Chapter 14. The sacroiliac joint
CHAPTER CONTENTS
Summary411
Commentary on the examination 417
Observation 417
History (subjective examination) 417
Inspection 419
State at rest 420
Examination by selective tension (objective examination) 420
Pain provocation tests 423
Pain provocation test for the anterior ligaments 425
Palpation 426
Dynamic asymmetry palpation tests to determine treatment technique 426
Mechanical lesions of the sacroiliac joint 427
Contraindications to sacroiliac joint manipulation 427
Sacroiliac manipulation procedure 427
Sacroiliac hypermobility 431
Traction 431
Sclerosant injections 432
SUMMARY
Sacroiliac dysfunction describes a broad set of signs and symptoms associated with the sacroiliac joint and its surrounding structures (Dreyfuss et al 1996, Levangie 1999). Pain due to hypomobility, hypermobility, malalignment, fixation, joint subluxation and ligament strain can lead to structural changes in the joint and soft tissues (Freburger & Riddle 2001). Lesions tend to be long-standing and are difficult to diagnose, often mimicking pain of lumbar or hip origin. This chapter begins with a presentation of the anatomy of the joint and links it with possible pathology and methods of differential diagnosis of its mechanical and non-mechanical lesions.
In general terms, treatment consists of mobilization, manipulation and/or exercise of hypomobile or subluxed joints, and stabilization through supportive belts, exercise and occasionally sclerosant injection for hypermobile joints. Intra-articular injections have also been discussed (Schmid 1984, Calvillo et al 2000). Contraindications to treatment are few and emphasis is placed on assessment strategies on which to base treatment selection and appropriate exercise programmes. The evidence to support current assessment methods is reviewed.
ANATOMY
The pelvis is a unique osteoarticular ring consisting of the two innominate bones, which articulate anteriorly at the symphysis pubis, and posteriorly at the sacrum, which is suspended between the innominate bones by its ligaments. Since form follows function, small structural differences occur between the sexes, with women exhibiting greater mobility of the sacroiliac joints (Harrison et al 1997). The function of the bony pelvis is to support and transmit body weight from the trunk to the lower limbs and, vice versa, to dampen the distribution of ground reaction forces occurring during gait activities. It protects and provides support for the viscera and also provides attachment for ligaments and leverage for muscles.
The sacrum is a large triangular mass of bone formed by the fusion of the five sacral vertebrae (Fig. 14.1). The sacral base lies superiorly and is angulated upwards and forwards, articulating with the fifth lumbar vertebra to form the lumbosacral angle. Its anterior border is the sacral promontory. The apex of the sacrum lies inferiorly and articulates with the coccyx, a small triangular bone formed by the fusion of approximately four small vertebrae.
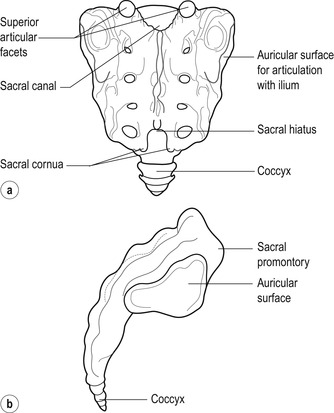 |
| Figure 14.1
(a,b) Sacrum, showing bony landmarks.
|
The pelvic surface of the sacrum is relatively smooth while its dorsal surface is roughened and displays three distinct crests: a median crest represents the fused spinous processes, an intermediate crest the fused articular processes and a lateral crest the fused transverse processes of the sacral vertebrae. The lateral crest provides attachment for the posterior sacroiliac ligaments.
The laminae and spinous processes of the fourth and fifth sacral vertebrae are absent, forming an opening known as the sacral hiatus. Anatomical anomalies are common here and elements of the other vertebrae may be missing, making this a variably sized opening (Trotter 1947). The sacral cornua are the remnants of the articular processes of the fourth or fifth sacral vertebra projecting downwards on either side of the sacral hiatus. They provide palpable bony landmarks for the sacral hiatus which is clinically relevant in the placement of a caudal epidural injection. To palpate the sacral cornua, place the thumb and middle finger of one hand on the posterior superior iliac spines (PSIS) and use the index finger to make an equilateral triangle. The position of the index finger now gives the approximate position of the sacral cornua and hence the sacral hiatus.
The sacral canal is triangular in shape and formed by the fused sacral vertebral foramina. The dural sac usually terminates at the level of the lower border of the second sacral vertebra where it contracts into a filament and continues through the sacral canal to the coccyx, to become continuous with the periosteum (Trotter 1947). Four pairs of sacral foramina provide an exit for the sacral spinal nerves. The lateral surface of the sacrum is expanded superiorly and provides an articulating surface for the sacroiliac joint. This surface bears an auricular (ear-like) surface anteriorly, which is shaped more like an ‘L’ than an ear, and a pitted irregular surface posteriorly, for the attachment of the posterior and interosseous sacroiliac ligaments.
The hip or innominate bone is made up of the ilium above, the pubis in front and the ischium behind. The acetabulum is the cup-shaped hollow on its outer surface at the junction of the three component bones.
The ilium possesses several palpable bony landmarks. Those relevant here are:
• The iliac crest which gives an approximate indication of the level of the spinous process of L4
• The anterior superior iliac spine (ASIS) which lies at the anterior end of the iliac crest
• The anterior inferior iliac spine (AIIS) which lies below the superior spine and is not so readily palpable
• The posterior superior iliac spine (PSIS), indicated by a dimple (dimple of Venus) approximately 4 cm lateral to the spinous process of S2
• The posterior inferior iliac spine (PIIS) lying below the superior spine and difficult to palpate.
The iliac fossa lies medially, its posterior aspect thickened, roughened and marked by the iliac tubercle for the attachment of the posterior and interosseous sacroiliac ligaments. In front of the roughened area lies an auricular-shaped articular surface corresponding to the articular surface of the sacrum. Laterally the blade of the ilium provides attachment for the gluteal muscles.
The sacroiliac joint
The sacroiliac joint is essentially a synovial joint with its surfaces covered by articular cartilage. It is lined with synovial membrane and surrounded by a fibrous capsule, reinforced by ligaments. The anterior third of the articulation between the sacrum and the ilium is considered to be a true synovial joint, with the remaining articulation supported by ligamentous attachments that convert the joint into a part syndesmosis (Harrison et al 1997). Due to its deep location, its position in the osteoarticular ring and the variability in anatomy between sides and individuals, the sacroiliac joint is a difficult joint to study (Zheng et al 1997).
The auricular-shaped articular facets on the ilium and the sacrum have reciprocally irregular joint surfaces which provide the joint with great stability. In basic terms, a bump or ridge on one surface will articulate with a pit or depression on the other. The joint surfaces are relatively planar in the young, but following puberty irregularities develop, more so in the male sacroiliac joint, making it inherently more stable. Two types of joint surface irregularities were described by Vleeming et al (1990a, 1990b) in a study of prepared human sacroiliac joints. Ridges on one joint surface had complementary depressions on the other, and areas of coarse and smooth texture existed. The irregularities in the joint surfaces appear to represent adaptations to stability promoted by increased body weight during the adolescent growth spurt. These irregularities also provide the joint surfaces with high coefficients of friction, further contributing to the joint’s renowned stability. The irregularities continue to progress with age and fusion of the joint is said to develop in the elderly. However, Vleeming et al (1990a) suggest caution when interpreting X-rays of the sacroiliac joints since the ridges and depressions can be misinterpreted as osteophytes.
The way in which the joint surfaces interdigitate allows weight-bearing but restricts movement, contributing to the stability of the joint. Major subluxation of the joint is not commonly seen clinically, but the interdigitating articular surfaces make minor subluxation a possibility. Vleeming et al (1990b) surmise from friction experiments that, under abnormal loading conditions, it is possible to force sacroiliac joint surfaces into a new position in which the ridges and depressions are no longer complementary, suggesting a blocked joint or minor subluxation.
The suspension of the wedge-shaped sacrum between the two ilia provides it with a self-locking mechanism. This self-locking mechanism involves both form and force closure (Lee 2000). Form closure indicates stability due to the closely fitting joint surfaces, the friction coefficient of the roughened articular cartilage and the integrity of the strong sacroiliac ligaments, so that little or no external forces are required to maintain static stability. Force closure indicates the dynamic stability of the joint in which extra forces are needed to maintain stability. Movements occurring in the sacroiliac joint are small, but, as the sacrum moves, activity in the surrounding muscle groups together with increased ligamentous tension enhances the compression forces on the joint, through tensioning of the pelvic ligaments and thoracolumbar fascia, to facilitate the force closure mechanism, making load transfer more efficient (Lee 2000, Hungerford et al 2007). Increasing weight applied to the sacral base, such as the effects of gravity or the compression forces of the trunk, will also enhance the force closure mechanism, holding the sacrum more tightly in situ through tension in its ligaments (Fig. 14.2) (Kapandji 1974). This arrangement is thought to be similar to the keystone of an arch in which stability is created where the greater the force applied, the greater the resistance offered (Harrison et al 1997).
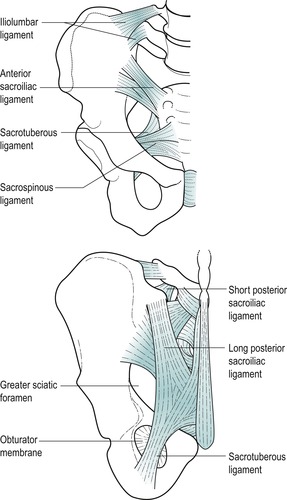 |
| Figure 14.2
The sacroiliac joint and ligaments.
