Chapter 14 The sacroiliac joint
This effect can be modelled by holding a pretzel in two hands and twisting it around its long axis in alternating directions. Eventually the pretzel will snap. The same occurs clinically. Insufficiency fractures of the sacrum occur in elderly individuals, particularly females, in whom the sacroiliac joint is relatively ankylosed and in whom the sacrum has been weakened by osteoporosis. Under these conditions the torsional stresses, normally buffered by the sacroiliac joint, are transferred to the sacrum, which fails by fracture. Conspicuously and strikingly, these fractures run vertically through the ala of the sacrum parallel to the sacroiliac joint.1–8
Structure
Bones
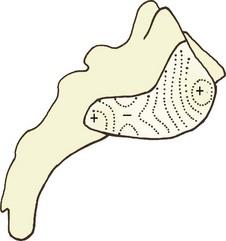
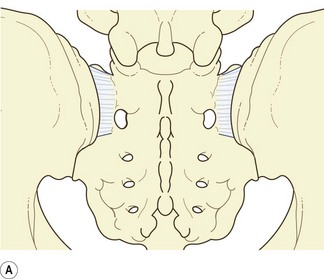
The first design imperative is to lock the sacrum into the pelvis. To this end, the articular surface of the sacrum presents an irregular contour, marked by ridges, prominences, troughs and depressions (Fig. 14.1). These are matched by reciprocal depressions, troughs, prominences and ridges on the ilium, so that the bones can lock into one another. This gives the sacroiliac joint a sinuous appearance in frontal view (Fig. 14.2).9
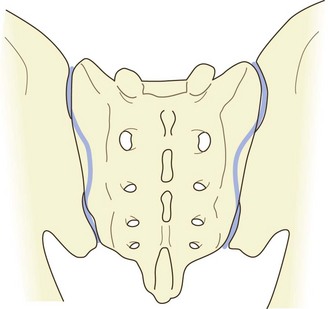
Figure 14.2 A posterior view of the sacroiliac joints showing the sinuous shape of the joint cavities.
Particularly evident is a major depression on the sacral surface, on the S2 segment, which receives a major prominence from the ilium, the latter being known as Bonnaire’s tubercle.10
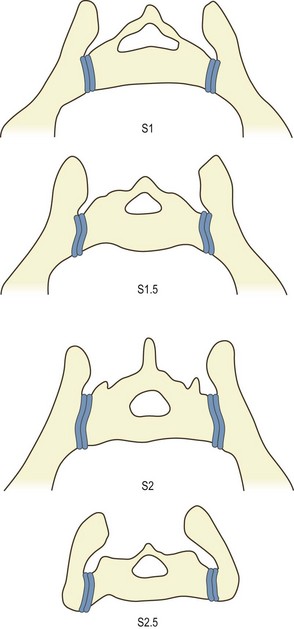
A further feature, noted in textbooks of anatomy11 but not verified by modern quantitative studies, pertains to the plane of the joint. The articular surface of the sacrum is twisted from above downwards. Opposite the S1 segment, the dorsal edge of the articular surface projects slightly further laterally than the ventral edge. Conversely, at the S3 segment, the ventral edge projects slightly more laterally than the dorsal edge. Because of this, when viewed in transverse section, the sacrum is wedge shaped but in opposite directions at opposite ends of the sacroiliac joint. At the S1 segment, the posterior width of the sacrum is greater than its anterior width. Conversely, at the S3 segment, the anterior width is greater than its posterior width (Fig. 14.3).
