12e |
The Safety and Quality of Health Care |
Safety and quality are two of the central dimensions of health care. In recent years it has become easier to measure safety and quality, and it is increasingly clear that performance in both dimensions could be much better. The public is—with good justification—demanding measurement and accountability, and payment for services will increasingly be based on performance in these areas. Thus, physicians must learn about these two domains, how they can be improved, and the relative strengths and limitations of the current ability to measure them.
Safety and quality are closely related but do not completely overlap. The Institute of Medicine has suggested in a seminal series of reports that safety is the first part of quality and that the health care system must first and foremost guarantee that it will deliver safe care, although quality is also pivotal. In the end, it is likely that more net clinical benefit will be derived from improving quality than from improving safety, though both are important and safety is in many ways more tangible to the public. The first section of this chapter will address issues relating to the safety of care and the second will cover quality of care.
SAFETY IN HEALTH CARE
Safety Theory and Systems Theory Safety theory clearly points out that individuals make errors all the time. Think of driving home from the hospital: you intend to stop and pick up a quart of milk on the way home but find yourself entering your driveway without realizing how you got there. Everybody uses low-level, semiautomatic behavior for many activities in daily life; this kind of error is called a slip. Slips occur often during care delivery—e.g., when people intend to write an order but forget because they have to complete another action first. Mistakes, by contrast, are errors of a higher level; they occur in new or nonstereotypic situations in which conscious decisions are being made. An example would be dosing of a medication with which a physician is not familiar. The strategies used to prevent slips and mistakes are often different.
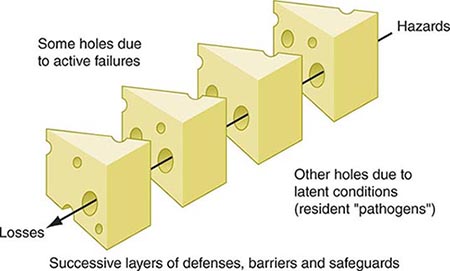
Systems theory suggests that most accidents occur as the result of a series of small failures that happen to line up in an individual instance so that an accident can occur (Fig. 12e-1). It also suggests that most individuals in an industry such as health care are trying to do the right thing (e.g., deliver safe care) and that most accidents thus can be seen as resulting from defects in systems. Systems should be designed both to make errors less likely and to identify those that do inevitably occur.
FIGURE 12e-1 “Swiss cheese” diagram. Reason argues that most accidents occur when a series of “latent failures” are present in a system and happen to line up in a given instance, resulting in an accident. Examples of latent failures in the case of a fall might be that the unit is unusually busy and the floor happens to be wet. (Adapted from J Reason: BMJ 320:768, 2000; with permission.)
Factors that Increase the Likelihood of Errors Many factors ubiquitous in health care systems can increase the likelihood of errors, including fatigue, stress, interruptions, complexity, and transitions. The effects of fatigue in other industries are clear, but its effects in health care have been more controversial until recently. For example, the accident rate among truck drivers increases dramatically if they work over a certain number of hours in a week, especially with prolonged shifts. A recent study of house officers in the intensive care unit demonstrated that they were about one-third more likely to make errors when they were on a 24-h shift than when they were on a schedule that allowed them to sleep 8 h the previous night. The American College of Graduate Medical Education has moved to address this issue by putting in place the 80-h workweek. Although this stipulation is a step forward, it does not address the most important cause of fatigue-related errors: extended-duty shifts. High levels of stress and heavy workloads also can increase error rates. Thus, in extremely high-pressure situations, such as cardiac arrests, errors are more likely to occur. Strategies such as using protocols in these settings can be helpful, as can simple recognition that the situation is stressful.
Interruptions also increase the likelihood of error and occur frequently in health care delivery. It is common to forget to complete an action when one is interrupted partway through it by a page, for example. Approaches that may be helpful in this area include minimizing interruptions and setting up tools that help define the urgency of an interruption.
Complexity represents a key issue that contributes to errors. Providers are confronted by streams of data (e.g., laboratory tests and vital signs), many of which provide little useful information but some of which are important and require action or suggest a specific diagnosis. Tools that emphasize specific abnormalities or combinations of abnormalities may be helpful in this area.
Transitions between providers and settings are also common in health care, especially with the advent of the 80-h workweek, and generally represent points of vulnerability. Tools that provide structure in exchanging information—for example, when transferring care between providers—may be helpful.
The Frequency of Adverse Events in Health Care Most large studies focusing on the frequency and consequences of adverse events have been performed in the inpatient setting; some data are available for nursing homes, but much less information is available about the outpatient setting. The Harvard Medical Practice Study, one of the largest studies to address this issue, was performed with hospitalized patients in New York. The primary outcome was the adverse event: an injury caused by medical management rather than by the patient’s underlying disease. In this study, an event either resulted in death or disability at discharge or prolonged the length of hospital stay by at least 2 days. Key findings were that the adverse event rate was 3.7% and that 58% of the adverse events were considered preventable. Although New York is not representative of the United States as a whole, the study was replicated later in Colorado and Utah, where the rates were essentially similar. Since then, other studies using analogous methodologies have been performed in various developed nations, and the rates of adverse events in these countries appear to be ~10%. Rates of safety issues appear to be even higher in developing and transitional countries; thus, this is clearly an issue of global proportions. The World Health Organization has focused on this area, forming the World Alliance for Patient Safety.
In the Harvard Medical Practice Study, adverse drug events (ADEs) were most common, accounting for 19% of all adverse events, and were followed in frequency by wound infections (14%) and technical complications (13%). Almost half of adverse events were associated with a surgical procedure. Among nonoperative events, 37% were ADEs, 15% were diagnostic mishaps, 14% were therapeutic mishaps, 13% were procedure-related mishaps, and 5% were falls.
ADEs have been studied more than any other error category. Studies focusing specifically on ADEs have found that they appear to be much more common than was suggested by the Harvard Medical Practice Study, although most other studies use more inclusive criteria. Detection approaches in the research setting include chart review and the use of a computerized ADE monitor, a tool that explores the database and identifies signals that suggest an ADE may have occurred. Studies that use multiple approaches find more ADEs than does any individual approach, and this discrepancy suggests that the true underlying rate in the population is higher than would be identified by a single approach. About 6–10% of patients admitted to U.S. hospitals experience an ADE.
Injuries caused by drugs are also common in the outpatient setting. One study found a rate of 21 ADEs per every 100 patients per year when patients were called to assess whether they had had a problem with one of their medications. The severity level was lower than in the inpatient setting, but approximately one-third of these ADEs were preventable.
The period immediately after a patient is discharged from the hospital appears to be very risky. A recent study of patients hospitalized on a medical service found an adverse event rate of 19%; about one-third of those events were preventable, and another one-third were ameliorable (i.e., they could have been made less severe). ADEs were the single leading error category.
Prevention Strategies Most work on strategies to prevent adverse events has targeted specific types of events in the inpatient setting, with nosocomial infections and ADEs having received the most attention. Nosocomial infection rates have been reduced greatly in intensive care settings, especially through the use of checklists. For ADEs, several strategies have been found to reduce the medication error rate, although it has been harder to demonstrate that they reduce the ADE rate overall, and no studies with adequate power to show a clinically meaningful reduction have been published.
Implementation of checklists to ensure that specific actions are carried out has had a major impact on rates of catheter-associated bloodstream infection and ventilator-associated pneumonia, two of the most serious complications occurring in intensive care units. The checklist concept is based on the premise that several specific actions can reduce the frequency of these issues; when these actions are all taken for every patient, the result has been an extreme reduction in the frequency of the associated complication. These practices have been disseminated across wide areas, in particular in the state of Michigan.
Computerized physician order entry (CPOE) linked with clinical decision support reduces the rate of serious medication errors, defined as those that harm someone or have the potential to do so. In one study, CPOE, even with limited decision support, decreased the serious medication error rate by 55%. CPOE can prevent medication errors by suggesting a default dose, ensuring that all orders are complete (e.g., that they include dose, route, and frequency), and checking orders for allergies, drug–drug interactions, and drug–laboratory issues. In addition, clinical decision support can suggest the right dose for a patient, tailoring it to level of renal function and age. In one study, patients with renal insufficiency received the appropriate dose only one-third of the time without decision support, whereas that fraction increased to approximately two-thirds with decision support; moreover, with such support, patients with renal insufficiency were discharged from the hospital half a day earlier. As of 2009, only ~15% of U.S. hospitals had implemented CPOE, but many plan to do so and will receive major financial incentives for achieving this goal.
Another technology that can improve medication safety is bar coding linked with an electronic medication administration record. Bar coding can help ensure that the right patient gets the right medication at the right time. Electronic medication administration records can make it much easier to determine what medications a patient has received. Studies to assess the impact of bar coding on medication safety are under way, and the early results are promising. Another technology to improve medication safety is “smart pumps.” These pumps can be set according to which medication is being given and at what dose; the health care professional will receive a warning if too high a dose is about to be administered.
The National Safety Picture Several organizations, including the National Quality Forum and the Joint Commission, have made recommendations for improving safety. In particular, the National Quality Forum has released recommendations to U.S. hospitals about what practices will most improve the safety of care, and all hospitals are expected to implement these recommendations. Many of these practices arise frequently in routine care. One example is “readback,” the practice of recording all verbal orders and immediately reading them back to the physician to verify the accuracy of what was heard. Another is the consistent use of standard abbreviations and dose designations; some abbreviations and dose designations are particularly prone to error (e.g., 7U may be read as 70).
Measurement of Safety Measuring the safety of care is difficult and expensive, since adverse events are, fortunately, rare. Most hospitals rely on spontaneous reporting to identify errors and adverse events, but the sensitivity of this approach is very low, with only ~1 in 20 ADEs reported. Promising research techniques involve searching the electronic record for signals suggesting that an adverse event has occurred. These methods are not yet in wide use but will probably be used routinely in the future. Claims data have been used to identify the frequency of adverse events; this approach works much better for surgical care than for medical care and requires additional validation. The net result is that, except for a few specific types of events (e.g., falls and nosocomial infections), hospitals have little idea about the true frequency of safety issues.
Nonetheless, all providers have the responsibility to report problems with safety as they are identified. All hospitals have spontaneous reporting systems, and, if providers report events as they occur, those events can serve as lessons for subsequent improvement.
Conclusions about Safety It is abundantly clear that the safety of health care can be improved substantially. As more areas are studied closely, more problems are identified. Much more is known about the epidemiology of safety in the inpatient setting than in outpatient settings. A number of effective strategies for improving inpatient safety have been identified and are increasingly being applied. Some effective strategies are also available for the outpatient setting. Transitions appear to be especially risky. The solutions to improving care often entails the consistent use of systematic techniques such as checklists and often involves leveraging of information technology. Nevertheless, solutions will also include many other domains, such human factors techniques, team training, and a culture of safety.
QUALITY IN HEALTH CARE
Assessment of quality of care has remained somewhat elusive, although the tools for this purpose have increasingly improved. Selection of health care and measurement of its quality are components of a complex process.
Quality Theory Donabedian has suggested that quality of care can be categorized by type of measurement into structure, process, and outcome. Structure refers to whether a particular characteristic is applicable in a particular setting—e.g., whether a hospital has a catheterization laboratory or whether a clinic uses an electronic health record. Process refers to the way care is delivered; examples of process measures are whether a Pap smear was performed at the recommended interval or whether an aspirin was given to a patient with a suspected myocardial infarction. Outcome refers to what actually happens—e.g., the mortality rate in myocardial infarction. It is important to note that good structure and process do not always result in a good outcome. For instance, a patient may present with a suspected myocardial infarction to an institution with a catheterization laboratory and receive recommended care, including aspirin, but still die because of the infarction.
Quality theory also suggests that overall quality will be improved more in the aggregate if the performance level of all providers is raised rather than if a few poor performers are identified and punished. This view suggests that systems changes are especially likely to be helpful in improving quality, since large numbers of providers may be affected simultaneously.
The theory of continuous quality improvement suggests that organizations should be evaluating the care they deliver on an ongoing basis and continually making small changes to improve their individual processes. This approach can be very powerful if embraced over time.
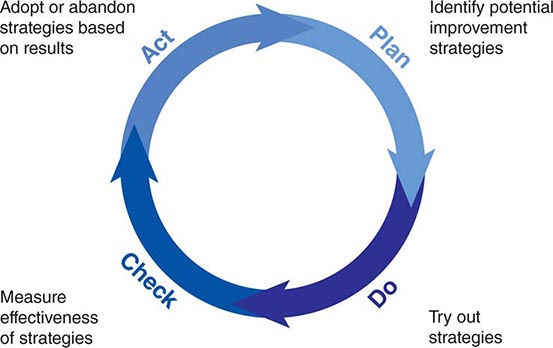
A number of specific tools have been developed to help improve process performance. One of the most important is the Plan-Do-Check-Act cycle (Fig. 12e-2). This approach can be used for “rapid cycle” improvement of a process—e.g., the time that elapses between a diagnosis of pneumonia and administration of antibiotics to the patient. Specific statistical tools, such as control charts, are often used in conjunction to determine whether progress is being made. Because most medical care includes one or many processes, this tool is especially important for improvement.
FIGURE 12e-2 Plan-Do-Check-Act cycle. This approach can be used to improve a specific process rapidly. First, planning is undertaken, and several potential improvement strategies are identified. Next, these strategies are evaluated in small “tests of change.” “Checking” entails measuring whether the strategies have appeared to make a difference, and “acting” refers to acting on the results.
Factors Relating to Quality Many factors can decrease the level of quality, including stress to providers, high or low levels of production pressure, and poor systems. Stress can have an adverse effect on quality because it can lead providers to omit important steps, as can a high level of production pressure. Low levels of production pressure sometimes can result in worse quality, as providers may be bored or have little experience with a specific problem. Poor systems can have a tremendous impact on quality, and even extremely dedicated providers typically cannot achieve high levels of performance if they are operating within a poor system.
Data about the Current State of Quality A study published by the RAND Corporation in 2006 provided the most complete picture of quality of care delivered in the United States to date. The results were sobering. The authors found that, across a wide range of quality parameters, patients in the United States received only 55% of recommended care overall; there was little variation by subtype, with scores of 54% for preventive care, 54% for acute care, and 56% for care of chronic conditions. The authors concluded that, in broad terms, the chances of getting high-quality care in the United States were little better than those of winning a coin flip.
Work from the Dartmouth Atlas of Health Care evaluating geographic variation in use and quality of care demonstrates that, despite large variations in utilization, there is no positive correlation between the two variables at the regional level. An array of data demonstrate, however, that providers with larger volumes for specific conditions, especially for surgical conditions, do have better outcomes.
Strategies for Improving Quality and Performance A number of specific strategies can be used to improve quality at the individual level, including rationing, education, feedback, incentives, and penalties. Rationing has been effective in some specific areas, such as persuading physicians to prescribe within a formulary, but it generally has been resisted. Education is effective in the short run and is necessary for changing opinions, but its effect decays fairly rapidly with time. Feedback on performance can be given at either the group or the individual level. Feedback is most effective if it is individualized and is given in close temporal proximity to the original events. Incentives can be effective, and many believe that they will prove to be a key to improving quality, especially if pay-for-performance with sufficient incentives is broadly implemented (see below). Penalties produce provider resentment and are rarely used in health care.
Another set of strategies for improving quality involves changing the systems of care. An example would be introducing reminders about which specific actions needed to be taken at a visit for a specific patient—a strategy that has been demonstrated to improve performance in certain situations, such as the delivery of preventive services. Another approach that has been effective is the development of “bundles” or groups of quality measures that can be implemented together with a high degree of fidelity. A number of hospitals have implemented a bundle for ventilator-associated pneumonia in the intensive care unit that includes five measures (e.g., ensuring that the head of the bed is elevated). These hospitals have been able to improve performance substantially.
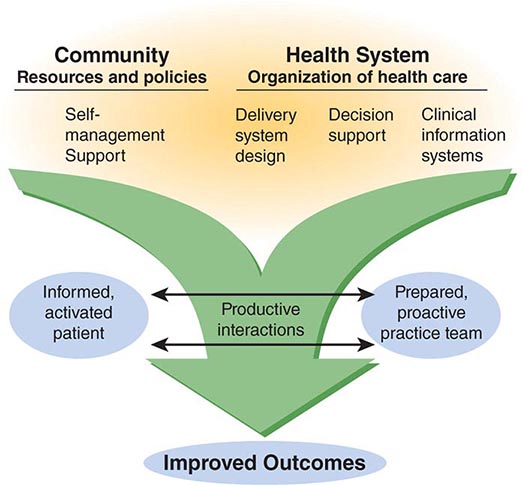
Perhaps the most pressing need is to improve the quality of care for chronic diseases. The Chronic Care Model has been developed by Wagner and colleagues (Fig. 12e-3); it suggests that a combination of strategies is necessary (including self-management support, changes in delivery system design, decision support, and information systems) and that these strategies must be delivered by a practice team composed of several providers, not just a physician.
FIGURE 12e-3 The Chronic Care Model, which focuses on improving care for chronic diseases, suggests that (1) delivery of high-quality care requires a range of strategies that must closely involve and engage the patient and (2) team care is essential. (From EH Wagner et al: Eff Clin Pract 1:2, 1998.)
Available evidence about the relative efficacy of strategies in reducing hemoglobin A1c (HbA1c) in outpatient diabetes care supports this general premise. It is especially notable that the outcome was the HbA1c level, as it has generally been much more difficult to improve outcome measures than process measures (such as whether HbA1c was measured). In this meta-analysis, a variety of strategies were effective, but the most effective ones were the use of team changes and the use of a case manager. When cost-effectiveness is considered in addition, it appears likely that an amalgam of strategies will be needed. However, the more expensive strategies, such as the use of case managers, probably will be implemented widely only if pay-for-performance takes hold.
National State of Quality Measurement In the inpatient setting, quality measurement is now being performed by a very large proportion of hospitals for several conditions, including myocardial infarction, congestive heart failure, pneumonia, and surgical infection prevention; 20 measures are included in all. This is the result of the Hospital Quality Initiative, which represents a collaboration among many entities, including the Hospital Quality Alliance, the Joint Commission, the National Quality Forum, and the Agency for Healthcare Research and Quality. The data are housed at the Center for Medicare and Medicaid Services, which publicly releases performance data on the measures on a website called Hospital Compare (www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/HospitalCompare.html). These data are reported voluntarily and are available for a very high proportion of the nation’s hospitals. Analyses demonstrate substantial regional variation in quality and important differences among hospitals. Analyses by the Joint Commission for similar indicators reveal that performance on measures by hospitals has improved over time and that, as might be hoped, lower performers have improved more than higher performers.
Public Reporting Overall, public reporting of quality data is becoming increasingly common. There are now commercial websites that have quality-related data for most regions of the United States, and these data can be accessed for a fee. Similarly, national data for hospitals are available. The evidence to date indicates that patients have not made much use of such data but that the data have had an important effect on provider and organization behavior. Instead, patients have relied on provider reputation to make choices, partly because little information was available until very recently and the information that was available was not necessarily presented in ways that were easy for patients to access. Many authorities think that, as more information about quality becomes available, it will become increasingly central to patients’ choices about where to access care.
Pay-for-Performance Currently, providers in the United States get paid exactly the same amount for a specific service, regardless of the quality of care delivered. The pay-for-performance theory suggests that, if providers are paid more for higher-quality care, they will invest in strategies that enable them to deliver that care. The current key issues in the pay-for-performance debate relate to (1) how effective it is, (2) what levels of incentives are needed, and (3) what perverse consequences are produced. The evidence on effectiveness is fairly limited, although a number of studies are ongoing. With respect to incentive levels, most quality-based performance incentives have accounted for merely 1–2% of total payment in the United States to date. In the United Kingdom, however, 40% of general practitioners’ salaries have been placed at risk according to performance across a wide array of parameters; this approach has been associated with substantial improvements in reported quality performance, although it is still unclear to what extent this change represents better performance versus better reporting. The potential for perverse consequences exists with any incentive scheme. One problem is that, if incentives are tied to outcomes, there may be a tendency to transfer the sickest patients to other providers and systems. Another concern is that providers will pay too much attention to quality measures with incentives and ignore the rest of the quality picture. The validity of these concerns remains to be determined. Nonetheless, it appears likely that, under health care reform, the use of various pay-for-performance schemes is likely to increase.
