). Medially it extends under the acromion to the acromioclavicular joint line and laterally it caps the greater tuberosity, separating it from the overlying deltoid muscle.
The subacromial space is sometimes considered to be a joint (Kapandji 1982, Pratt 1994). This is not a true articulation but it is critical to shoulder movement. As supraspinatus pulls the greater tuberosity superiorly and medially, the walls of the subacromial bursa glide over one another allowing the head of the humerus to slide (Netter 1987). The subacromial space is approximately 7–14 mm deep (Frame 1991) and is occupied by the subacromial bursa, the supraspinatus tendon, the superior part of the capsule of the shoulder joint and the tendon of the long head of biceps. The tightly packed structures move constantly in relation to one another and there is the potential for friction and degeneration. Inflammation, degeneration, the shape of the acromion or degeneration of the acromioclavicular joint can all contribute to a reduction of the vertical proportions or stenosis of the subacromial space. Impingement of a painful structure in the space may produce a painful arc between 60 and 120° of abduction.
Contractile structures
Four short muscles (supraspinatus, infraspinatus, teres minor and subscapularis) pass from the scapula to the head of the humerus and these are known as the rotator cuff. The rotator cuff muscles are particularly important to the function of the shoulder, working together as extensible ligaments to provide dynamic stability, maintaining and centralizing the head of the humerus in the glenoid fossa. Shoulder movement, particularly elevation, is governed by force couples that involve the interaction of deltoid and the rotator cuff muscles (Nordin & Frankel 2001). The rotator cuff muscles maintain the joint’s apposition, preventing excessive superior translatory movement that would lead to instability.
As the rotator cuff tendons insert into the head of the humerus they blend with the capsule of the joint forming a thickened common tendinous cuff. Fibres from subscapularis and infraspinatus interdigitate with those of supraspinatus in their deep layer, facilitating the distribution of forces directly or indirectly over a wider area (Clark & Harryman 1992). The tendon of the long head of biceps exits the capsule through a reinforced foramen at the junction of the insertions of supraspinatus and subscapularis onto the humerus (Hulstyn & Fadale 1995). These tendons are frequently a source of pain through degeneration and overuse.
Supraspinatus (suprascapular nerve C4–C6) takes origin from the medial two-thirds of the suprascapular fossa. The fibres, which are bipennate, converge to pass under the acromion, blending with the capsule of the shoulder joint and adjacent tendon fibres of subscapularis and infraspinatus, inserting mainly into the upper of the three facets on the greater tuberosity. As the tendon passes to its insertion it appears to be reinforced by the coracohumeral ligament that runs parallel and is firmly adherent to it (Clark & Harryman 1992). Supraspinatus produces abduction of the glenohumeral joint but its exact role in the mechanism of shoulder movement is controversial.
Supraspinatus, together with the other rotator cuff muscles, stabilizes the head of the humerus, providing horizontal compression and reducing vertical displacement. It is considered to be responsible for initiating abduction by holding the head of the humerus down on the glenoid, before deltoid takes over at approximately 20°, to provide the force for abduction (Pratt 1994, Palastanga et al 2006). However, both supraspinatus and deltoid have been shown to be active throughout the range of abduction with an early rise in tension in supraspinatus fixing the humeral head, and enabling deltoid to work at a better mechanical advantage (Cailliet 1991, Frame 1991). It may be that deltoid and supraspinatus can initiate and complete a full range of abduction independently.
Infraspinatus (suprascapular nerve C4–C6) is a thick triangular muscle that takes origin from the medial two-thirds of the infraspinous fossa. Its fibres converge to form a broad, thick tendon, passing over the posterior joint capsule, with which it blends, and inserting into the middle of the three facets on the greater tuberosity of the humerus, some of its fibres interdigitating with the adjacent supraspinatus. Together with teres minor, with which it is sometimes fused, infraspinatus produces lateral rotation of the glenohumeral joint during elevation.
Teres minor (axillary nerve C5–C6) takes origin from the upper two-thirds of the lateral border of the scapula, above the origin of teres major. It inserts into the lowest of the three facets on the posterior aspect of the greater tuberosity blending with the posterior capsule as it passes over it. It functions with infraspinatus to produce lateral rotation of the glenohumeral joint.
Subscapularis (upper and lower subscapular nerve C5–C6) takes origin from the medial two-thirds of the subscapular fossa on the costal surface of the scapula, and inserts by a broad, thin, membranous tendon into the lesser tuberosity of the humerus. It reinforces the anterior capsule, from which it is partially separated by a bursa which communicates with the joint. It functions to produce medial rotation of the glenohumeral joint. Fibres from subscapularis and supraspinatus blend together to contribute to the rotator interval (see above).
Trapezius (spinal accessory nerve, XI and ventral rami of C3–C4) is a large, flat triangular muscle forming a trapezium with its opposite number. It has a long line of attachment from the superior nuchal line, external occipital protruberance, ligamentum nuchae and the spinous processes and intervening supraspinous ligament from C7 to T12. The upper fibres descend to the posterior border of the lateral third of the clavicle, the middle fibres pass horizontally to the medial border of the acromion and the lower fibres pass upwards to the crest of the spine of the scapula. In conjunction with other muscles, trapezius stabilizes the scapula for functional movement of the arm and the individual portions of the muscle assist other muscles in producing primary movement. The upper fibres of trapezius and levator scapulae suspend the scapula against the thoracic cage and are constantly active during ambulation (Paine & Voight 1993). Trapezius, together with serratus anterior, forms a force couple to rotate the scapula on the thoracic wall (Frame 1991).
Rhomboids, major and minor (rhomboid branch of the dorsal scapular nerve, C4–C5), form a line of attachment from the lower ligamentum nuchae and the spines of C7 to T5 and pass to the medial border of the scapula, to assist in its stabilization against the thoracic cage. The rhomboids are active in scapular retraction, which is essential for overhead throwing movements and swimming strokes, e.g. crawl (Paine & Voight 1993).
Levator scapulae (C3–C5) descends from the transverse processes of the atlas and axis to the medial upper scapular border. Together with the rhomboids it controls and positions the scapula.
Latissimus dorsi (thoracodorsal nerve C6–C8) has an extensive origin from the lumbar spine, thoraco-lumbar fascia and thorax. The fibres converge towards the humerus, attaching to the inferior angle of the scapula as they pass by. The tendinous fibres twist through an angle of 180° before inserting into the floor of the bicipital groove. At the shoulder latissimus dorsi extends, adducts and medially rotates the humerus.
Teres major (lower subscapular nerve, C6–C7) passes from the lower dorsal aspect of the scapula near the inferior angle to insert into the medial lip of the bicipital groove. It functions together with latissimus dorsi to adduct and medially rotate the humerus and together they form the posterior fold of the axilla. In conjunction with pectoralis major, teres major stabilizes the shoulder joint.
Deltoid (axillary nerve C5–C6) gives the shoulder its rounded contour. The muscle has three sets of fibres which all converge to insert into the deltoid tubercle in the middle of the lateral aspect of the shaft of the upper humerus. The anterior fibres attach to the anterior border of the lateral third of the clavicle and assist flexion and medial rotation. The middle fibres attach to the acromion, assisting abduction, and the posterior fibres attach to the lower lip of the crest of the spine of the scapula assisting extension and lateral rotation. The direction of the muscle fibres is almost vertical and the muscle’s basic action is to elevate the head of the humerus up into the overhanging coracoacromial arch (Cailliet 1991). Overall, deltoid is a powerful abductor of the glenohumeral joint but its function is dependent on supraspinatus and the other rotator cuff muscles.
Pectoralis major (lateral and medial pectoral nerves, clavicular part C5–C6, sternocostal part C7–C8, T1) is a thick triangular muscle, originating as two separate parts from the anterior chest wall to insert into the lateral lip of the bicipital groove. As the fibres cross to the arm they twist to form the anterior axillary fold. The two parts of the muscle are both powerful adductors and medial rotators of the humerus; the clavicular part produces flexion. Together with latissimus dorsi, pectoralis major acts in climbing activities and is involved in pushing and throwing.
Pectoralis minor (both pectoral nerves, C6–C8) passes from the upper ribs to the coracoid process. In conjunction with other muscles that anchor the scapula, pectoralis minor protracts, depresses, rotates and tilts the scapula.
Serratus anterior (long thoracic nerve C5–C7, descending on its external surface) has an extensive origin from the side of the thorax, passing round the thoracic cage to insert into the medial border of the costal surface of the scapula. It is responsible for stabilizing the scapula during elevation and protraction of the scapula in the functional activities of reaching and pushing. Loss of its nerve supply leads to winging of the scapula.
Movement of the scapula on the thoracic cage occurs at the scapulothoracic joint between two fascial planes, the most superficial of which lies between subscapularis and serratus anterior (Kapandji 1982, Pratt 1994). The surrounding muscles stabilize this joint and dynamically position the glenoid fossa to facilitate efficient glenohumeral movement (Paine & Voight 1993).
Coracobrachialis (musculocutaneous nerve C5–C7) originates from the tip of the coracoid process, where it forms a conjoint tendon with the short head of the biceps, and inserts into the medial aspect of the middle of the shaft of the humerus. It adducts the humerus, its position being analogous to the adductor group of muscles at the hip.
Biceps brachii (musculocutaneous nerve C5–C6) has a short head arising from the tip of the coracoid process and a long head originating within the capsule of the glenohumeral joint from the supraglenoid tubercle and adjacent glenoid labrum. The intracapsular part of the tendon is surrounded by a double sheath, an extension of the synovial lining of the glenohumeral joint (Standring 2009). The long head passes through the subacromial space and exits the joint behind the transverse humeral ligament, emerging between the insertions of supraspinatus and subscapularis. It continues on into the bicipital groove together with its synovial sheath. The two muscle bellies fuse to insert into the tuberosity of the radius via the biceps tendon. Biceps has its main effect at the elbow where it is a powerful supinator and elbow flexor. The long head exerts a stabilizing effect on the superior aspect of the shoulder joint, which may be important if the shoulder becomes less stable (Itoi et al 1994). Its passage laterally, then turning a 90° angle into the bicipital groove, assists forward flexion of the shoulder (Cailliet 1991).
Triceps (radial nerve C6–C8) originates by three heads. The long head arises from the infraglenoid tubercle of the scapula and the glenoid labrum, where it exerts a stabilizing effect on the shoulder joint. It also assists adduction and extension movements of the humerus from the flexed position. The lateral head originates from the humerus above and lateral to the spiral groove, and the medial head from the posterior humerus below the spiral groove. The three heads come together to insert into the olecranon process. The main action of the triceps is to extend the elbow.
GUIDE TO SURFACE MARKING AND PALPATION
Posterior aspect (Fig. 5.4)
Palpate the inferior angle of the scapula which, in most people, can be grasped between a finger and thumb. Abducting the arm may make the inferior angle easier to locate as it advances around the chest wall.
 |
| Figure 5.4
Posterior aspect of the shoulder.
|
Palpate along the medial and lateral borders of the scapula. The lower medial border is subcutaneous and more readily palpable, lying parallel to and approximately three fingers’ width from the spinous processes. Visualize the position of latissimus dorsi as it crosses the inferior angle, and track the teres major and minor muscles that take origin from the lateral border of the scapula. Teres major originates below teres minor.
The crest of the spine of the scapula may be visible and is readily palpable. Feel it sloping medially down to meet the medial border of the scapula at the level of the spinous process of T3.
Palpate the lateral end of the spine of the scapula and follow the lower border round until it joins the lateral border of the acromion. A sharp 90° angle is formed here, the posterior angle of the acromion, which is a useful bony landmark.
Palpate the flat upper surface of the acromion which is subcutaneous and forms the summit of the shoulder, lying just lateral to the acromioclavicular joint. Palpate the anterior edge of the acromion with an index finger and the posterior angle with a thumb, to appreciate its width.
Lateral aspect
Palpate the lateral edge of the acromion. Note its depth and visualize the position of the subacromial bursa beneath it. Follow the anterior and posterior portions of the deltoid muscle down on to its insertion into the deltoid tubercle.
Anterior aspect (Fig. 5.5)
Palpate the clavicle; it is usually visible and palpable throughout its length in most people. Start at the medial end and follow the anterior curve as it lies over the first rib, then the reverse curve that produces a hollow at the lateral end of the clavicle. Below this hollow, between deltoid and pectoralis major, lies the infraclavicular fossa.
 |
| Figure 5.5
Anterior aspect of the shoulder.
|
Palpate the acromioclavicular joint line that lies between 1–2 cm, or approximately a finger’s width, medial to the lateral border of the acromion. The clavicular end of the joint may project a little higher than the acromion since it overrides it slightly, and this may produce a slight step down between the clavicle and acromion. If this is not obvious, palpate laterally along the anterior surface of the clavicle until a small, V-shaped depression is found that indicates the anterior joint line. It may also be found by palpating medially, approximately one finger’s width inwards from the lateral border of the acromion. Once identified, the joint line should be palpable from above. Apply a downwards pressure on the lateral end of the clavicle and ask the model (or patient) to flex and extend the shoulder to feel movement at the joint. Palpate the anterior edge of the acromion.
