CHAPTER 17 The Role of Wrist Arthroscopy in Intra-Articular Distal Radius Fracture Management
Introduction
Lafontaine has described several radiographic features that signify when a fracture of the distal radius is unstable.1 These include initial dorsal angulation greater than 20 degrees, extensive dorsal comminution, associated ulnar styloid fracture, significant intra–articular involvement, and older patients greater than the age of 60.
The prognosis for intra–articular fractures of the distal radius has been shown to depend on numerous factors.2 These include the amount of radial shortening, residual extra–articular angulation, articular congruity of both the radiocarpal and radioulnar joints, and associated intra–articular soft–tissue injuries. Trumble et al., in their review of 52 intra–articular fractures, noted that factors that strongly correlated with a successful outcome included the amount of residual radial shortening and intra–articular congruity.3
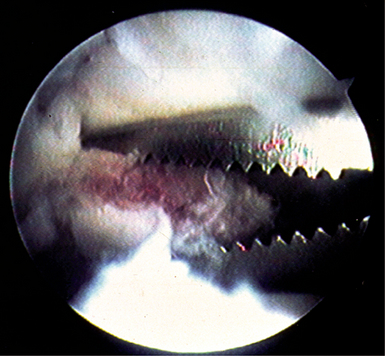
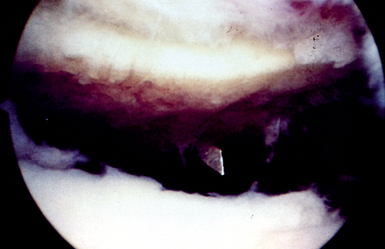
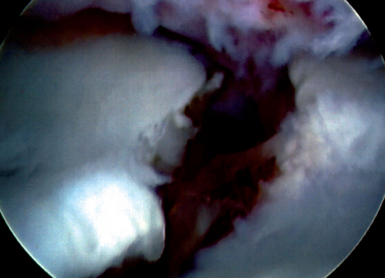
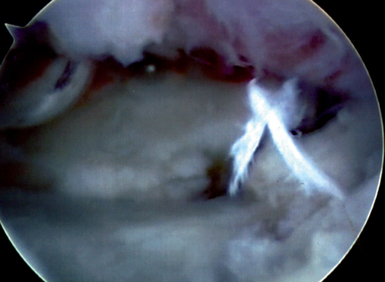
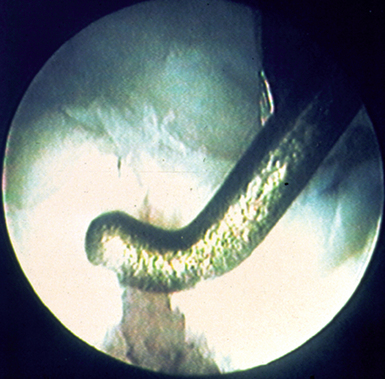
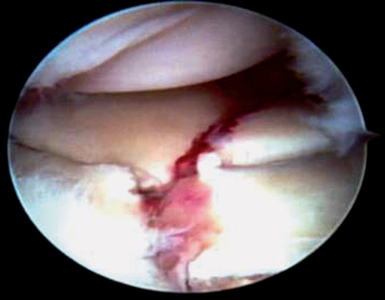
The use of wrist arthroscopy as an adjunct in the management of displaced intra–articular distal radius fractures takes advantage of its ability to view the articular surface with bright light and magnified conditions with minimal surgical morbidity.4 Fracture hematoma and debris may be arthroscopically lavaged, which potentially can improve the patient’s final range of motion5 (Figure 17.1). In addition, associated intra–articular soft–tissue injuries may be detected and managed at the same sitting6 (Figure 17.2). Pathology not readily identified on plain radiographs is frequently discovered during arthroscopic–assisted reduction and internal fixation of distal radius fractures. In most instances, it is much easier to manage an acute soft–tissue injury that occurs with a distal radius fracture than chronic pathology. The purpose of this chapter is to review the rationale and technique in the application of wrist arthroscopy as a useful adjunct in the management of displaced intra–articular fractures of the distal radius.
Two millimeters of articular displacement has over the past several years become a well–established critical threshold for articular incongruity of the distal radius. Knirk and Jupiter, in their classic article, demonstrated the importance of an articular reduction within 2 mm or less.7 A patient whose articular reduction is greater than 2 mm at final follow–up visit has a significantly higher incidence of degenerative changes within the wrist. Bradway and Amadio further substantiated these findings in their study.8
In their series of 40 patients, Fernandez and Geissler noted that the critical threshold may be as low as 1 mm or less.9 They reported in their study that the incidence of complications was substantially lower and articular reduction was within 1 mm or less.
Edwards et al. described the advantage of viewing intra–articular reduction by wrist arthroscopy compared to monitoring under fluoroscopy alone.10 In their series, 15 patients underwent arthroscopic evaluation of the articular surface of the distal radius following reduction and stabilization under fluoroscopy. They found that 33% of the patients had an articular step–off of 1 mm or more as viewed arthroscopically. Frequently, the fragment was rotated. Wrist arthroscopy is particularly useful in judging the rotation of fracture fragments, which is not readily identifiable under fluoroscopy. Edwards et al. concluded that utilizing wrist arthroscopy as an adjunct may detect residual gapping not previously identified under fluoroscopy alone.