CONCLUSIONS
The safety and quality of care in the United States could be improved substantially. A number of available interventions have been shown to improve the safety of care and should be used more widely; others are undergoing evaluation or soon will be. Quality also could be dramatically better, and the science of quality improvement continues to mature. Implementation of pay-for-performance should make it much easier for organizations to justify investments in improving safety and quality parameters, including health information technology. However, many improvements will also require changing the structure of care—e.g., moving to a more team-oriented approach and ensuring that patients are more involved in their own care. Health care reform is likely to result in increased use of pay-for-performance. Measures of safety are still relatively immature and could be made much more robust; it would be particularly useful if organizations had measures they could use in routine operations to assess safety at a reasonable cost. Although the quality measures available are more robust than those for safety, they still cover a relatively small proportion of the entire domain of quality, and more measures need to be developed. The public and payers are demanding better information about safety and quality as well as better performance in these areas. The clear implication is that these domains will have to be addressed directly by providers.
13e |
Primary Care in Low- and Middle-Income Countries |
The twentieth century witnessed the rise of an unprecedented global health divide. Industrialized or high-income countries experienced rapid improvement in standards of living, nutrition, health, and health care. Meanwhile, in low- and middle-income countries with much less favorable conditions, health and health care progressed much more slowly. The scale of this divide is reflected in the current extremes of life expectancy at birth, with Japan at the high end (83 years) and Sierra Leone at the low end (47 years). This nearly 40-year difference reflects the daunting range of health challenges faced by low- and middle-income countries. These nations must deal not only with a complex mixture of diseases (both infectious and chronic) and illness-promoting conditions but also, and more fundamentally, with the fragility of the foundations underlying good health (e.g., sufficient food, water, sanitation, and education) and of the systems necessary for universal access to good-quality health care. In the last decades of the twentieth century, the need to bridge this global health divide and establish health equity was increasingly recognized. The Declaration of Alma Ata in 1978 crystallized a vision of justice in health, regardless of income, gender, ethnicity, or education, and called for “health for all by the year 2000” through primary health care. While much progress has been made since the declaration, at the end of the first decade and a half of the twenty-first century, much remains to be done to achieve global health equity.
This chapter looks first at the nature of the health challenges in low- and middle-income countries that underlie the health divide. It then outlines the values and principles of a primary health care approach, with a focus on primary care services. Next, the chapter reviews the experience of low- and middle-income countries in addressing health challenges through primary care and a primary health care approach. Finally, the chapter identifies how current challenges and global context provide an agenda and opportunities for the renewal of primary health care and primary care.
PRIMARY CARE AND PRIMARY HEALTH CARE
The term primary care has been used in many different ways: to describe a level of care or the setting of the health system, a set of treatment and prevention activities carried out by specific personnel, a set of attributes for the way care is delivered, or an approach to organizing health systems that is synonymous with the term primary health care. In 1996, the U.S. Institute of Medicine encompassed many of these different usages, defining primary care as “the provision of integrated, accessible health care services by clinicians who are accountable for addressing a large majority of personal health care needs, developing a sustained partnership with patients, and practicing in the context of family and community.”1 We use this definition of primary care in this chapter. Primary care performs an essential function for health systems, providing the first point of contact when people seek health care, dealing with most problems, and referring patients onward to other services when necessary. As is increasingly evident in countries of all income levels, without strong primary care, health systems cannot function properly or address the health challenges of the communities they serve.
Primary care is only one part of a primary health care approach. The Declaration of Alma Ata, drafted in 1978 at the International Conference on Primary Health Care in Alma Ata (now Almaty in Kazakhstan), identified many features of primary care as being essential to achieving the goal of “health for all by the year 2000.” However, it also identified the need to work across different sectors, address the social and economic factors that determine health, mobilize the participation of communities in health systems, and ensure the use and development of technology that was appropriate in terms of setting and cost. The declaration drew from the experiences of low- and middle-income countries in trying to improve the health of their people following independence. Commonly, these countries had built hospital-based systems similar to those in high-income countries. This effort had resulted in the development of high-technology services in urban areas while leaving the bulk of the population without access to health care unless they traveled great distances to these urban facilities. Furthermore, much of the population lacked access to basic public health measures. Primary health care efforts aimed to move care closer to where people lived, to ensure their involvement in decisions about their own health care, and to address key aspects of the physical and social environment essential to health, such as water, sanitation, and education.
After the Declaration of Alma Ata, many countries implemented reforms of their health systems based on primary health care. Most progress involved strengthening of primary care services; unexpectedly, however, much of this progress was seen in high-income countries, most of which constructed systems that made primary care available at low or no cost to their entire populations and that delivered the bulk of services in primary care settings. This endeavor also saw the reinforcement of family medicine as a specialty to provide primary care services. Even in the United States (an obvious exception to this trend), it became clear that the populations of states with more primary care physicians and services were healthier than those with fewer such resources.
Progress was also made in many low- and middle-income countries. However, the target of “health for all by the year 2000” was missed by a large margin. The reasons were complex but partly entailed a general failure to implement all aspects of the primary health care approach, particularly work across sectors to address social and economic factors that affect health and provision of sufficient human and other resources to make possible the access to primary care attained in high-income countries. Furthermore, despite the consensus in Alma Ata in 1978, the global health community rapidly became fractured in its commitment to the far-reaching measures called for by the declaration. Economic recession tempered enthusiasm for primary health care, and momentum shifted to programs concentrating on a few priority measures such as immunization, oral rehydration, breast-feeding, and growth monitoring for child survival. Success with these initiatives supported the continued movement of health development efforts away from the comprehensive approach of primary health care and toward programs that targeted specific public health priorities. This approach was reinforced by the need to address the HIV/AIDS epidemic. By the 1990s, primary health care had fallen out of favor in many global-health policy circles, and low- and middle-income countries were being encouraged to reduce public sector spending on health and to focus on cost-effectiveness analysis to provide a package of health care measures thought to offer the greatest health benefits.
HEALTH CHALLENGES IN LOW- AND MIDDLE-INCOME COUNTRIES
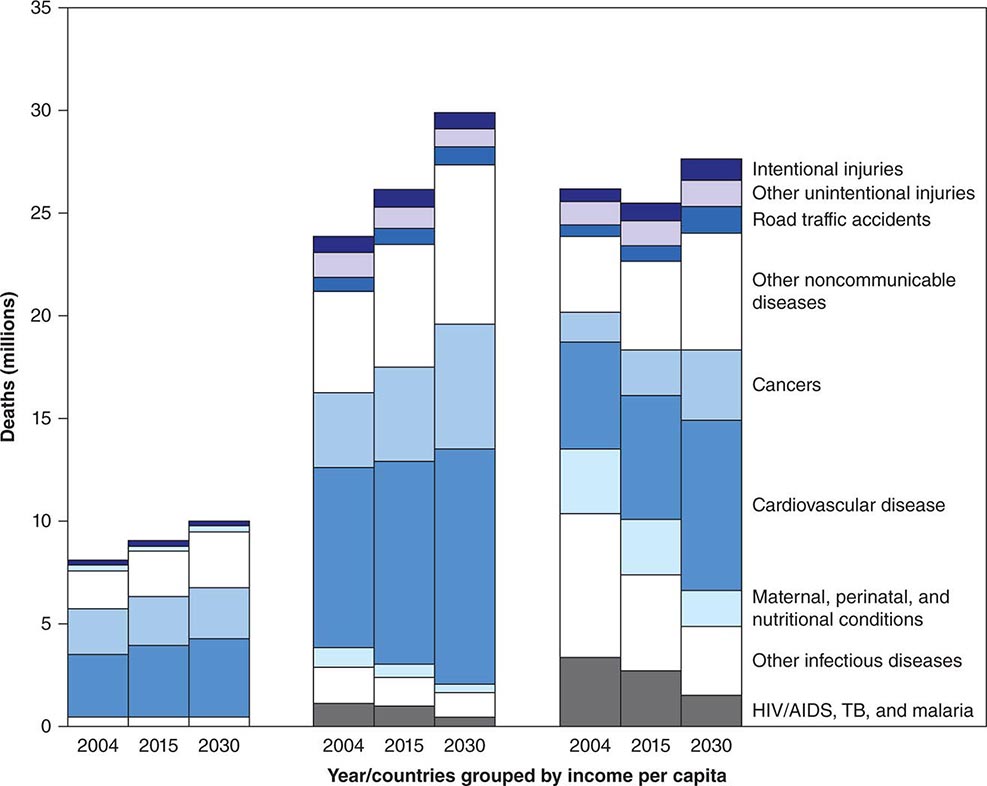
Low- and middle-income countries, defined by a per capita gross national income of <$12,476 (U.S.) per person per year, account for >80% of the world’s population. Average life expectancy in these countries lags far behind that in high-income countries: whereas the average life expectancy at birth in high-income countries is 74 years, it is only 68 years in middle-income countries and 58 years in low-income countries. This discrepancy has received growing attention over the past 40 years. Initially, the situation in poor countries was characterized primarily in terms of high fertility and high infant, child, and maternal mortality rates, with most deaths and illnesses attributable to infectious or tropical diseases among remote, largely rural populations. With growing adult (and especially elderly) populations and changing lifestyles linked to global forces of urbanization, a new set of health challenges characterized by chronic diseases, environmental overcrowding, and road traffic injuries has emerged rapidly (Fig. 13e-1). The majority of tobacco-related deaths globally now occur in low- and middle-income countries, and the risk of a child’s dying from a road traffic injury in Africa is more than twice that in Europe. Hence, low- and middle-income countries in the twenty-first century face a full spectrum of health challenges—infectious, chronic, and injury-related—at much higher incidences and prevalences than are documented in high-income countries and with many fewer resources to address these challenges.
FIGURE 13e-1 Projections of disease burden to 2030 for high-, middle-, and low-income countries (left, center, and right, respectively). TB, tuberculosis. (Source: World Health Organization: The Global Burden of Disease 2004 Update, 2008.)
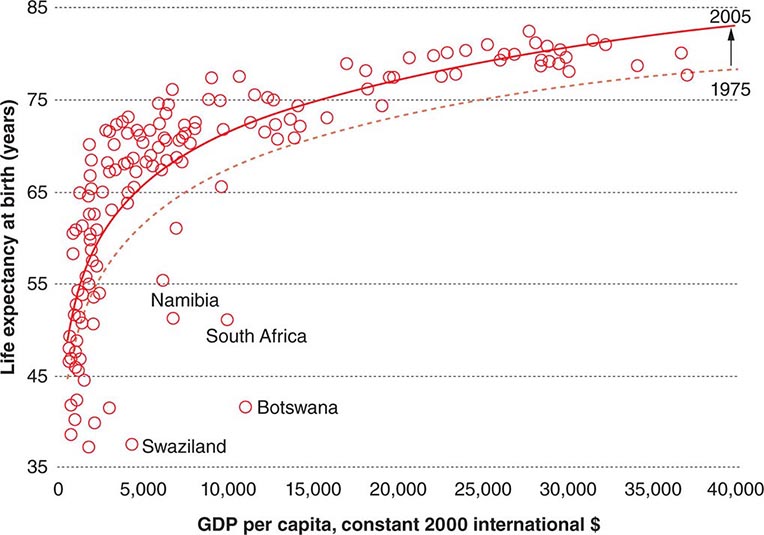
Addressing these challenges, however, does not mean simply waiting for economic growth. Analysis of the association between wealth and health across countries reveals that, for any given level of wealth, there is a substantial variation in life expectancy at birth that has persisted despite overall global progress in life expectancy during the past 30 years (Fig. 13e-2). Health status in low- and middle-income countries varies enormously. Nations such as Cuba and Costa Rica have life expectancies and childhood mortality rates similar to or even better than those in high-income countries; in contrast, countries in sub-Saharan Africa and the former Soviet bloc have experienced significant reverses in these health markers in the past 20 years.
FIGURE 13e-2 Gross domestic product (GDP) per capita and life expectancy at birth in 169 countries, 1975 and 2005. Only outlying countries are named. (Source: World Health Organization: Primary Health Care: Now More Than Ever. World Health Report 2008.)
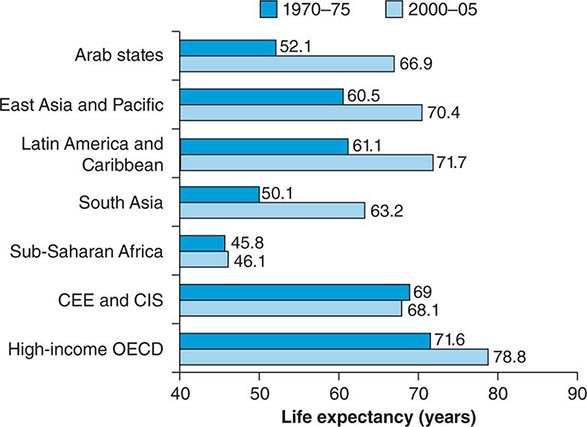
As Angus Deaton stated in the World Institute for Development Economics Research annual lecture on September 29, 2006, “People in poor countries are sick not primarily because they are poor but because of other social organizational failures, including health delivery, which are not automatically ameliorated by higher income.” This analysis concurs with classic studies of the array of societal factors explaining good health in poor settings such as Cuba and Kerala State in India. Analyses conducted over the past three decades indeed show that rapid health improvement is possible in very different contexts. That some countries continue to lag far behind can be understood through a comparison of regional differences in progress in terms of life expectancy over this period (Fig. 13e-3). While most regions have made impressive progress, sub-Saharan Africa and the former Soviet states have seen stagnation and even reversals.
FIGURE 13e-3 Regional trends in life expectancy. CEE and CIS, Central and Eastern Europe and the Commonwealth of Independent States; OECD, Organization for Economic Co-operation and Development. (Source: World Health Organization: Closing the Gap in a Generation: Health Equity Through Action on the Social Determinants of Health. Commission on Social Determinants of Health Final Report, 2008.)
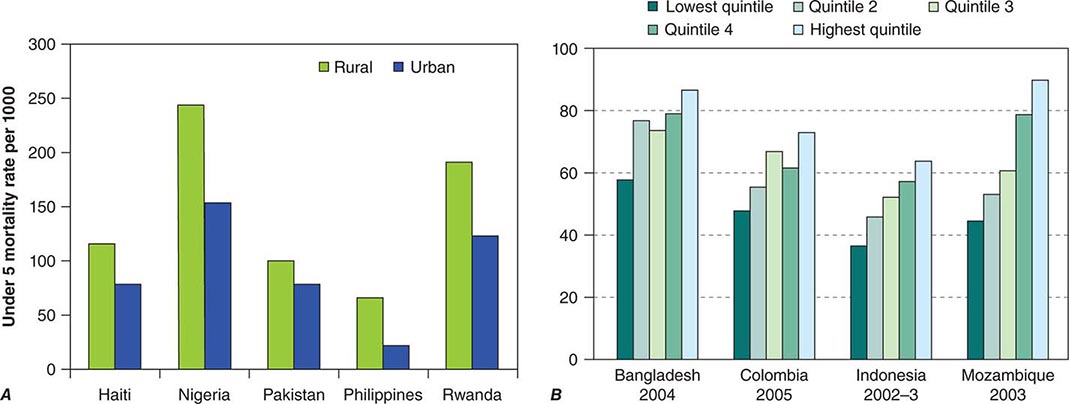
As average levels of health vary across regions and countries, so too do they vary within countries (Fig. 13e-4). Indeed, disparities within countries are often greater than those between high-income and low-income countries. For example, if low- and middle-income countries could reduce their overall childhood mortality rate to that of the richest one-fifth of their populations, global childhood mortality could be decreased by 40%. Disparities in health are mostly a result of social and economic factors such as daily living conditions, access to resources, and ability to participate in life-affecting decisions. In most countries, the health care sector actually tends to exacerbate health inequalities (the “inverse-care law”); because of neglect and discrimination, poor and marginalized communities are much less likely to benefit from public health services than those that are better off. Reforming health systems toward people-centered primary care provides an opportunity to reverse these negative trends.
FIGURE 13e-4 A. Mortality of children under 5 years old, by place of residence, in five countries. (Source: Data from the World Health Organization.) B. Full basic immunization coverage (%), by income group. (Source: Primary Health Care: Now More Than Ever. World Health Report 2008.)
Health services have failed to make their contribution to reducing these pervasive social inequalities by ensuring universal access to existing, scientifically validated, low-cost interventions such as insecticide-treated bed nets for malaria, taxes on cigarettes, short-course chemotherapy for tuberculosis, antibiotic treatment for pneumonia, dietary modification and secondary prevention measures for high blood pressure and high cholesterol levels, and water treatment and oral rehydration therapy for diarrhea. Despite decades of “essential packages” and “basic” health campaigns, the effective implementation of what is already known to work appears (deceptively) to be difficult.
Recent analyses have begun to focus on “the how” (as opposed to “the what”) of health care delivery, exploring why health progress is slow and sluggish despite the abundant availability of proven interventions for health conditions in low- and middle-income countries. Three general categories of reasons are being identified: (1) shortfalls in performance of health systems; (2) stratifying social conditions; and (3) skews in science.
SHORTFALLS IN PERFORMANCE OF HEALTH SYSTEMS
Specific health problems often require the development of specific health interventions (e.g., tuberculosis requires short-course chemotherapy). However, the delivery of different interventions is often facilitated by a common set of resources or functions: money or financing, trained health workers, and facilities with reliable supplies fit for multiple purposes. Unfortunately, health systems in most low- and middle-income countries are largely dysfunctional at present.
In the large majority of low- and middle-income countries, the level of public financing for health is woefully insufficient: whereas high-income countries spend, on average, 7% of the gross domestic product on health, middle-income countries spend <4% and low-income countries <3%. External financing for health through various donor channels has grown significantly over time. While these funds for health are significant (~$20 billion [U.S.] in 2008 for low- and middle-income countries), they represent <2% of total health expenditures in low- and middle-income countries and hence are neither a sufficient nor a long-term solution to chronic underfinancing. In Africa, 70% of health expenditures come from domestic sources. The predominant form of health care financing—charging patients at the point of service—is the least efficient and the most inequitable, tipping millions of households into poverty annually.
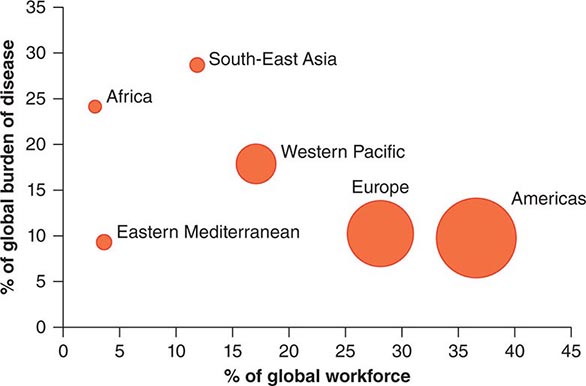
Health workers, who represent another critical resource, are often inadequately trained and supported in their work. Recent estimates indicate a shortage of >4 million health workers, constituting a crisis that is greatly exacerbated by the migration of health workers from low- and middle-income countries to high-income countries. Sub-Saharan Africa carries 24% of the global disease burden but has only 3% of the health workforce (Fig. 13e-5). The International Organization for Migration estimated in 2006 that there were more Ethiopian physicians practicing in Chicago than in Ethiopia itself.
FIGURE 13e-5 Global burden of disease and health workforce. (Source: World Health Organization: Working Together for Health, 2006.)