Cartilage
The cartilages differ on the sacrum and ilium. The sacral articular cartilage is normally white and smooth, and has the features of typical hyaline cartilage.12 Its thickness ranges from 1 to 3 mm.13 The iliac cartilage is duller in appearance and is marked by dense bundles of collagen, which give it the appearance of fibrocartilage,12 but histologically and biochemically it is nonetheless hyaline in nature.14 It is usually less than 1 mm thick. Its cell density, however, is greater than that of the sacral cartilage.15 Meanwhile, the subchondral plate of the ilium is some 50% thicker than that of the sacrum.15
The reasons for these differences between the sacral and iliac cartilages has not been established. One contention, however, is that the sacral cartilage is designed for transmitting forces (from the spine to the pelvis) whereas the iliac cartilage is designed to absorb them.15
Articulation
When articulated between the two ilia, the sacrum is held firmly in place by bony locking mechanisms. The interlocking contours of the sacrum and ilium prevent downward gliding of the sacrum under body weight. Indeed, the friction coefficient of the sacroiliac joint is larger than that of the knee and is considerably greater in proportion to the prominence of the ridges and depressions of the articular surface.16
Ligaments
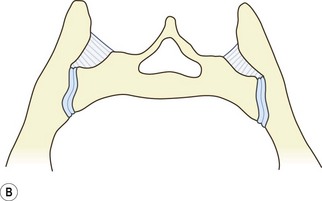
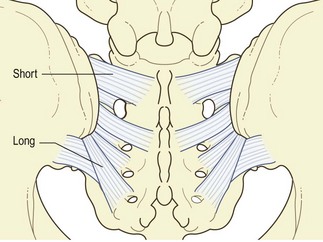
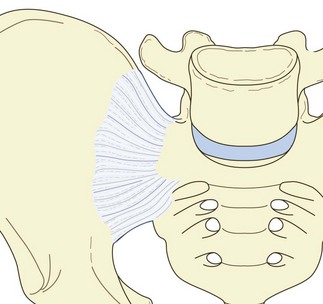
The most important ligament of the sacroiliac joint is the interosseous sacroiliac ligament. This ligament is a dense, thick collection of short collagen fibres that connect the ligamentous surface of the sacrum with that of ilium. It lies deep in the narrow recess between the sacrum and ilium dorsal to the cavity of the joint. The full thickness of the ligament is most clearly evident in transverse sections of the sacrum and ilium (Fig. 14.4). Gray’s Anatomy11 recognises deep and superficial parts of this ligament, each divided into superior and inferior bands. The superior superficial band connects the superior articular processes and lateral crest of the first two sacral segments to the neighbouring ilium, and is highlighted as the short posterior sacroiliac ligament.
Behind the interosseous ligament lies the posterior sacroiliac ligament proper. This consists of several fascicles of different lengths which connect the intermediate and lateral crests of the sacrum to the posterior superior iliac spine and the posterior end of the inner lip of the iliac crest. Those fibres from the third and fourth sacral segments are longer than the others and constitute the long posterior sacroiliac ligament (Fig. 14.5).11
The short posterior sacroiliac ligament is disposed to act in concert with the interosseous ligament to bind the ilium to the sacrum. Moreover, its posterior location allows it to prevent posterior flaring or diastasis of the joint. The long posterior sacroiliac ligament has a more longitudinal orientation and prevents backward rocking (counternutation) of the sacrum with respect to the ilium.17
The fibres are attached to these bones for considerable distances beyond the margins of the joint (Figs. 14.4, 14.6). Like the interosseous ligament, this ligament binds the ilium to the sacrum but its anterior location enables it to prevent anterior diastasis of the joint.
The sacrospinous ligament takes a broad origin from the lateral edge of the sacrum below the sacroiliac joint. Its fibres converge on the ischial spine. The sacrotuberous ligament arises from the posterior superior iliac spine, where it blends with the long posterior sacroiliac ligaments; from the transverse tubercles of the lower sacral segments; and from the lateral margin of the sacrum, where it blends with the sacrospinous ligament. From this broad origin, the ligament narrows but broadens again to attach to the medial margin of the ischial tuberosity. The superficial fibres of the ligament are continuous with the tendon of the biceps femoris.11
Capsule
There is scant mention in the literature of the structure of the capsule of the sacroiliac joint. This is because the joint is so intimately surrounded by thick ligaments. Under these circumstances, it is difficult, if not impossible, to discern where a ligament ends and a capsule begins. For this reason, authors report that the posterior capsule is rudimentary or absent18 and that the anterior sacroiliac ligament is a thickening of the anterior capsule.11
Innervation
In 1936, Pitkin and Pheasant19 lamented the lack of any description of the innervation of the sacroiliac joint in textbooks of anatomy. Indeed, this situation has still not changed.11 Instead, Pitkin and Pheasant relied on the 19th-century German literature to assert that the joint was innervated anteriorly by direct branches of the lumbosacral trunk, the superior gluteal nerve and the obturator nerve; posteriorly it was innervated by branches of the S1 and S2 dorsal rami.