From Anatomy and Human Movement by N Palastanga, D Field and R Soames. Reprinted by permission of Elsevier Ltd.
|
The fibrous capsule is reinforced by strong posterior ligaments and weaker anterior ligaments, while a set of accessory ligaments contributes a stabilizing effect on the joint. These strong ligaments prevent translation of the sacrum and separation of the joint and function as a connecting band between the sacrum and the ilium (Cohen 2005). The interosseous sacroiliac ligament forms the main union between the sacrum and ilium, filling the gap between the lateral sacral crest and the iliac tuberosity (Lee 2000). It strongly resists separation and translation forces and is a physical barrier to palpation of the sacroiliac joint which makes intra-articular injection difficult (Harrison et al 1997, Lee 2000).
The posterior sacroiliac ligament covers the interosseous ligament and has long and short fibres. Short horizontal fibres are placed superiorly where they resist forward movement of the sacral promontory. Longer vertical fibres, continuous with the sacrotuberous ligament, are more superficial and resist a downwards movement of the sacrum relative to the ilium. The long posterior fibres are said to be tense under counternutation, an upwards, backward, nodding movement of the sacrum (Vleeming et al 1996) (see below).
The anterior sacroiliac ligament forms a weak thickening of the anterior joint capsule.
Accessory ligaments exert a stabilizing effect on the joint:
The sacrotuberous ligament attaches by a broad base from the PSIS, the side of the sacrum and the coccyx, partially blending with the posterior ligaments. Its fibres converge to pass downwards and laterally, twisting and broadening again at its attachment to the ischial tuberosity where it blends with the tendon of biceps femoris and the lower fibres of gluteus maximus.
The sacrospinous ligament is thinner and triangular, lying anterior to the sacrotuberous ligament. It passes from the lower part of the sacrum and coccyx to the spine of the ischium and its pelvic surface blends with the coccygeus muscle.
The sacrotuberous and sacrospinous ligaments lie below and lateral to the joint, preventing the tendency for the apex of the sacrum to tilt upwards as body weight is directed down onto the base of the sacrum. The iliolumbar ligaments anchor the transverse processes of the fifth lumbar vertebra to the ilium (an attachment to the fourth lumbar vertebra may also be present), stabilizing the lumbosacral junction against the tendency for the sacral promontory to move forwards under the influence of gravity and body weight.
A network of muscles also supports the sacroiliac joint. Some of these muscles, including gluteus maximus, piriformis and biceps femoris, are functionally connected to the sacroiliac joint ligaments and their actions can affect joint mobility (Cohen 2005). This relationship is important when devising rehabilitation programmes to improve functional stability of the joint.
The sacrococcygeal joint
This is a symphysis between S5 and the first coccygeal segment, but the joint is often obliterated in old age. Flexion and extension movements occur which are largely passive (Lee 2000, Palastanga et al 2006).
The symphysis pubis
The symphysis pubis is the joint between the medial surfaces of the two innominate bones. An interpubic fibrocartilaginous disc is situated within the joint and the surrounding joint capsule is supported by ligamentous thickenings. A superior pubic ligament is a thick fibrous band joining the pubic crests and tubercles, while an arcuate pubic ligament arches between the inferior pubic rami, blending with the intra-articular disc, to support the joint inferiorly (Palastanga et al 2006).
Movement of the sacroiliac joint
Many strong muscles pass over the sacroiliac joint, but none directly affects it. However, the ligaments of the sacroiliac joint and lumbar spine fuse with the thoracolumbar fascia and as such provide attachments for the main trunk-stabilizing muscles. Activity in these stabilizing muscles provides a ‘self-bracing’ mechanism which in turn contributes to stability at the sacroiliac joints (Harrison et al 1997).
There seems to be a general agreement that some passive movement does occur at the sacroiliac joint, but how much and in which direction is still not certain. Movement descriptions applied to the sacroiliac joint include subluxation, upslip, downslip, outflare, inflare, anterior or posterior rotation or torsion, all of which describe movement of the ilium on the sacrum (Swezey 1998, Cibulka 2002, Oliver & Middleditch 2006, Standring 2009). Kapandji (1974) refers to the movements as nutation and counternutation (Latin, nutare=to nod) where movement of the sacrum on the ilium is described.
Cibulka (2002) questions the notion that all of these movements occur at the sacroiliac joint, arguing that, in common with other synovial joints, the movement patterns at the sacroiliac joint are determined by the shape and orientation of the articular surfaces. Therefore, although structurally separate, they act together functionally as one bicondylar joint, and have two degrees of freedom.
The primary movement is considered to be an anterior or posterior sagittal tilt otherwise called torsion, rotation or nutation in the descriptions above. However, minor frontal and transverse movements of the joints also occur, dependent upon the individual’s joint alignment, which possibly explains the observation of inflares and outflares. The secondary movement is an antagonistic innominate motion where movement on one side is accompanied by a correlative movement on the other, making the two sacroiliac joints interdependent on each other, and never independent.
During symmetrical activities such as sitting or standing, movement normally occurs simultaneously in the two sacroiliac joints with either an anterior or posterior innominate tilt or rotation that brings the two anterior and posterior superior iliac spines to lie in roughly the same horizontal plane. During asymmetrical activities such as walking or running, just as one hip flexes and the other extends, one innominate bone tilts posteriorly while the other tilts anteriorly. Cibulka (2002) suggests that the relationship between the right and left innominate bones should be observed, as patients with sacroiliac dysfunction demonstrate an antagonistic asymmetrical position even in symmetrical postures such as sitting and standing. This notion that movement of one innominate bone occurs with correlative movement of the opposite innominate can be applied to manipulative techniques which can be reversed and performed on the opposite side. Zheng et al (1997) produced an experimental biomechanical model of the pelvis to study the sacroiliac joint that emphasized this interdependence of the three joints of the pelvic ring, the two sacroiliac joints and the symphysis pubis.
In a study of healthy individuals between the ages of 20 and 50 years, the average total rotational movement in the sacroiliac joint between erect standing and standing on one leg was 2° (Jacob & Kissling 1995, Kissling & Jacob 1996). One subject, excluded from this analysis because of occasional symptoms, was found to have more than 6° of movement.
Functionally, movements at the sacroiliac joint occur in combination with the adjacent joints. Variations between the two joints and between individuals are common, making objective examination of these joints difficult.
Although the sacroiliac joints are relatively immobile and stable, they are susceptible to mechanical trauma. Compared with the lumbar spine, the sacroiliac joints can withstand a medially directed force six times greater but only half the torsion and one-twentieth of the axial compression load (Cohen 2005). Joint sprain and minor subluxations occur and, symptomatically, patients respond well to manipulation. In the discussion that follows below, the subjective judgments made on sacroiliac static or dynamic alignment are not reliable indicators of dysfunction; therefore correction of alignment is not necessarily indicative of cure. As synovial joints they are subject to the various forms of arthritis and the degenerative changes associated with the ageing process. Reduced mobility seems to occur through a process of fibrous bands or fibrocartilaginous adhesion formation rather than bony ankylosis (Cassidy 1992, Palastanga et al 2006).
Mechanical lesions are less common in the older age group as movements reduce. The ligaments of the female pelvis relax during pregnancy, increasing the range of movement and making the sacroiliac joint locking mechanism less effective. During this time the relative hypermobility of the sacroiliac joints makes them susceptible to strain and subluxation.
Nerve supply
The nerve supply is variable and differs between individuals and often between the two sacroiliac joints in the same person; a variety of explanations for this is offered by the various texts. Fortin et al (1999a) conducted an anatomical study on cadavers determining that the joint itself is predominantly innervated by sacral dorsal rami (S1–S3). This observation was supported by pain diagrams reported by asymptomatic volunteers upon direct capsular stimulation, and with reduced pain in symptomatic subjects treated by intra-articular injection of an anaesthetic. As well as revealing pain-sensitive nerve endings within the joint, observations revealed the presence of mechanoreceptors which, in addition to signalling pain, could inform the central nervous system of abnormal loading, excessive movement and inflammation. In spite of Fortin et al’s findings, however, a consensus on the nerve supply is hard to establish.
Hansen et al (2007) acknowledge the continuing confusion and debate concerning innervation noting that some of the supply is directly from the sacral plexus and dorsal rami and some indirectly via the superior gluteal nerve and obturator nerve. In general terms, however, the sacroiliac joint and its surrounding ligaments receive a supply derived from L2–S3 nerve roots anteriorly and L5–S2 posteriorly (Oliver & Middleditch 2006). A ‘ballpark’ suggestion such as this would seem to be reasonable in light of current knowledge.
This extensive segmental supply and variation means that pain patterns can be confusing and may mimic other conditions. In a case report, Dangaria (1998) described a female patient presenting with low back pain, frequency and urgency of micturition whose symptoms were completely relieved by manipulation of the sacroiliac joint. The relief of all symptoms was attributed to the common nerve supply between the bladder and sacroiliac joint.
Differential diagnosis at the sacroiliac joint
Manipulative techniques are appropriate for mechanical lesions of the sacroiliac joint, i.e. minor subluxations and ligamentous strain. Assessment for displacement of the joint may be attempted through palpation tests but, in clinical practice, the small amount of movement at the sacroiliac joint makes this assessment difficult. Other means of applying compression, shear and distraction to the joints will be suggested, to incriminate the joint as a cause of pain. This section will discuss the differential diagnosis at the sacroiliac joint to distinguish mechanical lesions from other pathology.
Mechanical lesions of the sacroiliac joint
Diagnosis is clinical, taking into account the history, palpation for asymmetry in static and dynamic postures and the pain provocation tests. Diagnosed sacroiliac joint sprain, with or without subluxation, usually responds well to manipulation. Although the ideal treatment is yet to be validated, Calvillo et al (2000) suggest that treatment should be directed at restoring joint homeostasis. With this in mind, the indications, contraindications and treatment techniques will be described later in this chapter.
