Chapter 1 The Scope of the EMG Examination
Electromyography (EMG) is a term that was first coined by Weddell et al in 1943 to describe the clinical application of needle electrode examination of skeletal muscles. Since then, and at least in North America, the nomenclature “EMG” or “clinical EMG” has been used by physicians to refer to the electrophysiologic examination of peripheral nerve and muscle that include the nerve conduction studies (NCS) as well as the needle evaluation of muscles. These terms continue to cause confusion that hinders communication among physicians and healthcare workers. Some physicians refer to the study as EMG/NCS, reserving the name EMG solely to the needle EMG evaluation and adding the term NCS to reflect the nerve conduction studies separately. Others have used the title needle EMG or needle electrode examination to reflect the needle evaluation of muscles, while keeping the term EMG to describe the entire evaluation of nerve and muscle. More recently, a nonspecific term, the “electrodiagnostic (EDX) examination,” has gained popularity to serve as an umbrella covering both the needle EMG and NCS. Other nomenclature used worldwide includes the electrophysiologic examination, which may be confused with the cardiac electrophysiological studies, and the electroneuromyographic (ENMG) examination which is the most accurate description of the study, yet unfortunately not widely used. Finally, physicians performing and interpreting these studies are called electromyographers (EMGers), electrodiagnosticians, or EDX consultants.
The EDX examination comprises a group of tests that are usually complementary to each other and often nec-essary to diagnose or exclude a neuromuscular problem (Table 1-1). These include principally the nerve conduction studies (NCS), that are sensory, motor, or mixed, and the needle EMG, sometimes referred as “conventional” or “routine” needle EMG to distinguish this test from other needle EMG studies including single fiber EMG and quantitative EMG. Also, “concentric” or “monopolar” needle EMG is sometimes utilized to reflect the type of needle electrode used. In addition to the two main components of the EMG examination, three late responses are often incorporated with the NCSs and have become an integral part of the NCSs. These include the F waves also referred to as F responses, the H reflexes also known as H responses, and the blink reflexes. Two specialized tests are often added to the routine EDX study mainly in patients with suspected neuromuscular junction disorders. These include the repetitive nerve stimulations and the single fiber EMG. Finally, a group of specialized studies that require special expertise as well as sophisticated equipment and software, used as a clinical and research tool in the assessment of the microenvironment of the motor unit, include motor unit action potential (MUAP) morphology analysis, MUAP turns and amplitudes analysis, macro EMG, motor unit number estimate (MUNE), and near-nerve recording studies.
Table 1-1 The Spectrum of Clinical Electromyography (Electrodiagnosis)
THE REFERRAL PROCESS TO THE EMG LABORATORY
Patients are referred to the EMG laboratory for EDX studies following a clinical assessment by a physician who suspects a disorder of the peripheral nervous system. For example, a patient with intermittent hand paresthesias and positive Phalen’s signs may be referred to the EMG laboratory to evaluate a possible carpal tunnel syndrome. The background and specialty of the referring physician plays a significant role in the planning and execution of the EDX study. In the experience of this author, this usually follows one of these three scenarios:
THE EMG LABORATORY PROCEDURES
Testing an Adult
Patients referred to the EMG laboratory should have a referral form completed by the referring physician with relevant clinical information and preferably a pertinent neurological differential diagnosis (Figure 1-1). Referring physicians should also describe the EDX study to their adult patients, particularly in regard to the discomfort associated with it, without creating unnecessary heightened anxiety. If unclear about the technical details of the procedure, they should encourage their patients to contact the EMG laboratory prior to the test date, to get a verbal or written description of the procedure. Such written descriptions should be widely available in all referring physicians’ offices (Table 1-2).
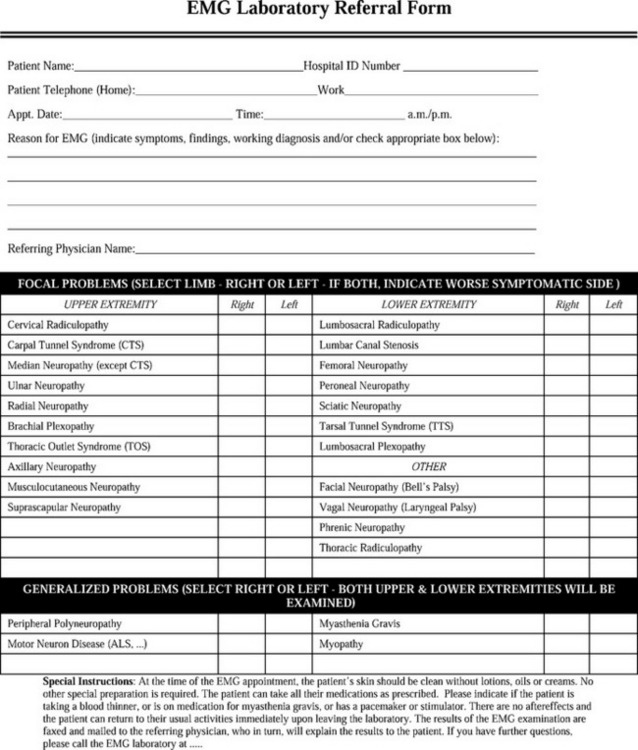
Figure 1-1 A sample of the referring request for an EMG examination.