Modern authors have endorsed this pattern, reporting a posterior innervation from the lateral branches of the posterior rami of L4 to S3, and an anterior innervation from the L2 to the S2 segments.18 However, the literature that they cite to this effect does not consist of authoritative anatomical studies. Others, referring to the same literature, describe a posterior innervation from L3 to S3 but emphasise that the principal segments are L5 to S2 but without citing any literature to this effect.20
Formal, modern anatomical studies provide conflicting conclusions. A German study21 stipulated a posterior innervation exclusively from the S1 and S2 dorsal rami but expressly denied an anterior innervation from either the sacral plexus or the obturator nerve. A Japanese study, however, reported a posterior innervation from the L5 and sacral dorsal rami and an anterior innervation from the L5 ventral ramus and S2 ventral ramus.22
Age changes
The future sacroiliac joint becomes apparent during the second month of fetal development, as a strip of mesenchyme between the cartilages of the future ilium and sacrum.23 Cavitation of this mesenchyme proceeds progressively and achieves its full extent by the seventh month. A synovial membrane appears by 37 weeks.12
In embryos, the articular surfaces remain smooth and flat. The anterior capsule is thin and lax, but the interosseous ligament is well developed.12
During the first 10 years of life, the joint enlarges in size but its surfaces remain flat; the anterior capsule thickens.12 Corrugation of the joint surfaces starts to develop during the second decade, starting with a depression along the articular surface of the sacrum matched by a reciprocal ridge along the ilium.12
With increasing age, the prominence of the iliac ridge increases but the surfaces of the articular cartilages start to exhibit superficial fibrillation and erosion, particularly on the iliac side.12 At the joint margins, the capsule and synovium become thicker and more fibrous, and osteophytes start to appear. By the fifth and sixth decades these changes are more marked. The articular cartilage loses its thickness and becomes fibrillated and eroded. Debris and fibrous tissue connecting the bones fill the joint cavity.12 Sinuous corrugations along the joint are established by the sixth decade9 but it is not clear when these start to develop.
By the eighth decade, osteophytes are large and interdigitate. Intra-articular fibrous adhesions are plentiful. The thickness of the articular cartilage is reduced to less than 1 mm on the sacrum and less than 0.5 mm on the ilium.12
Biomechanics
Because of these problems, studies based on plain radiographs24 or single specimens25 are, in principle, unreliable and, at best, only indicative of what might be found using more reliable techniques or larger numbers of specimens. To ensure accurate landmark recognition, implanted devices are required. These establish unique landmarks. However, even then the implanted landmarks must be three-dimensional and multiple, lest rotations out of the plane of view exaggerate or reduce the apparent movement in the plane of view.
In this regard, studies using single wires or rods implanted into each of two moving bones26 are unreliable because they do not account for three-dimensional movement. Furthermore, thin rods are subject to deformation and displacement by overlying skin, fascia and muscles.27
The first study to use implanted spheres examined four patients moving from supine and prone positions to positions of standing, standing on one leg, and standing with maximum lumbar lordosis.28 In essence, the range of sacroiliac motion observed in these manoeuvres, whether around a transverse, longitudinal or anteroposterior axis, was less that 2°, and was less than 1° in most cases. A later study of 25 patients, using the same technology confirmed these results.29 Mean rotations were less than 2° and ranges were less than 4°. The same picture has been borne out in studies of intact pelvises in cadavers.30,31
A study using rigidly fixed external devices in 21 volunteers examined the range of motion of the sacroiliac joint during forward flexion of the trunk, during maximum extension of the trunk and standing on one leg.32 The mean ranges of motion reported were less than 1°, with standard deviations of not more than 0.9°. However, these results are somewhat illusory. They constitute the mean magnitude of the motion, irrespective of direction. During flexion of the trunk, the sacrum was just as likely to flex as to extend around its transverse axis.32 Consequently, in a sample of individuals, the true mean range of motion of the sacroiliac joint is 0°, with as many individuals exhibiting up to 1° of rotation of the sacrum backwards as forwards, for the same excursion of the trunk. Thus, although the sacroiliac joints move, their direction of movement is irregular.