Other causes of sacroiliac pain and associated signs and symptoms
Arthritis can affect the sacroiliac joint since it is a mobile, weight-bearing, part synovial joint and may develop the same problems as other synovial joints. Normally, as described throughout this text, arthritis will manifest itself as the capsular pattern. However, at the sacroiliac joint, movements of accessory glide and translation mean that establishing the capsular pattern as such is difficult. The joint undergoes degenerative changes, reducing the mobility still further and making mechanical lesions less likely in the older age group.
The spondyloarthropathies such as ankylosing spondylitis, psoriatic arthritis and Reiter’s syndrome may manifest themselves initially as sacroiliitis in which the pain provocation tests described below will probably be positive, but the history will demonstrate an inflammatory rather than mechanical lesion.
• Ankylosing spondylitis is a chronic seronegative inflammatory arthritis affecting the axial skeleton in particular (Rai 1995, Kumar & Clark 2002). It affects men more commonly than women, although it may exist subclinically in women. It has an insidious onset in men under the age of 40, who complain of back and buttock pain, persisting for several months. The symptoms are typical of an inflammatory condition, with the pain and early-morning stiffness eased by movement and exercise. Sacroiliac joints are often the first target for the disease and sacroiliitis may be seen on X-ray. The later stages involve the whole spine, when the X-ray appearance is of a ‘bamboo’ spine. The disease is related to the presence of factor human leukocyte antigen (HLA)-B27 and blood tests will usually confirm clinical diagnosis. On examination there is loss of the lumbar lordosis, increased thoracic kyphosis and decreased chest expansion. Sacroiliitis gives severe pain when the sacroiliac joints are compressed.
• Reiter’s syndrome is a form of seronegative reactive arthritis that can follow gastrointestinal or genital tract infections (Keat 1995, Kumar & Clark 2002). The arthritis affects the lower limb joints, more readily the knees and ankles, but can also affect the sacroiliac joints. Non-specific urethritis and conjunctivitis may accompany the condition.
Serious non-mechanical conditions, including tumour, sepsis and fracture, can affect the sacroiliac joint and need to be excluded before manipulation is applied. Serious conditions of the pelvis may produce the ‘sign of the buttock’ (see Ch. 9). Pain associated with the sacroiliac joint in the elderly and in the young should be viewed with suspicion until proven otherwise, since mechanical lesions are rare in the sacroiliac joints in these age groups.
• Malignant disease can involve the sacroiliac joint directly or indirectly (Silberstein et al 1992). Metastases may be a cause of pain in the pelvis of older patients.
• Infection, as in osteomyelitis in the pelvis or upper femur, produces severe pain felt in the pelvic region and the patient is unwell with a high fever and marked tenderness over the affected bone.
• Septic arthritis, although uncommon in the sacroiliac joint, presents dramatically with pain, heat and swelling. The patient is unwell and febrile.
• Fracture of the sacrum or pelvic bones is suspected if the patient presents with a history of trauma, severe pain and much bruising.
Other musculoskeletal lesions can produce pain felt in the region of, or referred to, the sacroiliac joint. Differential diagnosis is difficult because the signs and symptoms overlap considerably. Muscle imbalances may need to be addressed, particularly weakness of gluteus medius, within the main hip abductors. Weakness of gluteus medius can cause a pelvic drop on the stance phase of gait, resulting in a compensatory hip hiking brought about by quadratus lumborum (Chen et al 2002).
• Lumbar disc lesions produce pain felt in one or both buttocks. Distinguishing features of the history may help exclude it as a cause of pain, but lesions commonly coexist. Disc lesions are aggravated by posture and movement, eased by rest, and often better in the early morning. Dural involvement produces pain on coughing, sneezing and straining; radicular involvement produces objective neurological signs and sensory neurological symptoms.
• Hip joint pathology refers pain to the L3 dermatome and may involve unilateral low back and upper buttock pain. Examination of the hip produces positive signs.
• Trochanteric bursitis may produce lateral hip and thigh pain.
• Myofascial pain due to trigger points in piriformis, gluteus maximus or quadratus lumborum may refer pain into the area of the sacroiliac joint (Chen et al 2002).
• Piriformis syndrome is caused by anatomical variations in either the muscle or the sciatic nerve and increased muscle tone or tightness can cause pain in the region of the sacroiliac joint or the sciatic notch. Sitting on a hard surface aggravates the pain that is eased by walking, and there is usually tenderness on palpation over the sciatic notch and the greater trochanter. Symptoms can be reproduced with resisted abduction with the hip in adduction and flexion. Pain may also be reproduced by resisted external rotation with the hip and knee flexed, beginning from a position of internal rotation so that end range is tested. The straight leg raise is negative (Brukner & Khan 2007, Tibor & Sekiya 2008).
• Coccydynia is pain in the region of the coccyx which can arise following direct trauma such as a fall directly onto the bottom. The lumbar spine can also refer pain to the area of the coccyx.
COMMENTARY ON THE EXAMINATION
Observation
A general observation is made, including the patient’s face, posture and gait. Serious conditions of the pelvis may produce severe pain, of which night pain is a feature, and this may be evident in the face of the patient, who looks tired and drawn from lack of sleep. The posture and gait may show abnormalities and these need careful assessment to ascertain if they are relevant to the patient’s presenting condition. Generally, a mechanical lesion of the sacroiliac joint rarely alters the gait pattern while sacroiliitis can be very painful, and the patient may not like to weight-bear on the affected side.
See the Box (p. 419) which lists ‘Red flags’ for the possible presence of serious pathology that should be listened for and identified throughout the subjective and objective examination. In isolation, many of the flags may have limited significance but it is for the clinician to consider the general profile of the patient and to decide whether contraindications to treatment exist and/or whether onward referral is indicated.
History (subjective examination)
A careful history is taken because the differential diagnosis of mechanical lesions, subluxation or strain of the sacroiliac joint is particularly reliant on features of the history.
The patient’s age is relevant as mechanical lesions of all joints in this region tend to present as a condition of middle age. Caution is required in the elderly and the young who seemingly present with a mechanical sacroiliac joint lesion, as this is uncommon. Younger patients may show postural asymmetry which may need correction to avoid later problems.
Occupation, sports, hobbies and lifestyle may all have relevance to a sacroiliac mechanical lesion. Any occupation or sport that involves increased weight-bearing through one leg may place abnormal stresses on the sacroiliac joint, e.g. driving, ballet, hurdling.
Mechanical lesions of the sacroiliac joint affect both sexes, but they are more common in women. The irregularities in the articular surfaces are more predominant in the male sacroiliac joint, giving it a greater inherent stability. During pregnancy, the ligaments of the pelvis soften to allow more movement and the joints are more susceptible to injury and subluxation. If subluxation occurs during this time and is not reduced, the abnormality remains once the ligaments tighten in the postpartum phase and the patient may encounter long-term problems.
The nature of the nerve supply to the sacroiliac joint and its surrounding ligaments makes the site and spread of the pain difficult to relate to specific diagnosis. The site and spread could be equally indicative of lumbar spine or hip pathology or mimic other conditions. Commonly a localized buttock pain is present, often centred around the PSIS. The spread of pain from the sacroiliac joint may be into the groin and front of the thigh, into the buttock and posterior thigh, and possibly into the calf.
Fortin, Dwyer, & West et al. (1994a) and Fortin, Aprill, & Ponthieux et al. (1994b) looked at patterns of pain referral using anaesthetic injections to map an area of hypaesthesia (a reduced sensibility to touch) in normal subjects and provocative injections followed by injection of anaesthetic in symptomatic subjects. All subjects felt hypaesthesia or pain locally over the sacroiliac joint, with variable referral to the lateral aspect of the buttock, to the greater trochanter and into the upper lateral thigh. This variation in pain response is consistent with the variable and extensive nerve root supply to the sacroiliac joint. Fortin et al felt it important to limit the pain mapping pattern to the area common to each subject and therefore most likely to represent sacroiliac joint symptoms. This was established as an area 3–10 cm just inferior to the PSIS. They concluded that the use of pain diagrams is a worthwhile preliminary diagnostic tool in conjunction with the history and complete physical examination.
Derby (1994) challenged Fortin et al’s results, suggesting that, although the first study mapped a consistent area of pain in asymptomatic volunteers, the second failed to report detailed pain relief information, or to control for a placebo response. Slipman et al (2000) attempted to develop the work of Fortin et al in a retrospective study and identified 18 potential areas of pain referral based on fluoroscopically guided diagnostic sacroiliac joint blocks on 50 consecutive patients. A total of 72% reported pain in the lower lumbar region, 94% in the buttock and 14% in the groin; 50% of the patients in this study reported symptoms in the lower limb, with younger patients more likely to describe pain below the knee. The authors give an honest appraisal of the limitations of their study and it is clear that more work is required to provide credible evidence.
Schwarzer et al (1995) found no conventional predictive features of sacroiliac joint pain except for a strong association with groin pain. Dreyfuss et al (1996) suggest that a distinguishing feature for sacroiliac joint pain syndrome may be the absence of pain felt above the L5 level, while Freburger & Riddle (2001), in reviewing the published evidence to guide examination of the sacroiliac joint, found some support for the following pain descriptions: absence of pain in the lumbar region, pain felt below L5 and pain in the region of the PSIS.
Fortin et al (1999b) expanded their studies on pain referral patterns by observing the pattern of contrast fluid movement during sacroiliac arthrography to determine whether any communication existed between the sacroiliac joint and adjacent neural structures. They established five principal patterns of extracapsular contrast fluid movement, three of which suggested a potential pathway of communication into the dorsal sacral foramina, into the fifth lumbar epiradicular sheath and into the lumbosacral plexus. They hypothesized that if the joint capsule is disrupted intra-articular contents such as inflammatory chemical mediators, in symptomatic patients, could leak and irritate adjacent neural structures which could produce lower limb symptoms similar to those seen in discogenic and facet joint pain.
Therefore, best practice currently relies on studies which provide the clinician with a model of possible pain referral that should not be taken in isolation but should encompass a full differential diagnosis.