(Adapted from Katirji B. The clinical electromyography examination. An overview. Neurol Clin N Am 2002;20:291–303.)
Table 1-2 A Sample of a Descriptive Explanation of the EMG Examination to be Given to Patients before Undergoing Testing
Reprinted with permission from Katirji B. The clinical electromyography examination. An overview. Neurol Clin N Am 2002;20:291–303.
The practice of electrodiagnosis is widely regarded as a practice of medicine. The electromyographer must have a good fund of knowledge of the anatomy, physiology, and disorders of the peripheral nervous system, and be familiar with the techniques that are necessary for performing the EDX study. Although a formal training in clinical EMG is necessary, the skills of the electromyograper are usually based on the number and type of patients studied. In practice, the electromyographer functions similar to a radiologist, by providing diagnostic studies directed by the patient clinical symptoms and working diagnosis. Hence, the EMG study should be as independent as possible, by providing an objective physiological assessment of the neuromuscular system.
Testing a Child
Sedation of young children, particularly those between the ages of 2 and 10 years, is advocated but still debated. Sedation has the advantage of allowing the performance of NCSs and repetitive nerve stimulation without any concern about movement artifacts. However, sedation has the disadvantage of rendering the needle EMG more difficult, if the child does not activate enough MUAPs needed for accurate analysis. In these situations, the evaluation of both MUAP morphology and recruitment may be suboptimal. Sedation of young children is not without risks and should be done under physician and nurse supervision and constant monitoring of vital signs and oxygenation. The use of chloral hydrate in the past was not always successful and occasionally resulted in deep and prolonged sedation. This drug has been replaced by agents that induce rapid hypnosis without excitation such as midazolam hydrochloride (Versed®) or propofol (Diprivan®).
Testing in the Intensive Care Unit
EDX testing of critically ill patients with suspected neuromuscular disorders in the intensive care unit (ICU) is often difficult and may be frustrating because of several limitations (Table 1-3). Particular attention should be given to the patient’s skin temperature since peripheral vasoconstriction is common and may lower skin temperature. A core temperature of greater than 36°C or skin temperature greater than 32°C should be aimed for, since lower temperatures result in slowing of distal latencies and conduction velocities. Excessive tissue edema may be associated with low amplitude sensory or motor responses or interferes with supramaximal stimulations and giving a false impression of axonal loss. The edema may be generalized (as with hypoalbunimemia) or limited to the legs (such as with congestive heart failure), hands (such as with extravasation of fluids from intravenous lines), or neck (such as following tracheostomy or central line placement). Many ICU patients have a bleeding diasthesis or are on anticoagulation that prevents extensive needle EMG testing. Excessive sweating, skin breakdown, central lines, pacemakers, monitoring devices, or communicable diseases also influence the type of procedure, the particular site, and extremity tested.
Table 1-3 Limitations of Electrodiagnostic Testing in the Intensive Care Unit
| Limitation | Result |
|---|---|
| Nerve conduction studies | |
| Cool extremities | Delayed distal latencies and conduction velocities |
| Edema | Low amplitude or unevoked sensory and motor responses |
| Excessive sweating | Artifacts and inadequate or unevoked responses |
| Skin breakdown | Inability to stimulate or record |
| Central line | Inability to stimulate near the line in fear of cardiac stimulation |
| Pacemaker | Inability to stimulate near the wires or pacer in fear of cardiac stimulation |
| Anterior neck swelling | Inability to percutaneously achieve supramaximal simulation of the phrenic nerves |
| Needle EMG | |
| Bleeding diasthesis | Inability to complete a thorough needle EMG |
| Coma or deep sedation | Inability to accurately assess MUAP morphology or recruitment |
| Agitation | Inability to accurately assess the insertional and spontaneous activities |
| Intubation/ventilation | Inability to turn the patient to needle test the paraspinal muscles |
In spite of these limitations, EDX testing, including needle EMG, NCS, and repetitive nerve stimulation, may be performed safely in the ICU, and often provide significant assistance in neuromuscular diagnosis and prognosis. Reviewing the history, physical examination, and medication history as well as discussing the queries and testing plan with the ICU team may prove beneficial to avoid possible pitfalls. Except in rare situations, the EDX tests done in the ICU are often less extensive than the studies done in the EMG laboratory, often with less NCS and needle EMG sampling. However, enough details are usually obtained to diagnose or exclude certain neuromuscular disorders that may be encountered in the ICU. In acute situations, serial studies are often necessary for final diagnosis and prognosis.