Subsequent, more recent, studies have examined the movements of the sacroiliac joint in a variety of postures and movements, such as the reciprocal straddle position,33 and standing hip flexion.34 They show that the range of movement is essentially only about 1°. Furthermore, even after therapeutic manipulation, the joint shows no change in position or movement.35
However, the nature of sacroiliac movements makes perfect sense in terms of the joint being a stress-relieving joint. In this regard the studies of Lavignolle et al. although not definitive, are nonetheless indicative.36
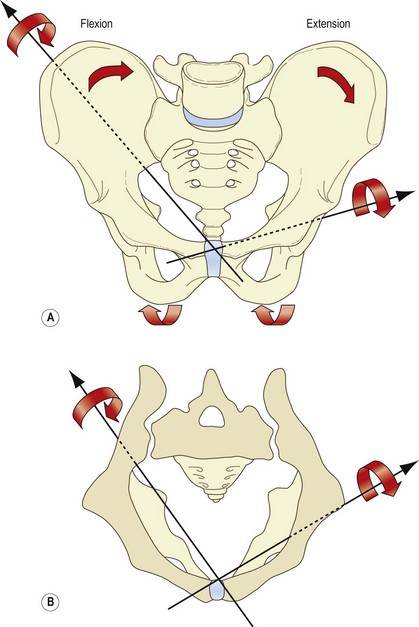
Instead of conventional axes passing transversely, longitudinally or sagittally through the joints, these investigators found that the axes of movement of the sacroiliac joints passed obliquely across the pelvis. For flexion, the axis passed backwards from the pubic symphysis to the greater sciatic notch. For extension, the axis passed from the pubic symphysis through the pelvis between the ischium and coccyx (Fig. 14.7). Given these axes, it is evident that during flexion and extension of the lower limbs, the sacrum undergoes complex movements. During flexion of the hip the ipsilateral ilium glides backwards and downwards across the sacrum and compresses against it, pivoting at the pubic symphysis. During extension, the ilium glides forwards and flares away from the sacrum.
1 Cooper KL, Beabout JW, Swee RG. Insufficiency fractures of the sacrum. Radiology. 1985;156:15-20.
2 Cotty P, Fouquet B, Mezenge C, et al. Insufficiency fractures of the sacrum. J Neuroradiol. 1989;16:160-171.
3 Davies AM, Evans NS, Struthers GR. Parasymphyseal and associated insufficiency fractures of the pelvis and sacrum. Br J Radiol. 1988;61:103-108.
4 De Smet AA, Neff JR. Pubic and sacral insufficiency fractures: clinical course and radiologic findings. Am J Roentgenol. 1985;145:601-606.
5 Lourie H. Spontaneous osteoporotic fracture of the sacrum: an unrecognized syndrome of the elderly. JAMA. 1982;248:715-716.
6 Peris P, Guanabens N, Pons F, et al. Clinical evolution of sacral stress fractures: influence of additional pelvic fractures. Ann Rheum Dis. 1993;52:545-547.
7 Ries T. Detection of osteoporotic fractures with radionuclides. Radiology. 1983;146:783-785.
8 Weber M, Hasler P, Gerber H. Insufficiency fractures of the sacrum. Twenty cases and review of the literature. Spine. 1993;18:2507-2512.
9 Vleeming A, Stoeckhart R, Volkers ACW, et al. Relation between form and function in the sacroiliac joint. Part I. Clinical anatomical aspects. Spine. 1990;15:130-132.
10 Wilder DG, Pope MH, Frymoyer JW. The functional topography of the sacroiliac joint. Spine. 1980;5:575-579.
11 Williams PL, editor. Gray’s Anatomy, 38th ed, Edinburgh: Churchill Livingstone, 1995.
12 Bowen V, Cassidy JD. Macroscopic and microscopic anatomy of the sacroiliac joint from embryonic life until the eighth decade. Spine. 1981;6:620-628.
13 Bellamy N, Park W, Rooney PJ. What do we know about the sacroiliac joint? Semin Arthritis Rheum. 1983;12:282-313.
14 Paquin JD, van der Rest M, Marie PJ, et al. Biochemical and morphologic studies of cartilage from the adult sacroiliac joint. Arthritis Rheum. 1983;26:887-895.