The mode of onset and duration of the symptoms of sacroiliac mechanical lesions can be helpful. Sacroiliac pain syndrome or dysfunction may have a sudden onset, when it is usually associated with some form of trauma, e.g. a fall from a height, slipping down the stairs jarring the leg, or a motor vehicle accident where the foot was placed heavily on the brake. Unidirectional pelvic shear or torsional strain is common and the mechanism of injury may involve straightening up from the stooped position (Leblanc 1992, Hansen et al 2007). Sporting activities which exert repetitive lower intensity forces or a single strong force, such as running, jumping and squatting, may produce excessive movement or stress in the sacroiliac joint and surrounding tissues, leading to overload injuries and soft tissue failure (Chen et al 2002).
A gradual strain of the sacroiliac joint may occur through repeated minor trauma, which is often related to occupation, e.g. constant driving over rough ground or persistent pressure being exerted through one sacroiliac joint. It can also be of idiopathic origin (Hansen et al 2007).
If female, the patient should be questioned about any significant events during pregnancy that may have provoked symptoms. Gynaecological surgery and obstetric delivery often require the use of the lithotomy position, when the woman is positioned lying on her back with her hips and knees flexed to 90°. This tilts the pelvis posteriorly and may place undue stress on the sacroiliac joints.
The duration is also relevant. Patients have usually had their problem for a long time since it produces a dull ache, which may be tolerated more than the pain of acute onset, or severe sciatica, associated with lumbar pathology. The duration of symptoms also gives a prognostic indicator. Adaptive shortening occurs in chronic subluxation and the chance of correction using manipulative techniques after a long duration is slim. However, manipulation may help the pain even without correction of the deformity.
The symptoms and behaviour need to be considered. The behaviour of the pain indicates the nature of the condition and should distinguish it from a lumbar or hip joint pathology. Typically the patient complains of early-morning stiffness and pain, relieved by movement and made worse with rest, which may be due to the presence of inflammation. This is also typical behaviour of a ligamentous lesion and consistent with the complex ligamentous structure of the joint. Sleep can be disturbed as the pain wakes the patient when turning at night. The pain may also be worse when lying on the affected side. Twinges of pain are common, especially after a period of rest, when the patient takes time to ‘get going’ again. Sit to stand movements may reproduce symptoms and patients commonly point to the sacral sulcus, which is tender to palpation (Cibulka 2002).
Patients may complain of other symptoms which are typical of mechanical sacroiliac pain and distinguish it from other lesions. They cannot sit still or stand for long periods and the joint likes to be moved and exercised. Sunbathing, for example, is extremely uncomfortable, since they do not like lying flat with legs outstretched and find it hard to lie prone while reading a book. They cannot balance very well on the affected leg.
The absence of certain symptoms is also relevant in distinguishing sacroiliac joint problems from pain of lumbar origin, particularly arising from nerve root compression. There should be no paraesthesia and no bladder or bowel symptoms. A cough and sneeze may provoke a little pain, but this should always be in the back and not in the leg.
Symptoms of serious pathology, such as night pain and sweats, fever, feeling generally unwell or unexplained recent weight loss, should be excluded.
Other joint involvement will alert the examiner to possible inflammatory arthritis. However, the initial presentation of ankylosing spondylitis in the sacroiliac joints is common, without other joint signs or symptoms.
Past medical history will give information concerning conditions that may be relevant to the patient’s current complaint, always with the possible presence of serious illness in mind. An indication of the general health of the patient will indicate any systemic illness and it may be pertinent to take the patient’s temperature. Recent pregnancy may be a less sinister element of medical history that could be relevant to sacroiliac joint problems. A mechanical lesion of the sacroiliac joint is a common cause of pain in pregnancy, particularly in the later stages. The increase in weight, change in posture and release of the hormone relaxin all contribute to mechanical instability of the pelvis. Manipulation is indicated in these patients and the pregnancy is not a contraindication in itself (Golighty 1982, Daly et al 1991). As well as past medical history, establish any ongoing conditions and treatment. Explore other previous or current musculoskeletal problems with previous episodes of the current complaint, any treatment given and the outcome of treatment.
The medications currently being taken by the patient should be listed. This may provide further indication of the patient’s past medical history or alert the examiner to possible serious pathology, contraindications to treatment, and indications of past history of primary tumour, e.g. tamoxifen, an anti-oestrogen medication which is used in the treatment of some forms of breast cancer (Rang et al 2003). Anticoagulants and the use of long-term steroids should also be considered. The use of regular analgesia is worth noting as this may provide an objective marker for reassessment.
• Young: Under 20
• Elderly: First episode over 55
• Violent trauma
• Past medical history of malignancy
• Constant progressive pain
• Cauda equina syndrome
• Unremitting night pain
• Systemically unwell
• Unexplained weight loss
• Drug abuse and HIV
• Long-term systemic steroid use
• Widespread neurological signs and symptoms
• Gait disturbance
• Thoracic pain
• Inflammatory arthritis
• Associated abdominal pain
• Osteopenic/osteoporotic
• Sign of the buttock (p. 274)
Inspection
Position the patient in standing, undressed to underwear and in a good light. Assessment for bony deformity and overall posture is made with particular attention to pelvic asymmetry.
Pelvic asymmetry in the static posture:
• Level of iliac crests (Fig. 14.3)
 |
| Figure 14.3
Assessing level of iliac crests and anterior superior iliac spines.
|
• Level of ASIS (Fig. 14.3)
• Level of PSIS (Fig. 14.4)
 |
| Figure 14.4
Assessing level of posterior superior iliac spines.
|
• Leg length
• General spinal curvatures
• Increased or decreased lordosis.
Be aware that these signs cannot be considered in isolation as anomalies and leg length discrepancies commonly exist. The presence or absence of obvious asymmetry without associated appropriate symptoms is not necessarily relevant to mechanical dysfunction of the sacroiliac joint.
The assessment for positional alignment of various landmarks around the pelvis to establish asymmetry in either static or dynamic postures is a popular assessment tool, but is not without controversy. It must be recognized that this method lacks reliability and validity and is a subjective interpretation based on the examiner’s eye and experience.
Freburger & Riddle (1999) tested a method for measuring sacroiliac alignment using handheld calipers and an inclinometer in 73 symptomatic patients, but their results did not prove any more reliable than the observations mentioned above. Such studies rely on skilful therapists who are assumed to have a high level of knowledge of anatomy and are able accurately to palpate bony landmarks. However, Koran & McConnell (cited in O’Haire & Gibbons 2000) suggest that this is not necessarily the case, and Lewitt & Rosina (1999) suggest that palpating bone through soft tissue can produce a palpatory illusion due to changes in the soft tissue that occur as the result of pain. A further source of error could be the difficulty in accurately palpating bony landmarks in obese patients.
Riddle & Freburger (2002) were unsuccessful in demonstrating inter-tester reliability of a composite of four tests of pelvic symmetry and sacroiliac joint movement using a large group of patients. It was concluded that provocative, rather than alignment or movement, tests may have more support (see below).
Colour changes, muscle wasting and swelling are unusual unless there is a history of trauma. In sacroiliac joint strain or subluxation, an area of apparent swelling is sometimes present over the sacrum, usually associated with muscle spasm.
State at rest
Before any movements are performed, the state at rest is established to provide a baseline for subsequent comparison.
Examination by selective tension (objective examination)
The suggested sequence for the objective examination will now be given, followed by a commentary including the reasoning in performing the movements and the significance of the possible findings.
Eliminate the lumbar spine
• Active lumbar extension (Fig. 14.5)
 |
| Figure 14.5
Active lumbar extension.
|
• Active right lumbar side flexion (Fig. 14.6a)
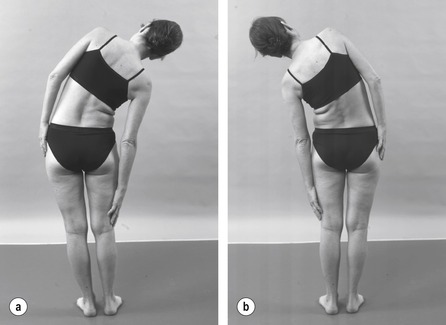 |
| Figure 14.6
(a,b) Active lumbar side flexions.
|
• Active left lumbar side flexion (Fig. 14.6b)
• Active lumbar flexion (Fig. 14.7)
 |
| Figure 14.7
Active lumbar flexion.
|
• Straight leg raise (Fig. 14.8)
 |
| Figure 14.8
Straight leg raise.
|
Eliminate the hip
• Passive hip flexion (Fig. 14.9a)
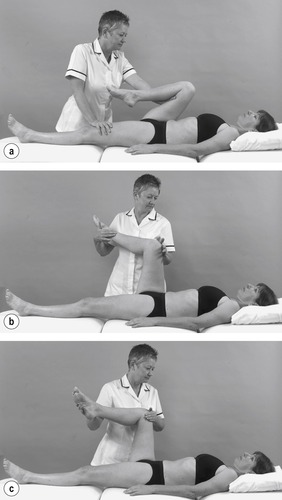 |
| Figure 14.9
Passive hip movements: (a) flexion; (b) medial; and (c) lateral rotation.
|
• Passive hip medial rotation (Fig. 14.9b)
• Passive hip lateral rotation (Fig. 14.9c)
Provocative shear tests for the posterior sacroiliac ligaments (Saunders 2000)
• Hip flexion towards the ipsilateral shoulder (Fig. 14.10)
 |
| Figure 14.10
Shear test with the femur pointing towards the ipsilateral shoulder.
|
• Hip flexion towards the contralateral shoulder (Fig. 14.11)
 |
| Figure 14.11
Shear test with the femur pointing towards the contralateral shoulder.
|
• Hip flexion towards the contralateral hip (Fig. 14.12)
 |
| Figure 14.12
Shear test with the femur pointing towards the contralateral hip.
|
Pain provocation test for the anterior ligaments
• FABER test (Fig. 14.13)
 |
| Figure 14.13
FABER or 4-test.
|
Further tests
• Distraction (gapping) test (Fig. 14.14)
 |
| Figure 14.14
Distraction test.