Below the junction of the lateral third and the medial two-thirds of the clavicle, in the lateral infraclavicular fossa, feel the prominent coracoid process which forms an anterior projection when the arm is resting at the side. This is covered by the anterior deltoid and deep palpation – which may be uncomfortable – is necessary. With a finger on the coracoid process, abduct the arm and the coracoid should move out from under your palpating finger.
Moving slightly downwards and laterally from the coracoid process, palpate the lesser tuberosity of the humerus. Immediately lateral to it is the bicipital groove and further laterally still the greater tuberosity should be palpable.
Place the arm in the anatomical position and feel the greater tuberosity lying laterally and the lesser tuberosity lying anteriorly on either side of the bicipital groove. Relax the arm, allowing it to fall into the more functional position with some medial rotation, and feel the greater tuberosity lying more anteriorly and the lesser tuberosity medially.
The greater tuberosity can be easily located as it lies in line with and above the lateral epicondyle of the humerus. It can be grasped with the thumb, index and middle fingers placed on its anterior, superior and posterior surfaces. Note its width. The greater tuberosity is slightly wider from anterior to posterior than the acromion process. Try to visualize its three facets for the insertions of supraspinatus, infraspinatus and teres minor.
Palpation of the insertions of the rotator cuff tendons
To palpate supraspinatus, the greater tuberosity must be brought forwards from under the acromion to expose its superior facet. Position the patient sitting up at an angle of about 45° against the couch. Medially rotate and extend the arm to position it behind the back. Palpate for the anterior edge of the acromion and locate the greater tuberosity. The tendon of supraspinatus is running directly forwards between the two bony points, roughly in line with the position of a shoulder strap (remember that you have turned the greater tuberosity to lie more anteriorly). The tendon of insertion is approximately one finger’s width (Fig. 5.6).
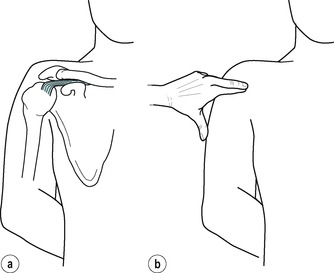 |
| Figure 5.6
Position of arm for palpation of the supraspinatus tendon.
|
To palpate infraspinatus, the greater tuberosity must be brought backwards from under the acromion to expose its middle facet. Position the patient in side-lying with the head raised on two pillows (or one folded). Rest the patient’s hand on the cheek, or on the pillow alongside the face. The forearm should be free to allow the elbow to drop to produce adduction and lateral rotation at the shoulder (Fig. 5.7). Palpate for the posterior angle of the acromion and locate the greater tuberosity. The tendon of infraspinatus runs parallel to the spine of the scapula to insert into the greater tuberosity, immediately below the posterior angle of the acromion. The tendon of insertion is approximately two fingers wide. Together with the insertion of teres minor the tendon is three fingers wide.
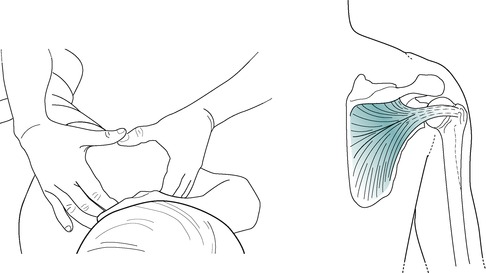 |
| Figure 5.7
Position of arm for palpation of the infraspinatus tendon.
|
To locate subscapularis, position the arm with the humerus in the anatomical position. Either palpate the coracoid process and move laterally and slightly downwards, or identify the bicipital groove and move directly medially to find the sharp lateral lip of the lesser tuberosity (Fig. 5.8). Follow round onto the medial aspect of the lesser tuberosity to locate the insertion of subscapularis. The tendon itself cannot be felt and the underlying bone is tender to palpation. The tendon is approximately three fingers wide.
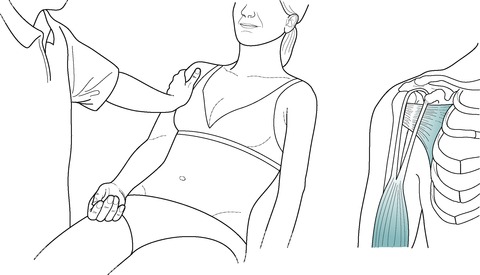 |
| Figure 5.8
Position of arm for palpation of the subscapularis tendon.
|
COMMENTARY ON THE EXAMINATION
The history at the shoulder is important, although it probably will not reveal a conclusive diagnosis. Cyriax (1982) considered the shoulder to be an ‘honest’ joint but most clues are related to the anatomy at the shoulder and are revealed in the objective examination rather than in the patient’s account. Lesions may be complicated and due to a contribution of several factors. For instance, pain tends to cause immobility and it is not uncommon to find a secondary capsulitis accompanying bursitis or tendinopathy.
Observation
A general observation of the patient’s face, posture and gait will alert the examiner to abnormalities and serious illness. Acute subacromial bursitis produces a constant acute pain that disturbs sleep and the patient looks tired.
The acute shoulder is usually held in a position of comfort, i.e. medially rotated with the elbow flexed and supported. An alteration in the rhythmical arm swing may be obvious. The head of the humerus is so positioned in the glenoid that functional movements tend to occur in diagonal patterns and this should be evident in the arm swing during gait activity.
Due to the many anatomical components that make up the shoulder region and the interrelationship between the function of each group, lesions can be subtly complicated. Multiple lesions can exist and instability can produce secondary problems at the shoulder. In focusing on the differential diagnosis of specific lesions, orthopaedic medicine looks at common lesions at the shoulder. For more detailed coverage of shoulder instability and its relationship to shoulder lesions the reader is referred to other texts that cover this subject.
History (subjective examination)
The age, occupation, sports, hobbies and lifestyle of the patient may give clues to diagnosis. Instability is the main cause of impingement in the younger patient. The younger patient engaged in physical work or active in sport may have a minor instability problem or a labral tear related to overuse, producing secondary impingement. The middle-aged patient may present with overuse rotator cuff lesions, impingement or chronic bursitis. In the older age group, degenerative rotator cuff lesions or tears with secondary or idiopathic capsulitis may occur. Overuse injuries are a common cause of pain felt at the shoulder and the lifestyle of the patient can be directly responsible for the condition. Knowledge of lifestyle is useful to advise the patient on preventing recurrence.
Shoulder injuries are common in throwing sports, swimming and all overhead activities. Tennis strokes involve rotation, abduction and elevation, leading to repetitive and stressful use of the arm in the overhead position, possibly causing instability and impingement pain that may be associated with a labral lesion (McCann & Bigliani 1994). It is relevant to know which is the dominant arm. With the increasing use of shoulder arthroscopy, diagnosis of glenoid labral tears has become more common, notably types of SLAP (superior labrum from anterior to posterior) lesion. The patient complains of a dull throbbing ache in the joint that can cause difficulty in sleeping. There is usually pain and a catching feeling as the arm is thrown into the overhead position and compression of the joint may also produce impingement pain.
Labral tears are difficult to diagnose clinically and to distinguish from other causes of impingement. Several tests have been devised but none of them is 100% sensitive or specific (Guanche & Jones 2003, Brukner & Khan 2007). A systematic review conducted by Munro & Healy (2009), on the validity and accuracy of clinical tests to detect labral pathology of the shoulder, found limited evidence for the biceps loading tests, the internal rotation resistance test, the Kim test and the Jerk tests as accurate tests for differentiating labral pathologies in selected populations. Other tests did not produce such accurate results. The reader is referred to the paper for a description of the tests themselves or they may be found in Hattam & Smeatham (2010). Surgical repair is needed in most cases and the associated instability should be addressed as part of rehabilitation.
Throwing has several different mechanisms, for example the straight-arm throw of the javelin, the centrifugally induced velocity of hammer throwing, the explosive push of putting the shot or the spinning pull of the discus thrower. A ‘dead arm’ syndrome may be produced during the acceleration phase of throwing, when the arm becomes useless and drops down by the side. It may be associated with pins and needles and takes several minutes to recover. It is considered to be due to momentary subluxation of the glenohumeral joint associated with compression of the brachial plexus (Copeland 1993, Clarnette & Miniaci 1998).
The site of the pain does not reliably indicate the site of the lesion. The shoulder joint and its surrounding capsule, ligaments and muscles are mainly derived from the C5 segment. Lesions of any of these structures will cause the pain to be referred into the C5 dermatome which extends into the anterolateral aspect of the arm and forearm as far as the base of the thumb. The most common point of referral for these structures is to the area over the insertion of deltoid. Rotator cuff pathology usually produces anterolateral shoulder pain (Clarnette & Miniaci 1998). The more irritable the lesion, the further the referral of pain into the C5 dermatome, such that the spread of pain will give an indication of the severity of the lesion. As a deep joint lying proximally in its dermatome, the glenohumeral joint has the potential to refer pain over a considerable distance. The cervical spine may produce pain in the shoulder area or refer pain into the C5 dermatome; therefore it will need to be excluded as a source of symptoms.
The acromioclavicular joint and surrounding ligaments produce an accurate localization of pain over the joint. This is because, in contrast to the glenohumeral joint, the acromioclavicular joint is a superficial joint giving little reference.
The symptoms and behaviour need to be considered. The shoulder area is a point of referral of pain from other deep structures. The cervical spine in particular can refer pain to the area and visceral problems may mimic musculoskeletal lesions. The diaphragm is a C4 structure and will produce pain felt at the point of the shoulder if affected by adjacent conditions such as pleurisy.
The onset of the pain may be sudden or gradual. If the onset was sudden it is important to know if there was any related trauma, with the possibility of fracture. A fall on the outstretched hand may initiate a traumatic shoulder joint capsulitis or, less commonly, chronic subacromial bursitis, tendon strain or acromioclavicular joint sprain.
Acromioclavicular lesions are usually associated with a traumatic onset. Degeneration of the joint in the middle-aged to elderly may result from repeated trauma and provide an alternative cause of pain.
An acute subacromial bursitis has a characteristic sudden onset with no apparent cause.
The common shoulder lesions of overuse tendinopathy, bursitis or capsulitis present most typically with a gradual onset of pain due to overuse factors. A capsulitis may be precipitated by trauma, but this is often minor and the patient cannot recall the incident. Stiffness and loss of functional movement are usually indicative of capsulitis. Tendinopathy may be provoked by overstretching or contraction against strong resistance.
The duration of the symptoms gives an indication of the stage the lesion has reached in the inflammatory cycle.
Non-specific shoulder pain may be associated with nerve entrapment, which would be confirmed by signs of objective weakness but with no pain on shoulder movements (Biundo & Harris 1993, Schulte & Warner 1995).
The behaviour of the pain is relevant to diagnosis with the common lesions producing typical musculoskeletal pain on movement which is eased by rest. The patient should be asked if the pain is constant or only present on movement, giving an indication of the irritability of the lesion. Chronic overuse tendinopathy or bursitis often produces a dull ache rather than a pain, although twinges of pain may be experienced if impingement occurs during movement. An acute subacromial bursitis produces severe pain that is constant and often unrelenting, disturbing sleep.
A capsulitis shows an increasing worsening pain, referring further and further into the C5 dermatome. The inflammatory nature of the pain may be obvious in complaints of pain and stiffness on waking. ‘Catching’ pain may be described on activities such as reaching for a seat belt or into the back of the car, or placing an arm in a coat sleeve, and may indicate impingement of structures under the coracoacromial arch.
The behaviour can also help to assess the severity and irritability of the lesion as well as distinguish it from a lesion that is referring pain into the shoulder area. If the patient is unable to lie on that side because the increase in pain disturbs sleep, the lesion is irritable. It may indicate a chronic subacromial bursitis, rotator cuff lesion or more commonly an irritable capsulitis. Sleeping postures may cause stress in structures, inducing microtrauma or impingement.
• Does the pain spread below the elbow? (site and spread)
• Can you lie on that side at night? (symptoms)
• Is the pain constant? (behaviour)
A loss of functional activity such as being unable to do up a bra or reach into the back pocket will indicate limitation of movement. There may be evidence of shoulder instability or labral tears in patients complaining of ‘clicking’, ‘snapping’ or feeling as if the shoulder is ‘coming out’. Crepitus or grating sounds may indicate degenerative changes.