Critical diagnostics and drugs often do not reach patients in need because of supply-chain failures. Moreover, facilities fail to provide safe care: new evidence suggests much higher rates of adverse events among hospitalized patients in low- and middle-income countries than in high-income countries. Weak government planning, regulatory, monitoring, and evaluation capacities are associated with rampant, unregulated commercialization of health services and chaotic fragmentation of these services as donors “push” their respective priority programs. With such fragile foundations, it is not surprising that low-cost, affordable, validated interventions are not reaching those who need them.
STRATIFYING SOCIAL CONDITIONS
Health care delivery systems do not exist in a vacuum but rather are embedded in a complex of social and economic forces that often stratify opportunities for health unfairly. Most worrisome are the pervasive forces of social inequality that serve to marginalize populations with disproportionately large health needs (e.g., the urban poor; illiterate mothers). Why should a poor slum dweller with no income be expected to come up with the money for a bus fare needed to travel to a clinic to learn the results of a sputum test for tuberculosis? How can a mother living in a remote rural village and caring for an infant with febrile convulsions find the means to get her child to appropriate care? Shaky or nonexistent social security systems, dangerous work environments, isolated communities with little or no infrastructure, and systematic discrimination against minorities are among the myriad forces with which efforts for more equitable health care delivery must contend.
SKEWS IN SCIENCE
While science has yielded enormous breakthroughs in health in high-income countries, with some spillover to low- and middle-income countries, many important health problems continue to affect primarily low- and middle-income countries whose research and development investments are deplorably inadequate. The past decade has seen growing efforts to right this imbalance with research and development investment for new drugs, vaccines, and diagnostics that effectively cater to the specific health needs of populations in low- and middle-income countries. For example, the Medicines for Malaria Venture has revitalized a previously “dry” pipeline for new malaria drugs. This is but one of many such efforts, but much more needs to be done.
As discussed above, the primary constraint on better health in low- and middle-income countries is related less to the availability of health technologies and more to their effective delivery. Underlying these systems and social challenges to greater equity in health is a major bias regarding what constitutes legitimate “science” to improve health equity. The lion’s share of health research financing is channeled toward the development of new technologies—drugs, vaccines, and diagnostics; in contrast, virtually no resources are directed toward research on how health care delivery systems can become more reliable and overcome adverse social conditions. The complexity of systems and social context is such that this issue of delivery requires an enormous investment in terms not only of money but also of scientific rigor, with the development of new research methods and measures and the attainment of greater legitimacy in the mainstream scientific establishment.
These common challenges to low- and middle-income countries partly explain the resurgence of interest in the primary health care approach. In some countries (mostly middle-income), significant progress has been made in expanding coverage by health systems based on primary care and even in improving indicators of population health. More countries are embarking on the creation of primary care services despite the challenges that exist, particularly in low-income countries. Even when these challenges are acknowledged, there are many reasons for optimism that low- and middle-income countries can accelerate progress in building primary care.
PRIMARY HEALTH CARE IN THE TWENTY-FIRST CENTURY
The new millennium has seen a resurgence of interest in primary health care as a means of addressing global health challenges. This interest has been driven by many of the same issues that led to the Declaration of Alma Ata: rapidly increasing disparities in health between and within countries, spiraling costs of health care at a time when many people lack quality care, dissatisfaction of communities with the care they are able to access, and failure to address changes in health threats, especially noncommunicable disease epidemics. These challenges require a comprehensive approach and strong health systems with effective primary care. Global health development agencies have recognized that sustaining gains in public health priorities such as HIV/AIDS requires not only robust health systems but also the tackling of social and economic factors related to disease incidence and progression. Weak health systems have proved a major obstacle to delivering new technologies, such as antiretroviral therapy, to all who need them. Changing disease patterns have led to a demand for health systems that can treat people as individuals whether or not they present to a health facility with the public health “priority” (e.g., HIV/AIDS or tuberculosis) to which that facility is targeted. We discuss experiences in low- and middle-income countries in relation to primary care in greater detail below. First, we consider the features of primary health care and primary care as currently understood.
REVITALIZATION OF PRIMARY HEALTH CARE
At the 2009 World Health Assembly (an annual meeting of all countries to discuss the work of the World Health Organization [WHO]), a resolution was passed reaffirming the principles of the Declaration of Alma Ata and the need for national health systems to be based on primary health care. This resolution did not suggest that nothing had changed in the intervening 30 years since the declaration, nor did it dispute that its prescription needed reframing in light of changing public health needs. The 2008 WHO World Health Report describes how a primary health care approach is necessary “now more than ever” to address global health priorities, especially in terms of disparities and new health challenges. As discussed below, this report highlights four broad areas in which reform is required (Fig. 13e-6). One of these areas—the need to organize health care so that it places the needs of people first—essentially relates to the necessity for strong primary care in health systems and what this requirement entails. The other three areas also relate to primary care. All four areas require action to move health systems in a direction that will reduce disparities and increase the satisfaction of those they serve. The World Health Report’s recommendations present a vision of primary health care that is based on the principles of Alma Ata but that differs from many attempts to implement primary health care in the 1970s and 1980s.
FIGURE 13e-6 The four reforms of primary health care renewal. (Source: World Health Organization: Primary Health Care: Now More Than Ever. World Health Report 2008.)
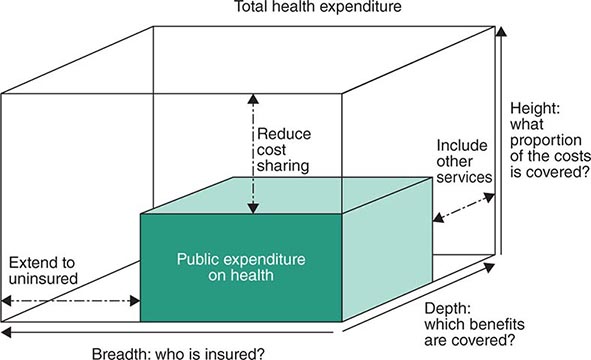
Universal Coverage Reforms to Improve Health Equity Despite progress in many countries, most people in the world can receive health care services only if they can pay at the point of service. Disparities in health are caused not only by a lack of access to necessary health services but also by the impact of expenditure on health. More than 100 million people are driven into poverty each year by health care costs, with countless others deterred from accessing services at all. Moving toward prepayment financing systems for universal coverage, which ensure access to a comprehensive package of services according to need without precipitating economic ruin, is therefore emerging as a major priority in low- and middle-income countries. Increasing coverage of health services can be considered in terms of three axes: the proportion of the population covered, the range of services underwritten, and the percentage of costs paid (Fig. 13e-7). Moving toward universal coverage requires ensuring the availability of health care services to all, eliminating barriers to access, and organizing pooled financing mechanisms, such as taxation or insurance, to remove user fees at the point of service. It also requires measures beyond financing, including expansion of health services in poorly served areas, improvement in the quality of services provided to marginalized communities, and increased coverage of other social services that significantly affect health (e.g., education).
FIGURE 13e-7 Three ways of moving toward universal coverage.
Service Delivery Reforms to Make Health Systems People-Centered Health systems have often been organized around the needs of those who provide health care services, such as clinicians and policymakers. The result is a centralization of services or the provision of vertical programs that target single diseases. The principles of primary health care, including the development of primary care, reorient care around the needs of the people to whom services cater. This “people-centered” approach aims to provide health care that is both more effective and appropriate.
The increase in noncommunicable diseases in low- and middle-income countries offers a further stimulus for urgent reform of service delivery to improve chronic disease care. As discussed above, large numbers of people currently fail to receive relatively low-cost interventions that have reduced the incidence of these diseases in high-income countries. Delivery of these interventions requires health systems that can address multiple problems and manage people over a long period within their own communities, yet many low- and middle-income countries are only now starting to adapt and build primary care services that can address noncommunicable diseases and communicable diseases requiring chronic care. Even some countries (e.g., Iran) that have had significant success in reducing communicable diseases and improving child survival have been slow to adapt their health systems to rapidly accelerating noncommunicable disease epidemics.
People-centered care requires a safe, comprehensive, and integrated response to the needs of those presenting to health systems, with treatment at the first point of contact or referral to appropriate services. Because no discrete boundary separates people’s needs for health promotion, curative interventions, and rehabilitation services across different diseases, primary care services must address all presenting problems in a unified way. Meeting people’s needs also involves improved communication between patients and their clinicians, who must take the time to understand the impact of the patients’ social context on the problems they present with. This enhanced understanding is made possible by improvements in the continuity of care so that responsibility transcends the limited time people spend in health care facilities. Primary care plays a vital role in navigating people through the health system; when people are referred elsewhere for services, primary care providers must monitor the resulting consultations and perform follow-up. All too often, people do not receive the benefit of complex interventions undertaken in hospitals because they lose contact with the health care system once discharged. Comprehensiveness and continuity of care are best achieved by ensuring that people have an ongoing personal relationship with a care team.
Public Policy Reforms to Promote and Protect the Health of Communities Public policies in sectors other than health care are essential to reduce disparities in health and to make progress toward global public health targets. The 2008 final report of the WHO Commission on Social Determinants of Health provides an exhaustive review of the intersectoral policies required to address health inequities at the local, national, and global levels. Advances against major challenges such as HIV/AIDS, tuberculosis, emerging pandemics, cardiovascular disease, cancers, and injuries require effective collaboration with sectors such as transport, housing, labor, agriculture, urban planning, trade, and energy. While tobacco control provides a striking example of what is possible if different sectors work together toward health goals, the lack of implementation of many evidence-based tobacco control measures in most countries just as clearly illustrates the difficulties encountered in such intersectoral work and the unrealized potential of public policies to improve health. At the local level, primary care services can help enact health-promoting public policies in other sectors.
Leadership Reforms to Make Health Authorities More Responsive The Declaration of Alma Ata emphasized the importance of participation by people in their own health care. In fact, participation is important at all levels of decision-making. Contemporary health challenges require new models of leadership that acknowledge the role of government in reducing disparities in health but that also recognize the many types of organizations that provide health care services. Governments need to guide and negotiate among these different groups, including nongovernmental organizations (NGOs) and the private sector, and to provide strong regulation where necessary. This difficult task requires a massive reinvestment in leadership and governance capacity, especially if action by different sectors is to be effectively implemented. Moreover, disadvantaged groups and other actors are increasingly expecting that their voices and health needs will be included in the decision-making process. The complex landscape for leadership at the national level is mirrored in many ways at the international or global level. The transnational character of health and the increasing interdependence of countries with respect to outbreak diseases, climate change, security, migration, and agriculture place a premium on more effective global health governance.
EXPERIENCES WITH PRIMARY CARE IN LOW- AND MIDDLE-INCOME COUNTRIES
Aspects of the primary health care approach described above, with an emphasis on primary care services, have been implemented to varying degrees in many low- and middle-income countries over the past half-century. As discussed above, some of these experiences inspired and informed the Declaration of Alma Ata, which itself led many more countries to attempt to implement primary health care. This section describes the experiences of a selection of low- and middle-income countries in improving primary care services that have enhanced the health of their populations.
Before Alma Ata, few countries had attempted to develop primary health care on a national level. Rather, most focused on expanding primary care services to specific communities (often rural villages), making use of community volunteers to compensate for the absence of facility-based care. In contrast, in the post–World War II period, China invested in primary care on a national scale, and life expectancy doubled within roughly 20 years. The Chinese expansion of primary care services included a massive investment in infrastructure for public health (e.g., water and sanitation systems) linked to innovative use of community health workers. These “barefoot doctors” lived in and expanded care to rural villages. They received a basic level of training that enabled them to provide immunizations, maternal care, and basic medical interventions, including the use of antibiotics. Through the work of the barefoot doctors, China brought low-cost universal basic health care coverage to its entire population, most of which had previously had no access to these services.
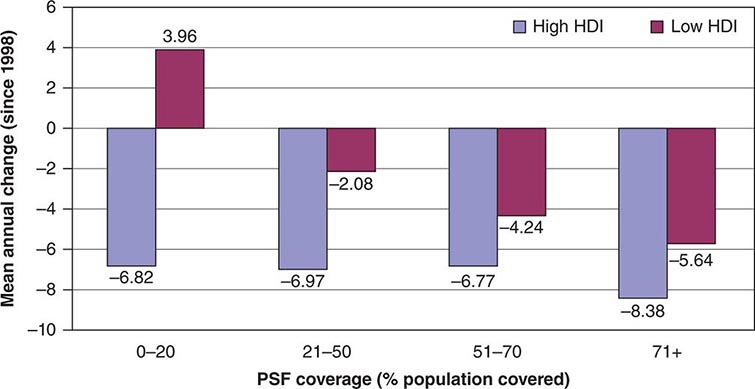
In 1982, the Rockefeller Foundation convened a conference to review the experiences of China along with those of Costa Rica, Sri Lanka, and the state of Kerala in India. In all of these locations, good health care at low cost appeared to have been achieved. Despite lower levels of economic development and health spending, all of these jurisdictions, along with Cuba, had health indicators approaching—or in some cases exceeding—those of developed countries. Analysis of these experiences revealed a common emphasis on primary care services, with expansion of care to the entire population free of charge or at low cost, combined with community participation in decision-making about health services and coordinated work in different sectors (especially education) toward health goals. During the three decades since the Rockefeller meeting, some of these countries have built on this progress, while others have experienced setbacks. Recent experiences in developing primary care services show that the same combination of features is necessary for success. For example, Brazil—a large country with a dispersed population—has made major strides in increasing the availability of health care in the past quarter century. In this millennium, the Brazilian Family Health Program has expanded progressively across the country, with almost all areas now covered. This program provides communities with free access to primary care teams made up of primary care physicians, community health workers, nurses, dentists, obstetricians, and pediatricians. These teams are responsible for the provision of primary care to all people in a specified geographic area—not only those who access health clinics. Moreover, individual community health workers are responsible for a named list of people within the area covered by the primary care team. Problems with access to health care persist in Brazil, especially in isolated areas and urban slums. However, solid evidence indicates that the Family Health Program has already contributed to impressive gains in population health, particularly in terms of childhood mortality and health inequities. In fact, this program has already had an especially marked impact on childhood mortality reduction in less developed areas (Fig. 13e-8).
FIGURE 13e-8 Improvements in childhood mortality following the Family Health Program in Brazil. HDI, Human Development Index; PSF, Program Saúde da Família (Family Health Program). (Source: Ministry of Health, Brazil.)
Chile has also built on its existing primary care services in the past decade, aiming to improve the quality of care and the extent of coverage in remote areas, above all for disadvantaged populations. This effort has been made in concert with measures aimed at reducing social inequalities and fostering development, including social welfare benefits for families and disadvantaged groups and increased access to early-childhood educational facilities. As in Brazil, these steps have improved maternal and child health and have reduced health inequities. In addition to directly enhancing primary care services, Brazil and Chile have instituted measures to increase both the accountability of health providers and the participation of communities in decision-making. In Brazil, national and regional health assemblies with high levels of public participation are integral parts of the health policy–making process. Chile has instituted a patient’s charter that explicitly specifies the rights of patients in terms of the range of services to which they are entitled.
Other countries that have made recent progress with primary health care include Bangladesh, one of the poorest countries in the world. Since achieving its independence from Pakistan in 1971, Bangladesh has seen a dramatic increase in life expectancy, and childhood mortality rates are now lower than those in neighboring nations such as India and Pakistan. The expansion of access to primary health care services has played a major role in these achievements. This progress has been spearheaded by a vibrant NGO community that has focused its attention on improving the lives and livelihoods of poor women and their families through innovative and integrated microcredit, education, and primary care programs.
The above examples, along with others from the past 30 years in countries such as Thailand, Malaysia, Portugal, and Oman, illustrate how the implementation of a primary health care approach, with a greater emphasis on primary care, has led to better access to health care services—a trend that has not been seen in many other low- and middle-income countries. This trend, in turn, has contributed to improvements in population health and reductions in health inequities. However, as these nations have progressed, other countries have shown how previous gains in primary care can easily be eroded. In sub-Saharan Africa, undermining of primary care services has contributed to catastrophic reversals in health outcomes catalyzed by the HIV/AIDS epidemic. Countries such as Botswana and Zimbabwe implemented primary health care strategies in the 1980s, increasing access to care and making impressive gains in child health. Both countries have since been severely affected by HIV/AIDS, with pronounced decreases in life expectancy. However, Zimbabwe has also seen political turmoil, a decline of health and other social services, and the flight of health personnel, whereas Botswana has maintained primary care services to a greater extent and has managed to organize widespread access to antiretroviral therapy for people living with HIV/AIDS. Zimbabwe’s health situation has therefore become more desperate than that in Botswana.
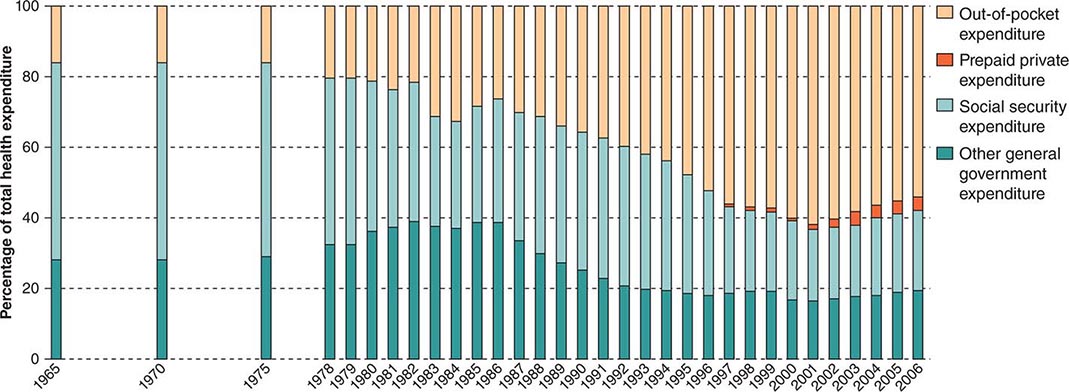
China provides a particularly striking example of how changes in health policy relevant to the organization of health systems (Fig. 13e-9) can have rapid, far-reaching consequences for population health. Even as the 1982 Rockefeller conference was celebrating China’s achievements in primary care, its health system was unraveling. The decision to open up the economy in the early 1980s led to rapid privatization of the health sector and the breakdown of universal health coverage. As a result, by the end of the 1980s, most people, especially the poorer segments of the population, were paying directly out of pocket for health care, and almost no Chinese had insurance—a dramatic transformation. The “barefoot doctor” schemes collapsed, and the population either turned to care paid for at hospitals or simply became unable to access care. This undermining of access to primary care services in the Chinese system and the resulting increase in impoverishment due to illness contributed to the stagnation of progress in health in China at the same time that incomes in that country increased at an unprecedented rate. Reversals in primary care have meant that China now increasingly faces health care issues similar to those faced by India. In both countries, rapid economic growth has been linked to lifestyle changes and noncommunicable disease epidemics. The health care systems of the two nations share two negative features that are common when primary care is weak: a disproportionate focus on specialty services provided in hospitals and unregulated commercialization of health services. China and India have both seen expansion of private hospital services that cater to middle-class and urban populations who can afford care; at the same time, hundreds of millions of people in rural areas now struggle to access the most basic services. Even in the former groups, a lack of primary care services has been associated with late presentation with illness and with insufficient investment in primary prevention approaches. This neglect of prevention poses a risk of large-scale epidemics of cardiovascular disease, which could endanger continued economic growth. In addition, the health systems of both countries now depend for the majority of their funding on out-of-pocket payments by people when they use services. Thus substantial proportions of the population must sacrifice other essential goods as a result of health expenditure and may even be driven into poverty by this cost. The commercial nature of health services with inadequate or no regulation has also led to the proliferation of charlatan providers, inappropriate care, and pressure for people to pay for expensive and sometimes unnecessary care. Commercial providers have limited incentives to use interventions (including public health measures) that cannot be charged for or that are what the person who is paying can afford.