(Source: Olson: Manual Physical Therapy of the Spine, 2008 Elsevier)
|
• Compression test (Fig. 14.15)
 |
| Figure 14.15
Compression test.
(Source: Olson: Manual Physical Therapy of the Spine, 2008 Elsevier)
|
• Sacral thrust test (Fig. 14.16)
 |
| Figure 14.16
Sacral thrust test.
(Source: Olson: Manual Physical Therapy of the Spine, 2008 Elsevier)
|
Palpation
• For tenderness
Dynamic asymmetry palpation test to determine treatment technique
• The ‘walk’ test (Fig. 14.17a,b)
 |
| Figure 14.17
(a,b) The ‘walk’ test.
|
Examination of the sacroiliac joint must include elimination of the lumbar spine and hip joint as possible alternative causes of pain. The active movements of the lumbar spine and passive hip movements are assessed for range of movement and provocation of pain. If the symptoms are arising from the sacroiliac joint, pain is more commonly felt at the end of range of these movements, especially lumbar extension and passive hip lateral rotation. A unilateral reduction of hip lateral rotation has been associated with sacroiliac dysfunction (Chen et al 2002). The gross limitation of movement associated with lumbar lesions is not expected. Cited in Cibulka (2002), Mennell & Stoddard are credited with suggesting that, in sacroiliac dysfunction, palpation of the lumbar vertebrae in a posterior/anterior direction does not provoke the patient’s pain, whereas the patient may have pain on springing the sacrum or compression of the sacroiliac joints.
Pain provocation tests
Radiological and scanning techniques do not appear to be helpful towards the diagnosis of sacroiliac joint problems (Cohen 2005). Guided anaesthetic injections have traditionally been considered as the ‘gold standard’ for diagnosis. The technique is invasive and unwieldy in general clinical practice (Calvillo et al 2000, Chen et al 2002) and in principally investigating intra-articular sources of pain it appears to neglect the structures surrounding the sacroiliac joint, outside the joint capsule. The pain provocation tests claim to load the supporting structures surrounding the joint well (Robinson et al 2007). The ability to make the diagnosis of sacroiliac joint pain through the application of mechanical testing procedures is an important objective (Laslett et al 2005). En route to achieving this objective several studies have attempted to judge the reliability of various traditional tests for sacroiliac joint pain.
Most authors are in agreement that pain provocation tests are more reliable than palpation tests for sacroiliac joint dysfunction (Kokmeyer et al 2002, Robinson et al 2007). However, no individual pain provocation test has sufficient reliability or validity, leaving this a controversial topic. A battery of tests is used in clinical practice and it is commonplace to select three or four individual tests (Broadhurst & Bond 1998, Chen et al 2002).
Dreyfuss et al (1996) attempted to validate 12 commonly used tests by intra-articular diagnostic blocks using a stringent criterion of 90% relief of pain on reassessment. The tests assessed failed to show diagnostic value, but four tests proved the most sensitive in this study in the following order: sacral sulcus tenderness; pain over the sacroiliac joint; buttock pain; patient pointing to the posterior superior iliac spine.
Laslett & Williams (1994) assessed the reliability of various provocation tests and found that the distraction, compression, posterior thigh thrust and pelvic torsion tests (Gaenslen’s test) had the greatest inter-therapist reliability out of seven tests assessed, but that these needed to be studied further in order to establish their diagnostic power.
Broadhurst & Bond (1998) included the FABER test in their study, determining it to have a high degree of sensitivity and specificity.
Van der Wurff et al (2000) presented a systematic methodological review of reliability studies for pain provocation and motion palpation tests, identifying nine studies with acceptable methodological scores. The thrust test using the femur as a lever and Gaenslen’s test (see below) seemed to have the greatest reliability. However, the results were not shown to be uniformly reliable and the authors suggested that upgrading the methodology of the studies might have improved the results.
Freburger & Riddle (2001) found some support in the literature for the following pain provocation tests: FABER test, palpation over the sacral sulcus, thigh thrust or posterior shear test, resisted hip abduction, iliac compression and gapping. They suggest that in the absence of stronger evidence, positive pain provocation tests together with the patient’s descriptive information on pain referral patterns should be used towards diagnosis of sacroiliac joint dysfunction.
Kokmeyer et al (2002) recruited 78 subjects in a study to determine the reliability of a multitest regimen of five sacroiliac joint pain provocation tests for dysfunction. They describe the tests, but suggest that they have been modified, which raises the issue of standardization. They conclude that better statistical reliability could have been achieved by using the five tests in combination, rather than the individual tests themselves, and advocate a regimen of three positive indicators in the five tests. Levin, Nilsson-Wikmar, & Stendtröm (1998) and Levin, Nilsson-Wikmar, & Harms-Ringdahl et al. (2001) also raised standardization issues by examining the consistency of force variation and force distribution during pain provocation tests and their importance to pain response. They proposed that force registration would be a step towards standardizing the pain provocation tests.
The study to test the validity of individual provocation tests and composites of tests (Laslett et al 2005) was praised for its methodological quality in a rigorous review by Stuber (2007). Six provocation tests were selected for the study with justification for their selection based on previous study (Laslett & Williams 1994). The tests selected were: the distraction provocation (gapping) test; the thigh thrust provocation test; Gaenslen’s provocation test; compression provocation test; sacral thrust provocation test. The reader is referred to the paper itself (Laslett et al 2005) for a description of the tests as they were applied.
The study set out to explore the ability of the tests, or composites of the tests, to predict the results of fluoroscopically guided, contrast-enhanced sacroiliac anaesthetic block injections. The distraction test was found to have the highest single positive predictive value and was the most specific. The thigh thrust test was the most sensitive and with the compression and sacral thrust tests improved the overall diagnostic ability. Gaenslen’s test did not contribute positively and it was suggested that it could be removed from the procedure without affecting the diagnosis.
The key finding of the paper was that the tests should be applied as a composite test and, based on the study’s findings, to apply the distraction, thigh thrust, compression and sacral thrust techniques in that order, but to stop when there are two positives. This improved the sensitivity and specificity of the testing procedure. Any two of the remaining tests (excluding Gaenslen’s test) produced almost as good a result but because the thigh thrust and distraction tests have the highest individual sensitivity and specificity respectively it seems reasonable to apply those tests first. If none of the provocation tests provokes the patient’s pain, the sacroiliac joint can be ruled out as the source (Laslett et al 2005).
Robinson et al (2007) also looked at an array of one palpation and six provocation tests for sacroiliac joint pain with a focus on inter-rater reliability. They agreed with Laslett et al (2005) with regard to the reliability of the thigh thrust test. The reliability of the distraction and compression tests was found to be acceptable, but the reliability of the compression test was challenged in earlier studies. They also supported the value of using a cluster of tests to aid diagnosis and, in agreement with Laslett et al (2005), found that the specific tests selected were not as important as the number of the tests that were positive. In their study when three out of five tests were used as a marker for sacroiliac joint pain, there was good reliability amongst experienced therapists.
Arab et al (2009) looked at a relatively small sample of 25 patients and found that there was moderate to substantial intra- and inter-examiner reliability for individual tests and clusters of tests. Motion palpation tests fared well as part of the clusters too, where they had tended to be discounted in previous studies.
With regard to Robinson et al’s point above that there was ‘good reliability amongst experienced therapists’, they note that the physiotherapists used in their study were experienced manual therapists and had had additional training to encourage consistency in the application of the tests, which were applied in the same clinical setting. There may be less agreement between physiotherapists in an ordinary clinical setting or between various other medical specialists applying the procedures. Other factors such as size and shape of the patient matched with those similar features in the therapist might affect the ability to perform the techniques with a similar amount of pressure, or it might not be possible to perform them at all. The distraction technique can be uncomfortable for patients as pressure is applied against the anterior superior iliac spines, for example, and is difficult to apply in obese or pregnant patients
O’Sullivan & Beales (2007) suggest that the active straight leg raise is a means of testing the ability to transfer load between the lower limb and trunk, via the sacroiliac joint. The test involves lying supine and raising the leg 5 cm off the supporting surface. The test is positive if it brings on pain that is accompanied by a sensation of profound heaviness in the leg. The pain is relieved by applying compression to the ilia which may enhance the closure force through the sacroiliac joint.
Stuber (2007) highlights the specificity of the REAB test (REsisted hip ABduction) which should be borne in mind when differentiating between pain arising from the hip or sacroiliac joint. Arab et al (2009) supported Stuber and indicated substantial reliability for resisted abduction as a single test.
In the orthopaedic medicine approach, tests are applied to stress the posterior and anterior ligaments supporting the joint.
For the purposes of assessment in orthopaedic medicine, the three pain provocation tests for the posterior ligaments, and one pain provocation test, the FABER test for the anterior ligaments, will be described. Reproduction of the patient’s pain on the provocation tests constitutes a positive result for that test.
For the posterior ligaments, a version of the thigh thrust or posterior shear (POSH) test is applied. The aim of this test is to apply a posterior shearing force to the sacroiliac joint via the femur but it relies on the lumbar spine and hip first being excluded as a cause of pain. The patient lies supine with the ipsilateral knee flexed to approximately 90° and the contralateral leg extended. The examiner adducts the femur to the midline and applies axial pressure along the length of the femur. A similar test has also been described by Saunders (2000) and has been modified to include two additional provocative testing positions:
• Hip flexion towards the ipsilateral shoulder (see Fig. 14.10)
• Hip flexion towards the contralateral shoulder (see Fig. 14.11)
• Hip flexion towards the contralateral hip (see Fig. 14.12).