To distinguish the lesion from one of cervical or thoracic origin the patient should be questioned about the presence of paraesthesia, and whether pain is increased on a cough, sneeze or deep breath. Heaviness, tiredness, puffiness, sweating or altered temperature may indicate associated or referred autonomic symptoms.
Assessment of other joint involvement will indicate generalized arthritis, possibly rheumatoid. It is also interesting to note whether the patient has had previous shoulder problems since both ‘frozen shoulder’ (adhesive capsulitis) and acute subacromial bursitis often affect the other shoulder some years after the first incidence. In frozen shoulder the patient may complain of cervical involvement and there may be associated trigger points over the posterior aspect of the shoulder (Grubbs 1993). This may be due to compensatory overuse of other muscles and holding the shoulder in a position of ease, or may be indicative of abnormal neural mobility.
The past medical history will alert the examiner to serious illness and operations experienced by the patient. The patient should be specifically asked about a history of diabetes since there is an association between diabetes mellitus and the development of a frozen shoulder (Owens-Burkhart 1991, Clarnette & Miniaci 1998). The examiner should be on the alert for possible contraindications to treatment. An indication of the patient’s current state of health is necessary and the patient should be asked about recent unexplained weight loss. Tumours involving the shoulder area are rare but a history of primary tumour should raise the suspicion of metastatic disease as a possible diagnosis (Clarnette & Miniaci 1998). As well as past medical history, establish any ongoing conditions and treatment. Explore other previous or current musculoskeletal problems with previous episodes of the current complaint, any treatment given and the outcome of treatment.
Medications currently being taken by the patient are determined to eliminate possible contraindications to treatment. The amount of analgesia required by the patient gives an indication of the severity of the lesion.
From the history, the possible diagnoses are noted. If the eventual diagnosis is one of capsulitis, three special questions relating to the spread of pain and provocation factors asked during the history (see Box page 97) will give an indication of the severity of the lesion and act as a guide to treatment.
Inspection
The patient should undress to allow the area to be inspected in a good light.
A general inspection will determine any bony deformity. Look at the position of the cervical spine and take an overall view of the spinal curvatures in general. The general posture of the patient can be important and any observations of asymmetry are recorded if they are relevant to the presenting condition. It has been postulated that abnormal cervical and thoracic posture, particularly an increased thoracic kyphosis, alters the resting position of the scapula and may be related to shoulder pain caused by overuse (Greenfield et al 1995).
The attitude of the shoulder should be noted. Is one higher than the other or excessively medially rotated? In a frozen shoulder, one shoulder may be held higher than the other due to pain, with the scapula elevated and retracted. The position of the scapulae should be noted. Are they more or less symmetrical, lying approximately three fingers from the midline, or are they excessively retracted or protracted? There may be evidence of winging of the scapula but this is usually more obvious on movement.
Lumps, scars, bony prominences and bruising should be observed. A prominent bump at the end of the clavicle may signify an old fracture or dislocation of the acromioclavicular joint.
Colour changes and swelling are unusual findings at the shoulder unless associated with direct trauma. Muscle wasting is suspected if the spine of the scapula is prominent, due to neuritis or rotator cuff rupture. In chronic rotator cuff tendinopathy and/or degenerative tears, wasting of supraspinatus and infraspinatus may be obvious. The ‘pop-eye’ deformity of a rupture of the long head of the biceps is usually obvious, but the patient does not particularly complain of pain. In deltoid atrophy, squaring of the shoulder occurs as deltoid is no longer rounded out over the humeral head and may be indicative of anterior dislocation (Clarnette & Miniaci 1998).
State at rest
Before any movements are performed, the state at rest is established to provide a baseline for subsequent comparison.
Examination by selective tension (objective examination)
The suggested sequence for an objective examination of the shoulder will now be given, followed by a commentary including the reasoning in performing the movements and the significance of the possible findings. Comparison should always be made with the other side.
Eliminate the cervical spine
• Active cervical extension (Fig. 5.9a)
 |
| Figure 5.9
Six active movements of the cervical spine: (a) extension; (b, c) rotations; (d, e) side flexions; (f) flexion.
|
• Active right cervical rotation (Fig. 5.9b)
• Active left cervical rotation (Fig. 5.9c)
• Active right cervical side flexion (Fig. 5.9d)
• Active left cervical side flexion (Fig. 5.9e)
• Active cervical flexion (Fig. 5.9f)
Shoulder elevation tests
Passive glenohumeral movements
Resisted tests
• Resisted shoulder abduction (Fig. 5.17)
 |
| Figure 5.17
Resisted abduction.
|
• Resisted shoulder adduction (Fig. 5.18)
 |
| Figure 5.18
Resisted adduction.
|
• Resisted shoulder lateral rotation (Fig. 5.19)
 |
| Figure 5.19
Resisted lateral rotation.
|
• Resisted shoulder medial rotation (Fig. 5.20)
 |
| Figure 5.20
Resisted medial rotation.
|
• Resisted elbow flexion (Fig. 5.21)
 |
| Figure 5.21
Resisted elbow flexion.
|
• Resisted elbow extension (Fig. 5.22)
 |
| Figure 5.22
Resisted elbow extension.
|
Accessory test for acromioclavicular joint or lower fibres of subscapularis
• Passive shoulder flexion and adduction (scarf test) (Fig. 5.23)
 |
| Figure 5.23
The scarf test.
|
Palpation
• Once a diagnosis has been made, the structure at fault is palpated for the exact site of the lesion
The examination of the shoulder should first exclude possible cervical lesions; therefore six active cervical movements are performed and if a pattern of signs emerges implicating the cervical spine then a full assessment of this region must be conducted.
Three elevation tests are conducted for the glenohumeral joint. Since the shoulder is considered to be an ‘emotional’ area, active elevation indicates the patient’s willingness to move the joint. The range of movement and level of pain should then be consistent with other findings as the objective examination proceeds.
Passive elevation is added to assess pain, range of movement and end-feel. The normal end-feel of passive elevation is elastic. Any limitation of passive elevation suggests that the capsular pattern exists at the glenohumeral joint and this will be confirmed when the passive glenohumeral movements are assessed individually.
Active elevation through abduction is conducted in the coronal plane to assess for the presence of a painful arc. This involves abduction to 90° followed by lateral rotation, to enable the greater tuberosity to clear the coracoacromial arch. The test performed in this way is usually consistent with the patient’s account of symptoms. However, functionally, the arm is more commonly lifted through scaption (see p. 91).
A painful arc is a localizing sign and indicates impingement of a painful structure in the subacromial space – which structure will be revealed only by completing the full examination procedure. An arc is more easily elicited on active movement as contraction of the muscle groups tends to raise the humeral head and reduce the space; it is generally found between 60 and 120° of abduction.
Be prepared to explore for a painful arc, especially in the light of findings later in the examination, remembering that a diagnosis is not made until the full examination has been completed. The position may be modified to place the rotator cuff tendons into a more vulnerable position for compression against the coracoacromial arch.
Elevation of the humerus through abduction in the coronal plane favours compression of the distal end of the supraspinatus tendon. Abduction with medial rotation, palm down, brings infraspinatus forwards and increases the possibility of its compression, while abduction with lateral rotation, palm up, brings the upper part of subscapularis to face upwards to be compressed against the arch (Figure 5.12 and Figure 5.13). Forward elevation in the sagittal plane combined with lateral rotation, palm up, compresses the tendon of the long head of the biceps (Burns & Whipple 1993).
The passive glenohumeral movements are conducted looking for pain, range of movement and end-feel. Since variation in movement between individuals is probable, movements should always be compared with the other side. However, variation between sides may exist, for example in tennis players or fast bowlers, who may have a greater range of one rotation, at the expense of the other, on the dominant side. Passive lateral and medial rotations have a normal elastic end-feel; passive abduction is assessed for range of movement only, since it is not possible to appreciate the end-feel. Assessment of the passive glenohumeral movements may confirm the presence of the capsular pattern, indicating arthritis.
As movements become limited in the capsular pattern they develop an abnormally ‘hard’ end-feel. The capsular pattern results in overall limitation of passive elevation. Limitation or pain at the end of range of lateral rotation only may be a sign of early capsulitis.
It may not be possible fully to assess the range of medial rotation in severe capsulitis since the accompanying limitation of abduction prevents the arm from being placed behind the patient’s back. As a guide for subsequent comparison, measure the range of movement against certain landmarks that can be reached by the hand, e.g. pocket, buttock, waist, inferior angle of scapula.
Subacromial bursitis provides a typical example of a non-capsular pattern of movement at the shoulder. While the acromioclavicular joint does not demonstrate its own capsular pattern, it produces a non-capsular pattern of movement at the glenohumeral joint.
The resisted tests are conducted looking for pain and reduced power which will indicate a muscle lesion or possible neurological involvement. The resisted tests performed in the upright position apply a degree of upwards shearing and compression to the glenohumeral joint in stabilizing the head of the humerus. For this reason the resisted tests may be accessory signs in subacromial bursitis, or show involvement of the joint. To confirm diagnosis, the resisted tests may be repeated in lying, with some joint distraction, where the effect of compression and shear on the joint is reduced (Figure 5.24 and Figure 5.25).
 |
| Figure 5.24
Resisted shoulder abduction with distraction.
|
 |
| Figure 5.25
Resisted elbow extension with distraction.
|
Resisted abduction tests mainly supraspinatus; resisted adduction tests latissimus dorsi and pectoralis major; resisted lateral rotation tests mainly infraspinatus and teres minor; resisted medial rotation tests mainly subscapularis; resisted elbow flexion tests biceps; and resisted elbow extension tests triceps. The anatomical interdigitation of the tendinous insertions of the rotator cuff tendons means that the resisted tests described may not definitively implicate one tendon; subsequent palpation of the structures implicated will identify the site of the lesion.
Painful weakness on resisted testing may indicate partial rupture, but it may be difficult to decide whether a test is producing real or apparent weakness since the patient is limited by pain from making a maximal effort (Pellecchia et al 1996).
In athletes it may be difficult to produce positive findings, especially on resisted testing, as the symptoms may only be provoked during the athletic or sporting activity itself. It may be necessary for the patient to provoke the pain before the examination is carried out.
An accessory test, the ‘scarf’ test (as in putting a scarf over the opposite shoulder), may be performed to localize the lesion. This compresses the acromioclavicular joint or impinges the lower fibres of the subscapularis tendon against the coracoid process. It may also be positive as part of the ‘muddle’ of signs of a chronic subacromial bursitis.
Palpation is conducted for the site of the lesion, but only along the structure determined to be at fault since the shoulder is notorious for tender trigger points.
Through this scheme, a working diagnosis is established on which to base a treatment programme, with constant monitoring and reassessment. This approach is just one possible way of assessing the shoulder. Pellecchia et al (1996) looked at the intertester reliability of the Cyriax evaluation and showed it to be highly reliable in the assessment of patients with shoulder pain, facilitating the identification of diagnostic categories for subjects with shoulder pain.
However, the approach does not investigate hypermobility at the shoulder with consequent instability, and the reader is recommended to employ provocative instability tests as appropriate. In addition, specific impingement tests and tests for labral tears can be employed as necessary (see Hattam & Smeatham 2010). The examination of neural structures can also be incorporated into the procedure.
CAPSULAR LESIONS
The movements limited in the capsular pattern have a characteristic ‘hard’ end-feel, although this is less marked in the early stage, and any restriction of the glenohumeral range is usually consistent with an overall loss of shoulder elevation. The presence of the capsular pattern at the shoulder indicates arthritis. Commonly this is idiopathic, primary arthritis or traumatic (secondary) arthritis. This is synonymous with frozen shoulder or adhesive capsulitis, as discussed below. Less commonly, the shoulder can be affected by degenerative osteoarthrosis, rheumatoid arthritis or any of the spondyloarthropathies.
‘Frozen shoulder’ (adhesive capsulitis)
The term frozen shoulder is commonly used by the general public to describe any stiff or painful shoulder, but it is an overused term, much criticized, since it appears to avoid a more specific diagnosis. It is, however, an easy term to use and describes the signs and symptoms indicating involvement of the capsule of the shoulder joint, which is the key factor.
The natural history of the condition is that it follows a pattern of increasing signs and symptoms (freezing), followed by a plateau stage (frozen) before a slow, spontaneous recovery of partial or complete function (thawing). Recovery tends to occur within 1–3 years (Wadsworth 1986). A short painful period is associated with a short recovery period and a longer painful period with a longer period of recovery (Owens-Burkhart 1991).
Several authors have reviewed the history of the frozen shoulder (Wadsworth 1986, Owens-Burkhart 1991, Anton 1993). It was first described by Duplay in 1872 and Codman was responsible for using the term ‘frozen shoulder’ in 1934, but used it in association with rotator cuff tendinopathy. Neviaser introduced the concept of ‘adhesive capsulitis’ in 1945 because of the appearance of the thickened, adherent capsule that could be peeled from the bone like sticky plaster.