FIGURE 13e-9 Changes in source of health expenditure in China over the past 40 years. (Source: World Health Organization: Primary Health Care: Now More Than Ever. World Health Report 2008.)
Faced with these problems, China and India have implemented measures to strengthen primary health care. China has increased government funding of health care, has taken steps toward restoring health insurance, and has enacted a target of universal access to primary care services. India has similarly mobilized funding to greatly expand primary care services in rural areas and is now duplicating this process in urban settings. Both countries are increasingly using public resources from their growing economies to fund primary care services.
These encouraging trends are illustrative of new opportunities to implement a primary health care approach and strengthen primary care services in low- and middle-income countries. Brazil, India, China, and Chile are being joined by many other low- and middle-income countries, including Indonesia, Mexico, the Philippines, Turkey, Rwanda, Ethiopia, South Africa, and Ghana, in ambitious initiatives mobilizing new resources to move toward universal coverage of health services at affordable cost.
OPPORTUNITIES TO BUILD PRIMARY CARE IN LOW- AND MIDDLE-INCOME COUNTRIES
Global public health targets will not be met unless health systems are significantly strengthened. More money is currently being spent on health than ever before. In 2005, global health spending totaled $5.1 trillion (U.S.)—double the amount spent a decade earlier. Although most expenditure occurs in high-income countries, spending in many emerging middle-income countries has rapidly accelerated, as has the allocation of monies for this purpose by both governments in and donors to low-income countries. These twin trends—greater emphasis on building health systems based on primary care and allotment of more money for health care—provide opportunities to address many of the challenges discussed above in low- and middle-income countries.
Accelerating progress requires a better understanding of how global health initiatives can more effectively facilitate the development of primary care in low-income countries. A review by the WHO Maximizing Positive Synergies Collaborative Group looked at programs funded by the Global Fund to Fight AIDS, Tuberculosis and Malaria; the Global Alliance for Vaccines and Immunisation (GAVI); the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR); and the World Bank (on HIV/AIDS). This group found that global health initiatives had improved access to and quality of the targeted health services and had led to better information systems and more adequate financing. The review also identified the need for better alignment of global health initiatives with other national health priorities and systematic exploitation of potential synergies. If global health initiatives implement programs that work in tandem with other components of national health systems without undermining staffing and procurement of supplies, they have the potential to contribute substantially to the capacity of health systems to provide comprehensive primary care services.
Even in the aftermath of the global financial crisis, global health initiatives continue to draw significant funding. In 2009, for example, U.S. President Barack Obama announced increasing development assistance from the United States for global health, earmarking $63 billion over the period 2009–2014 for a Global Health Initiative. New funding is also promised through a range of other initiatives focusing particularly on maternal and child health in low-income countries. The general trend is to coordinate this funding in order to reduce fragmentation of national health systems and to concentrate more on strengthening these systems. Comprehensive primary care in low-income countries must inevitably deal with the rapid emergence of chronic diseases and the growing prominence of injury-related health problems; thus, international health development assistance must become more responsive to these needs.
Beyond the new streams of funding for health services, other opportunities exist. Increased social participation in health systems can help build primary care services. In many countries, political pressure from community advocates for more holistic and accountable care as well as entrepreneurial initiatives to scale up community-based services through NGOs have accelerated progress in primary care without major increases in funding. Participation of the population in the provision of health care services and in relevant decision-making often drives services to cater to people’s needs as a whole rather than to narrow public health priorities.
Participation and innovation can help address critical issues related to the health workforce in low- and middle-income countries by establishing effective people-centered primary care services. Many primary care services do not need to be delivered by a physician or a nurse. Multidisciplinary teams can include paid community workers who have access to a physician if necessary but who can provide a range of health services on their own. In Ethiopia, more than 30,000 community health workers have been trained and deployed to improve access to primary care services, and there is increasing evidence that this measure is contributing to better health outcomes. In India, more than 600,000 community health advocates have been recruited as part of expanded rural primary care services. In Niger, the deployment of community health workers to deliver essential child health interventions (as a component of integrated community case management) has had impressive results in reducing childhood mortality and decreasing disparities. After the Declaration of Alma Ata, experiences with community health workers were mixed, with particular problems about levels of training and lack of payment. Current endeavors are not immune from these concerns. However, with access to physician support and the deployment of teams, some of these concerns may be addressed. Growing evidence from many countries indicates that shifting appropriate tasks to primary care workers who have had shorter, less expensive training than physicians will be essential to address the human resources crisis.
Finally, recent improvements in information and communication technologies, particularly mobile phone and Internet systems, have created the potential for systematic implementation of e-health, telemedicine, and improved health data initiatives in low- and middle-income countries. These developments raise the tantalizing possibility that health systems in these countries, which have long lagged behind those in high-income countries but are less encumbered by legacy systems that have proved hard to modernize in many settings, could leapfrog their wealthier counterparts in exploiting these technologies. Although the challenges posed by poor or absent infrastructure and investment in many low- and middle-income countries cannot be underestimated and will need to be addressed to make this possibility a reality, the rapid rollout of mobile networks and their use for health and other social services in many low-income countries where access to fixed telephone lines was previously very limited offer great promise in building primary care services in low- and middle-income countries.
CONCLUSION
As concern continues to mount about glaring inequities in global health, there is a growing commitment to redress these egregious shortfalls, as exemplified by global mobilization around the United Nations’ Millennium Development Goals and the early discussions on what targets should build on these goals in the post-2015 era. This commitment begins first and foremost with a clear vision of the fundamental importance of health in all countries, regardless of income. The values of health and health equity are shared across all borders, and primary health care provides a framework for their effective translation across all contexts.
The translation of these fundamental values has its roots in four types of reforms that reflect the distinct but interlinked challenges of (re)orienting a society’s resources on the basis of its citizens’ health needs: (1) organizing health care services around the needs of people and communities; (2) harnessing services and sectors beyond health care to promote and protect health more effectively; (3) establishing sustainable and equitable financing mechanisms for universal coverage; and (4) investing in effective leadership of the whole of society. This common primary health care agenda highlights the striking similarity, despite enormous differences in context, in the nature and direction of the reforms that national health systems must undertake to promote greater equity in health. This shared agenda is complemented by the growing reality of global health interconnectedness due, for example, to shared microbial threats, bridging of ethnolinguistic diversity, flows in migrant health workers, and mobilization of global funds to support the neediest populations. Embracing solidarity in global health while strengthening health systems through a primary health care approach is fundamental to sustained progress in global health.
1Institute of Medicine. Primary Care: America’s Health in a New Era (1996).
14e |
Complementary, Alternative, and Integrative Health Practices |
The search for health includes many beliefs and practices that are outside conventional medicine. Physicians are important sources for information and guidance about health matters, but our patients also rely on a wide range of other sources including family and friends, cultural traditions, alternative practitioners, and increasingly the Internet, popular media, and advertising. It is essential for physicians to understand what patients are doing to seek health, as this understanding is important to harness potential benefits and to help patients avoid harm.
DEFINITIONS AND SCOPE
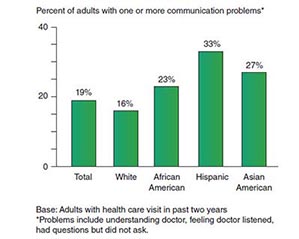
The phrase complementary and alternative medicine is used to describe a group of diverse medical and health care systems, practices, and products that have historic origins outside mainstream medicine. Most of these practices are used together with conventional therapies and therefore have been called complementary to distinguish them from alternative practices, those used as a substitute for standard care. Use of dietary supplements; mind-body practices such as acupuncture, massage, meditation, and hypnosis; and care from a traditional healer all fall under this umbrella. Brief definitions for some of the common complementary and alternative health practices are provided in Table 14e-1. Although some complementary health practices are implemented by a complementary health care provider such as a chiropractor, acupuncturist, or naturopathic practitioner, or by a physician, many of these practices are undertaken as “self-care.” Most are paid for out of pocket.
|
TERMINOLOGY OF COMPLEMENTARY AND ALTERNATIVE MEDICAL PRACTICES |
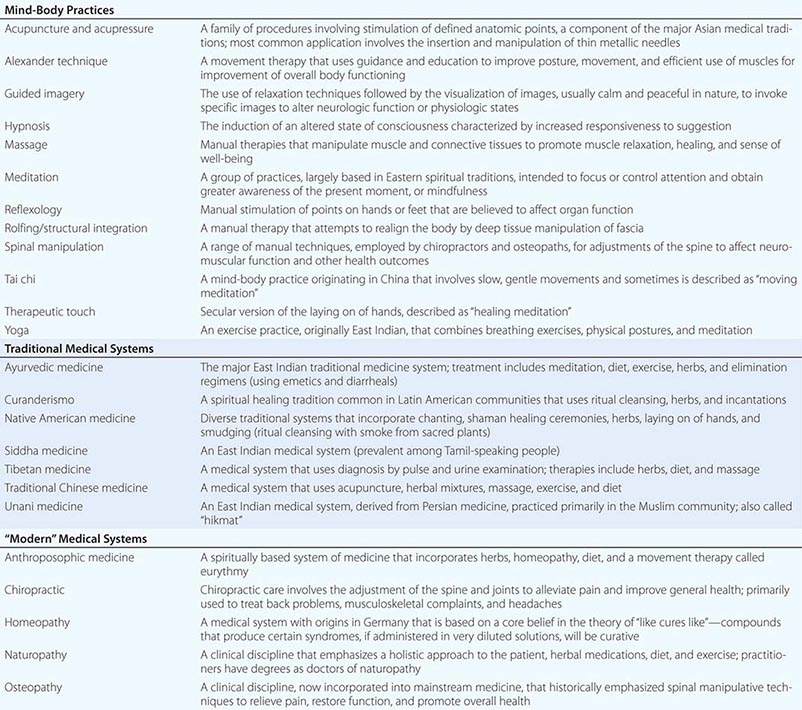
In the last decade or so, the terms integrative care and integrative medicine have entered the dialogue. A 2007 national survey conducted by the Centers for Disease Control and Prevention’s National Center for Health Statistics found that 42% of hospices had integrated complementary health practices into the care they provide. Integration of select complementary approaches is also common in Veterans Administration and Department of Defense facilities, particularly as part of management of pain and post-traumatic stress disorder.
The term integrative medicine is usually used to refer to a style of practice that places strong emphasis on a holistic approach to patient care while focusing on reduced use of technology. Physicians advocating this approach generally include selected complementary health practices in the care they offer patients, and many have established practice settings that include complementary health practitioners. Although this approach appears to be attractive to many patients, the heavy use of dietary supplements and the weaknesses in the evidence base for a number of the interventions offered in integrative practices continue to attract substantial concern and controversy.
Until a decade ago or so, “complementary and alternative medicine” could be defined as practices that are neither taught in medical schools nor reimbursed, but this definition is no longer workable, since medical students increasingly seek and receive some instruction about complementary health practices, and some practices are reimbursed by third-party payers. Another definition, practices that lack an evidence base, is also not useful, since there is a growing body of research on some of these modalities, and some aspects of standard care do not have a strong evidence base.
By its nature, the demarcation between mainstream medicine and complementary health practices is porous, varying from culture to culture and over time. Traditional Chinese medicine and the Indian practice of Ayurvedic medicine were once the dominant health teachings in those cultures. Certain health practices that arose as challenges to the mainstream have been integrated gradually into conventional care. Examples include the teachings of Fernand Lamaze that led to the widespread use of relaxation techniques during childbirth, the promotion of lactation counseling by the La Leche League, and the teaching of Cicely Saunders and Elizabeth Kübler-Ross that established the hospice movement.
The late nineteenth century saw the development of a number of healing philosophies by care providers who were critical of the medicine of the time. Of these, naturopathy and homeopathy, which arose in Germany, and chiropractic and osteopathy, which developed in the United States, have continued to endure. Osteopathic medicine is currently thoroughly integrated into conventional medicine, although the American Medical Association (AMA) labeled it a cult as late as 1960. The other three traditions have remained resolutely separate from mainstream medicine, although chiropractic care is available in some conventional care settings.
PATTERNS OF USE
The first large survey of use of these practices was performed by David Eisenberg and associates in 1993. It surprised the medical community by showing that more than 30% of Americans use complementary or alternative health approaches. Many studies since that time have extended those conclusions. Subsequently, the National Health Interview Survey (NHIS), a large, national survey conducted by the National Center for Health Statistics, a component of the Centers for Disease Control and Prevention, has addressed the use of complementary health practices and largely confirmed those results. The NHIS is a household survey of many kinds of health practices in the civilian population; it uses methods that create a nationally representative sample and has a sample size large enough to permit valid estimates about some subgroups. In 2002, 2007, and 2012, the survey included a set of questions that addressed complementary and alternative health approaches. Information was obtained from 31,000 adults in 2002 and 23,300 adults and 9400 children in 2007. Only preliminary data are available from the 2012 survey. In all three surveys, approximately 40% of adults report using some form of complementary therapy or health practice. In the 2007 study, 38% of adults and 12% of children had used one or more modalities. These surveys yield the estimate that nonvitamin, nonmineral dietary supplements are used by approximately 18% of the population. The most prevalent mind-body practices are relaxation techniques and meditation, chiropractic, and therapeutic massage. Americans are willing to pay for these services; the estimated out-of-pocket expenditure for complementary health practices in 2007 was $34 billion, representing 1.5% of total health expenditures and 11% of out-of-pocket costs.
The appeal of unproven complementary health approaches continues to perplex many physicians. Many factors contribute to these choices. Some patients seek out complementary health practitioners because they offer optimism or greater personal attention. For others, alternative approaches reflect a “self-help” approach to health and wellness or satisfy a search for “natural” or less invasive alternatives, since dietary supplements and other natural products are believed, correctly or not, to be inherently healthier and safer than standard pharmaceuticals. In NHIS surveys, the most common health conditions cited by patients for use of complementary health practices involve management of symptoms often poorly controlled by conventional care, particularly back pain and other painful musculoskeletal complaints, anxiety, and insomnia.
PRACTITIONER-BASED DISCIPLINES
Licensure and Accreditation At present, six fields of complementary health practice—osteopathic manipulation, chiropractic, acupuncture and traditional Chinese medicine, therapeutic massage, naturopathy, and homeopathy—are subject to some form of educational accreditation and state licensure. Accreditation of educational programs is the responsibility of professional organizations or commissions under federal oversight by the Department of Education. Licensure, in contrast, is strictly a state matter, generally determined by state legislatures. Legal recognition establishes public access to therapies even when there is no scientific consensus about their clinical value.
Osteopathic Manipulative Therapy Founded in 1892 by the physician Andrew Taylor Still, osteopathic medicine was originally based on the belief that manipulation of soft tissue and bone can correct a wide range of diseases of the musculoskeletal and other organ systems. Over the ensuing century, the osteopathic profession has welcomed increasing integration with conventional medicine. Today, the postgraduate training, practice, credentialing, and licensure of osteopathic physicians are virtually indistinguishable from those of allopathic physicians. Osteopathic medical schools, however, include training in manual therapies, particularly spinal manipulation. Approximately 70% of family practice osteopathic physicians perform manipulative therapies on some of their patients.
Chiropractic The practice of chiropractic care, founded by David Palmer in 1895, is the most widespread practitioner-based complementary health practice in the United States. Chiropractic practice emphasizes manual therapies for treatment of musculoskeletal complaints, although the scope of practice varies widely, and in some rural areas, chiropractors may serve a primary care role, due in part to the lack of other providers. According to the NHIS, approximately 8% of Americans receive chiropractic manipulation in a given year.
Since the mid-1970s, chiropractors have been licensed in all 50 states and reimbursed by Medicare. Chiropractic educational standards mandate 2 years of undergraduate training, 4 years of training at an accredited school of chiropractic, and in most states, successful completion of a standardized board examination. Postgraduate training is not required. The U.S. Department of Labor estimates that there are 52,000 licensed chiropractors (2010 figure). There is substantial geographic variation, with greater numbers of practitioners and greater use in the midwest, particularly in rural areas, and lower use in the southeast.
Historically, the relationship between the medical and chiropractic professions has been strained. Extending through the 1970s, the AMA set forth standards prohibiting physicians consulting or entering into professional relationships with chiropractors, but in 1987, after a decade of complex litigation, the U.S. District Court found the AMA in violation of antitrust laws. An uneasy truce has followed, with continued physician skepticism, but also evidence for robust patient demand and satisfaction.
The role of both osteopathic and chiropractic spinal manipulative therapies (SMTs) in back pain management has been the subject of a number of carefully performed trials and many systematic reviews. Conclusions are not consistent, but the most recent guidelines from the American College of Physicians and the American Pain Society conclude that SMT is associated with small to moderate benefit for low-back pain of less than 4 weeks in duration (evidence level B/C) and moderate benefit (evidence level B) for subacute or chronic low-back pain. The evidence of benefit for neck pain is not as extensive, and continued concern that cervical manipulation may occasionally precipitate vascular injury clouds a contentious debate.
Naturopathy Naturopathy is a discipline that emerged in central Europe in the nineteenth century as part of the Natural Cure movement and was introduced to the United States in the early twentieth century by Benjamin Lust. Fifteen states currently license naturopathic physicians, with considerable variation in the scope of practice. The naturopathic profession is actively seeking licensure in other states. There are estimated to be approximately 3000 licensed naturopathic physicians in the United States. There is also a robust naturopathy presence in Canada. Conventional and unconventional diagnostic tests and medications are prescribed, with an emphasis on relatively low doses of drugs, herbal medicines, healthy diet, and exercise. While there is some support for success of naturopathic practitioners in motivating healthy behaviors, concern exists about the heavy promotion of dietary supplements, most with little rigorous evidence.
Homeopathy Homeopathy was widespread in the United States in the late nineteenth and early twentieth centuries and continues to be a common alternative practice in many European countries, but estimates from the NHIS suggest that less than 1.5% of Americans visit a homeopathic practitioner in any given year. In the United States, licensure as a homeopathic physician is only possible in three states (Arizona, Connecticut, and Nevada) where it is restricted to licensed physicians. The number of practitioners is uncertain, however, because some states include homeopathy within the scope of practice of other fields, including chiropractic and naturopathy, and some practitioners may self-identify as homeopathic practitioners. As discussed below, the regulatory framework for homeopathic remedies differs from other dietary supplements. Homeopathic remedies are widely available and commonly recommended by naturopathic physicians, chiropractors, and other licensed and unlicensed practitioners.
Therapeutic Massage The field of therapeutic massage is growing rapidly, as use by the public is increasing. According to U.S. Department of Labor statistics, there are approximately 155,000 licensed massage therapists employed in the United States, and by 2020, this number is projected to grow by 20%. Forty-three states and the District of Columbia currently have laws regulating massage therapy; however, there is little consistency, and in some states, regulation is by town ordinance. States that do provide licensure for massage therapists typically require a minimum of 500 hours of training at an accredited institution, as well as meeting specific continuing education requirements and carrying malpractice insurance. Massage training programs generally are approved by a state board, but some may also be accredited by an independent agency, such as the Commission on Massage Therapy Accreditation (COMTA). The development of regulatory standards for therapeutic massage has not yet caught up with the evolution of the field or the high demand. Many techniques used are also employed by physical therapists.
Acupuncture and Traditional Chinese Medicine A venerable component of traditional Chinese medicine, with a history of use that extends at least 2000 years, acupuncture became better known in the United States in 1971, when New York Times reporter James Reston wrote about how doctors in China used needles to ease his pain after surgery. More than 3 million adults in the United States use acupuncture, according to NHIS data. In a number of European countries, acupuncture is performed primarily by physicians. In the United States, the training and licensure processes for physicians and nonphysicians differ. Currently, acupuncture is licensed in 42 states and the District of Columbia, with licensure standards varying within the scope of practice of each state. Licensure for nonphysicians generally requires 3 years of accredited training and the successful completion of a standardized examination. The main accrediting organization is the Accreditation Commission for Acupuncture and Oriental Medicine. Acupuncture is included in doctor of medicine (MD) and doctor of osteopathic medicine (DO) licensure in 31 states, with 11 states requiring additional training for physicians performing acupuncture.