With the above tests, care should be taken not to excessively adduct the femur as this is uncomfortable even in the normal state and may contribute to false-positive results.
The tests are applied as a thrust through the shaft of the femur to assess the posterior ligaments. All three tests are performed on the pain-free side first for subsequent comparison with the painful side.
(1) Place the patient in supine-lying, flex the hip to approximately 90° and adduct the femur towards the ipsilateral shoulder. Grasp the patient’s knee with linked hands and apply a thrust down through the line of the shaft of the femur to stress the posterior sacroiliac joint ligaments. Pain in the buttock on the affected side denotes a positive test (Fig. 14.10).
The test is then repeated twice, but using in turn: (2) hip flexion towards the contralateral shoulder (see Fig. 14.11); and (3) hip flexion and adduction towards the contralateral hip (see Fig. 14.12) as the starting positions. Take care to release some pressure from the hip joint flexion and adduction before applying the downward thrust.
Drawn from the discussion above, the practitioner may also want to proceed to apply the distraction (gapping) technique, the compression technique and the sacral thrust technique. Sacroiliac pain is indicated once two of the tests are painful but if none of the tests reproduces the patient’s pain the sacroiliac joint can be ruled out as the cause (Laslett et al 2005).
Distraction (gapping) test
The patient lies supine (see Fig. 14.14). Cross your hands over and place the fleshy heel of each hand against the anterior superior iliac spines on the pelvis. Press down and outwards with your hands (posteriorly and laterally). This can be an uncomfortable test for the patient as the soft tissues are compressed against the bone as the pressure is applied. Care should be taken to apply the test as comfortably as possible by adjusting your palms and the patient should be warned before the pressure is applied. The test is positive if the patient’s pain is reproduced, which is usually in the gluteal region or posterior thigh.
Compression test
The patient is placed in supine (Fig. 14.5) or preferably side-lying, painful side uppermost (see Fig. 14.15). Place your hands on the upper part of the iliac crest and press downwards towards the floor. It is easier to apply the pressure if your arms are straight. The test is positive if the patient’s pain is reproduced or if there is a sensation of increased discomfort in the region of the sacroiliac joint.
Sacral thrust test
The patient lies prone (see Fig. 14.16). Place the heel of your hand on the base of the patient’s sacrum and reinforce with your other hand on top if necessary. Keep your arm(s) straight if possible and apply a downward forward thrust onto the sacrum to cause a shearing force through the sacroiliac joints. If positive, the test produces pain within the affected joint and there may be some accompanying referral into the buttock and posterior thigh.
Pain provocation test for the anterior ligaments
The distraction test described above aims to stretch the anterior sacroiliac ligaments. The FABER test (see Fig. 14.13) also assesses mainly the anterior ligaments and derives its name from the combination of movements applied, being Flexion, ABduction and External Rotation of the hip. It is also known as Patrick’s test or the ‘4-test’ because of the resultant position of the limb. The FABER test has not been discounted as strenuously as some of the other tests and it is commonly used in clinical practice (Cohen 2005). Broadhurst & Bond (1998) determined it to have a high degree of sensitivity and specificity but this was challenged by van der Wurff et al (2000). The test ties in with the pain and limitation of movement that can be provoked by lateral rotation at the hip, as mentioned above.
Perform the test on the pain-free side first for subsequent comparison. With the patient in supine-lying, the foot of one leg is placed on the knee of the other and the leg allowed to rest in lateral rotation and abduction. An assessment is made of the range of movement which is usually limited in sacroiliac joint problems. Pain reported at this stage is more likely to be indicative of hip joint pathology. Stabilize the opposite side of the pelvis and stress the sacroiliac joint by placing gentle downward pressure on the flexed knee. Pain now reported in the back incriminates the sacroiliac joint as a cause of symptoms (Hoppenfeld 1976).
Other tests should be recognized as a guide until reliability and validity are confirmed. It must also be acknowledged that the pain provocation tests are non-specific because they stress a number of adjacent structures around the hip, the lower lumbar spine and the sciatic and femoral nerves (Chen et al 2002).
Palpation
Palpation may be conducted for tenderness which is often located over the PSIS, sacral sulcus and surrounding area and is absent on the unaffected side. However, such tenderness is also often present in lumbar pathology and should not be taken by itself as a positive sign of sacroiliac joint involvement.
Dynamic asymmetry palpation tests to determine treatment technique
Dynamic palpation tests assess symmetry and movement of the pelvis and are applied to determine the choice of treatment technique. Like the pain provocation tests above, these tests are also a source of controversy within the literature and most authors are in agreement that pain provocation tests are more reliable than palpation tests for sacroiliac joint dysfunction (Kokmeyer et al 2002, Robinson et al 2007). O’Haire & Gibbons (2000) demonstrated a greater intra-tester reliability than inter-tester, stating that the reliability of palpation requires validation. One might expect that the examiner’s level of experience would be reflected in their palpation skills but this is not supported by the literature and disappointing results may be due to examiners failing to palpate the same structures.
Levangie (1999) assessed the association between innominate torsion and four movement tests and concluded that the tests were not useful in identifying innominate torsion, warning clinicians to be cautious in their use until more reliable data are available.
Palpation tests to detect joint mobility will be included here as a guide to treatment technique selection but at the time of writing little evidence has been found in the literature to support them (see Arab et al 2009 above). It is also worth considering that in assessing the standing forward flexion test, Egan et al (1996) found a positive result in asymptomatic patients, which questions the belief in a cause–effect relationship between asymmetry and symptoms.
The ‘walk’ test (Saunders 2000) (Fig. 14.17a,b) may be applied. The patient stands with both hands on a wall or chair to balance themselves. Crouch down so that you are at eye level with the sacrum and the PSISs. Tuck each thumb up and under the PSIS on either side firmly to locate their position. Ask the patient to flex alternate hips to 90° without tilting the pelvis, as if taking a marching step, and note the movement of one PSIS in relation to the other. If normal, the clinician would expect the PSIS on the non-weight-bearing leg to rotate posteriorly. In order for the test to be significant and imply hypomobility, a comparison between the two sides is made. If the symptomatic side rotates less posteriorly or more posteriorly than the asymptomatic side a clue is given to help treatment choice.
The authors have observed clinically that, in conducting the ‘walk’ test, balance on the standing leg may be difficult, especially on the symptomatic side, and that juddering of the abdominal muscles and/or hip flexors of the non-weight-bearing leg may occur, possibly indicating poor core stability. Hungerford et al (2007) describe the ‘stork test’ that assesses the ability to maintain a stable alignment of the innominate relative to the sacrum. In single-leg stance, the innominate bone should rotate posteriorly relative to the sacrum but in subjects with pelvic girdle pain the bone tends to rotate anteriorly suggesting a failure of the self-bracing mechanism.
The ‘walk’ test may provide a clue for the application of treatment techniques in that if the PSIS on the painful side appears to rotate more posteriorly in relation to the other then a technique, and appropriate exercises, will be selected to produce anterior rotation, and vice versa. If no movement abnormality is detected, a more general technique will be applied.
An alternative is the Gillet test, also known as the ipsilateral kinetic test or ipsilateral rotation test (Fowler 1994, Dreyfuss et al 1996, Levangie 1999, Lee 2000) which may also be applied to assess symmetry on movement. With the patient in standing, supported against a wall, place your right thumb on the right PSIS. Place your left thumb on the median sacral crest at the level of S2, or the sacral base, keeping thumbs parallel. Ask the patient to flex the right hip and knee. The right innominate bone should rotate posteriorly relative to the fixed sacrum and therefore the movement of the right thumb should be caudal. The test is positive and demonstrates hypomobility if the right thumb fails to move posteriorly relative to the sacrum. Repeat the test on the other side to compare.
To recap, diagnosis at the sacroiliac joint relies on the history (subjective examination) and positive pain provocation tests. The dynamic asymmetry palpation tests provide clues to treatment.
Treatment for sacroiliac joint pain aims to restore normal function – movement and stability – and the assessment and rehabilitation of stability is outside the scope of this text. With regard to restoring normal movement, having completed the examination, a hypothesis is established relating to the patient’s signs and symptoms. If a diagnosis of a mechanical lesion of the sacroiliac joint is made, manipulation is the treatment of choice provided no contraindications exist.
Mechanical lesions of the sacroiliac joint
Diagnosis at the sacroiliac joint is challenging due to varied and overlapping symptoms, a rich and varied nerve supply and because symptoms may be due to a distant manifestation of injury in other parts of the kinetic chain (Chen et al 2002). Cohen (2005) looked at the prevalence of sacroiliac joint pain by reviewing studies that had used guided anaesthetic injections to confirm diagnosis. Based on the studies reviewed he concluded that the prevalence of sacroiliac joint pain in patients presenting with low back pain was in the 15–20% range. Hansen et al (2007) widened the range to 10–27% and Hungerford et al (2007) claimed the single figure of 15%. It must be recognized that, until supported by evidence, diagnosis depends on the clinician’s interpretation of a number of factors including the subsequent response to treatment. Progression of treatment is based on the process of constant re-examination. As examination of the sacroiliac joint is not usually conducted in isolation, the recommended guidelines for safe practice of manipulation are the same as those covered in the lumbar spine (see Ch. 13). The clinician must take all due care when applying the treatment techniques.
Indications for sacroiliac joint manipulation are as follows:
• History of a mechanical lesion of the sacroiliac joint, implying hypomobility on the symptomatic side due to subluxation or sprain
• Absence of signs in the lumbar spine and hip
• At least one positive pain provocation test
• Static and dynamic palpation tests can indicate a pelvic rotation or asymmetry that may help with choice of treatment technique after clinical diagnosis.
Contraindications to sacroiliac joint manipulation
It is impossible to be absolutely definitive about all contraindications and nothing can substitute for a rigorous assessment of the presenting signs and symptoms and an accurate diagnosis of a mechanical sacroiliac lesion.