The cause of the condition is unknown. It is probably multifactorial, including a period of immobilization due to pain, and may include local periarticular inflammatory and degenerative changes. Association with other lesions has been reported, including cervical spine disorders, dysfunction of neural structures, thoracic spine immobility, thoracic or breast surgery, trauma, neurological disease, reflex sympathetic dystrophy, cardiovascular disease, stroke, systemic disease, in particular diabetes mellitus, and the presence of immunological factors, e.g. human leukocyte antigen (HLA)-B27 (Jeracitano et al 1992, Anton 1993, Grubbs 1993, Stam 1994).
Pathology of frozen shoulder
In a review of the literature, various authors observed and reported the following changes seen at arthrography, arthroscopy and surgery (Wadsworth 1986, Owens-Burkhart 1991, Wiley 1991, Uhthoff & Sarkar 1992, Anton 1993, Grubbs 1993, Uitvlugt et al 1993, Stam 1994, Bunker & Anthony 1995, Bunker et al 2000, Smith et al 2001):
• Volumes of less than 10 mL, compared with the normal intra-articular volume, and a failure to fill the subscapularis bursa or biceps tendon sheath
• Inflammatory changes, adhesion formation, erythematous fibrinous pannus over the synovium and loss of the redundant axillary fold
• Fibrosis, not inflammation, with changes similar to those seen in Dupuytren’s disease of the hand
• Retraction of the capsule away from the greater tuberosity, thickening of the coracohumeral ligament and subscapularis tendon, and a loss of the normal interval between the glenoid and humeral head.
Involvement of the joint capsule seems to be a common feature of all cases studied, but the above list shows that debate still continues over the nature of that involvement.
Frozen shoulder consists of a spontaneous onset of gradually increasing shoulder pain, referring to the deltoid region and forearm if severe, with an increasing limitation of movement. Lundberg (1969) divided the syndrome into primary or secondary types:
• Primary frozen shoulder is idiopathic
• Secondary frozen shoulder occurs following a precipitating trauma or can arise from other causes.
The ‘steroid-sensitive arthritis’ and ‘traumatic arthritis’, as described by Cyriax (1982), fit into the primary and secondary groups, respectively.
Primary frozen shoulder
Cyriax (1982) called this condition ‘steroid-sensitive arthritis’ or ‘monoarticular rheumatoid arthritis’. The condition seems particularly resistant to physical treatment, but responds well to corticosteroid injection.
Bunker & Anthony (1995) described the pathology as similar to Dupuytren’s disease with increased collagen, myofibroblast and fibroplasia. Of the 50 patients with primary idiopathic frozen shoulder studied, 58% also had Dupuytren’s disease elsewhere. There was also an association with diabetes. Although the condition is said to be fibrosing rather than inflammatory, once developed, the inflammatory drivers for Dupuytren’s disease and frozen shoulder are similar: TGF-β (transforming growth factor-beta) and PDGF (platelet-derived growth factor) (Funk 2008).
The patient’s condition follows a typical pattern:
• The patient is usually between 40 and 70 years old
• Women are affected slightly more frequently than men
• There is no reason for the onset
• The condition progresses slowly to spontaneous recovery over 2–3 years
• Recurrence of the condition in the other shoulder within 2–5 years is common (Cyriax 1982).
Secondary frozen shoulder
Causes of secondary frozen shoulder may include trauma or any condition which causes immobilization of the shoulder, e.g. neurological conditions, fracture and pain associated with bursitis or tendinopathy, thyroid disease, cardiac disease, thoracic surgery, pulmonary disease, diabetes mellitus, postmenopausal hormonal changes, or psychological factors such as depression, apathy and emotional stress (Owens-Burkhart 1991, Stam 1994, Siegel et al 1999).
This type of arthritis most frequently occurs secondary to trauma. A painful shoulder may be kept relatively immobile by involuntary muscle spasm, contributing to pain and stiffness, but the close proximity of other anatomical structures may also be relevant. The subacromial bursa, rotator cuff tendons and the long head of the biceps are all closely related to the capsule of the shoulder joint and it may be possible for changes in these structures to have a secondary effect on the capsule.
If precipitated by trauma, the incident may be minor and the initial pain usually settles. Therefore the patient may have difficulty recalling a traumatic incident or associating it with the onset of the pain. As a guideline, the condition can be classified into three stages, each of which gives an indication of the irritability of the lesion and a suggested programme of treatment. The three special questions taken from the history (see below) and the assessment of the degree of capsular pattern, together with the end-feel of the passive movements, provide reliable diagnostic criteria.
Stage 1
After the precipitating incident, the initial pain settles. Approximately 1 week later, pain develops and gradually increases. The pain is felt over the area of deltoid, but as inflammation increases, the pain is referred further into the C5 dermatome. The extent of reference of pain indicates the degree of severity of the condition. This stage develops over several weeks and pain is the key feature, not the limited movement.
Since the shoulder joint has a wide range of movement, the early developing capsular pattern may not affect function and the patient may be oblivious to the loss of movement at this stage. Diagnosis in this early stage is not easy but it becomes conclusive once the capsular pattern of limited movement occurs. If treated early enough, it may be possible to abort the progressive cycle of the condition. Unfortunately, as pain is the main feature of this stage and not loss of function, patients may not seek help for the condition early enough.
The examination of the patient provides a set of signs and symptoms that classifies the patient as having stage 1 capsulitis and indicates a possible line of treatment.
From the history the three special questions reveal that:
• The pain is usually above the elbow
• The pain is not usually constant
• The patient can usually sleep on that side at night.
The objective examination shows that:
• A minor capsular pattern exists (this may involve lateral rotation only)
• The end-feel of passive movements remains relatively elastic, but is harder than the normal end-feel.
The history and examination indicate a relatively non-irritable joint capsule that may respond to peripheral Grade B mobilization or corticosteroid injection. Of course, any mobilizing technique can be applied to such a joint and the treatment programme for each individual patient is formulated based on the therapist’s experience. Orthopaedic medicine treatment techniques will be described below.
Stage 2
Pain and loss of function are now the key features of the condition. The capsular pattern has developed to affect abduction and medial rotation adversely, and, subjectively, the latter is the most inconvenient functional movement for the patient to lose. As the pain gradually peaks and spreads, the patient notices an inability to reach into a back pocket, for example, or to do up a bra. The limitation of lateral rotation is apparent in that the patient is unable to comb the hair.
From the history the three special questions reveal that:
• The pain usually spreads beyond the elbow
• The pain is usually constant
• The patient usually cannot sleep on that side at night.
The objective examination shows that:
• A full capsular pattern is present
• The characteristic ‘hard’ end-feel of arthritis exists due to involuntary muscle spasm and capsular contracture.
The history and examination reveal an irritable joint capsule. The presence of the capsular pattern is marked. Adhesion formation in the axillary fold, tightness in the anterior capsular ligaments, shortening of subscapularis and contracture of the rotator interval combine to limit lateral rotation and abduction significantly, producing the capsular pattern. At this stage corticosteroid injection may be used to treat the pain and/or relatively gentle pain-free mobilization may be applied to restore accessory range. The orthopaedic medicine treatment techniques will be described below.
Stage 3
If the patient progresses through the complete cycle of the condition, this represents the stage of recovery. The pain is settling and receding and full functional movement is returning. However, the end result of the condition may leave the patient with a degree of pain and some limited movement, especially lateral rotation and full elevation. Shaffer et al (1992), in a long-term follow-up (average 7 years) of idiopathic frozen shoulder treated non-operatively, showed 50% of patients to have residual mild pain or stiffness of the shoulder, or both. Limitation of lateral rotation was present when restriction of movement was a feature.
Stage 3 shows similar signs and symptoms to stage 1 and the same treatment may be applied together with rehabilitation, including strengthening and stretching exercises, towards full function.
Treatment techniques for frozen shoulder
There is no standard agreed treatment for frozen shoulder. Various approaches have been advocated, including analgesic drugs, corticosteroid injections, mobilization techniques and exercises of various forms, manipulation under anaesthetic, brisement (forcible breaking of adhesions) or distension arthrography, arthroscopic distension and surgical release of adhesions (Hsu & Chan 1991, Hulstyn & Weiss 1993, Sharma et al 1993, Ogilvie-Harris et al 1995). Microadhesiolysis has been developed as a minimally invasive technique for releasing adhesions with significant subjective and objective improvements (Ahn et al 2008). Studies on non-operative treatments for frozen shoulder have shown that physiotherapy (not defined) improves range of movement but not necessarily pain relief. Corticosteroid injections have a benefit for short-term pain relief only but no long-term pain relief (Haslan & Celiker 2001, Ryan 2005 (cited in Funk 2007)).
The aim of treatment in each of the measures listed above, as in the use of orthopaedic medicine techniques, is to relieve pain and restore function.
For primary frozen shoulder, i.e. steroid-sensitive arthritis, Cyriax (1982) suggested a course of intra-articular injections of corticosteroids to treat the pain. These are given over increasing intervals and, with the relief of pain, a gradual increase in movement occurs with recovery to full function.
For secondary frozen shoulder, i.e. traumatic arthritis, the clinician has a choice of treatment dependent upon the stage of irritability and the techniques available. Those recommended in orthopaedic medicine will be described, but the reader is urged not to be limited to this choice, but to draw on experience of other mobilization techniques that can be incorporated to provide an individual treatment programme for each patient.
Suggested needle size: 21G × 1½ in (0.8 × 40 mm) or 2 in (0.8 × 50 mm) green needle
Dose: 20–40 mg triamcinolone acetonide in a total volume of 3–5 mL
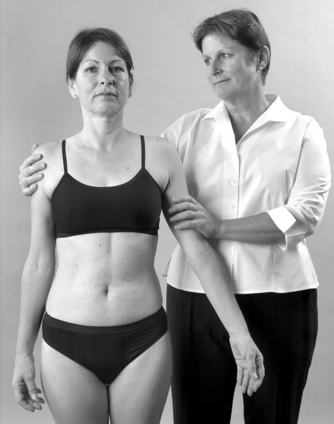
Position the patient comfortably either in prone-lying or sitting in a chair (Fig. 5.26). Place the affected arm to rest in medial rotation across the abdomen with the elbow flexed.
 |
| Figure 5.26
Injection of the glenohumeral joint, sitting.
|
Stand behind the patient and place your thumb on the posterior angle of the acromion and your index or middle finger on the coracoid process. Insert the needle 1 cm below your thumb placed on the acromion and direct it forwards towards the index finger placed on the coracoid process (Fig. 5.27). Once the needle rests against the articular surface, deliver the injection as a bolus, withdrawing slightly if there is resistance.
 |
| Figure 5.27
Injection of the glenohumeral joint, showing direction of approach and needle position.
|
An explanation of the condition and prognosis is important. The principle is to give another injection if the pain begins to peak, which usually occurs at increasing intervals. Generally not more than three or four injections are given in total. The patient is instructed to apply relative rest for up to 2 weeks and then to begin pain-free mobilization. Injections of corticosteroid are efficacious in treating frozen shoulder providing the patients selected fulfil the diagnostic criteria based on Cyriax, described above in stages 1, 2 and 3 of the condition (Cameron 1995).
Jacobs et al (1991) looked at the effect of administrating intra-articular steroids with distension for the management of the early frozen shoulder. Fifty patients with frozen shoulder were divided into three treatment groups: a distension group only, a steroid group only and a steroid and distension group. A total of three injections were offered at 6-week intervals using the posterior approach described above. All patients were provided with an information sheet explaining capsulitis and a home exercise programme.
All patients entered into the study showed improvement during treatment, with a decreased need for analgesia and improvement in pain symptoms. A significantly increased rate of improvement in the range of passive abduction and forward flexion occurred in the two groups treated with intra-articular corticosteroid, indicating a positive role for the use of corticosteroids in the early frozen shoulder.
Grade B mobilization (saunders 2000)
Peripheral Grade B mobilization (see Ch. 4) is applied to the non-irritable joint only. The aim is to relieve pain and increase the range of movement. Heat may be used beforehand to assist the technique since heating enhances the viscoelastic properties of the capsule. The condition, prognosis and treatment are explained carefully to the patient since the recovery time may be prolonged over many months, or even years, and the patient must be encouraged to continue the stretching techniques at home, eventually taking over treatment, with the therapist remaining in a supervisory role for as long as necessary.