15 McLauchlan GJ, Gardner DL. Sacral and iliac articular cartilage thickness and cellularity: relationship to subchondral bone end-plate thickness and cancellous bone density. Rheumatology. 2002;41:375-380.
16 Vleeming A, Volkers ACW, Snijders CJ, et al. Relation between form and function in the sacroiliac joint. Part II. Biomechanical aspects. Spine. 1990;15:133-135.
17 Vleeming A, Pool-Goudzwaard AL, Hammudoghlu D, et al. The function of the long dorsal sacroiliac ligament: its implication for understanding low back pain. Spine. 1996;21:556-562.
18 Bernard TN, Cassidy JD. The sacroiliac joint syndrome. Pathophysiology, diagnosis, and management. In: Frymoyer JW, editor. The Adult Spine. Principles and practice. New York: Raven Press; 1991:2107-2130.
19 Pitkin HC, Pheasant HC. Sacrarthogenetic telalgia I. A study of referred pain. J Bone Joint Surg. 1936;18:111-133.
20 Cole AJ, Dreyfuss P, Pauza K. Sacroiliac joint injection techniques. In: Vleeming A, Mooney V, Snijders C, et al, editors. Second Interdisciplinary World Congress on Low Back Pain: the Integrated Function of the Lumbar Spine and Sacroiliac Joints. Rotterdam: European Conference Organizers; 1995:569-597.
21 Grob KR, Neuhuber WL, Kissling RO. Innervation of the human sacroiliac joint. Z Rheumatol. 1995;54:117-122.
22 Ikeda R. Innervation of the sacroiliac joint: macroscopical and histological studies. Nippon Ika Daigaku Zasshi. 1991;58:587-596.
23 Schunke GB. The anatomy and development of the sacro-iliac joint in man. Anat Rec. 1938;72:313-331.
24 Weisl H. The movements of the sacroiliac joints. Acta Anat. 1955:80-91.
25 Frigerio NA, Stowe RR, Howe JW. Movement of the sacro-iliac joint. Clin Orthop. 1974;100:370-377.
26 Colachis SC, Worden RE, Bechtol CO, et al. Movement of the sacroiliac joint in the adult male. Arch Phys Med Rehab. 1963;44:490-498.
27 Vleeming A, Stoeckhart R, Snijders CJ. General introduction. In: Vleeming A, Mooney V, Snijders C, et al, editors. First Interdisciplinary World Congress on Low Back Pain and its Relation to the Sacroiliac Joint. Rotterdam: European Conference Organizers; 1992:3-64.
28 Egund N, Olsson TH, Schmid H, et al. Movements in the sacroiliac joints demonstrated with roentgen stereophotogrammetry. Acta Radiol. 1978;19:833-846.
29 Sturesson B, Selvik G, Uden A. Movements of the sacroiliac joints: a roentgen stereophotogrammetric analysis. Spine. 1989;14:162-165.
30 Miller JAA, Schultz AB, Andersson GB. Load–displacement behaviour of sacroiliac joints. J Orthop Res. 1987;5:92-101.
31 Vleeming A, van Wingerden JP, Dijkstra PF, et al. Mobility in the sacroiliac joints in the elderly: a kinematic and radiologic study. Clin Biomech. 1992;7:170-176.
32 Jacob HAC, Kissling RO. The mobility of the sacroiliac joints in healthy volunteers between 20 and 50 years of age. Clin Biomech. 1995;10:352-361.
33 Sturesson B, Uden A, Vleeming A. A radiostereometric, analysis of the movements of the sacroiliac joints in the reciprocal straddle position. Spine. 2000;25:214-217.
34 Sturesson B, Uden A, Vlemming A. A radiostereometric analysis of movements of the sacroiliac joints during the standing hip flexion test. Spine. 2000;25:364-366.
35 Tulberg T, Blomberg S, Branth B, et al. Manipulation does not alter the position of the sacroiliac joint. A Roentgen stereophotogrammetric analysis. Spine. 1998;23:1124-1129.
36 Lavignolle B, Vital JM, Senegas J, et al. An approach to the functional anatomy of the sacroiliac joints in vivo. Anat Clin. 1983;5:169-176.