‘Red flags’ are signs and symptoms found in the patient’s subjective and objective examination that may indicate serious pathology and provide contraindications to sacroiliac joint manipulation (Greenhalgh & Selfe 2006, Sizer et al 2007) (see ‘Red flags’ Box on p. 419).
In the sacroiliac joint there are few contraindications but it may be useful to use the mnemonic ‘ COINS’ (a contraction of ‘ contra indication s’), as an aide-mémoire to be able to create mental categories for the contraindications: Circulatory, Osseous, Inflammatory, Neurological and suspicious features indicating Serious pathology. If the first and last two letters are pushed together as ‘ CONS’, the crucial need for consent is emphasized.
Absence of informed patient consent is an absolute contraindication. An absence of dural, cauda equina and radicular signs and/or symptoms would be expected. The clinician should be alert to suspicious features as indicators of serious pathology and any drug history requiring caution. Sacroiliac dysfunction in the elderly is an uncommon cause of pain and caution is suggested before proceeding with the manipulative techniques described below (Dar et al 2008). Occasionally the patient may present with a highly irritable inflammatory lesion and it may not be possible to apply the manipulative techniques. In such a case, for the reasons suggested above, it may be possible to reverse the technique and apply it to the asymptomatic side.
Sacroiliac manipulation procedure
It is recommended that a course in orthopaedic medicine is attended before the treatment techniques described are applied in clinical practice (see Appendix 1). For all sacroiliac techniques, the height of the couch is a matter of personal choice. As a suggestion, placing the couch at the level of your mid-thigh gives you the opportunity to assist the technique by gapping/distraction of the joint. However, the position will ultimately be determined by the relative sizes of the clinician and the patient – in general, the larger the patient, the lower the bed.
Sacroiliac joint gapping/distraction technique (Saunders 2000)
The indication for this technique is diagnosis of sacroiliac joint hypomobility with no observable pelvic asymmetry or difference in movement of the PSIS during the dynamic palpation tests.
Position the patient in side-lying, painful side uppermost, pulling the underneath shoulder well through to stabilize the patient. Flex the upper leg so that the hip is in a neutral position with the knee over the edge of the bed. Stand in front of and facing the patient and take your forearm that is closest to the patient’s head and place it comfortably in the patient’s waist under the ribs, pushing backwards against the soft tissues to fix the lumbar spine, and allowing the pelvis to fall slightly backwards from the midline. Apply gentle downwards pressure along the line of the femur to gap/distract the sacroiliac joint and maintain this by resting your caudal knee against the patient’s flexed knee (Fig. 14.18a). Place your other forearm on the blade of the ilium, to be at right angles with your forearm in the patient’s waist. Continue to take up the slack by drawing the forearm on the ilium towards you and apply a minimal amplitude, high velocity thrust at the end of range (Fig. 14.18b).
 |
| Figure 14.18
(a,b) Sacroiliac joint-gapping technique.
|
Rotation of the pelvis down/posteriorly on the painful side (Saunders 2000)
The indication for this technique is diagnosis of sacroiliac joint hypomobility with either static or dynamic palpation tests, indicating that the PSIS is rotated up or anteriorly on the painful side in relation to the other PSIS. Position the patient as above and fix under the rib cage with the forearm as before. Place the patient’s flexed hip and knee towards more hip flexion to assist rotation of the pelvis posteriorly on the painful side. Gap/distract the sacroiliac joint as described above. Place the medial epicondyle of your other elbow on the patient’s ischial tuberosity. Once all the slack has been taken up by rotating your body and arms to pull the ischial tuberosity towards you, apply a minimal amplitude, high velocity thrust (Fig. 14.19).
 |
| Figure 14.19
Rotation of the pelvis posteriorly or downwards on the painful side.
|
Rotation of the pelvis up/anteriorly on the painful side (Saunders 2000)
The indication for this technique is diagnosis of sacroiliac joint hypomobility with the palpation tests indicating that the PSIS is rotated down or posteriorly on the painful side in relation to the other PSIS.
Position the patient as above and fix under the rib cage with one forearm. Place the flexed hip and knee towards hip extension to assist rotation of the pelvis anteriorly on the painful side. Gap/distract the sacroiliac joint as described above. Place the forearm of your other arm to apply pressure just behind the iliac crest, but keep your forearms parallel. Pull your arm on the iliac crest towards you and under your other arm and, once all the slack has been taken up, apply a minimal amplitude, high velocity thrust (Fig. 14.20).
 |
| Figure 14.20
Rotation of the pelvis anteriorly or upwards on the painful side.
|
Leg tug
The indication for this technique is any diagnosis of sacroiliac joint hypomobility. It is particularly useful during the later stages of pregnancy when the associated hypermobility may allow malalignment of the joint surfaces, which can then appear as objective hypomobility (see below). Position the patient comfortably in supine-lying with the couch at about knee height. Hold the patient’s ankle of the symptomatic side and place your knee against the patient’s foot on the good side, to prevent the patient slipping down the bed. Apply a degree of distraction together with a circumduction movement of the hip. Once the patient relaxes, apply a sharp caudal tug (Fig. 14.21).
 |
| Figure 14.21
Leg tug.
|
Reducing hypomobility due to a sacroiliac subluxation or relieving stress on the ligaments can be very successful. Following treatment, attention should be given to the prevention of recurrence. Discussions with the patient will allow advice to be given about lifestyle habits that may be contributing to the condition and any imbalances and postural problems can be addressed. Following reduction of subluxation in the later stages of pregnancy, a supportive brace may be helpful. The following exercises may be useful in a maintenance programme:
• In supine-lying, ask the patient to flex one knee to the chest while the other leg hangs over the edge of the couch. Anterior or upwards rotation is encouraged in the extended leg and posterior or downwards rotation in the flexed leg (Fig. 14.22).
 |
| Figure 14.22
Exercise in supine-lying, encouraging movement of the posterior superior iliac spine.
|
• Standing with one leg on a stool, ask the patient to make a lunging movement forwards, involving flexion at the hip and extension at the lumbar spine. Anterior or upwards rotation of the PSIS is encouraged on the side of the standing, extended leg, and posterior or downwards rotation of the PSIS is encouraged on the side of the flexed leg (Fig. 14.23a,b).
 |
| Figure 14.23
(a,b) Exercise in standing, encouraging movement of the posterior superior iliac spine.
|
Sacroiliac hypermobility
Hypermobility or instability of one sacroiliac joint may be due to a traumatic incident, repetitive microtrauma or secondary to hormonal changes (Lee 2000). Diagnosis will again be clinical depending on the history and the pain provocation tests. The static and dynamic palpation tests will demonstrate asymmetry while objectively the joint will give an impression of hypomobility when the pain provocation tests are applied. Applying the manipulative techniques (see above) may successfully correct the malalignment of the symptomatic sacroiliac joint. Once reduction has been effected, stability tests reveal the excessive range of movement and this will need the support of a pelvic belt and correction of any muscle imbalances. This topic is outside the scope of this text, however, and the reader is referred to other texts. Sclerosant injections have also been described (see below).
Traction
The use of traction is not indicated with a sacroiliac joint problem. Where the differential diagnosis is uncertain between a lumbar or sacroiliac joint problem, the latter may be suspected if the application of traction makes the pain worse, since the position of the pelvic harness over the ilia applies stress through the sacroiliac joints when the traction is applied.
Sclerosant injections
In cases of extreme laxity of the sacroiliac joints, associated with frequent episodes of subluxation, sclerosant injections may be used to induce scarring in the ligaments, so tightening the tissues to support the joint (Cohen 2005) (see Ch. 4). It is important that the subluxation is reduced before the injections are given. Sclerosants would not be appropriate in pregnancy but, in any event, the ligamentous softening is likely to resolve spontaneously within 4–5 months of delivery.
REFERENCES
Arab, A.M.; Abdollahi, I.; Joghataei, M.T.; et al., Inter- and intra-examiner reliability of single and composites of selected motion palpation and pain provocation tests for sacroiliac joint, Man. Ther. 14 (2009) 213–221.
Broadhurst, N.A.; Bond, M.J., Pain provocation tests for the assessment of sacroiliac dysfunction, J. Spinal Disord. 11 (4) ( 1998) 341–345.
Brukner, P.; Khan, K., Clinical Sports Medicine. 3rd edn. ( 2007)McGraw Hill, Sydney.
Calvillo, O.; Skaribas, I.; Turnipseed, J., Anatomy and pathophysiology of the sacroiliac joint, Curr. Rev. Pain 4 (5) ( 2000) 356–361.
Cassidy, J.D., The pathoanatomy and clinical significance of the sacro-iliac joints, J. Manip. Physiol. Ther. 15 (1992) 41–42.
Chen, Y.C.; Fredericson, M.; Smuck, M., The sacroiliac joint pain syndrome in active patients: a look behind the pain, Phys. Sports Med. 30 (11) ( 2002) 30–37.
Cibulka, M.T., Understanding sacroiliac joint movement as a guide to the management of a patient with unilateral low back pain, Man. Ther. 7 (4) ( 2002) 215–221.
Cohen, S.P., Sacroiliac joint pain: a comprehensive review of anatomy, diagnosis and treatment, Anesth. Analg. 101 (2005) 1440–1453.
Daly, K.M.; Frame, P.S.; Rapaza, P.A., Sacro-iliac subluxation: a common, treatable cause of low back pain in pregnancy, Fam. Pract. Res. J. 11 (1991) 149–159.
Dangaria, T.R., A case report of sacroiliac joint dysfunction with urinary symptoms, Man. Ther. 3 (4) ( 1998) 220–221.
Dar, G.; Khamis, S.; Peleg, S.; et al., Sacroiliac joint fusion and the implications for manual therapy diagnosis and treatment, Man. Ther. 13 (2008) 155–158.
Derby, R., Point of view, Spine 19 (1994) 1489.