Position the patient comfortably in lying with the arm in as much elevation as possible (Fig. 5.28). Place a hand on the sternum or scapula to stabilize the thorax and the other hand over the patient’s raised elbow to apply a stretch into elevation. The principles of Grade B mobilization are applied: heating, holding and repeating the stretch, working on the principles of creep (see Ch. 2), and the arm is returned under some distraction for comfort (Fig. 5.29).
 |
| Figure 5.28
Grade B mobilization of the glenohumeral joint.
|
 |
| Figure 5.29
Returning the arm from the elevated position, with distraction for comfort.
|
This technique is fairly aggressive and will cause a certain amount of post-treatment soreness. The pain may be aggravated for 2–4 hours and this should be explained to the patient. An increase in mobility is often reported before the reduction of pain but both are indications for continued treatment.
Distraction techniques
These are a form of Grade A mobilization since they occur within the pain-free range of movement. The aim is to restore the accessory range of movement to the joint. The techniques can be applied together with Grade B mobilization in the non-irritable joint, to settle the tissues after treatment, or alone in the more irritable joint, particularly if injection is not an option. Once the end-feel of the limited movements regains some elasticity, the joint is deemed to be non-irritable and techniques can be progressed, adding Grade B mobilization.
Lateral distraction (Cyriax 1984, Cyriax & Cyriax 1993)
Position the patient comfortably in supine lying close to the edge of the couch, which is raised to approximately hip height. Place a pillow under and around the arm to support it in the loose packed position of adduction and some medial rotation. Place a hand into the axilla to apply the lateral distraction while simultaneously applying counterpressure to the patient’s elbow, resting against your hip (Fig. 5.30). The distraction is held for as long as possible and repeated often.
 |
| Figure 5.30
Lateral distraction.
|
Caudal distraction
Position the patient as above. Hook your forearm into the crook of the patient’s flexed elbow (Fig. 5.31). Apply sustained and repeated caudal distractions.
 |
| Figure 5.31
Caudal distraction.
|
A ‘seat belt’ can be used to aid the distraction techniques, but the reader is referred to courses and texts on ‘seat belt therapy’ for the description of its use. Other mobilizing techniques can also be incorporated into this regime.
NON-CAPSULAR LESIONS
Acute subacromial bursitis
The existence of this condition as described by Cyriax (1982) and Cyriax & Cyriax (1993) is controversial and it may be the same as, or similar to, a condition described by others as acute calcific tendinitis. The calcific deposit in the rotator cuff, usually supraspinatus, increases in size and ruptures into the subacromial bursa (Berg 1997). This provides a plausible explanation for the acute onset and intensity of the pain in the relatively short acute phase. Magnetic resonance imaging (MRI) would confirm the presence of calcific deposits and/or inflammation in the subacromial space or overlying rotator cuff.
Acute subacromial bursitis is a completely separate entity from chronic subacromial bursitis, described below. It has a typical presentation of a rapid onset of pain for no apparent reason. The pain is felt in the shoulder area; it rapidly increases in severity and within hours the pain is referred into the whole C5 dermatome. The patient may look tired and unwell as the condition is very painful and disturbs sleep. Since the bursa is an extra-articular structure, it is not protected by involuntary muscle spasm. Voluntary muscle spasm is responsible for the patient holding the arm in an antalgic position, and in the attempt to sleep the patient loses the protective voluntary muscle spasm, waking with severe pain. Severe twinges of pain are experienced on attempted active movement, especially abduction, which compresses the painful bursa in the subacromial space. It is important to consider serious pathology and onward referral should be made if the severe pain does not settle within 1 week. Otherwise, the condition is self-limiting and is usually very much better within 7–10 days, clearing completely within 6 weeks, but prone to recurrence (Cyriax 1982).
On examination, a non-capsular pattern of limited movement is present. Voluntary muscle spasm is responsible for producing an empty end-feel on examination, where the examiner is aware that much more range is available but the patient will not tolerate further movement. Usually full lateral rotation can be coaxed, especially with a little distraction applied to the joint, but the range of abduction is severely limited by pain, indicating a non-capsular pattern. Swelling and tenderness may be present along the lateral border of the acromion.
Treatment does not alter the course of the condition but should take the form of pain-relieving modalities and an explanation to the patient. The application of transcutaneous nerve stimulation and oral administration of analgesics are appropriate. Advice should also be given on sleeping position, suggesting that the arm should be well supported by pillows, bandaged to the side or supported inside a tight-fitting T-shirt to maintain comfort when the protective muscle spasm is lost. A collar-and-cuff sling provides less support but may be used if the patient is unable to tolerate the compression of the previous suggestions.
An injection of corticosteroid is usually helpful, although it may increase the pain initially as the bursa is already swollen and very painful. The technique is the same as for chronic subacromial bursitis, see page 114, but less volume is used.
Treatment, ideally, consists of an injection of a small volume of low-dose local anaesthetic together with an appropriate amount of corticosteroid. General advice should be given on how to support the area whilst the symptoms settle and other pain-relieving modalities can be applied.
Position the patient comfortably in sitting with the arm hanging by the side. Locate the midpoint of the lateral border of the acromion and insert the needle just below, at an oblique angle upwards with respect to the acromion (Figure 5.32 and Figure 5.33).
 |
| Figure 5.32
Injection of the subacromial bursa.
|
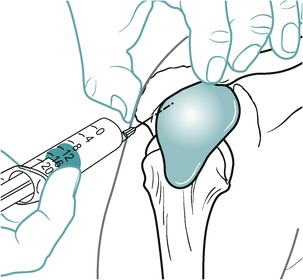 |
| Figure 5.33
Injection of the subacromial bursa showing direction of approach and needle position.
|
Acromioclavicular joint
The pain from the acromioclavicular joint is characteristically felt in the epaulette region of the shoulder. The onset may be precipitated by trauma – either a fall on the outstretched hand or a direct blow such as a heavy fall against the wall while playing squash, in a rugby tackle or at touchdown.
On examination, a non-capsular pattern of glenohumeral movement is present with pain felt at extremes of passive elevation, lateral and medial rotation; the acromioclavicular joint itself does not display a capsular pattern as such. The diagnosis is confirmed by a positive scarf test reproducing the pain by compressing and shearing the joint (Hattam & Smeatham 2010).
Degenerative osteoarthrosis affects the acromioclavicular joint, especially in those who have been extremely active in sport (Stenlund 1993). Overuse can provoke a traumatic arthritis of the degenerate joint. The degenerative changes cause narrowing and osteophyte formation, which can have a secondary effect on the structures in the subacromial space.
Allman classified injuries of the acromioclavicular joint into three categories (Cailliet 1991, Hartley 1995):
• Type I injury is sprain or partial tearing of the capsuloligamentous fibres with local pain and tenderness and no joint instability.
• Type II injury involves tearing of capsuloligamentous fibres and minor subluxation, but as the coracoclavicular ligament remains intact, there is no instability.
• Type III injury is dislocation of the acromioclavicular joint with disruption of the capsule and the coracoclavicular ligament. Treatment for type III injury is usually surgery.
Orthopaedic medicine treatment may be useful in type I and II lesions. In Chronic lesions, corticosteroid injection of the joint may be curative. if the superior aspect of the capsular ligament is involved, it may be treated with transverse frictions as appropriate.
Position the patient comfortably in sitting or half-lying and palpate the superior aspect of the joint line (Fig. 5.34). There is considerable variation in the size, shape and direction of the joint surfaces and if the joint is narrowed by degenerative changes it may be difficult to enter. The needle may have to be angled obliquely inferomedially and the presence of the articular disc may make entry difficult. Insert the needle into the joint and deliver the injection as a bolus, or pepper the superior ligament if needle entry proves to be difficult (Fig. 5.35). This would be more appropriate for chronic lesions and, if acute, it is more appropriate to allow the ligamentous lesion to settle if entry into the joint is not possible, to avoid possible delay in healing. The patient is advised to maintain a period of relative rest for approximately 2 weeks following injection.
 |
| Figure 5.34
Injection of the acromioclavicular joint.
|
 |
| Figure 5.35
Injection of the acromioclavicular joint showing direction of approach and needle position.
|
Transverse frictions to the superior acromioclavicular capsular ligament (Cyriax 1984, Cyriax & Cyriax 1993)
Stand behind the seated patient and palpate the joint line. Using an index finger reinforced by a middle finger, thumb-down on the scapula for counterpressure, direct the pressure down onto the tender ligament and impart the transverse frictions in an anteroposterior direction. The grade of application will depend on the irritability of the lesion (Fig. 5.36).
 |
| Figure 5.36
Transverse frictions to the acromioclavicular joint.
|
SUBACROMIAL IMPINGEMENT SYNDROME
‘Impingement syndrome’ is a generic term for rotator cuff lesions encompassing all stages of tendon disease. The subacromial bursa may also be involved and impingement may be due to subacromial space stenosis, inflammation and/or fibrosis of the contents of the space. Anatomical anomalies, particularly type III hook-shaped acromions or congenital subacromial stenosis, may predispose to impingement syndrome (Farley et al 1994, Frieman et al 1994, Burkhart 1995). Shoulder instability is also a possible mechanism, especially in younger athletes (Hanchard et al 2004, Brukner & Khan 2007). Brukner & Khan (2007) emphasize that ‘impingement’ is a clinical sign, not a diagnosis. Impingement syndrome accounts for 44–66% of all complaints of shoulder pain (Michener et al 2004).
Microtrauma of the cuff tendons may interfere with their stabilizing function, allowing the humeral head to ride higher in the glenoid and further reducing the subacromial space. Impingement may be associated with shoulder instability, degenerative changes in the acromioclavicular joint, osteophyte formation, degenerative spur formation under the acromion and thickening of the coracoacromial ligament.
The rotator cuff, especially supraspinatus, maintains the subacromial space by depressing the head of the humerus to prevent superior translation during abduction and elevation movements. Repetitive use, fatigue or overload results in cumulative microtrauma, and the cuff muscles are unable to resist this superior translation, leading to subtle instability (Copeland 1993).
Patients under 35 years, particularly athletes using the arm in the overhead position (e.g. swimming, tennis, squash, javelin, golf), in which large ranges of movement, forces, acceleration and repetitive movements are involved, may present with signs of impingement. This may be secondary to minor instability, possibly involving labral tears (Copeland 1993, Jobe & Pink (1993) and Jobe & Pink (1994)). Subtle or subclinical subluxation reduces the maximum congruency of the glenoid and it appears that the supraspinatus and infraspinatus tendons are pinched in the posterosuperior labrum. The combination of instability, impingement and rotator cuff lesions should be considered in the younger athlete and the management directed at improving movement patterns to correct the instability (Iannotti 1994).
In patients over 35 years, changes occur in the subacromial space which are related to degeneration and the ageing process. Fatigue and degeneration of fibres may produce muscle imbalances which lead to altered neuromuscular control and abnormal movement patterns. The humeral head is no longer effectively depressed and superior translation occurs, compromising the subacromial space (Copeland 1993, Wilk & Arrigo 1993, Greenfield et al 1995).
Richards et al (2005) demonstrated a correlation between narrowed coracohumeral distance and subscapularis tears and Di Mario & Fraracci (2005) also linked this finding to subacromial impingement.
The impingement syndrome involves inflammation and oedema in the subacromial bursa in the first instance, and secondary thickening and fibrosis is followed by partial or full tears of the rotator cuff. The tears are usually longitudinal and on the undersurface of the tendons, which may be relatively avascular compared with the bursal surface (Cailliet 1991, Uhthoff & Sarkar 1992, Copeland 1993, Fukuda et al 1994, McCann & Bigliani 1994). Early tendon lesions may involve intrasubstance tears and calcific deposits can occur within the substance of the tendon (Meister & Andrews 1993).
Neer (1983) was responsible for classifying the impingement syndrome into three progressive stages and provided additional evidence that impingement occurs against the anterior edge and undersurface of the anterior third of the acromion and the coracoacromial ligament; sometimes the acromioclavicular joint is involved but not the lateral edge of the acromion:
• Stage I impingement involves oedema and haemorrhage, characteristically seen in younger patients. Conservative treatment at this stage usually has good results and can reverse the condition.
• Stage II follows repeated episodes of mechanical inflammation and the subacromial bursa may become thickened and fibrotic. This stage occurs in older patients and the shoulder functions well for light use but becomes symptomatic after overuse, particularly in the overhead position. Neer recommends conservative management, with surgery considered only if the condition fails to respond to treatment after an 18-month period.
• Stage III involves incomplete or complete tears of the rotator cuff, biceps lesions and bone alteration of the anterior acromion and greater tuberosity. These are found almost exclusively in the over-40 age group, with tears of supraspinatus occurring in a ratio of 7:1 over biceps. Stage III lesions are referred for surgical opinion. Neer also states that, in his experience, 95% of tears of the cuff are initiated by impingement wear rather than circulatory impairment or trauma, although trauma may enlarge an existing tear.