MIND-BODY INTERVENTIONS
Mind-body practices are a large and diverse group of techniques that are administered or taught to others by a trained practitioner or teacher. Examples include acupuncture, massage therapy, meditation, relaxation techniques, spinal manipulation, and yoga. These approaches are being used more frequently in mainstream health care facilities for both patients and health care providers. Mind-body practices such as meditation and yoga are not licensed in any state, and training in those practices is not subject to national accreditation.
Americans often turn to complementary approaches for help in managing health conditions associated with physical and psychological pain—especially back pain, headache, musculoskeletal complaints, and functional pain syndromes. Chronic pain management is often refractory to conventional medical approaches, and standard pharmacologic approaches have substantial drawbacks. Health care guidelines of the American Pain Society and other professional organizations recognize the value of certain complementary approaches as adjuncts to pharmacologic management.
The evidence base for the effectiveness of these modalities is still relatively incomplete, but a few rigorous examples where there is promise of usefulness and safety include acupuncture for osteoarthritis pain; tai chi for fibromyalgia pan; and massage, yoga, and spinal manipulation for chronic back pain. In addition, new research is shedding light on the effects of meditation and acupuncture on central mechanisms of pain processing and perception and regulation of emotion and attention. Although many unanswered questions remain about these effects, findings are pointing to scientifically plausible mechanisms by which these modalities might yield benefit.
DIETARY SUPPLEMENTS
Regulation The Dietary Supplements Health and Education Act (DSHEA), passed in 1994, gives authority to the U.S. Food and Drug Administration (FDA) to regulate dietary supplements, but with expectations that differ in many respects from the regulation of drugs or food additives. Purveyors of dietary supplements cannot claim that they prevent or treat any disease. They can, however, claim that they maintain “normal structure and function” of body systems. For example, a product cannot claim to treat arthritis, but it can claim to maintain “normal joint health.” Homeopathic products predate FDA drug regulations and are sold with no requirement that they be proved effective. Although homeopathic products are widely believed to be safe because they are highly dilute, one product, a nasal spray called Zicam, was withdrawn from the market when it was found to produce anosmia, probably because of a significant zinc content. Homeopathic products, and indeed other complementary health products and practices, also convey the very significant risk that individuals will use them instead of effective conventional modalities.
Regulation of advertising and marketing claims is the purview of the Federal Trade Commission (FTC). The FTC does take legal action against promoters or websites that advertise or sell dietary supplements with false or deceptive statements.
Inherent Toxicity Although the public may believe that “natural” equates with “safe,” it is abundantly clear that natural products can be toxic. Misidentification of medicinal mushrooms has led to liver failure. Contamination of tryptophan supplements caused the eosinophilia-myalgia syndrome. Herbal products containing particular species of Aristolochia were associated with genitourinary malignancies and interstitial nephritis. In 2013, dietary supplements containing 1,3-dimethylamylamine (DMAA), often touted as a “natural” stimulant, led to cardiovascular problems, including heart attacks. Among the most controversial dietary supplements is Ephedra sinica, or ma huang, a product used in traditional Chinese medicine for short-term treatment of asthma and bronchial congestion. The scientific basis for these indications was revealed when ephedra was shown to contain the ephedrine alkaloids, especially ephedrine and pseudoephedrine. With the promulgation of the DSHEA regulations, supplements containing ephedra and herbs rich in caffeine sold widely in the U.S. marketplace because of their claims to promote weight loss and enhance athletic performance. Reports of severe and fatal adverse events associated with use of ephedra-containing products led to an evidence-based review of the data surrounding them, and in 2004, the FDA banned their sale in the United States.
Another major current concern with dietary supplements is adulteration with pharmacologic active compounds. Multi-ingredient products marketed for weight loss, body building, “sexual health,” and athletic performance are of particular concern. Recent FDA recalls have involved contamination with steroids, diuretics, stimulants, and phosphodiesterase type 5 inhibitors.
Herb-Drug Interactions A number of herbal products have potential impact on the metabolism of drugs. This effect was illustrated most compellingly with the demonstration in 2000 that consumption of St. John’s wort interferes with the bioavailability of the HIV protease inhibitor indinavir. Later studies showed its similar interference with metabolism of topoisomerase inhibitors such as irinotecan, with cyclosporine, and with many other drugs. The breadth of interference stems from the ability of hyperforin in St. John’s wort to upregulate expression of the pregnane × receptor, a promiscuous nuclear regulatory factor that promotes the expression of many hepatic oxidative, conjugative, and efflux enzymes involved in drug and food metabolism.
Because of the large number of compounds that alter drug metabolism and the large number of agents some patients are taking, identification of all potential interactions can be a daunting task. Several useful Web resources are available as information sources (Table 14e-2). Clearly, attention to this problem is particularly important with drugs with a narrow therapeutic index, such as anticoagulants, antiseizure medications, antibiotics, immunosuppressants, and cancer chemotherapeutic agents.
|
RESOURCES FOR DIETARY SUPPLEMENT–DRUG INTERACTIONS |
Abbreviation: PDA, personal digital assistant.
PATIENT AND PROVIDER RESOURCES
Physicians regularly face difficult challenges in providing patients with advice and education about complementary practices. Of particular concern to all physicians are practices of uncertain safety and practices that raise inappropriate hopes. Cancer therapies, antiaging regimens, weight-loss programs, sexual function, and athletic performance are frequently targeted for excessive claims and irresponsible marketing. A number of Internet resources provide critical tools for patient education (Table 14e-3). Because many complementary health products and practices are used as self-care and because many patients research these approaches extensively on the Internet, directing patients to responsible websites can often be very helpful.
|
INTERNET RESOURCES ON COMPLEMENTARY HEALTH APPROACHES |
The scientific evidence regarding complementary therapies is fragmentary and incomplete. Nonetheless, in some areas, particularly pain management, it is increasingly possible to perform the kind of rigorous systematic reviews of complementary health approaches that are the cornerstone of evidence-based medicine. A particularly valuable resource in this respect is the Cochrane Collaboration, which has performed more than 300 systematic reviews of complementary health practices. Practitioners will find this a valuable source to answer patient questions. Practice guidelines, particularly for pain management, are also available from several professional organizations. Links to these resources are provided in Table 14e-3.
SUMMARY
The use of complementary and alternative health practices reflects an active interest in improved health. An array of unproven modalities will always be used by our patients. While some of these choices need to be actively discouraged, many are in fact innocuous and can be accommodated. Some may be genuinely helpful, particularly in the management of troublesome symptoms. The dialogue with patients about complementary health practices is an opportunity to understand patients’ beliefs and expectations and use those insights to help guide health-seeking practices in a constructive way.
ACKNOWLEDGMENT
The late Dr. Stephen Straus contributed this chapter in prior editions, and some material from his chapter has been retained here.
15e |
The Economics of Medical Care |
The purpose of this chapter is to explain to physicians how economists think about physicians’ decision-making with regard to the treatment of patients. Economists’ mode of thinking has shaped health care policy and institutions and thus the environment in which physicians practice, not only in the United States but in many other countries as well. It may prove useful for physicians to understand some aspects of the economists’ way of thinking, even if it sometimes seems foreign or uncongenial.
Physicians see themselves as professionals and as healers, assisting their patients with their health care needs. When economists are patients, they probably see physicians the same way, but when they view doctors through the lens of economics as a discipline, they see physicians—and their patients as well—as economic agents. In other words, economists are interested in the degree to which physicians and patients respond to various incentives in deciding how to deploy the resources over which they exercise choice. Examples of issues that would concern an economist include how much time physicians devote to seeing a patient; which tests they order; what drugs, if any, they prescribe; whether they recommend a procedure; whether they refer a patient; and whether they admit a patient to the hospital. In addition, patients consider the cost when they make a decision about whether to seek care.
To say that economists view physicians and patients as economic agents is not to say that economists consider financial incentives the predominant factor in the decisions that either physicians or patients make about treatment; it is to say only that these incentives have some influence on these decisions. In fact, the role played by financial incentives in medical decision-making may often be dwarfed by the roles played by scientific knowledge, by professional norms and ethics, and by the influence of peers. However, economic policy greatly influences financial incentives, and economists tend to focus on this domain. Their interest stems from fundamental economic questions: What goods and services are produced and consumed? In particular, how much medical care is available, and how much of other goods and services? How is medical care produced? For example, what mix of specific services is used in treating a particular episode of illness? Who receives particular treatments?
Physicians in all societies live and function in economic markets, although those markets differ greatly both from the simple competitive markets depicted in introductory economics textbooks and from country to country, depending on national institutions. Many of the differences between actual medical markets and textbook competitive markets cause what economists term market failure, a condition in which some individuals can be made better off without making anyone else worse off.
This chapter explains two features of health care financing that cause market failure: selection and moral hazard. A common response to market failure in medical care is what economists refer to as administered prices, which this chapter also describes. Unfortunately, administered prices exact a cost, leading to what economists call regulatory or government failure. All societies seek a balance between market failure and regulatory failure, a topic addressed in this chapter’s conclusion.
SELECTION
In the idealized competitive market found in economic textbooks, buyers and sellers have the same knowledge about the goods or services they are buying and selling. When one party knows more—or when goods of different quality are being sold at the same price, which is analytically similar—markets can break down in the following sense: There may be a price at which an equally well informed buyer and seller could make a transaction that would make them both better off, but that transaction does not occur because one party knows more than the other. Hence, both the potential buyer and the potential seller are worse off.
The used car market is a classic example of differential information. Owners of used cars (potential sellers) know more about the quality of their cars than do potential buyers. At any specific market price for a certain make and model of car, the only used cars offered will be those whose sellers value them at less than that price. Assuming that quality varies among used cars, those that are offered for sale will differentially be of low quality (“lemons”) relative to the given price. Owners of higher-quality cars may simply hold on to them. If, however, a potential buyer knew that the car was of higher quality, the buyer might be willing to pay enough so that the owner of the higher-quality car would sell. It is for this reason that sellers may offer warranties and guarantees, although these are uncommon (but not unknown) in medical care.
The same thing happens when goods of different quality are sold at the supermarket at the same price. Shoppers are happy to take any box of a particular brand of breakfast cereal or any bottle of a particular soft drink on the shelf because the quality of the contents of any box or bottle is the same; however, that is not the case in the produce section, where shoppers will inspect the fruit they pick up to ensure that the apple is not bruised or the banana overly ripe. At the end of the day, it is the bruised apples and overly ripe bananas that are left in the store. In effect, the seller has not used all the available information in pricing the produce, and buyers exploit that information differential.
Selection affects markets for individual—and, to some degree, small-group—health insurance in a fashion similar to that seen in the used car market and at the produce stand, but in this case it is the buyer of insurance who has more knowledge than the seller. Individuals who use above-average amounts of care—for example, those with a chronic disease or a strong proclivity to seek care for a symptom—will value health insurance more than will those who are healthy or who for various reasons shun medical care even if they are symptomatic. However, the insurer does not necessarily know the risk of those it insures, and so it gears insurance premiums to an average risk, which in some instances is conditional on certain observable characteristics, such as age. Just as shoppers do not want the bruised apples and used car buyers do not want lemons, many healthy people will not want to buy insurance voluntarily if its price mainly reflects its use by those who are sick. (Healthy but very risk-averse individuals still may be willing to pay premiums well above their expected use.) In an extreme case, healthy people drop out of the insurance pool, premiums rise because the average person left in the pool is sicker, that rise causes still more people to drop out of the pool, premiums rise further, and so forth, until few people remain to buy insurance.
For this reason, no developed country relies primarily on voluntary individual insurance to finance health care, although many countries use it in the supplemental insurance market, and selection is, in fact, often a feature of that market. Instead, governments and/or employers provide or heavily subsidize the purchase of either mandated or voluntary health insurance (e.g., in Canada or Germany, the Medicare and Medicaid programs in the United States and the purchase of insurance in exchanges by lower-income persons) or provide health services directly (e.g., the United Kingdom and the U.S. Veterans Health Administration). In addition, governments or third parties administering individual insurance markets with competing insurers may “risk-adjust” payments to insurers; that is, transfer monies from insurers who enroll better risks (as measured by observable features, such as diagnoses that are not used to rate premiums) to insurers who enroll worse risks. This feature is found in the American Medicare Advantage program and American insurance exchanges as well as in Germany and the Netherlands. The idea is to reduce insurers’ incentives to structure their products in order to appeal to good risks, especially when insurers are making choices about networks and formularies.
Moreover, countries that rely on employment-based health insurance, such as the United States and Germany, either mandate taxes to finance that insurance or provide large tax subsidies for its purchase; otherwise, many healthy employees would prefer that the employer give them the money the employer uses to subsidize the insurance as cash wages. Because an employer that offers health insurance will pay lower cash wages than an otherwise equivalent employer that does not, larger American employers that, before the Affordable Care Act was implemented in 2014, were not required to offer insurance may not, in fact, have offered it if they had many low-wage employees; the reason is that, if they had offered insurance, the cash wage they could afford to pay would have been below the minimum wage. (For the same reason, these employers typically do not offer a pension benefit.) Many low-wage employers, however, are small businesses that might not be viable if they had to subsidize health insurance. As a result, the Affordable Care Act exempted firms with fewer than 50 employees from any penalties if their employees received a public subsidy and purchased insurance in the exchange. Some self-employed individuals or those who work at small firms may belong to a trade association or a professional society through which they can purchase insurance, but because that purchase is voluntary, it is subject to selection.
How does this situation affect the practice of medicine? Prior to the Affordable Care Act, individual and small-group insurance policies typically had preexisting condition clauses to protect the insurer against selection—that is, to protect the insurer against a person’s purchasing insurance (or more complete insurance) after that person had been diagnosed with a disease that is expensive to treat. Even though there is now a penalty for remaining uninsured, some individuals still choose to do so, and others purchase insurance with substantial amounts of cost sharing that they may not be able to pay if they become sick. Caring for such patients may give the physician a choice between making do with less than clinically optimal treatment and proceeding in a clinically optimal way but leaving the patient with a large bill and possible bankruptcy—and potentially leaving the physician with bill collection issues or unpaid bills.
Selection can arise in a different guise when physicians are reimbursed a fixed amount per patient (i.e., capitation) rather than receiving fee-for-service payments. Depending on the adequacy of any adjustments in the capitated amount for the resources that a specific patient will require (“risk adjustment”), physicians who receive a fixed amount have a financial incentive to avoid caring for sicker patients. Similarly, physicians who receive a capitated amount for their own services but are not financially responsible for hospital care or the services of other physicians may make an excessive number of referrals, just as physicians reimbursed in a fee-for-service arrangement may make too few.
MORAL HAZARD
The term moral hazard comes from the actuarial literature; it originally referred to the weaker incentives of an insured individual to prevent the loss against which he or she is insured. A classic example is failure of homeowners in areas prone to brush fires to cut the brush around their houses or possibly install fire-resistant shingles on their roofs because of their expectation that insurance will compensate them if their houses burn down. In some lines of insurance, however, moral hazard is not a substantive issue. Persons who buy life insurance on their own lives are not likely to commit suicide so that their heirs can receive the proceeds. Moreover, despite the brush fire example, homeowner’s insurance probably has little moral hazard associated with it because individuals often cannot replace some valued personal items when a house burns down. In short, if moral hazard is negligible, insured persons take appropriate precautions against the potential loss.
In the context of health insurance, this classic form of moral hazard refers to potentially reduced incentives to prevent illness, but that is probably not a major issue. Sickness and disease generally imply some pain and suffering, not to mention possibly shortened life expectancy. Because there is no insurance for pain and suffering, individuals have strong incentives to try to remain healthy regardless of how much health insurance they have. Put another way, having better health insurance probably does not alter those incentives much.
Instead of weakened incentives to prevent illness, moral hazard in the health insurance context typically refers to the incentives for better-insured individuals to use more medical services. For instance, a patient with back pain or shoulder pain might seek an MRI if it costs him or her little or nothing, even if the physician feels the clinical value of the MRI is negligible. Conversely, the physician may be more cautious in ordering a test that seems likely to produce little information if there are severe financial consequences for the patient.
Some of the strongest evidence on this point comes from the randomized RAND Health Insurance Experiment conducted in the late 1970s and early 1980s. Families whose members were under 65 years of age were randomized to insurance plans in which the amount they had to pay when using services (“cost sharing”) varied from nothing (fully insured care) to a large deductible (catastrophic insurance). All the plans capped families’ annual out-of-pocket payments, with a reduced cap for low-income families. Families with complete insurance used ~40% more services in a year than did families with catastrophic insurance, a figure that did not vary much across the six geographically dispersed sites in which the experiment was run. Although these data come from the era before managed care in the United States, subsequent observational studies in this country and elsewhere have largely confirmed the experiment’s findings with respect to the relationship between variations in care use and variations in patient payment at the point of service. The difference among the plans was almost entirely related to the likelihood that a patient would seek care. Once care was sought, there appeared to be little difference in how physicians treated their patients in different plans.
One might assume that the additional care provided to fully insured patients would have resulted in improved outcomes, but by and large it did not. In fact, there was little or no difference in average health outcomes among the different health plans, with the important exception that hypertension, especially in patients with low incomes, was better controlled when care was free.
A possible explanation for the paucity of beneficial effects attributable to the additional medical services used by fully insured patients lies in the observations that (1) the additional care targeted both problems for which care can be efficacious and those for which it is not and (2) the population in the experiment, which consisted of nonelderly community-dwelling individuals, was mostly healthy. Perhaps the additional two visits and the greater number of hospitalizations when care was free were as likely to lead to poor outcomes as to good outcomes in that population. Certainly, the subsequent literature on quality of care and medical error rates has implied that a good deal of inappropriate care was—and is—provided to patients. For example, more than half of the antibiotics prescribed to the experiment’s participants were prescribed for viral conditions. Moreover, about one-quarter of patients who were hospitalized (in all plans) were admitted for procedures that could have been performed equally well outside the hospital, in line with the substantial decrease in hospital use over the last three decades. In short, the additional inappropriate care provided when care was free was not necessarily innocuous; if a mainly healthy person saw a physician, he or she could have been made worse off. The literature on inappropriate care is mostly American in origin, but the finding probably holds elsewhere as well.
Finally, patients’ health habits did not change in response to insurance status. This finding is consistent with the intuition that moral hazard does not much affect incentives to prevent illness.
Recently, another randomized experiment was conducted in Oregon among low-income, childless adults who were uninsured. Many people who gained insurance coverage in 2014 when the United States implemented the Affordable Care Act are from this group. Some of the uninsured childless adults won a lottery that made them eligible for Medicaid; those who did not win became the comparison group. After ~2 years, the results suggested that the use of services by persons on Medicaid had increased by ~25–35%. Medicaid served its purpose of providing protection against large medical bills; there was an 81% reduction in the proportion of families who spent >30% of their income on medical care, and there were large reductions in both medical debt and borrowing to pay for medical care. Turning to health outcomes, there was a 30% reduction in depression among the uninsured who received Medicaid relative to the comparison group as well as an increase in the numbers of diagnosed diabetics and of diabetics taking medication. Although there were no statistically significant changes in measures of blood pressure, lipids, or glycosylated hemoglobin, confidence intervals were sufficiently large that clinically meaningful effects could not be ruled out.
In sum, insurance is certainly desirable to protect families against the financial risk of large medical expenses and in some instances to address underuse of valuable medical services (e.g., by a patient with cardiovascular disease who fails to take medications for financial reasons). Thus, the remedy for moral hazard is not to abolish insurance but instead to strike the right balance between financial protection and incentives to seek care. Moreover, it is probably useful to vary the amounts that patients pay out of pocket, depending on the specific service and the patient’s clinical condition. Health outcomes after myocardial infarction, for example, were better among patients who were randomized to have no copayments for statins, beta blockers, angiotensin-converting enzyme inhibitors, and angiotensin receptor blockers than among those who had to pay for these drugs.