EMG LABORATORY REPORT
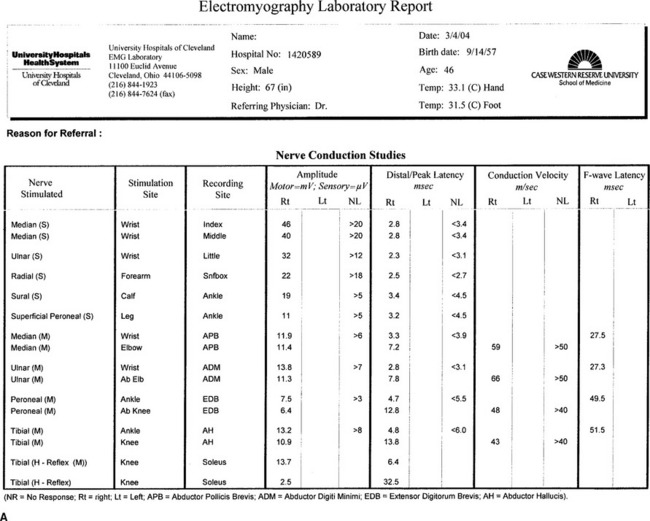
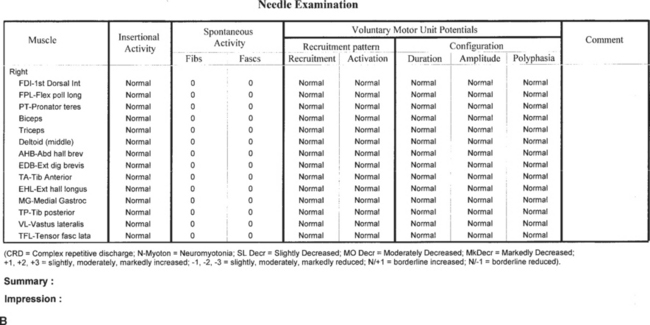
Generating a concise and understandable EMG laboratory report is an important function of the electromyographer. The EDX report should be typed (not hand written) since it constitutes an integral part of the patient’s medical records. The report should contain all the pertinent data acquired during the study, despite that some referring physicians are only interested in the final conclusion (Figure 1-2). In addition to the demographic data (patient name, age, birth date, sex, hospital number, date of study, and referring physician), the EMG laboratory report should include the following:
Aminoff MJ. Electromyography in clinical practice, 3rd ed. New York: Churchill-Livingstone, 1998.
Dumitru D. Electrodiagnostic medicine, 2nd ed. Philadelphia: Hanley and Belfus, 2001.
Katirji B. Clinical electromyography. In: Bradley WG, Daroff RB, Fenichel GM, Jankovic J, editors. Neurology in clinical practice. 4th ed. Boston: Butterworth-Heinemann; 2004:491-520.
Katirji B, editor. Clinical electromyography. Neurology clinics. Philadelphia: WB Saunders, 2002.
Katirji B. The clinical electromyography examination. An overview. Neurol Clin N Am. 2002;20:291-303.
Kimura J. Electrodiagnosis in diseases of nerve and muscle: principles and practice, 3rd ed. New York: Oxford University Press, 2001.
Preston DC, Shapiro BE. Electromyography and neuromuscular disorders. Philadelphia: Elsevier/Butterworth-Heinemann, 2005.
Shapiro BE, Katirji B, Preston DC. Clinical electromyography. In: Katirji B, Kaminski HJ, Preston DC, Ruff RL, Shapiro EB, editors. Neuromuscular disorders in clinical practice. Boston: Butterworth-Heinemann; 2002:80-140.
Smith SJM. Electrodiagnosis. In: Birch R, Bonney G, Wynn Parry CB, editors. Surgical disorders of the peripheral nerves. Edinburgh: Churchill-Livingstone; 1998:467-490.
Wilbourn AJ, Ferrante MA. Clinical electromyography. In: Joynt RJ, Griggs RC, editors. Baker’s clinical neurology on CD-ROM. Philadelphia: WB Saunders, 2000.