Dreyfuss, P.; Michaelsen, M.; Pauza, K.; et al., The value of medical history and physical examination in diagnosing sacroiliac joint pain, Spine 21 (1996) 2594–2602.
Egan, D.; Cole, J.; Twomey, L., The standing forward flexion test: an inaccurate determinant of sacroiliac joint dysfunction, Physiotherapy 82 (4) ( 1996) 236–242.
Fortin, J.D.; Dwyer, A.P.; West, S.; et al., Sacro-iliac joint – pain referral maps upon applying a new injection/arthrography technique, part I. Asymptomatic volunteers, Spine 19 (13) ( 1994) 1475–1482.
Fortin, J.D.; Aprill, C.N.; Ponthieux, B.; et al., Sacroiliac joint – pain referral maps upon applying a new injection/arthrography technique, part II. Clinical evaluation, Spine 19 (13) ( 1994) 1483–1489.
Fortin, J.D.; Kissling, R.O.; O’Connor, B.L.; et al., Sacroiliac joint innervation and pain – a review paper, Am. J. Orthop. 28 (12) ( 1999) 687–690.
Fortin, J.D.; Washington, W.J.; Falco, F.J.E., Three pathways between the sacroiliac joint and neural structures, Am. J. Neuroradiol. 20 (8) ( 1999) 1429–1434.
Fowler, C., Muscle energy techniques for pelvic dysfunction, In: (Editors: Boyling, J.D.; Palastanga, N.) Grieve’s Modern Manual Therapy2nd edn. ( 1994)Churchill Livingstone, Edinburgh, pp. 781–791.
Freburger, J.K.; Riddle, D.L., Measurement of sacroiliac joint dysfunction: a multicentre intertester reliability study, Phys. Ther. 79 (12) ( 1999) 1134–1141.
Freburger, J.K.; Riddle, D.L., Using published evidence to guide the examination of the sacroiliac joint, Phys. Ther. 81 (5) ( 2001) 1135–1143.
Golighty, R., Pelvic arthropathy in pregnancy and the puerperium, Physiotherapy 68 (1982) 216–220.
Greenhalgh, S.; Selfe, J., Red Flags. ( 2006)Elsevier, Edinburgh.
Hansen, H.C.; McKenzie-Brown, A.M.; Cohen, S.; et al., Sacroiliac joint interventions: a systematic review, Pain Physician. 10 (2007) 165–184.
Harrison, D.E.; Harrison, D.D.; Troyanovich, S.J., The sacroiliac joint: a review of anatomy and biomechanics with clinical implications, J. Manip. Physiol. Ther. 20 (9) ( 1997) 607–617.
Hoppenfeld, S., Physical Examination of the Spine and Extremities. ( 1976)Appleton Century Crofts, Philadelphia.
Hungerford, B.A.; Gilleard, W.; Moran, M.; et al., Evaluation of the ability of physical therapists to palpate intrapelvic motion with the Stork test on the support side, Phys. Ther. 87 (7) ( 2007) 879–887.
Jacob, H.A.C.; Kissling, R.O., The mobility of the sacro-iliac joints in healthy volunteers between 10 and 50 years of age, Clin. Biomech. 10 (1995) 352–361.
Kapandji, I.A., The Physiology of the Joints, the Trunk and the Vertebral Column. vol. 3 ( 1974)Churchill Livingstone, Edinburgh.
Reiter’s syndrome and reactive arthritis, In: Collected Reports on the Rheumatic Diseases ( 1995)Arthritis and Rheumatism Council for Research, London, pp. 61–64.
Kissling, R.O.; Jacob, H.A.C., The mobility of the sacroiliac joints in healthy subjects, Bull. Hosp. Joint Dis. 54 (3) ( 1996) 158–164.
Kokmeyer, D.J.; van der Wurff, P.; Aufdemkampe, G.; et al., The reliability of multitest regimens with sacroiliac pain provocation tests, J. Manip. Physiol. Ther. 25 (1) ( 2002) 42–48.
Kumar, P.; Clark, M., Clinical Medicine. 5th edn. ( 2002)Baillière Tindall, London.
Laslett, M.; Williams, M., The reliability of selected pain provocation tests for sacro-iliac joint pathology, Spine 19 (11) ( 1994) 1243–1249.
Laslett, M.; Aprill, C.N.; McDonald, B.; et al., Diagnosis of sacroiliac joint pain: validity of individual provocation tests and composites of tests, Man. Ther. 10 (2005) 207–218.
Leblanc, K., Sacro-iliac sprain: an overlooked cause of back pain, Am. Fam. Phys. November (1992) 1459–1463.
Lee, D., The Pelvic Girdle. ( 2000)Churchill Livingstone, Edinburgh.
Levangie, P.K., Four clinical tests of sacroiliac dysfunction: the association of test results with innominate torsion among patients with and without low back pain, Phys. Ther. 79 (11) ( 1999) 1043–1057.
Levin, U.; Nilsson-Wikmar, L.K.; Stendtröm, C.H., Reproducibility of manual pressure force on provocation of the sacroiliac joint, Physiother. Res. Int. 3 (1) ( 1998) 1–14.
Levin, U.; Nilsson-Wikmar, L.; Harms-Ringdahl, K.; et al., Variability of forces applied by experienced physiotherapists during provocation of the sacroiliac joint, Clin. Biomech. 16 (2001) 300–306.
Lewitt, K.; Rosina, A., Why yet another diagnostic sign of sacro-iliac movement restriction?J. Manip. Physiol. Ther. 22 (3) ( 1999) 154–160.
O’Haire, C.; Gibbons, P., Inter-examiner and intra-examiner agreement for assessing sacroiliac anatomical landmarks using palpation and observation: a pilot study, Man. Ther. 5 (1) ( 2000) 13–20.
Oliver, J.; Middleditch, A., Functional Anatomy of the Spine. 2nd edn. ( 2006)Butterworth-Heinemann, Edinburgh.
O’Sullivan, P.B.; Beales, D.J., Changes in pelvic floor and diaphragm kinematics and respiratory patterns in subjects with sacroiliac joint pain following a motor learning intervention: a case series, Man. Ther. 12 (3) ( 2007) 209–218.
Palastanga, N.; Field, D.; Soames, R., Anatomy and Human Movement. 5th edn. ( 2006)Butterworth-Heinemann, Edinburgh.
Rai, A., Ankylosing spondylitis, In: Collected Reports on the Rheumatic Diseases ( 1995)Arthritis and Rheumatism Council for Research, London, pp. 65–68.
Rang, H.P.; Dale, M.M.; Ritter, J.M.; et al., Pharmacology. 5th edn. ( 2003)Churchill Livingstone, Edinburgh.
Riddle, D.; Freburger, J.K., Evaluation of the presence of sacroiliac joint region dysfunction using a combination of tests: a multicentre intertester reliability study, Phys. Ther. 82 (8) ( 2002) 772–781.
Robinson, H.S.; Brox, J.I.; Robinson, R.; et al., The reliability of selected motion- and pain provocation tests for the sacroiliac joint, Man. Ther. 12 (2007) 72–79.
Saunders, S., Orthopaedic Medicine Course Manual. ( 2000)Saunders, London.
Schmid, H.J.A., Sacroiliac diagnosis and treatment, Man. Med. 1 (1984) 33–38.
Schwarzer, A.C.; Aprill, C.N.; Bogduk, N., The sacro-iliac joint in chronic low back pain, Spine 20 (1995) 31–37.
Silberstein, M.; Hennessy, O.; Lau, L., Neoplastic involvement of the sacroiliac joint – MR and CT features, Australas. Radiol. 36 (1992) 334–338.
Sizer, P.; Brismée, J.; Cook, C., Medical screening for red flags in the diagnosis and management of musculoskeletal spine pain, Pain Pract. 7 (1) ( 2007) 53–71.
Slipman, C.W.; Jackson, H.B.; Lipetz, J.S.; et al., Sacroiliac joint pain referral zones, Arch. Phys. Med. Rehabil. 81 (3) ( 2000) 334–338.
Standring, S., Gray’s Anatomy: The Anatomical Basis of Clinical Practice. 40th edn. ( 2009)Churchill Livingstone, Edinburgh.
Stuber, K.J., Specificity, sensitivity, and predictive values of clinical tests of the sacroiliac joint: a systematic review of the literature, J. Can. Chiroprac. Assoc. 51 (1) ( 2007) 30–41.
Swezey, R.L., The sacroiliac joint, Phys. Med. Rehabil. Clin. N. Am. 9 (2) ( 1998) 515–519.
Tibor, L.M.; Sekiya, J.K., Differential diagnosis of pain around the hip joint, Arthroscopy 24 (12) ( 2008) 1407–1421.
Trotter, M., Variations of the sacral canal: their significance in the administration of caudal analgesia, Curr. Res. Anesth. Analg. 26 (1947) 192–202.
van der Wurff, P.; Hagmeijer, R.H.M.; Meyne, W., Clinical test of the sacroiliac joint, part I. Reliability, Man. Ther. 5 (1) ( 2000) 30–36.
Vleeming, A.; Stoeckart, R.; Volkers, C.W.; et al., Relation between form and function in the sacro-iliac joint, part I. Clinical anatomical aspects, Spine 15 (2) ( 1990) 130–132.
Vleeming, A.; Stoeckart, R.; Volkers, C.W.; et al., Relation between form and function in the sacro-iliac joint, part II. Biomechanical aspects, Spine 15 (2) ( 1990) 133–135.
Vleeming, A.; Pool-Goudzwaard, L.; Hammudoghlu, D.; et al., The function of the long dorsal sacro-iliac ligament, Spine 21 (5) ( 1996) 556–562.
Zheng, N.; Watson, L.G.; Yong-Hing, K., Biomechanical modelling of the human sacroiliac joint, Med. Biol. Eng. Comput. 35 (2) ( 1997) 77–82.