ADMINISTERED PRICES
Because insurers, whether public or private, cannot pay any price that a physician sets, prices in medical markets with widespread insurance are either set administratively or negotiated. In the simple textbook model of a competitive market, prices approximate the cost of production, but this is not necessarily the case when prices are administered. In the traditional American Medicare program, for example, the government sets a take-it-or-leave-it price. Because of the market share represented by the program, the great majority of physicians choose to take the government’s price rather than leave the program. In some countries (e.g., Canada and Germany), medical societies negotiate fees for all physicians in the nation or in a subnational area. In the United States, commercial insurers negotiate fees with individual physicians or groups of physicians.
The principal problem with administered prices arises because someone must set them and that person has an imperfect knowledge of cost. If the price that is set departs markedly from incremental cost, distortions inevitably result. Because the price-setter typically has little information about incremental cost, the set price could be, and often is, far from the actual cost. If the regulator sets the price below cost, the service may not be available or, if it is, will have to be cross-subsidized from a profitable service. If the price is set above cost, there may well be excess entry and too many services being offered on too small a scale. A beneficent regulator in theory could approximate a competitive price by trial and error if technology did not change, but that condition clearly does not hold in medical care. Not only do new goods and services appear continually, but physicians often become more skilled at delivering a service that is already available or at developing new tools to deliver that service at a different (and frequently lower) cost. For example, cataract surgery, which took upward of 8 h when first introduced, can now be completed in <30 min.
The distortions between price and cost when prices are administered have consequences for the way medical care is produced. There may well be too much capacity in “profitable” areas of medicine, such as cardiac services and sports medicine, and too little in less profitable areas, such as primary care. A fee above incremental cost for a procedure encourages more procedures.
Conversely, payment methods that attempt to cover many services with one fixed payment, such as capitation and a per-admission payment, pay nothing for doing more and therefore may result in too few services and in choices by providers to reduce the number of unprofitable patients under their care, much as a hospital may shutter an emergency room if it becomes a magnet for the uninsured. These phenomena also reflect the asymmetry of information between patients and physicians and, in the case of fee-for-service payment, the incentive for insured patients to go along with a recommendation for additional services (“I am pretty sure I know what the problem is, but let’s just carry out this additional test to be sure”).
There is good evidence that physicians respond to prices that are set. For example, if there is a general reduction in fees that, other things being equal, would lower practice income, some physicians order more services, whereas the opposite pertains if all fees increase. This behavior is sufficiently well established empirically that the U.S. Medicare program’s actuaries account for it in their estimates of what various changes in fees will cost or save. The outcome is different if the fee for one procedure or service changes and that procedure accounts for a modest proportion of income. In that case, another service can be substituted. For example, if the fee for a mastectomy increases relative to that for breast-conserving surgery, there will be a higher proportion of mastectomies. A particularly striking example of this type of behavior occurred when Medicare sharply reduced the fees it paid oncologists for chemotherapy in 2005. The proportion of lung cancer patients who received chemotherapy rose by 10%. Margins for some chemotherapeutic agents, however, were cut more than those for other agents, and thereafter oncologists made less use of the agents whose margins had fallen more.
Negotiated prices may get closer to cost than administered prices that are set, but they are not a panacea. First, negotiated prices may well exceed cost when there is no effective competition among similar physicians in a particular market. Because medical care markets are typically local, there may only be one group or a few groups in any particular specialty in a smaller market, in which case physicians will have considerable market power to obtain more favorable reimbursement. Further increasing physicians’ market power is the fact that many, and probably most, patients are reluctant to change physicians because their current physician knows their medical history, because they are uncertain whether a new physician would be an improvement, and because insurance may shield them from most of the cost differences among physicians. Finally, in the United States, commercial insurers often negotiate fees as a multiple of the Medicare fee schedule; thus, any distortion in administratively determined relative fees is carried over into negotiated fees. For example, in the Medicare fee schedule, procedures generally are more profitable than cognitive services known as “evaluation and management,” and this difference probably plays a role in the numerical insufficiency of primary care physicians in the United States.
CONCLUSION
One branch of economics—positive economics—seeks to explain actual phenomena without making a judgment about the desirability of those phenomena. Another branch—normative economics—seeks to prescribe what should happen and, in particular, what public policy should be developed to ensure that it happens. The main result of the application of normative economics is that, under certain very special assumptions, competitive markets result in a system in which no one can be made better off without another person’s being made worse off. These assumptions do not hold in medical care, in part because of selection and moral hazard; economists term the result a market failure. By contrast, as the discussion of administered prices in this chapter indicates, even a beneficent regulator will introduce distortions from lack of sufficient information; moreover, there is no guarantee that a regulator will be beneficent, as periodic corruption scandals show. Economists term this phenomenon regulatory or government failure. Economists see decisions about the proper form and amount of public intervention and regulation in medical care as a matter of finding the right balance between various types of market failures and various types of regulatory failures—a balance that different societies may choose to strike differently.
16e |
Racial and Ethnic Disparities in Health Care |
Over the course of its history, the United States has experienced dramatic improvements in overall health and life expectancy, largely as a result of initiatives in public health, health promotion, disease prevention, and chronic care management. Our ability to prevent, detect, and treat diseases in their early stages has allowed us to target and reduce rates of morbidity and mortality. Despite interventions that have improved the overall health of the majority of Americans, racial and ethnic minorities (blacks, Hispanics/Latinos, Native Americans/Alaskan Natives, Asian/Pacific Islanders) have benefited less from these advances than whites and have suffered poorer health outcomes from many major diseases, including cardiovascular disease, cancer, and diabetes. Research has revealed that minorities may receive less care and lower-quality care than whites, even when confounders such as stage of presentation, comorbidities, and health insurance are controlled. These differences in quality are called racial and ethnic disparities in health care. Addressing these disparities has taken on greater importance with the significant transformation of the U.S. health care system and the implementation of health care reform and value-based purchasing. The shift toward creating financial incentives and disincentives to achieve quality goals makes focusing on those who receive lower-quality care more important than ever before. This chapter will provide an overview of racial and ethnic disparities in health and health care, identify root causes, and provide key recommendations to address these disparities at both the clinical and health system levels.
NATURE AND EXTENT OF DISPARITIES
Minority Americans have poorer health outcomes than whites from preventable and treatable conditions such as cardiovascular disease, diabetes, asthma, cancer, and HIV/AIDS (Fig. 16e-1). Multiple factors contribute to these racial and ethnic disparities in health. First and foremost, social determinants—such as lower socioeconomic status (SES; e.g., lower income, less wealth, and lower educational attainment), inadequate and unsafe housing, and racism—are strongly linked to poor health outcomes. These factors disproportionately impact minority populations. In fact, SES has consistently been found to be one of the strongest predictors of health outcomes. While the mechanisms are complex (i.e., does poverty cause poor health, or does poor health cause poverty?), it is clear that low-SES populations experience disparities in health and that low SES is a major factor in racial/ethnic disparities.
FIGURE 16e-1 Age-adjusted death rates for selected causes by race and Hispanic origin, 2005. (From the U.S. Census Bureau, 2009.)
Racial/ethnic disparities are documented globally, although their assessment has centered more on the comparison of individuals by SES in other countries than in the United States. Similar to the U.S. pattern, low-SES residents of other nations tend to have poorer health outcomes. It is noteworthy that results are mixed when the health status of nations is compared by SES. High-SES nations such as the United States do not necessarily have health outcomes that correlate with their high expenditures for health care. For example, as of 2011, the United States ranks 34th in the world—just behind Cuba—on basic public health measures such as infant mortality. This ranking may be due in part to the correlation between wealth distribution and SES rather than just absolute SES. This area of active research is outside the scope of this chapter.
Racism has more recently been shown to predict poorer health outcomes. The physiologic impact of the stress imposed by racism (and poverty), including increased cortisol levels, can lead to chronic adverse effects on health. Lack of access to care also takes a significant toll. Uninsured individuals are less likely to have a regular source of care and are more likely to delay seeking care and to go without needed care; this limited access results in avoidable hospitalizations, emergency hospital care, and adverse health outcomes.
In addition to racial and ethnic disparities in health, there are racial and ethnic disparities in the quality of care for persons with access to the health care system. For instance, disparities have been found in the treatment of pneumonia (Fig. 16e-2) and congestive heart failure, with blacks receiving less optimal care than whites when hospitalized for these conditions. Moreover, blacks with end-stage renal disease are referred less often to the transplant list than are their white counterparts (Fig. 16e-3). Disparities have been found, for example, in the use of cardiac diagnostic and therapeutic procedures (with blacks being referred less often than whites for cardiac catheterization and bypass grafting), prescription of analgesia for pain control (with blacks and Latinos receiving less pain medication than whites for long-bone fractures and cancer), and surgical treatment of lung cancer (with blacks receiving less curative surgery than whites for non-small-cell lung cancer). Again, many of these disparities have occurred even when variations in factors such as insurance status, income, age, comorbid conditions, and symptom expression are taken into account. However, one additional factor—disparities in the quality of care provided at the sites where minorities tend to receive care—has been shown to be an important contributor to overall disparities.
FIGURE 16e-2 Recommended hospital care received by Medicare patients with pneumonia, by race/ethnicity, 2006. The reference population consisted of Medicare beneficiaries with pneumonia who were hospitalized. The composite was calculated by averaging the percentage of the population that received each of the five incorporated components of care. (Adapted from Agency for Healthcare Research and Quality: The 2008 National Health Care Disparities Report.)
FIGURE 16e-3 Referral for evaluation at a transplantation center or placement on a waiting list/receipt of a renal transplant within 18 months after the start of dialysis among patients who wanted a transplant, according to race and sex. The reference population consisted of 239 black women, 280 white women, 271 black men, and 271 white men. Racial differences were statistically significant among both the women and the men (p<.0001 for each comparison). (From JZ Ayanian et al: N Engl J Med 341:1661, 1999.)
Little progress has been made in addressing racial/ethnic disparities in cardiovascular procedures and other advanced surgical procedures, whereas some progress has been made in eliminating disparities in primary-care process measures. Data from the National Registry of Myocardial Infarction found evidence of continued disparities in guideline-based admission, procedural, and discharge therapy use from 1994 to 2006. Black patients were less likely than white patients to receive percutaneous coronary intervention/coronary artery bypass grafting (PCI/CABG), a disparity that has improved little since 1994. Further, compared with whites, black patients were less likely to receive lipid-lowering medications at discharge, with a gap that has widened since 1998 (Fig. 16e-4). A 2009 study showed that blacks had worse post–myocardial infarction outcomes than whites but that the difference could be explained by site of care and patient factors (such as socioeconomic status and comorbid conditions).
FIGURE 16e-4 Racial differences in guideline-based treatments for acute myocardial infarction (AMI). The reference population consisted of 2,515,106 patients with AMI admitted to U.S. hospitals between July 1990 and December 2006. CABG, coronary artery bypass grafting; PCI, percutaneous coronary intervention. (From ED Peterson et al: Am Heart J 156:1045, 2008.)
The Centers for Disease Control and Prevention (CDC) analyzed national and state rates of total knee replacement (TKR) for Medicare enrollees for the period 2000–2006, with patients stratified by sex, age, and black or white race. TKR rates overall in the United States increased 58%, with similar increases among whites (61%) and blacks (56%). However, the TKR rate for blacks was 37% lower than the rate for whites in 2000 and 39% lower in 2006; i.e., the disparity not only did not improve but even worsened slightly (Fig. 16e-5). More recent data (up to 2010) show no apparent change in these figures. Data for enrollees in Medicare managed-care plans provides evidence for a narrowing in racial disparities between 1997 and 2003 in several “report card” preventive care measures, such as mammography and glucose and cholesterol testing. However, racial disparities in more complex measures, such as glucose control in diabetic patients and cholesterol levels in patients after a heart attack, actually worsened during that interval.
FIGURE 16e-5 Racial trends in age-adjusted total knee replacement in Medicaid enrollees from 2000 to 2006. The reference population consisted of Medicaid part A enrollees ≥65 years of age who were not members of a managed-care plan. (From the Centers for Disease Control and Prevention, 2009.)
The 2012 National Healthcare Disparities Report, released by the Agency for Healthcare Research and Quality, found little improvement in disparities for core measures of quality over the previous decade. In fact, for blacks, Asians, Native Americans/Alaskan Natives, Hispanics, and poor people, the vast majority of core quality measures (87–92%) stayed the same, and a small proportion (2–8%) got worse, including measures of effectiveness, patient safety, and timeliness of care. While a small number of these measures improved, disparities were eliminated in no measured area. This annual report is particularly important, given that most studies of disparities have not been repeated with the same methodology used to document possible trends. Some studies have tracked disparities using specific disease and treatment registries. For example, by 2008, the use of acute and discharge medications for myocardial infarction had largely been equalized among racial and ethnic groups; however, African-American and Hispanic patients still experienced longer delays before reperfusion, with door-to-balloon times of <90 min for 83% of white patients as opposed to 75% and 76% of black and Hispanic patients, respectively.
ROOT CAUSES OF DISPARITIES
The Institute of Medicine (IOM) report Unequal Treatment, released in March 2002, remains the preeminent study of racial and ethnic disparities in health care in the United States. The IOM was charged with assessing the extent of racial/ethnic differences in health care that are not otherwise attributable to known factors, such as access to care. To provide recommendations regarding interventions aimed at eliminating health care disparities, the IOM studied health system, provider, and patient factors. The study found the following:
• Racial and ethnic disparities in health care exist and, because they are associated with worse health outcomes, are unacceptable.
• Racial and ethnic disparities in health care occur in the context of (1) broader historic and contemporary social and economic inequality and (2) evidence of persistent racial and ethnic discrimination in many sectors of American life.
• Many sources—including health systems, health care providers, patients, and utilization managers—may contribute to racial and ethnic disparities in health care.
• Bias, stereotyping, prejudice, and clinical uncertainty on the part of health care providers may contribute to racial and ethnic disparities in health care.
• A small number of studies suggest that minority patients may be more likely to refuse treatments, yet these refusal rates are generally small and do not fully explain health care disparities.
Unequal Treatment went on to identify a set of root causes that included the following:
• Health system factors: These include issues related to the complexity of the health care system, the difficulty that minority patients may have in navigating this complex system, and the lack of availability of interpreter services to assist patients with limited English proficiency. In addition, health care systems are generally ill prepared to identify and address disparities.
• Provider-level factors: These include issues related to the health care provider, including stereotyping, the impact of race/ethnicity on clinical decision-making, and clinical uncertainty due to poor communication.
• Patient-level factors: These include patients’ mistrust of the health care system leading to refusal of services, poor adherence to treatment, and delay in seeking care.
A more detailed analysis of these root causes is presented below.
Health System Factors • HEALTH SYSTEM COMPLEXITY Even among persons who are insured and educated and who have a high degree of health literacy, navigating the U.S. health care system can be complicated and confusing. Some individuals may be at higher risk for receiving substandard care because of their difficulty navigating the system’s complexities. These individuals may include those from cultures unfamiliar with the Western model of health care delivery, those with limited English proficiency, those with low health literacy, and those who are mistrustful of the health care system. These individuals may have difficulty knowing how and where to go for a referral to a specialist; how to prepare for a procedure such as a colonoscopy; or how to follow up on an abnormal test result such as a mammogram. Since people of color in the United States tend to be overrepresented among the groups listed above, the inherent complexity of navigating the health care system has been seen as a root cause for racial/ethnic disparities in health care.
OTHER HEALTH SYSTEM FACTORS Racial/ethnic disparities are due not only to differences in care provided within hospitals but also to where and from whom minorities receive their care; i.e., certain specific providers, geographic regions, or hospitals are lower-performing on certain aspects of quality. For example, one study showed that 25% of hospitals cared for 90% of black Medicare patients in the United States and that these hospitals tended to have lower performance scores on certain quality measures than other hospitals. That said, health systems generally are not well prepared to measure, report, and intervene to reduce disparities in care. Few hospitals or health plans stratify their quality data by race/ethnicity or language to measure disparities, and even fewer use data of this type to develop disparity-targeted interventions. Similarly, despite regulations concerning the need for professional interpreters, research demonstrates that many health care organizations and providers fail to routinely provide this service for patients with limited English proficiency. Despite the link between limited English proficiency and health-care quality and safety, few providers or institutions monitor performance for patients in these areas.
Provider-Level Factors • PROVIDER–PATIENT COMMUNICATION Significant evidence highlights the impact of sociocultural factors, race, ethnicity, and limited English proficiency on health and clinical care. Health care professionals frequently care for diverse populations with varied perspectives, values, beliefs, and behaviors regarding health and well-being. The differences include variations in the recognition of symptoms, thresholds for seeking care, comprehension of management strategies, expectations of care (including preferences for or against diagnostic and therapeutic procedures), and adherence to preventive measures and medications. In addition, sociocultural differences between patient and provider influence communication and clinical decision-making and are especially pertinent: evidence clearly links provider–patient communication to improved patient satisfaction, regimen adherence, and better health outcomes (Fig. 16e-6). Thus, when sociocultural differences between patient and provider are not appreciated, explored, understood, or communicated effectively during the medical encounter, patient dissatisfaction, poor adherence, poorer health outcomes, and racial/ethnic disparities in care may result.
FIGURE 16e-6 The link between effective communication and patient satisfaction, adherence, and health outcomes. (From the Institute of Medicine: Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC, National Academy Press, 2002.)
A survey of 6722 Americans ≥18 years of age is particularly relevant to this important link between provider–patient communication and health outcomes. Whites, blacks, Hispanics/Latinos, and Asian Americans who had made a medical visit in the past 2 years were asked whether they had trouble understanding their doctors; whether they felt the doctors did not listen; and whether they had medical questions they were afraid to ask. The survey found that 19% of all patients experienced one or more of these problems, yet whites experienced them 16% of the time as opposed to 23% of the time for blacks, 33% for Hispanics/Latinos, and 27% for Asian Americans (Fig. 16e-7).
FIGURE 16e-7 Communication difficulties with physicians, by race/ethnicity. The reference population consisted of 6722 Americans ≥18 years of age who had made a medical visit in the previous 2 years and were asked whether they had had trouble understanding their doctors, whether they felt that the doctors had not listened, and whether they had had medical questions they were afraid to ask. (From the Commonwealth Fund Health Care Quality Survey, 2001.)
In addition, in the setting of even a minimal language barrier, provider–patient communication without an interpreter is recognized as a major challenge to effective health care delivery. These communication barriers for patients with limited English proficiency lead to frequent misunderstanding of diagnosis, treatment, and follow-up plans; inappropriate use of medications; lack of informed consent for surgical procedures; high rates of serious adverse events; and a lower-quality health care experience than is provided to patients who speak fluent English. Physicians who have access to trained interpreters report a significantly higher quality of patient–physician communication than physicians who use other methods. Communication issues related to discordant language disproportionately affect minorities and likely contribute to racial/ethnic disparities in health care.
CLINICAL DECISION-MAKING Theory and research suggest that variations in clinical decision-making may contribute to racial and ethnic disparities in health care. Two factors are central to this process: clinical uncertainty and stereotyping.
First, a doctor’s decision-making process is nested in clinical uncertainty. Doctors depend on inferences about severity based on what they understand about illness and the information obtained from the patient. A doctor caring for a patient whose symptoms he or she has difficulty understanding and whose “signals”—the set of clues and indications that physicians rely on to make clinical decisions—are hard to read may make a decision different from the one that would be made for another patient who presents with exactly the same clinical condition. Given that the expression of symptoms may differ among cultural and racial groups, doctors—the overwhelming majority of whom are white—may understand symptoms best when expressed by patients of their own racial/ethnic groups. The consequence is that white patients may be treated differently from minority patients. Differences in clinical decisions can arise from this mechanism even when the doctor has the same regard for each patient (i.e., is not prejudiced).