Clinical testing is of use in early screening but a subacromial anaesthetic injection is more reliable in giving a definitive diagnosis (Alvarez-Nemegyei & Canoso 2003). Positive impingement signs include painful or weak resisted abduction, external rotation or internal rotation and a painful arc, and there may be a combination of several signs if the subacromial bursa is involved. The pain is usually felt in the deltoid region. Mohtadi et al (2004) add maximal tenderness over the supraspinatus tendon as a sign of impingement.
The most sensitive tests have been found to be the Hawkins–Kennedy, Neer and horizontal adduction tests and the tests with the highest specificity are the ‘drop arm’ Yergason and painful arc tests (Calis et al 2000). Johansson & Ivarson (2009) confirm further that the Neer impingement sign, Hawkins—Kennedy impingement test, Patte manoeuvre and Jobe’s test are highly reproducible and therefore reliable to use in clinical practice. The reader is referred to Hattam & Smeatham (2010) for a description of the tests themselves.
Chronic subacromial bursitis
The subacromial bursa may be involved in impingement syndrome and chronic subacromial bursitis is a relatively common cause of pain at the shoulder. However, it can present a challenge to diagnosis because of the muddled picture presented on examination. The bursa’s intimate relationship with the capsule, the rotator cuff tendons and the biceps tendon makes it difficult to diagnose definitively and treatment response can help to confirm or refute diagnosis.
Furthermore, lesions can coexist, and a primary lesion can indirectly affect the structures closely related to it. In reviewing the anatomy it will be seen that the inner synovial aspect of the bursa is also the outer aspect of the rotator cuff, the supraspinatus tendon in particular. Therefore, they cannot be separated and a lesion of one may affect the other.
Prolonged inflammation can cause adhesion formation between the layers of the bursa and may produce a secondary frozen shoulder. In an unwell patient subacromial abscess or infective bursitis may be suspected (Ward & Eckardt 1993).
Chronic subacromial bursitis has a gradual onset of pain due to the microtrauma of overuse. Together with rotator cuff lesions, chronic bursitis is a common cause of pain in athletes using the arm in the overhead position, e.g. racquet sports, throwing activities of all kinds, swimming, etc. Occasionally it can be directly caused by a fall on the outstretched hand or may be due to the congenital shape of the acromion process reducing the vertical height of the subacromial space and producing impingement. Altered joint mechanics, posture, incorrect or overtraining and muscle imbalances which affect the steering mechanism of the rotator cuff tendons are all factors which may contribute to chronic bursitis at the shoulder.
The patient complains of a low-grade ache over the insertion of deltoid and may not be able to sleep on that side at night. On examination there is a non-capsular pattern of movement, often with pain felt at the end of range of passive elevation. A painful arc may be present and various resisted tests may also produce the pain. The room in the subacromial space is minimal and impingement under the coracoacromial arch may inflame the bursa, producing a painful arc on movement.
The application of resisted tests produces some compression of the glenohumeral joint and subacromial space. This produces a characteristic muddle of signs associated with a bursitis. The pain may be on the application of resistance, on the release of resistance or may produce several positive signs, e.g. pain on resisted abduction, lateral rotation and elbow extension. The resisted tests may not be consistent and on reassessment of the patient a completely different set of resisted tests may be present.
Treatment, ideally, consists of an injection of a large volume of low-dose local anaesthetic together with an appropriate amount of corticosteroid.
Position the patient comfortably in sitting with the arm hanging by the side. Locate the midpoint of the lateral border of the acromion and insert the needle just below, at an oblique angle upwards with respect to the acromion (Fig. 5.32). Insert the needle and deliver the injection as a bolus, having detected the area, or areas, of less resistance (Fig. 5.33). The synovial folds and adhesions within the bursa may present a resistance to the injection and it may be necessary to deliver the injection by a series of horizontal withdrawals and reinsertions once the needle is in place. The patient is advised to maintain a period of relative rest for approximately 2 weeks following injection.
According to Beals et al (1998), the bursa lies under the anterior half of the acromion, so accurate needle placement is important. Nonetheless, a posterior approach is selected in preference by some clinicians, as there is more room to gain access to the subacromial space. Any difference in outcomes by using the different approaches has still to be tested.
As mentioned above, it may be difficult to distinguish chronic subacromial bursitis from chronic rotator cuff tendinopathy and injection into the subacromial space may be an appropriate choice of treatment when the dilemma occurs.
Attention should be paid to the mechanism by which the bursa becomes involved, as described above. An explanation is given to the patient together with restoration of balanced forces, aiming to ensure normal shoulder movement and to avoid excessive superior translation.
CONTRACTILE LESIONS
The more common contractile lesions at the shoulder involve the rotator cuff tendons, particularly supraspinatus. Rotator cuff lesions can vary from simple tendinopathy to degeneration and partial or complete thickness tears. The lesion may be secondary to subacromial impingement and may also involve the subacromial bursa and tendon of the long head of the biceps, which all lie in very close proximity. Tendinopathy may lead to secondary capsulitis through abnormal movement patterns due to pain.
Tendinopathy occurs from the cumulative effects of microtrauma which has a gradual onset, usually due to overuse. Single traumatic incidents may produce tendinopathy but this is unusual, and the effect of trauma in this case is more likely to cause tearing of an already degenerate tendon. Other causes can be abnormalities in the tendon itself or fatigue failure of muscles that provide support mechanisms for the humeral head in the glenoid. This can follow prolonged repetitive over-the-shoulder physical loads, poor posture and vibration (Alvarez-Nemegyei & Canoso 2003). September et al (2007) have also explored a genetic component, noting that, relative to a control group, siblings have more than twice the risk of developing rotator cuff tears and nearly five times the risk of experiencing symptoms.
Pain is localized to the deltoid area and, although the patient may be aware of a vague ache, the pain is increased considerably by use and movements such as reaching, pushing and pulling, in particular those activities associated with using the hands above shoulder level.
On examination, pain is reproduced on the appropriate resisted test and there may be localizing signs of a painful arc and/or positive scarf test. Resisted abduction may implicate supraspinatus, resisted lateral rotation may implicate infraspinatus and teres minor, and resisted medial rotation may implicate subscapularis. However, as discussed above, the tendons interdigitate and insert to form a tendinous cuff; therefore it can be difficult to differentiate between the tendons and it may not be possible to make a definitive diagnosis.
Two or more resisted tests may be positive and subsequent palpation will determine the site of the lesion. Passive movements should be of full range with a normal end-feel, but occasionally the opposite passive movement or end-range passive elevation reproduces the pain by stretching or compressing the tendinous insertion respectively. A further complication may be a secondary capsulitis, in which case a capsular pattern will be superimposed on the non-capsular pattern described above.
Early onset of tendinopathy may respond to conservative treatment and corticosteroid injection into the adjacent subacromial bursa, or transverse frictions may be successful. Extracorporeal shock wave therapy lithotripsy, previously used to shatter stones in the kidney, bladder, ureters and gall bladder, has emerged as an appropriate treatment for calcific tendonitis and has also shown promise in the treatment of tendinopathies (Hsu et al 2008). The mechanism of how lithotripsy acts or is beneficial is not fully understood. It has been shown to enhance neovascularization at the tendon–bone junction with early release of growth and proliferating factors which lead to improved blood supply and tissue regeneration.
Tendinopathy involves focal degenerative changes within the tendon leading to partial or full thickness tears; further complications may include involvement of the nearby subacromial bursa or biceps tendon, or involve subtle instability or lesions of the glenoid labrum.
The aim of treatment for rotator cuff tendinopathy is to relieve pain and to restore full functional movement to the shoulder, the resisted tests often proving weak and painful. This weakness may be due to tears or muscle inhibition due to pain. The cause of the lesion should be determined and factors such as instability and muscle imbalance should be addressed, with the rehabilitation of movement patterns to ensure restoration of the dynamic stabilizing function of the rotator cuff. Excessive superior and anterior translation should be prevented, to avoid the long-term complications of impingement which may eventually lead to surgery.
Supraspinatus tendinopathy
MRI is highly accurate in detecting full thickness tears of the rotator cuff with a specificity as high as 95%. It is less accurate at detecting partial thickness tears although this is improving with continuing development in technology (J. Smith, unpublished study 2008).
The role of MRI in identifying supraspinatus tendinopathy is uncertain. Sein et al (2007) set out to determine intraobserver and interobserver reliability when identifying supraspinatus tendinosis on MRI. The result was that a well-trained single observer could identify and grade supraspinatus tendinosis with little variation but interobserver reliability was only fair to good. The link to symptoms may not be explicit in that some studies have identified abnormal signal intensity of supraspinatus in asymptomatic individuals (Lewis & Tennent 2007). This was not the case in this study, however, where supraspinatus tendinosis identified by MRI correlated well with positive impingement signs. The MRI images are therefore more relevant if they are supported by clinical findings.
Dalton (1994) reported that an area of hypovascularity in supraspinatus, 1 cm from its insertion, has been both proposed and disputed. A critical zone of vascular ischaemia has been proposed, existing between the supraspinatus tendon and the coracohumeral ligament, where degeneration and tears usually occur (Cailliet 1991). The critical zone is said to vary from being ischaemic when the vascular anastomosis is constricted, to hyperaemic when it is allowed to flow freely. The vessels are elongated when the arm is hanging by the side and compressed when the rotator cuff tendons contract to produce movement, both potentially causing relative ischaemia. Hyperaemia is said to occur only when the arm is passively supported at rest.
Clark & Harryman (1992), however, studied cadaver shoulders aged between 17 and 70 years and found no avascular area in supraspinatus. The blood vessels in the deeper tendon layers were found to be small compared with those in the superficial layers. There was no associated evidence of degeneration and the authors concluded that the blood supply was adequate for the metabolic needs of the tissue.
A lesion in supraspinatus produces pain on resisted abduction. Weakness may also be present and it is difficult to be certain whether this is due to muscle inhibition because of the pain, or partial or full thickness tears of the tendon. A painful arc or pain at the end of range of passive elevation localizes the lesion to the distal end of the tendon, usually at the teno-osseous junction. If pain is produced on resisted abduction only, without this localizing sign, the lesion is probably at the musculotendinous junction. Either way, palpation will confirm the exact site of the lesion.
Currently the whole question of tendinopathy is under debate with inflammation disputed as a component of the problem and degeneration of the tendon proposed as the cause. This leads to questions being asked with regard to the prognosis for the patient. An inflammatory problem is expected to resolve with treatment in up to approximately 3 weeks; a degenerative problem will take much longer (see discussion in Ch. 3). Furthermore, if the pathology of rotator cuff tendinopathy is degenerative, more questions are raised, such as why corticosteroid injection relieves pain. Khan & Cook (2000) acknowledge that clinical experience and some studies show that corticosteroid injection produces short-term relief of pain in these lesions although the mechanisms for this pain relief are currently not known.
The following treatment techniques of injection and transverse frictions may be successful, but they do not stand alone and should be incorporated into a holistic treatment programme in which all components of the patient’s problem are addressed, including eliminating the possible cause. Injection of the individual tendons may be appropriate, as discussed below, but there is growing controversy on whether this could contribute to degenerative change, leading to tendon rupture, although the current evidence does not support this.
Hollingworth et al (1983) compared two methods of corticosteroid injection with local anaesthetic to various shoulder joint or tendon lesions. One method was injection accurately placed anatomically into the lesion, based on diagnosis by selective tension, and the other involved injection into the trigger point or the point most tender to palpation. The anatomical injection group gave 60% success compared with the tender or trigger point group, which gave 20% success.
Alvarez-Nemegyei & Canoso (2003) reported successful treatment of rotator cuff tendinopathy with corticosteroid subacromial injection when compared with placebo. Matthews & Glousman (2004) claimed that accurate steroid placement demonstrated radiographically is associated with improved clinical benefit at a 2-week evaluation and Chen et al (2006) also described improved abduction range if injection into the subacromial bursa is carried out under ultrasound guidance compared to a blind injection.
However, the need for specificity in subacromial injection for rotator cuff disease was disputed by a study by Ekeberg et al (2009) who compared subacromial ultrasound-guided injection with systemic gluteal steroid injection and found no important differences in the short-term outcomes. There was modest improvement in both groups. Weaknesses of the study were acknowledged in that there was no sham injection group to examine the effect of placebo, the injecting physician was not blinded and the dose used of 20 mg triamcinolone acetonide might have been regarded as a low dose for the systemic treatment. It could also be claimed that the dose was towards the low end for that recommended for the subacromial bursa injection but the role of the local anaesthetic included in the injection should also be considered as a possible contributor to the modest improvement noted.