Second, the literature on social cognitive theory highlights how natural tendencies to stereotype may influence clinical decision-making. Stereotyping can be defined as the way in which people use social categories (e.g., race, gender, age) in acquiring, processing, and recalling information about others. Faced with enormous information loads and the need to make many decisions, people often subconsciously simplify the decision-making process and lessen cognitive effort by using “categories” or “stereotypes” that bundle information into groups or types that can be processed more quickly. Although functional, stereotyping can be systematically biased, as people are automatically classified into social categories based on dimensions such as race, gender, and age. Many people may not be aware of their attitudes, may not consciously endorse specific stereotypes, and paradoxically may consider themselves egalitarian and not prejudiced.
Stereotypes may be strongly influenced by the messages presented consciously and unconsciously in society. For instance, if the media and our social/professional contacts tend to present images of minorities as being less educated, more violent, and nonadherent to health care recommendations, these impressions may generate stereotypes that unnaturally and unjustly impact clinical decision-making. As signs of racism, classism, gender bias, and ageism are experienced (consciously or unconsciously) in our society, stereotypes may be created that impact the way doctors manage patients from these groups. On the basis of training or practice location, doctors may develop certain perceptions about race/ethnicity, culture, and class that may evolve into stereotypes. For example, many medical students and residents are often trained—and minorities cared for—in academic health centers or public hospitals located in socioeconomically disadvantaged areas. As a result, doctors may begin to equate certain races and ethnicities with specific health beliefs and behaviors (e.g., “these patients” engage in risky behaviors, “those patients” tend to be noncompliant) that are more associated with the social environment (e.g., poverty) than with a patient’s racial/ethnic background or cultural traditions. This “conditioning” phenomenon may also be operative if doctors are faced with certain racial/ethnic patient groups who frequently do not choose aggressive forms of diagnostic or therapeutic intervention. The result over time may be that doctors begin to believe that “these patients” do not like invasive procedures; thus they may not offer these procedures as options. A wide range of studies have documented the potential for provider biases to contribute to racial/ethnic disparities in health care. For example, one study measured physicians’ unconscious (or implicit) biases and showed that these were related to differences in decisions to provide thrombolysis for a hypothetical black or white patient with a myocardial infarction.
It is important to differentiate stereotyping from prejudice and discrimination. Prejudice is a conscious prejudgment of individuals that may lead to disparate treatment, and discrimination is conscious and intentional disparate treatment. All individuals stereotype subconsciously, yet, if left unquestioned, these subconscious assumptions may lead to lower-quality care for certain groups because of differences in clinical decision-making or differences in communication and patient-centeredness. For example, one study tested physicians’ unconscious racial/ethnic biases and showed that patients perceived more biased physicians as being less patient-centered in their communication. What is particularly salient is that stereotypes tend to be activated most in environments where the individual is stressed, multitasking, and under time pressure—the hallmarks of the clinical encounter.
Patient-Level Factors Lack of trust has become a major concern for many health care institutions today. For example, an IOM report, To Err Is Human: Building a Safer Health System, documented alarming rates of medical errors that made patients feel vulnerable and less trustful of the U.S. health care system. The increased media and academic attention to problems related to quality of care (and of disparities themselves) has clearly diminished trust in doctors and nurses.
Trust is a crucial element in the therapeutic alliance between patient and health care provider. It facilitates open communication and is directly correlated with adherence to the physician’s recommendations and the patient’s satisfaction. In other words, patients who mistrust their health care providers are less satisfied with the care they receive, and mistrust of the health care system greatly affects patients’ use of services. Mistrust can also result in inconsistent care, “doctor-shopping,” self-medication, and an increased demand by patients for referrals and diagnostic tests.
On the basis of historic factors such as discrimination, segregation, and medical experimentation, blacks may be especially mistrustful of providers. The exploitation of blacks by the U.S. Public Health Service during the Tuskegee syphilis study from 1932 to 1972 left a legacy of mistrust that persists even today among this population. Other populations, including Native Americans/Alaskan Natives, Hispanics/Latinos, and Asian Americans, also harbor significant mistrust of the health care system. A national Kaiser Family Foundation survey of 3884 individuals found that 36% of Hispanics and 35% of blacks (compared with 15% of whites) felt they had been treated unfairly in the health care system in the past because of their race/ethnicity. Perhaps even more alarming, 65% of blacks and 58% of Hispanics (compared with 22% of whites) were afraid of being treated unfairly in the future on that basis (Fig. 16e-8).
FIGURE 16e-8 Patient perspectives regarding unfair treatment (Tx) based on race/ethnicity. The reference population consisted of 3884 individuals surveyed about how fairly they had been treated in the health care system in the past and how fairly they felt they would be treated in the future on the basis of their race/ethnicity. (From Race, Ethnicity & Medical Care: A Survey of Public Perceptions and Experiences. Kaiser Family Foundation, 2005.)
This mistrust may contribute to wariness in accepting or following recommendations, undergoing invasive procedures, or participating in clinical research, and these choices, in turn, may lead to misunderstanding and the perpetuation of stereotypes among health professionals.
KEY RECOMMENDATIONS TO ADDRESS RACIAL/ETHNIC DISPARITIES IN HEALTH CARE
The publication Unequal Treatment provides a series of recommendations to address racial and ethnic disparities in health care, focusing on a broad set of stakeholders. These recommendations include health system interventions, provider interventions, patient interventions, and general recommendations, which are described in more detail below.
Health System Interventions • COLLECTION AND REPORTING OF DATA ON HEALTH CARE ACCESS AND USE, BY PATIENTS’ RACE/ETHNICITY Unequal Treatment found that the appropriate systems to track and monitor racial and ethnic disparities in health care are lacking and that less is known about the disparities affecting minority groups other than African Americans (Hispanics, Asian Americans, Pacific Islanders, Native Americans, and Alaskan Natives). For instance, only in the mid-1980s did the Medicare database begin to collect data on patient groups outside the standard categories of “white,” “black,” and “other.” Federal, private, and state-supported data-collection efforts are scattered and unsystematic, and many health care systems and hospitals still do not collect data on the race, ethnicity, or primary language of enrollees or patients. A survey by Regenstein and Sickler in 2006 found that 78% of 501 U.S. hospitals collected information on race, 50% collected data on ethnicity, and 50% collected data on primary language. However, the information was not collected by standard categories or collection methods and thus was of questionable accuracy. Surveys by America’s Health Insurance Plans in 2003 and 2006 showed that the proportion of enrollees in plans that collected race/ethnicity data of some type increased from 54% to 67%; however, the total percentage of plan enrollees whose race/ethnicity and language are recorded is still much lower than these figures.
ENCOURAGEMENT OF THE USE OF EVIDENCE-BASED GUIDELINES AND QUALITY IMPROVEMENT Unequal Treatment highlights the subjectivity of clinical decision-making as a potential cause of racial and ethnic disparities in health care by describing how clinicians—despite the existence of well-delineated practice guidelines—may offer (consciously or unconsciously) different diagnostic and therapeutic options to different patients on the basis of their race or ethnicity. Therefore, the widespread adoption and implementation of evidence-based guidelines is a key recommendation in eliminating disparities. For instance, evidence-based guidelines are now available for the management of diabetes, HIV/AIDS, cardiovascular diseases, cancer screening and management, and asthma—all areas where significant disparities exist. As part of ongoing quality-improvement efforts, particular attention should be paid to the implementation of evidence-based guidelines for all patients, regardless of their race and ethnicity.
SUPPORT FOR THE USE OF LANGUAGE INTERPRETATION SERVICES IN THE CLINICAL SETTING As described previously, a lack of efficient and effective interpreter services in a health care system can lead to patient dissatisfaction, to poor comprehension and adherence, and thus to ineffective/lower-quality care for patients with limited English proficiency. Unequal Treatment’s recommendation to support the use of interpretation services has clear implications for delivery of quality health care by improving doctors’ ability to communicate effectively with these patients.
INCREASES IN THE PROPORTION OF UNDERREPRESENTED MINORITIES IN THE HEALTH CARE WORKFORCE Data for 2004 from the Association of American Medical Colleges indicate that, of the 72.4% of U.S. physicians whose race and ethnicity are known, Hispanics make up 2.8%, blacks 3.3%, and Native American and Alaskan Natives 0.3%. Furthermore, U.S. national data show that minorities (excluding Asians) compose just 7.5% of medical school faculty. In addition, minority faculty in 2007 were more likely to be at or below the rank of assistant professor, while whites composed the highest proportion of full professors. Despite representing ∼26% of the U.S. population (a number projected to almost double by 2050), minority students are still underrepresented in medical schools. In 2007, matriculants to U.S. medical schools were 7.2% Latino, 6.4% African American, 0.2% Native Hawaiian or Other Pacific Islander, and 0.3% Native American or Alaskan Native. These percentages have decreased or remained the same since 2007. It will be difficult to develop a diverse health-care workforce that can meet the needs of an increasingly diverse population without dramatic changes in the racial and ethnic composition of medical student bodies.
Provider Interventions • INTEGRATION OF CROSS-CULTURAL EDUCATION INTO THE TRAINING OF ALL HEALTH CARE PROFESSIONALS The goal of cross-cultural education is to improve providers’ ability to understand, communicate with, and care for patients from diverse backgrounds. Such education focuses on enhancing awareness of sociocultural influences on health beliefs and behaviors and on building skills to facilitate understanding and management of these factors in the medical encounter. Cross-cultural education includes curricula on health care disparities, use of interpreters, and effective communication and negotiation across cultures. These curricula can be incorporated into health-professions training in medical schools, residency programs, and nursing schools and can be offered as a component of continuing education. Despite the importance of this area of education and the attention it has attracted from medical education accreditation bodies, a national survey of senior resident physicians by Weissman and colleagues found that up to 28% felt unprepared to deal with cross-cultural issues, including caring for patients who have religious beliefs that may affect treatment, patients who use complementary medicine, patients who have health beliefs at odds with Western medicine, patients who mistrust the health care system, and new immigrants. In a study at one medical school, 70% of fourth-year students felt inadequately prepared to care for patients with limited English proficiency. Efforts to incorporate cross-cultural education into medical education will contribute to improving communication and to providing a better quality of care for all patients.
INCORPORATION OF TEACHING ON THE IMPACT OF RACE, ETHNICITY, AND CULTURE ON CLINICAL DECISION-MAKING Unequal Treatment and more recent studies found that stereotyping by health care providers can lead to disparate treatment based on a patient’s race or ethnicity. The Liaison Committee on Medical Education, which accredits medical schools, issued a directive that medical education should include instruction on how a patient’s race, ethnicity, and culture might unconsciously impact communication and clinical decision-making.
Patient Interventions Difficulty navigating the health care system and obtaining access to care can be a hindrance to all populations, particularly to minorities. Similarly, lack of empowerment or involvement in the medical encounter by minorities can be a barrier to care. Patients need to be educated on how to navigate the health care system and how best to access care. Interventions should be used to increase patients’ participation in treatment decisions.
General Recommendations • INCREASE AWARENESS OF RACIAL/ETHNIC DISPARITIES IN HEALTH CARE Efforts to raise awareness of racial/ethnic health care disparities have done little for the general public but have been fairly successful among physicians, according to a Kaiser Family Foundation report. In 2006, nearly 6 in 10 people surveyed believed that blacks received the same quality of care as whites, and 5 in 10 believed that Latinos received the same quality of care as whites. These estimates are similar to findings in a 1999 survey. Despite this lack of awareness, most people believed that all Americans deserve quality care, regardless of their background. In contrast, the level of awareness among physicians has risen sharply. In 2002, the majority (69%) of physicians said that the health care system “rarely or never” treated people unfairly on the basis of their racial/ethnic background. In 2005, less than one-quarter (24%) of physicians disagreed with the statement that “minority patients generally receive lower-quality care than white patients.” Increasing awareness of racial and ethnic health disparities among health care professionals and the public is an important first step in addressing these disparities. The ultimate goals are to generate discourse and to mobilize action to address disparities at multiple levels, including health policy makers, health systems, and the community.
CONDUCT FURTHER RESEARCH TO IDENTIFY SOURCES OF DISPARITIES AND PROMISING INTERVENTIONS While the literature that formed the basis for the findings reported and recommendations made in Unequal Treatment provided significant evidence for racial and ethnic disparities, additional research is needed in several areas. First, most of the literature on disparities focuses on black-versus-white differences; much less is known about the experiences of other minority groups. Improving the ability to collect racial and ethnic patient data should facilitate this process. However, in instances where the necessary systems are not yet in place, racial and ethnic patient data may be collected prospectively in the setting of clinical or health services research to more fully elucidate disparities for other populations. Second, much of the literature on disparities to date has focused on defining areas in which these disparities exist, but less has been done to identify the multiple factors that contribute to the disparities or to test interventions to address these factors. There is clearly a need for research that identifies promising practices and solutions to disparities.
IMPLICATIONS FOR CLINICAL PRACTICE
Individual health care providers can do several things in the clinical encounter to address racial and ethnic disparities in health care.
Be Aware that Disparities Exist Increasing awareness of racial and ethnic disparities among health care professionals is an important first step in addressing disparities in health care. Only with greater awareness can care providers be attuned to their behavior in clinical practice and thus monitor that behavior and ensure that all patients receive the highest quality of care, regardless of race, ethnicity, or culture.
Practice Culturally Competent Care Previous efforts have been made to teach clinicians about the attitudes, values, beliefs, and behaviors of certain cultural groups—the key practice “dos and don’ts” in caring for “the Hispanic patient” or the “Asian patient,” for example. In certain situations, learning about a particular local community or cultural group, with a goal of following the principles of community-oriented primary care, can be helpful; when broadly and uncritically applied, however, this approach can actually lead to stereotyping and oversimplification of culture, without respect for its complexity.
Cultural competence has thus evolved from merely learning information and making assumptions about patients on the basis of their backgrounds to focusing on the development of skills that follow the principles of patient-centered care. Patient-centeredness encompasses the qualities of compassion, empathy, and responsiveness to the needs, values, and expressed preferences of the individual patient. Cultural competence aims to take things a step further by expanding the repertoire of knowledge and skills classically defined as “patient-centered” to include those that are especially useful in cross-cultural interactions (and that, in fact, are vital in all clinical encounters). This repertoire includes effectively using interpreter services, eliciting the patient’s understanding of his or her condition, assessing decision-making preferences and the role of family, determining the patient’s views about biomedicine versus complementary and alternative medicine, recognizing sexual and gender issues, and building trust. For example, while it is important to understand all patients’ beliefs about health, it may be particularly crucial to understand the health beliefs of patients who come from a different culture or have a different health care experience. With the individual patient as teacher, the physician can adjust his or her practice style to meet the patient’s specific needs.
Avoid Stereotyping Several strategies can allow health care providers to counteract, both systemically and individually, the normal tendency to stereotype. For example, when racially/ethnically/culturally/socially diverse teams in which each member is given equal power are assembled and are tasked to achieve a common goal, a sense of camaraderie develops and prevents the development of stereotypes based on race/ethnicity, gender, culture, or class. Thus, health care providers should aim to gain experiences working with and learning from a diverse set of colleagues. In addition, simply being aware of the operation of social cognitive factors allows providers to actively check up on or monitor their behavior. Physicians can constantly reevaluate to ensure that they are offering the same things, in the same ways, to all patients. Understanding one’s own susceptibility to stereotyping—and how disparities may result—is essential in providing equitable, high-quality care to all patients.
Work to Build Trust Patients’ mistrust of the health care system and of health care providers impacts multiple facets of the medical encounter, with effects ranging from decreased patient satisfaction to delayed care. Although the historic legacy of discrimination can never be erased, several steps can be taken to build trust with patients and to address disparities. First, providers must be aware that mistrust exists and is more prevalent among minority populations, given the history of discrimination in the United States and other countries. Second, providers must reassure patients that they come first, that everything possible will be done to ensure that they always get the best care available, and that their caregivers will serve as their advocates. Third, interpersonal skills and communication techniques that demonstrate honesty, openness, compassion, and respect on the part of the health care provider are essential tools in dismantling mistrust. Finally, patients indicate that trust is built when there is shared, participatory decision-making and the provider makes a concerted effort to understand the patient’s background. When the doctor–patient relationship is reframed as one of solidarity, the patient’s sense of vulnerability can be transformed into one of trust. The successful elimination of disparities requires trust-building interventions and strengthening of this relationship.
CONCLUSION
The issue of racial and ethnic disparities in health care has gained national prominence, both with the release of the IOM report Unequal Treatment and with more recent articles that have confirmed their persistence and explored their root causes. Furthermore, another influential IOM report, Crossing the Quality Chasm, has highlighted the importance of equity—i.e., no variations in quality of care due to personal characteristics, including race and ethnicity—as a central principle of quality. Current efforts in health care reform and transformation, including a greater focus on value (high-quality care and cost-control), will sharpen the nation’s focus on the care of populations who experience low-quality, costly care. Addressing disparities will become a major focus, and there will be many obvious opportunities for interventions to eliminate them. Greater attention to addressing the root causes of disparities will improve the care provided to all patients, not just those who belong to racial and ethnic minorities.
ACKNOWLEDGMENT
The authors thank Marina Cervantes for her contributions to this chapter.
17e |
Ethical Issues in Clinical Medicine |
Twenty-first-century physicians face novel ethical dilemmas that can be perplexing and emotionally draining. For example, electronic medical records, handheld personal devices, and provision of care by interdisciplinary teams all hold the promise of more coordinated and comprehensive care but also raise new concerns about confidentiality, appropriate boundaries of the doctor–patient relationship, and responsibility. Chapter 1 puts the practice of medicine into a professional and historical context. The current chapter presents approaches and principles that physicians can use to address the ethical issues they encounter in their work. Physicians make ethical judgments about clinical situations every day. Traditional professional codes and ethical principles provide instructive guidance for physicians but need to be interpreted and applied to each situation. Physicians need to be prepared for lifelong learning about ethical issues and dilemmas as well as about new scientific and clinical developments. When struggling with difficult ethical issues, physicians may need to reevaluate their basic convictions, tolerate uncertainty, and maintain their integrity while respecting the opinions of others. Discussing perplexing ethical issues with other members of the health care team, ethics consultation services, or the hospital ethics committee can clarify issues and reveal strategies for resolution, including improving communication and dealing with strong or conflicting emotions.
APPROACHES TO ETHICAL PROBLEMS
Several approaches may be useful for resolving ethical issues. Among these approaches are those based on ethical principles, virtue ethics, professional oaths, and personal values. These various sources of guidance encompass precepts that may conflict in a particular case, leaving the physician in a quandary. In a diverse society, different individuals may turn to different sources of moral guidance. In addition, general moral precepts often need to be interpreted and applied in the context of a particular clinical situation. When facing an ethical challenge, physicians should articulate their concerns and reasoning, discuss and listen to the views of others involved in the case, and call on available resources as needed. Through these efforts, physicians can gain deeper insight into the ethical issues they face and often can reach mutually acceptable resolutions to complex problems.
ETHICAL PRINCIPLES
Ethical principles can serve as general guidelines to help physicians determine the right thing to do.
Respecting Patients Physicians should always treat patients with respect, which entails understanding patients’ goals, communicating effectively, obtaining informed and voluntary consent for interventions, respecting informed refusals, and protecting confidentiality. Different clinical goals and approaches are often feasible, and interventions can cause both benefit and harm. Individuals place different values on health and medical care and weigh the benefits and risks of medical interventions differently. Generally, the values and informed choices of patients should be respected.
OBTAINING INFORMED CONSENT To help patients make informed decisions, physicians should discuss with them the nature of the proposed care; the alternatives; and the risks, benefits, and likely consequences of each option. Informed consent involves more than obtaining signatures on consent forms. Physicians should promote shared decision-making by educating patients, answering their questions, making recommendations, and helping them deliberate. Patients can be overwhelmed by medical jargon, needlessly complicated explanations, or the provision of too much information at once. Patients can make informed decisions only if they receive honest and understandable information. Competent, informed patients may refuse recommended interventions and choose among reasonable alternatives. If patients cannot give consent in an emergency and if delay of treatment while surrogates are contacted will place their lives or health in peril, treatment can be given without informed consent. People are presumed to want such emergency care unless they have previously indicated otherwise.
Respect for patients does not entitle the patients to insist on any care they want. Physicians are not obligated to provide interventions that have no physiologic rationale, that have already failed, or that are contrary to evidence-based practice recommendations, good clinical judgment, or public policies. National policies and laws also dictate certain decisions—e.g., allocating cadaveric organs for transplantation and, in most states, prohibiting physician-assisted suicide.
Physicians should disclose and discuss relevant and accurate information about diagnosis, prognosis, and treatment options. To help patients cope with bad news, doctors can adjust the pace of disclosure, offer empathy and hope, provide emotional support, and call on other resources such as spiritual care or social work. Physicians may be tempted to withhold a serious diagnosis, misrepresent it by using ambiguous terms, or limit discussions of prognosis or risks for fear that certain information will make patients anxious or depressed. Providing honest information about clinical situations preserves patients’ autonomy and trust and promotes sound communication with patients and colleagues. However, patients may choose not to receive such information, asking surrogates to make decisions on their behalf, as is common with serious diagnoses in some traditional cultures.
AVOIDING DECEPTION Health care providers sometimes consider using lies or deception to obtain benefits for patients. Lying refers to statements known to be false and intended to mislead the listener. Deception includes statements and actions intended to mislead the listener, whether or not they are literally true. For example, a physician might sign a disability form for a patient who does not meet disability criteria. Although motivated by a desire to help the patient, such deception is ethically problematic because it undermines physicians’ credibility and trustworthiness.
MAINTAINING CONFIDENTIALITY Maintaining confidentiality is essential in respecting patients’ autonomy and privacy, encourages them to seek treatment and to discuss problems candidly, and prevents discrimination. However, confidentiality may be overridden to prevent serious harm to third parties or to the patient. Exceptions to confidentiality are justified if the risk is serious and probable, if there are no less restrictive measures by which to avert risk, if the adverse effects of overriding confidentiality are minimized, and if these adverse effects are deemed acceptable by society. For example, the law requires physicians to report cases of tuberculosis, sexually transmitted infection, elder or child abuse, and domestic violence.
CARING FOR PATIENTS WHO LACK DECISION-MAKING CAPACITY Some patients are not able to make informed decisions because of unconsciousness, dementia, delirium, or other medical conditions. Although only the courts have the legal authority to determine that a patient is incompetent for making medical decisions, in practice, physicians determine when patients lack the capacity to make health care decisions and arrange for surrogates to make decisions for them, without involving the courts. Patients with decision-making capacity can express a choice and appreciate the medical situation; the nature of the proposed care; the alternatives; and the risks, benefits, and consequences of each alternative. Their choices should be consistent with their values and not the result of delusions or hallucinations. Psychiatrists may help assess decision-making capacity in difficult cases. When impairments are fluctuating or reversible, decisions should be postponed if possible until the patient recovers decision-making capacity.
If a patient lacks decision-making capacity, physicians should ask: Who is the appropriate surrogate, and what would the patient want done? Patients may designate someone to serve as their health care proxy or to assume durable power of attorney for health care; such choices should be respected. (See Chap. 10 for further details about advance care planning.) Unless a patient without decision-making capacity has previously designated a health care proxy, physicians usually ask family members to serve as surrogates. Many patients want family members as surrogates, and family members generally have the patient’s best interests at heart. Statutes in most U.S. states delineate a prioritized list of relatives who may serve as surrogates if the patient has not designated a proxy. Surrogates’ decisions should be guided by the patient’s values, goals, and previously expressed preferences. However, it may be appropriate to override previous preferences in favor of the patient’s current best interests if an intervention is highly likely to provide a significant benefit, if previous statements do not fit the situation well, or if the patient expressed a desire for the surrogate to have leeway in making decisions.
ACTING IN THE BEST INTERESTS OF PATIENTS Respect for patients is broader than respecting their autonomy to make informed choices about their medical care and promoting shared decision-making. Physicians should also be compassionate and dedicated and should act in the best interests of their patients.
The principle of beneficence requires physicians to act for the patient’s benefit. Patients typically lack medical expertise and may be vulnerable because of their illness. They rely on physicians to provide sound recommendations and to promote their well-being. Physicians encourage such trust and have a fiduciary duty to act in the best interests of the patient, which should prevail over the physicians’ own self-interest or the interests of third parties, such as hospitals or insurers. Physicians’ fiduciary obligations contrast sharply with business relationships, which are characterized by “let the buyer beware,” not by reliance and trust. A related principle, “first do no harm,” forbids physicians to provide ineffective interventions or to act without due care. Although often cited, this precept alone provides only limited guidance because many beneficial interventions pose serious risks. Physicians should prevent unnecessary harm by recommending interventions that maximize benefit and minimize harm.
MANAGING CONFLICTS BETWEEN RESPECTING PATIENTS AND ACTING IN THEIR BEST INTERESTS Conflicts can arise when patients’ refusal of interventions thwarts their own goals for care or causes them serious harm. For example, if a young woman with asthma refuses mechanical ventilation for reversible respiratory failure, simple acceptance of this decision by the physician, in the name of respecting autonomy, is morally constricted. Physicians should elicit patients’ expectations and concerns, correct their misunderstandings, and try to persuade them to accept beneficial therapies. If disagreements persist after such efforts, patients’ informed choices and views of their own best interests should prevail. While refusing recommended care does not render a patient incompetent, it may lead the physician to probe further to ensure that the patient has the capacity to make informed decisions.
Acting Justly The principle of justice provides guidance to physicians about how to ethically treat patients and to make decisions about allocating important resources, including their own time. Justice in a general sense means fairness: people should receive what they deserve. In addition, it is important to act consistently in cases that are similar in ethically relevant ways. Otherwise, decisions may be arbitrary, biased, and unfair. Justice forbids discrimination in health care based on race, religion, gender, sexual orientation, or other personal characteristics (Chap. 16e).
Justice also requires that limited health care resources be allocated fairly. Universal access to medically needed health care remains an unrealized moral aspiration in the United States and much of the rest of the world. Patients without health insurance often cannot afford health care and lack access to safety-net services. Even among insured patients, insurers may deny coverage for interventions recommended by the physician. In this situation, physicians should advocate for patients and try to help them obtain needed care. Doctors might consider—or patients might request—the use of deception to obtain such benefits. However, avoiding deception is a basic ethical guideline that sets limits on advocating for patients.
Allocation of health care resources is unavoidable because these resources are limited. Ideally, decisions about allocation are made at the level of public policy, with physician input. For example, the United Network for Organ Sharing (www.unos.org) provides criteria for allocating scarce organs. Ad hoc resource allocation at the bedside is problematic because it may be inconsistent, unfair, and ineffective. Physicians have an important role, however, in avoiding unnecessary interventions. Evidence-based lists of tests and procedures that physicians and patients should question and discuss were developed through the recent initiative Choosing Wisely (http://www.choosingwisely.org/). At the bedside, physicians should act as patient advocates within constraints set by society, reasonable insurance coverage, and evidence-based practice. For example, if a patient’s insurer has a higher copayment for nonformulary drugs, it still may be reasonable for physicians to advocate for nonformulary products for good reasons (e.g., when the formulary drugs are ineffective or not tolerated).
VIRTUE ETHICS
Virtue ethics focuses on physicians’ character and qualities, with the expectation that doctors will cultivate such virtues as compassion, dedication, altruism, humility, and integrity. Proponents argue that, if such characteristics become ingrained, they help guide physicians in novel situations. Moreover, merely following ethical precepts or principles without these virtues leads to uncaring doctor–patient relationships.
PROFESSIONAL OATHS AND CODES
Professional oaths and codes are useful guides for physicians. Most physicians take oaths at student white-coat ceremonies and at medical school graduation, and many are members of professional societies that have professional codes. Members of the profession pledge to the public and to their patients that they will be guided by the principles and values in these oaths or codes. Oaths and codes focus physicians on ethical ideals rather than on daily pragmatic concerns. However, professional oaths and codes—even the Hippocratic tradition—have been criticized for lack of patient or public input and the limited role given to patients in making decisions.
PERSONAL VALUES
Personal values, cultural traditions, and religious beliefs are important sources of personal morality that help physicians address ethical issues and cope with the moral distress they may experience in practice. While essential, personal morality is a limited ethical guide in clinical practice. Physicians have role-specific ethical obligations that go beyond their obligations as good people, including the duties to obtain informed consent and maintain confidentiality discussed earlier in this chapter. Furthermore, in a culturally and religiously diverse world, patients and colleagues have personal moral beliefs that commonly differ from their physicians’.
Claims of Conscience Some physicians have conscientious objections to providing or referring patients for certain treatments, such as contraception. While physicians should not be asked to violate deeply held moral beliefs or religious convictions, patients need to receive medically appropriate, timely care. Institutions such as clinics and hospitals have a collective duty to provide care that patients need while making reasonable attempts to accommodate health care workers’ conscientious objections—for example, by arranging for another professional to provide the service in question. Patients seeking a relationship with a doctor or health care institution should be notified in advance of any conscientious objections to the provision of specific interventions. Since patients commonly must select providers for insurance purposes, switching providers when a specific service is needed would be burdensome. There are important limits on claims of conscience. Health care workers may not insist that patients receive unwanted medical interventions and may not refuse to treat patients because of their race, ethnicity, national origin, gender, or religion. Such discrimination is illegal and violates the physician’s duty to respect patients.
Moral Distress Physicians and other health care providers may experience moral distress when they feel they know the ethically correct action to take in a particular situation but are constrained by institutional policies, limited resources, or a position subordinate to the ultimate decision-maker. Moral distress can lead to anger, anxiety, frustration, fatigue, and work dissatisfaction. Discussing complex clinical situations with colleagues and seeking assistance with difficult decisions helps to alleviate moral distress, as does a healthy work environment characterized by open communication and mutual respect.
These various sources of guidance contain precepts that may conflict in a particular case, leaving the physician in a quandary. In a diverse society, different individuals may turn to different sources of moral guidance. In addition, general moral precepts often need to be interpreted and applied in the context of a particular clinical situation. When facing an ethical challenge, physicians should articulate their concerns and reasoning, discuss and listen to the views of others involved in the case, and call on available resources as needed. Through these efforts, physicians can gain deeper insight into the ethical issues they face and often reach mutually acceptable resolutions to complex problems.
CHANGES IN ORGANIZATION AND DELIVERY OF CARE
Recent changes in the organization and delivery of health care have led to new ethical challenges for physicians.
WORK HOURS
The Accreditation Council for Graduate Medical Education requires medical students and residents to observe work-hour limitations, which are intended to help prevent physician burnout, reduce mistakes, and create a better balance between work and private life. In addition to continuing controversy over their effectiveness, some ethical concerns are raised by work-hour limitations. One concern is that physicians may develop a shift-worker mentality that undermines their dedication to the well-being of patients. Forced handoffs to colleagues may actually increase the risk of errors, and inflexibility can be detrimental. In some cases, trainees could provide an irreplaceable benefit to a patient or family by going beyond work-hour limits, especially if there is rapport with the patient or family that is not easily transferred to another provider. For example, a resident may want to discuss decisions about life-sustaining interventions or to comfort a family member over a patient’s death (Chap. 10). Thus strict adherence to work-hour limits is not always consistent with the ideal of acting for the good of the patient and with compassion. Exceptions to work-hour limits, however, should remain exceptions and should not be allowed to undercut work-hour policies.
TEAM-BASED CARE
Physicians’ roles are changing as care is increasingly provided by multidisciplinary teams. The traditional hierarchy in which the physician is the “captain of the ship” may be inappropriate, particularly in areas such as prevention, disease management and its coordination, and patient education. Physicians should respect team members and acknowledge the expertise of those from other disciplinary backgrounds. Team-based care promises to provide more comprehensive and higher-quality care. However, regular communication and planning are critical to avoid diffusion of responsibility and to ensure that someone is accountable for the completion of patient-care tasks.
CLINICAL PRACTICE GUIDELINES
The increasing use of evidence-based practice guidelines and benchmarking of performance raises the overall quality of care. However, practice guideline recommendations may be inappropriate for an individual patient, while another option may provide substantially greater benefits. In such situations, physicians’ duty to act in the patient’s best interests should take priority over benefits to society as a whole. Physicians need to understand practice guidelines, to recognize situations in which exceptions might be reasonable, and to be prepared to justify an exception.
GLOBAL HEALTH FIELD EXPERIENCES
![]() With the growing importance of and interest in global health, many physicians and trainees work overseas for various periods. Typically, physicians gain valuable experience while providing service to patients in need. Such arrangements, however, can raise ethical challenges—for example, because of differences in beliefs about health and illness, expectations regarding health care and the physician’s role, standards of clinical practice, and norms for disclosure of serious diagnoses. Additional dilemmas arise if visiting physicians take on responsibilities beyond their level of training or if donated drugs and equipment are not appropriate to local needs. Visiting physicians and trainees should exercise due diligence in obtaining needed information about the cultural and clinical practices in the host community, should work closely with local professionals and team members, and should be explicit about their skills, knowledge, and limits. In addition, these arrangements can pose risks. The visiting physician may face personal risk from infectious disease or motor vehicle accident. The host institution incurs administrative and supervisory costs. Advance preparation for these possibilities minimizes harm, distress, and misunderstanding.
With the growing importance of and interest in global health, many physicians and trainees work overseas for various periods. Typically, physicians gain valuable experience while providing service to patients in need. Such arrangements, however, can raise ethical challenges—for example, because of differences in beliefs about health and illness, expectations regarding health care and the physician’s role, standards of clinical practice, and norms for disclosure of serious diagnoses. Additional dilemmas arise if visiting physicians take on responsibilities beyond their level of training or if donated drugs and equipment are not appropriate to local needs. Visiting physicians and trainees should exercise due diligence in obtaining needed information about the cultural and clinical practices in the host community, should work closely with local professionals and team members, and should be explicit about their skills, knowledge, and limits. In addition, these arrangements can pose risks. The visiting physician may face personal risk from infectious disease or motor vehicle accident. The host institution incurs administrative and supervisory costs. Advance preparation for these possibilities minimizes harm, distress, and misunderstanding.
PHYSICIANS’ USE OF SOCIAL MEDIA
Increasingly, physicians use social and electronic media to share information with patients and other providers. Social networking may be especially useful in reaching young or otherwise hard-to-access patients. However, the use of social media, including blogs, social networks, and websites, raises ethical challenges and can have harmful consequences if not approached prudently. Injudicious use of social media can pose risks to patient confidentiality, expose patients to intimate details of physicians’ personal lives, cross professional boundaries, and jeopardize therapeutic relationships. Posts may be considered unprofessional and lead to adverse consequences for a provider’s reputation, safety, or even employment, especially if they express frustration or anger over work incidents, disparage patients or colleagues, use offensive or discriminatory language, reveal highly personal information, or picture a physician intoxicated, using illegal drugs, or in sexually suggestive poses. Physicians should remember that, in the absence of highly restrictive privacy settings, postings on the Internet in general and on social networking sites in particular are usually permanent and may be accessible to the public, their employers, and their patients. Physicians should separate professional from personal websites, social networking accounts, and blogs and should follow guidelines developed by institutions and professional societies on using social media to communicate with patients.
CONFLICTS OF INTEREST
Acting in patients’ best interests may conflict with the physician’s self-interest or the interests of third parties such as insurers or hospitals. From an ethical viewpoint, patients’ interests should be paramount. Even the appearance of a conflict of interest may undermine trust in the profession.
FINANCIAL INCENTIVES
Health care providers may be offered financial incentives to improve the quality or efficiency of care. Such pay-for-performance incentives, however, could lead physicians to avoid sicker patients with more complicated cases or to focus on benchmarked outcomes even when such a focus is not in the best interests of an individual patient. In contrast, fee-for-service payments offer physicians incentives to order more interventions than may be necessary or to refer patients to laboratory or imaging facilities in which they have a financial stake. Regardless of financial incentives, physicians should recommend available care that is in the patient’s best interests—no more and no less.
RELATIONSHIPS WITH PHARMACEUTICAL COMPANIES
Financial relationships between physicians and industry are increasingly scrutinized. Gifts from drug and device companies may create an inappropriate risk of undue influence, induce subconscious feelings of reciprocity, impair public trust, and increase the cost of health care. Many academic medical centers have banned drug-company gifts of pens, notepads, and meals to physicians. Under the new Physician Payment Sunshine Act, companies must disclose publicly the names of physicians to whom they have made payments or transferred material goods and the amount of those payments or transfers. The challenge will be to distinguish payments for scientific consulting and research contracts—which are consistent with professional and academic missions and should be encouraged—from those for promotional speaking and consulting whose goal is to increase sales of company products.
OCCUPATIONAL RISKS
Some health care workers, fearing fatal occupational infections, have refused to care for certain patients, such as those with HIV infection or severe acute respiratory syndrome (SARS). Such fears about personal safety need to be acknowledged. Health care institutions should reduce occupational risk by providing proper training, protective equipment, and supervision. To fulfill their mission of helping patients, physicians should provide appropriate care within their clinical expertise, despite some personal risk.
RESPONSE TO MEDICAL ERRORS
Errors are inevitable in clinical medicine, and some errors cause serious adverse events that harm patients. Most errors are caused by lapses of attention or flaws in the system of delivering health care; only a few result from blameworthy individual behavior (Chaps. 3 and 12e). Physicians and students may fear that disclosing errors will damage their careers. However, patients appreciate being told when an error occurs, receiving an apology, and being informed about efforts to prevent similar errors in the future. Physicians and health care institutions show respect for patients by disclosing errors, offering appropriate compensation for harm done, and using errors as opportunities to improve the quality of care. Overall, patient safety is more likely to be improved through a quality improvement approach to errors rather than a punitive one except in cases of gross incompetence, physician impairment, boundary violations, or repeated violations of standard procedures.
LEARNING CLINICAL SKILLS
Physicians’ interest in learning, which fosters the long-term goal of benefiting future patients, may conflict with the short-term goal of providing optimal care to current patients. When trainees learn to carry out procedures on patients, they lack the proficiency of experienced physicians, and patients may experience inconvenience, discomfort, longer procedures, or even increased risk. Although patients’ consent for trainee participation in their care is always important, it is particularly important for intimate examinations, such as pelvic, rectal, breast, and testicular examinations, and for invasive procedures. To ensure patients’ cooperation, some care providers introduce students as physicians or do not tell patients that trainees will be performing procedures. Such misrepresentation undermines trust, may lead to more elaborate deception, and makes it difficult for patients to make informed choices about their care. Patients should be told who is providing care and how trainees are supervised. Most patients, when informed, allow trainees to play an active role in their care.
PHYSICIAN IMPAIRMENT
Physicians may hesitate to intervene when colleagues impaired by alcohol abuse, drug abuse, or psychiatric or medical illness place patients at risk. However, society relies on physicians to regulate themselves. If colleagues of an impaired physician do not take steps to protect patients, no one else may be in a position to do so.
ETHICAL ISSUES IN CLINICAL RESEARCH
Clinical research is essential to translate scientific discoveries into beneficial tests and therapies for patients. However, clinical research raises ethical concerns because participants face inconvenience and risks in research that is designed not specifically to benefit them but rather to advance scientific knowledge. Ethical guidelines for researchers require them to obtain informed and voluntary consent from participants and approval from an institutional review board, which determines that risks to participants are acceptable and have been minimized and recommends appropriate additional protections when research includes vulnerable participants. Physicians may be involved as clinical research investigators or may be in a position to refer or recommend clinical trial participation to their patients. Physicians should be critical consumers of clinical research results and keep up with advances that change standards of practice. Courses and guidance on the ethics of clinical research are widely available.