As mentioned above, injection into the teno-osseous junctions of the individual tendons is controversial and a direct link with tendon rupture has been proposed but not proven. A consensus of opinion is hard to pin down and there appears to be a range of practice between those who continue to inject into the tendon itself in younger patients, where the good health of the tendon is assumed, and those who would always use an injection into the subacromial bursa to be able to bathe the intimately related tissues, whilst avoiding direct infiltration of the tendon structure. An ultrasound scan of the tendons prior to injection of the teno-osseous junction, to establish the state of degeneration of the tendons, is common practice. To exercise caution, a generic injection into the subacromial bursa may be more appropriate, particularly if impingement of the degenerate tendons produces inflammation in the subacromial space. It may be wise to exploit the effectiveness of a subacromial injection before considering injection of individual tendon insertions.
Hanchard et al (2004) note the absence of good quality evidence to support the use of injections in the treatment of subacromial impingement syndrome and, in light of the associated risks, take the view that conservative treatment should precede the use of injections unless severe pain is present. This supports the case for treating the rotator cuff tendons with frictions first, as part of a programme of physiotherapy management, and to leave injection as the second option rather than the ‘treatment of choice’.
It is up to suitably qualified clinicians to exercise judgment based on current best practice and also having ascertained the views of their local orthopaedic consultants.
Suggested needle size: 25G × 5/8 in (0.5 × 16 mm) orange needle or 23G × 1 in (0.6 × 25 mm) blue needle
Dose: 10 mg triamcinolone acetonide in a total volume of 1 mL
Position the patient in sitting at an angle of 45°, medially rotating the shoulder and placing the arm behind the back to expose the tendon insertion (Fig. 5.37). Insert the needle perpendicular to the teno-osseous junction and deliver the injection using a peppering technique (Fig. 5.38). The patient is advised to maintain a period of relative rest for approximately 2 weeks following injection.
 |
| Figure 5.37
Injection of the supraspinatus tendon.
|
 |
| Figure 5.38
Injection of the supraspinatus tendon showing direction of approach and needle position.
|
Transverse frictions to supraspinatus (Cyriax 1984, Cyriax & Cyriax 1993)
Teno-osseous junction
Position the patient as above. Stand at the side of the patient and identify the area of tenderness. Place an index finger, reinforced by the middle finger, onto the tendon and direct the pressure down onto the insertion (Fig. 5.39). Deliver the frictions transversely across the fibres, keeping the index finger parallel to the anterior edge of the acromion process. The supraspinatus tendon is approximately one finger’s width (1 cm). Maintain the technique for 10 min after the analgesic effect has been achieved. Relative rest is advised where functional movements may continue, but no overuse or stretching until pain-free on resisted testing.
 |
| Figure 5.39
Transverse frictions to the supraspinatus tendon, teno-osseous site.
|
Musculotendinous junction
Position the patient in sitting with the painful shoulder abducted to 90° and supported comfortably on the couch. Stand on the opposite side of the patient but facing forwards with your arm straight across and behind the patient’s shoulders. Locate the musculotendinous junction in the ‘V’ created by the clavicle and the acromion process (Fig. 5.40). Using the middle finger reinforced by the index finger, direct the pressure down onto the tendon and deliver the transverse frictions by rotating the forearm for 10 min after the analgesic effect has been achieved. Relative rest is advised where functional movements may continue, but no overuse or stretching until pain-free on resisted testing.
 |
| Figure 5.40
Transverse frictions to the supraspinatus tendon, musculotendinous junction.
|
Infraspinatus tendinopathy (+ teres minor)
A lesion in infraspinatus and teres minor produces pain on resisted lateral rotation. A painful arc and pain at the end of range of passive elevation indicate that the lesion lies at the distal end of the tendon, usually at the teno-osseous junction. If no arc is present the lesion is often a little further proximally in the body of the tendon. Palpation will confirm the exact site of the lesion.
The position shown for the injection (Fig. 5.41) may be uncomfortable for the patient to maintain and the position described here is preferable. The principles of injection are the same. Position the patient in side-lying with the head raised on two pillows (or one folded), the hand resting on the cheek and the forearm free to allow the elbow to drop down below the shoulder. This laterally rotates and adducts the affected arm to expose the greater tuberosity (Fig. 5.43). Locate the area of tenderness over the greater tuberosity, which now lies approximately two fingers’ width below to the posterior angle of the acromion. Insert the needle and deliver the injection by a peppering technique to the whole extent of the lesion, which may be up to 2–3 cm wide (Fig. 5.42). The patient is advised to maintain a period of relative rest for approximately 2 weeks following injection.
 |
| Figure 5.41
Injection of the infraspinatus tendon.
|
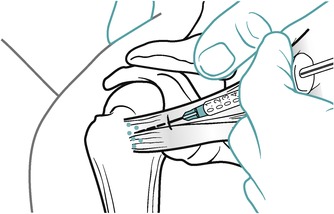 |
| Figure 5.42
Injection of the infraspinatus tendon showing direction of approach and needle position.
|
 |
| Figure 5.43
Transverse frictions to the infraspinatus tendon (and position for injection).
|
Transverse frictions to infraspinatus (Cyriax 1984, Cyriax & Cyriax 1993)
Position the patient as above (Fig. 5.43), or the alternative position can be used if it can be tolerated by the patient (Fig. 5.44). Locate the area of tenderness and place a thumb on the area parallel to the direction of the tendon fibres; reinforce this with the other thumb (Fig. 5.44).
 |
| Figure 5.44
Alternative position for transverse friction massage of the infraspinatus tendon.
|
Standing back to apply body weight, press down onto the tendon and deliver a transverse sweep across the fibres, aiming to touch the posterior angle of the acromion with each stroke. The infraspinatus is two fingers (2 cm) wide; if teres minor is involved, the sweep should cover a width of three fingers (3 cm). Ten minutes’ friction is delivered after achieving the analgesic effect. Relative rest is advised where functional movements may continue, but no overuse or stretching until pain-free on resisted testing.
If the lesion lies in the body of the tendon, the technique for transverse frictions is the same, but applied a little more proximally at the site of the lesion, identified by palpation.
Subscapularis tendinopathy
A lesion in subscapularis produces pain on resisted medial rotation. A painful arc indicates a lesion in the upper fibres; a positive scarf test indicates a lesion in the lower fibres. Palpation will confirm the exact site of the lesion, which may cover a large area of tendon, i.e. approximately three fingers (3 cm) wide.
Position the patient in sitting with the arm supported to allow the humerus to rest in the anatomical position (Fig. 5.45). Locate the lesser tuberosity and deliver the injection by peppering technique to the full width of the lesion at the insertion onto the lesser tuberosity (Fig. 5.46). The patient is advised to maintain a period of relative rest for approximately 2 weeks following injection.
 |
| Figure 5.45
Injection of the subscapularis tendon.
|
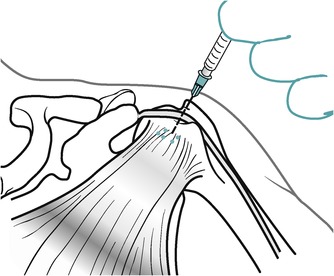 |
| Figure 5.46
Injection of the subscapularis tendon showing direction of approach and needle position.
|
Transverse frictions to subscapularis (Cyriax 1984, Cyriax & Cyriax 1993)
Position the patient as above and locate the area of tenderness (upper fibres, lower fibres or both) on the medial aspect of the lesser tuberosity (Fig. 5.47). Place the thumb perpendicular to the direction of the fibres, parallel to the shaft of the humerus and directed laterally; deliver the transverse frictions in a supero-inferior direction transversely across the fibres. The subscapularis tendon is approximately three fingers wide (3 cm). If the full width of the tendon is affected it may be necessary to divide the area into two sites for treatment as it is difficult to friction across the entire structure and a blister may be raised. Ten minutes’ transverse frictions are delivered after the analgesic effect is achieved. Relative rest is advised where functional movements may continue, but no overuse or stretching until pain-free on resisted testing. The therapist’s position can be varied to give better access to the tendon (Fig. 5.48).
 |
| Figure 5.47
Transverse frictions to the subscapularis tendon.
|
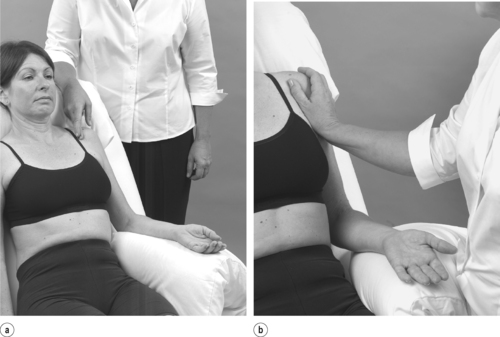 |
| Figure 5.48
Alternative positions for transverse frictions to the subscapularis tendon.
|
Tendinopathy of the long head of biceps
In its position in the subacromial space, the tendon of the long head of biceps may be involved in an impingement syndrome. It will produce pain felt at the shoulder on resisted elbow flexion. With the former lesion, a painful arc is usually present on forward flexion of the shoulder with a straight arm and the palm uppermost.
Position the patient in sitting with the arm supported so that the humerus rests in the anatomical position (Fig. 5.49). Locate the bicipital groove and slide the needle in, parallel to the groove (Fig. 5.50). Deliver the injection by a bolus technique alongside the tendon. The patient is advised to maintain a period of relative rest for approximately 2 weeks following injection.
 |
| Figure 5.49
Injection of the long head of biceps tendon.
|
 |
| Figure 5.50
Injection of the long head of biceps tendon showing direction of approach and needle position.
|
Transverse frictions to the long head of the biceps (Cyriax 1984, Cyriax & Cyriax 1993)
Position the patient as above and place a thumb parallel to the tendon in the groove, fingers wrapped around the arm for counterpressure (Fig. 5.51). Deliver the transverse frictions by alternately rotating the arm into medial and lateral rotation. Alternatively, the therapist may hold the patient’s arm stationary and deliver the friction by abducting and adducting the thumb. Relative rest is advised where functional movements may continue, but no overuse or stretching until pain-free on resisted testing.
 |
| Figure 5.51
Transverse frictions to the long head of biceps tendon.
|
REFERENCES
Ahn, K.; Lee, E.H.; Yang, S.M., Interventional micoadhesiolysis: a new nonsurgical release technique for adhesive capsulitis of the shoulder., BMC Musculoskelet. Disord. 9 (2008) 12.
Alvarez-Nemegyei, J.; Canoso, J., Evidence-based soft tissue rheumatology part 1. Subacromial impingement syndrome, J. Clin. Rheumatol. 9 (3) ( 2003) 193–199.
Anton, H.A., Frozen shoulder, Can. Fam. Physician 39 (1993) 1773–1777.
Beals, T.C.; Harryman, D.T.; Lazarus, M., Useful boundaries of the subacromial bursa, J. Arthroscopic Relat. Surg. 14 (5) ( 1998) 465–470.
Berg, E., Calcific tendinitis of the shoulder, Orthop. Nurs. 16 (6) ( 1997) 68–69.
Biundo, J.J.; Harris, M.A., Peripheral nerve entrapment, occupation-related syndromes and sports injuries, and bursitis, Curr. Opin. Rheumatol. 5 (1993) 224–229.
Brukner, P.; Khan, K., Clinical Sports Medicine. 3rd edn. ( 2007)McGraw-Hill, Sydney.
Bunker, T.D.; Anthony, P.P., The pathology of frozen shoulder, J. Bone Joint Surg. 77B (1995) 677–683.
Bunker, T.D.; Reilly, J.; Baird, K.S.; et al., Expression of growth factors, cytokines and matrix metalloproteinases in frozen shoulder., J. Bone Joint Surg. 82B (2000) 768–773.
Burkhart, S.S., Congenital subacromial stenosis, J. Arthroscopic Relat. Surg. 11 (1995) 63–68.
Burns, W.C.; Whipple, T.L., Anatomic relationships in the shoulder impingement syndrome, Clin. Orthop. Relat. Res. 294 (1993) 96–102.
Cailliet, R., Shoulder Pain. 3rd edn. ( 1991)F A Davis, Philadelphia.
Calis, M.; Kenan, A.; Birtane, M., Diagnostic values of clinical diagnostic tests in subacromial impingement syndrome, Ann. Rheum. Dis. 59 (2000) 44–47.
Cameron, G., The shoulder is a weight-bearing joint: implications for clinical practice, J. Orthop. Med. 17 (1995) 46–50.
Chen, M.J.; Lew, H.L.; Hsu, T.C.; et al., Ultrasound-guided shoulder injections in the treatment of musculoskeletal disorders: current perspectives and future prospects, Clin. J. Pain 17 (2006) 25–32.
Clark, J.M.; Harryman, D.T., Tendons, ligaments and capsule of the rotator cuff, J. Bone Joint Surg. 74A (1992) 713–725.
Clarnette, R.G.; Miniaci, A., Clinical examination of the shoulder, Med. Sci. Sports Exerc. 30 (4 Suppl.) ( 1998) S1–S6.
Cooper, D.E.; O’Brien, S.J.; Warren, R.F., Supporting layers of the glenohumeral joint: an anatomic study, Clin. Orthop. Relat. Res. 289 (1993) 144–155.
Copeland, S., Throwing injuries of the shoulder, Br. J. Sports Med. 27 (1993) 221–227.
Cyriax, J., 8th edn.Textbook of Orthopaedic Medicine. vol. 1 ( 1982)Baillière Tindall, London.
Cyriax, J., 11th edn.Textbook of Orthopaedic Medicine. vol. 2 ( 1984)Baillière Tindall, London.
Cyriax, J.; Cyriax, P., Cyriax’s Illustrated Manual of Orthopaedic Medicine. ( 1993)Butterworth Heinemann, Oxford.
Dalton, S.E., The conservative management of rotator cuff disorders, Br. J. Rheumatol. 33 (1994) 663–667.
Di Mario, M.; Fraracci, L., MR study of the intrinsic acromial angle in 74 symptomatic patients, Radiol. Med. 110 (3) ( 2005) 273–279.
Ekeberg, O.M.; Bautz-Holter, E.; Tveitå, E.K., Subacromial ultrasound guided or systemic steroid injection for rotator cuff disease: randomised double blind study, Br. Med. J. 338 (2009) 273–276.
Farley, T.E.; Neumann, C.H.; Steinbach, L.S.; et al., The coracoacromial arch – MR evaluation and correlation with rotator cuff pathology, Skeletal Radiol. 23 (1994) 641–645.
Flatow, E.L.; Soslowsky, L.J.; Ticker, J.B.; et al., Excursion of the rotator cuff under the acromion, Am. J. Sports Med. 22 (1994) 779–788.
Frame, M.K., Anatomy and biomechanics of the shoulder, In: (Editor: Donatelli, R.A.) Clinics in Physical Therapy, Physical Therapy of the Shoulder ( 1991)Churchill Livingstone, Edinburgh, pp. 1–18.
Frieman, B.G.; Albert, T.J.; Fenlin, J.M., Rotator cuff disease – a review of diagnosis, pathophysiology and current trends in treatment, Arch. Phys. Med. Rehabil. 75 (1994) 604–609.
Fukuda, H.; Hamada, K.; Nakajima, T.; et al., Pathology and pathogenesis of the intratendinous tearing of the rotator cuff viewed from en bloc histologic sections, Clin. Orthop. Relat. Res. 304 (1994) 60–67.
Funk L., 2007. Frozen Shoulder. Online. Available: http://www.shoulderdoc.co.uk (17.03.09).
Funk, L., Frozen Shoulder, Int. Musculoskelet. Med. 31 (1) ( 2008) 36–39.
Greenfield, B.; Catlin, P.A.; Coats, P.W.; et al., Posture in patients with shoulder overuse injuries in healthy individuals, J. Orthop. Sports Phys. Ther. 21 (1995) 287–295.
Grubbs, N., Frozen shoulder syndrome – a review of the literature, J. Orthop. Sports Phys. Ther. 18 (1993) 479–487.
Guanche, C.A.; Jones, D.C., Clinical testing for tears of the glenoid labrum, J. Arthroscopic Relat. Surg. 19 (5) ( 2003) 517–523.
Halder, A.M.; An, K.-N., Anatomy and biomechanics of the shoulder, Orthop. Clin. N. Am. 31 (2) ( 2000) 159–176.
Hanchard, N.; Cummins, J.; Jeffries, C., Evidence-based clinical guidelines for the diagnosis, assessment and physiotherapy management of shoulder impingement syndrome, Chartered Society of Physiotherapy, London ( 2004).
Hartley, A., Practical Joint Assessment, Upper Quadrant. 2nd edn. ( 1995)Mosby, London.
Hattam, P.; Smeatham, A., Special Tests in Musculoskeletal Examination. ( 2010)Churchill Livingstone, Edinburgh.
Hollingworth, G.R.; Ellis, R.; Hattersley, T.S., Comparison of injection techniques for shoulder pain – results of a double blind, randomized study, Br. Med. J. 287 (1983) 1339–1341.
Hsu, S.Y.C.; Chan, K.M., Arthroscopic distension in the management of frozen shoulder, Int. Orthop. 15 (1991) 79–83.
Hsu, C.J.; Wang, D.Y.; Tseng, K.F.; et al., Extracorporeal shock wave therapy for calcifying tendinitis of the shoulder, J. Shoulder Elbow Surg. 17 (1) ( 2008) 55–59.
Hulstyn, M.J.; Fadale, P.D., Arthroscopic anatomy of the shoulder, Orthop. Clin. N. Am. 26 (1995) 597–612.
Hulstyn, M.J.; Weiss, A., Adhesive capsulitis of the shoulder, Orthop. Rev. 22 (1993) 425–433.
Iannotti, J.P., Evaluation of the painful shoulder, J. Hand Ther. 7 (1994) 77–83.
Itoi, E.; Newman, S.R.; Kuechle, D.K.; et al., Dynamic anterior stabilizers of the shoulder with the arm in abduction, J. Bone Joint Surg. 76B (1994) 834–836.
Jacobs, L.G.H.; Barton, M.A.J.; Wallace, W.A.; et al., Intra-articular distension and steroids in the management of capsulitis of the shoulder, Br. Med. J. 302 (1991) 1498–1501.
Jeracitano, D.; Cooper, R.; Lyon, L.J.; et al., Abnormal temperature control suggesting sympathetic dysfunction in the shoulder skin of patients with frozen shoulder, Br. J. Rheumatol. 31 (1992) 539–542.
Jobe, F.W.; Pink, M., Classification and treatment of shoulder dysfunction in the overhead athlete, J. Orthop. Sports Phys. Ther. 18 (1993) 427–432.
Jobe, F.W.; Pink, M., The athlete’s shoulder, J. Hand Ther. 7 (1994) 107–110.
Johansson, K.; Ivarson, S., Intra- and interexaminer reliability of four manual shoulder maneuvers used to identify subacromial pain, Man. Ther. 14 (2009) 231–239.
Jost, B.; Koch, P.; Gerber, C., Anatomy and functional aspects of the rotator interval, J. Shoulder Elbow Surg. 9 (4) ( 2000) 336–341.
Kapandji, I.A., The Physiology of the Joints, Upper Limb. 5th edn ( 1982)Churchill Livingstone, Edinburgh.
Khan, K.M.; Cook, J.L., Overuse tendon injuries: where does the pain come from, Sports Med. Arthroscopic Rev. 8 (2000) 17–31.
Lewis, J.S.; Tennent, T.D., How effective are diagnostic tests for the assessment of rotator cuff disease of the shoulder? In: (Editors: MacAuley, D.; Best, T.M.) Evidenced Based Sports Medicine2nd edn ( 2007)Blackwell Publishing, London.
Lundberg, B.J., The frozen shoulder, Acta Orthop. Scand. Suppl. 119 (1969) 1–59.
McCann, P.D.; Bigliani, L.U., Shoulder pain in tennis players, Sports Med. 17 (1994) 53–64.
Matthews, P.; Glousman, R., Accuracy of subacromial injection: anterolateral versus posterior approach, J. Shoulder Elbow Surg. 86A (2004) 219–224.
Meister, K.; Andrews, J.R., Classification and treatment of rotator cuff injuries in the overhead athlete, J. Orthop. Sports Phys. Ther. 18 (1993) 413–421.
Michener, L.; Walsworth, M.; Burnet, E., Effectiveness of rehabilitation for patients with subacromial impingement syndrome: a systematic review, J. Hand Ther. 17 (2) ( 2004) 152–163.
Mohtadi, N.; Vellet, D.; Clark, M.; et al., A prospective double blind comparison of magnetic resonance imaging and arthroscopy in the evaluation of patients presenting with shoulder pain, J. Shoulder Elbow Surg. 13 (3) ( 2004) 258–265.
Munro, W.; Healy, R., The validity and accuracy of clinical tests used to detect labral pathology of the shoulder – a systematic review, Man. Ther. 14 (2009) 119–130.
Neer, C.S., Impingement lesions, Clin. Orthop. Relat. Res. 173 (1983) 70–77.
Netter, F.H., Musculoskeletal System Part I. Ciba Collection of Medical Illustrations. vol. 8 ( 1987)Ciba-Giegy, New Jersey.
Nordin, M.; Frankel, V.H., Basic Biomechanics of the Musculoskeletal System. 3rd edn ( 2001)Lippincott, Williams & Wilkins, Philadelphia.
Ogilvie-Harris, D.J.; Biggs, D.J.; Fistsialos, D.P.; et al., The resistant frozen shoulder: manipulation versus arthroscopic release, Clin. Orthop. Relat. Res 319 (1995) 238–248.
Owens-Burkhart, H., Management of frozen shoulder, In: (Editor: Donatelli, R.A.) Clinics in Physical Therapy, Physical Therapy of the Shoulder ( 1991)Churchill Livingstone, Edinburgh, pp. 91–116.
Paine, R.M.; Voight, M., The role of the scapula, J. Orthop. Sports Phys. Ther. 18 (1993) 386–391.
Palastanga, N.; Field, D.; Soames, R., Anatomy and Human Movement. 5th edn. ( 2006)Butterworth-Heinemann, Edinburgh.
Pellecchia, G.L.; Paolino, J.; Connell, J., Intertester reliability of the Cyriax evaluation in assessing patients with shoulder pain, J. Orthop. Sports Phys. Ther. 23 (1996) 34–38.
Petersilge, C.A.; Witte, D.H.; Sewell, B.O.; et al., Normal regional anatomy of the shoulder, MRI Clin. N. Am. 5 (4) ( 1997) 667–680.
Pratt, N.E., Anatomy and biomechanics of the shoulder, J. Hand Ther. 7 (1994) 65–76.
Richards, D.P.; Burkhart, S.S.; Campbell, S.E., Relation between narrowed coracohumeral distance and subscapularis tears, Arthroscopy 21 (100) ( 2005) 1223–1228.
Saunders, S., Orthopaedic Medicine Course Manual. ( 2000)Saunders, London.
Schulte, K.R.; Warner, J.J.P., Uncommon causes of shoulder pain in the athlete, Orthop. Clin. N. Am. 26 (1995) 505–528.
Sein, M.L.; Walton, J.; Linklater, J.; et al., Reliability of MRI assessment of supraspinatus tendinopathy, Br. J. Sports Med. 41 (4) ( 2007) 227–231.
September, A.V.,, Tendon and ligament injuries: the genetic component, Br. J. Sports Med. 41 (4) ( 2007) 241–246.
Shaffer, B.; Tibone, J.E.; Kerlan, R.K., Frozen shoulder – a long term follow-up, J. Bone Hand Surg. 74A (1992) 738–746.
Sharma, R.K.; Bajekal, R.A.; Bhan, S., Frozen shoulder syndrome, Int. Orthop. 17 (1993) 275–278.
Siegel, L.B.; Cohen, N.J.; Gall, E.P., Adhesive capsulitis: a sticky issue, Am. Fam. Physician 59 (1) ( 1999) 1843–1852.
Smith, S.P.; Devaraj, V.S.; Bunker, T.D., The association between frozen shoulder and Dupuytren’s disease, J. Shoulder Elbow Surg. 10 (2) ( 2001) 149–151.
Speer, K.P., Anatomy and pathomechanics of shoulder instability, Clin. Sports Med. 14 (1995) 751–760.
Stam, H.W., Frozen shoulder – a review of current concepts, Physiotherapy 80 (1994) 588–598.
Standring, S., Gray’s Anatomy: The Anatomical Basis of Clinical Practice. 40th edn ( 2009)Churchill Livingstone, Edinburgh.
Stenlund, B., Shoulder tendinitis and osteoarthrosis of the acromioclavicular joint and their relation to sports, Br. J. Sports Med. 27 (1993) 125–130.
Uhthoff, K.J.; Sarkar, K., Periarticular soft tissue conditions causing pain in the shoulder, Curr. Opin. Rheumatol. 4 (1992) 241–246.
Uitvlugt, G.; Detrisac, D.A.; Johnson, L.J.; et al., Arthroscopic observations before and after manipulation of frozen shoulder, J. Arthroscop. Relat. Surg. 9 (1993) 181–185.
Wadsworth, C.T., Frozen shoulder, Phys. Ther. 66 (1986) 1878–1883.
Ward, W.G.; Eckardt, J.J., Subacromial/subdeltoid bursa abscesses, an overlooked diagnosis, Clin. Orthop. Relat. Res. 288 (1993) 189–194.
Wiley, A.M., Arthroscopic appearance of frozen shoulder, J. Arthroscopic Relat. Surg. 7 (1991) 138–143.
Wilk, K.E.; Arrigo, C., Current concepts in the rehabilitation of the athletic shoulder, J. Orthop. Sports Phys. Ther. 18 (1993) 365–378.