A high incidence of associated intra–articular soft–tissue injuries involving the triangular fibrocartilage complex and the interosseous ligaments has been shown by several studies of displaced intra–articular fractures of the distal radius.11 Mohanti and Fontes, in two separate wrist arthrogram studies, noted a high incidence of tears of the triangular fibrocartilage complex associated with distal radius fractures. Fontes, in his series, noted a 66% incidence of tears of the triangular fibrocartilage complex in 58 patients.12 Similarly, Mohanti noted an injury of the triangular fibrocartilage complex in 45% of 60 patients in his series.13
Several recent arthroscopic studies have documented incidences of associated intercarpal soft–tissue injuries with fractures of the distal radius. In three recent published studies, an injury to the triangular fibrocartilage complex seems to be the most common associated intra–articular soft–tissue injury. Geissler et al. reported their experience in 60 patients with displaced intra–articular fractures of the distal radius undergoing arthroscopic–assisted reduction and evaluation.14 The criterion for surgical stabilization in his series was an intra–articular fracture displaced 2 mm or more that cannot be reduced by closed manipulation. In Geissler et al.’s series, 49% of the patients had a tear of the triangular fibrocartilage complex. An injury to the interosseous ligaments was less common. Tears to the scapholunate interosseous ligament were present in 32% of patients, and injury to the lunotriquetral interosseous ligament was identified in 15%.
Lindau, in a similar arthroscopic study of 50 patients, noted that tears of the triangular fibrocartilage complex were present in 78% of patients, injuries to the scapholunate ligament were identified in 54% of patients, and tears of the lunotriquetral interosseous ligament were less common and seen in 16% of patients.15 Hanker, in a series of 65 patients, noted that tears of the triangular fibrocartilage complex were very common and were present in 55% of the patients in his series.16 Although it is clearly documented that associated soft–tissue injuries are common with displaced intra–articular fractures of the distal radius, how they may affect the final outcome in patients is still unknown.
Geissler et al. described an arthroscopic classification of an interosseous ligament injury based on their work on arthroscopic management of fractures of the distal radius.14 They noted that a spectrum of injury may occur to the interosseous ligament. The ligament attenuates, and then eventually tears, and the degree of rotation between the carpal bones increases. The scapholunate interosseous ligament appears to tear from volar to dorsal. This arthroscopic classification of carpal instability is based on observation of interosseous ligaments from both the radiocarpal and midcarpal spaces (Table 17.1).
Table 17.1 Geissler Arthroscopic Classification of Carpal Instability
| Grade | Description | Management |
|---|---|---|
| I | Attenuation/hemorrhage of interosseous ligament as seen from the radiocarpal joint. No incongruency of carpal alignment in the midcarpal space. | Immobilization |
| II | Attenuation/hemorrhage of interosseous ligament as seen from the radiocarpal joint. Incongruency/step-off as seen from midcarpal space. A slight gap (less than width of a probe) between the carpal bones may be present. | Arthroscopic reduction and pinning |
| III | Incongruency/step-off of carpal alignment is seen in both the radiocarpal and midcarpal space. The probe may be passed through gap between the carpal bones. | Arthroscopic/open reduction and pinning |
| IV | Incongruency/step-off of carpal alignment is seen in both the radiocarpal and midcarpal space. Gross instability with manipulation is noted. A 2.7-mm arthroscope may be passed through the gap between the carpal bones. | Open reduction and repair |
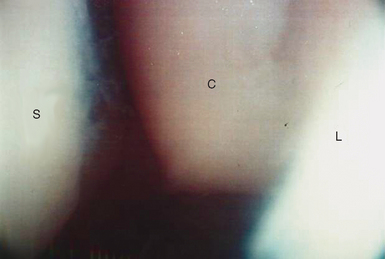
The normal scapholunate and lunotriquetral interosseous ligaments have a concave appearance between the carpal bones as viewed from the radiocarpal space. The scapholunate ligament is best seen with the arthroscope in the 3–4 portal. The lunotriquetral interosseous ligament is best observed with the arthroscope placed in either the 4–5 or 6–R portal. The lunotriquetral interval will not be adequately seen with the scope in the 3–4 portal alone. In the midcarpal space, the scapholunate interval should be tight and congruent without any articular step–off. Similarly, the lunotriquetral interval should be congruent, but usually a 1–mm step–off or slightly increased play may be seen between the lunate and triquetrum as observed from the radial midcarpal space. A probe or needle may be inserted in the ulnar midcarpal space to evaluate the amount of play between the carpal bones.
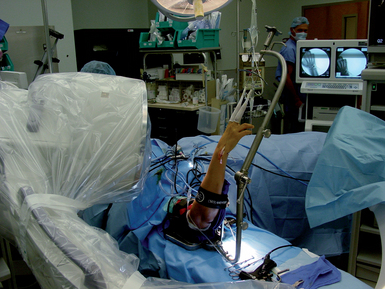
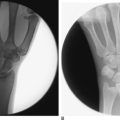
A traction tower is very useful in the arthroscopic–assisted management of intra–articular fractures of the distal radius. A traction tower allows the surgeon to flex, extend, and radial and ulnar deviate the wrist to help reduce the fracture fragments while maintaining constant traction to allow visualization. A new traction tower was designed to allow the surgeon to simultaneously evaluate arthroscopically the articular reduction and to monitor the reduction under fluoroscopy (Figure 17.3). The traction bar is uniquely placed at the side of the wrist rather than at its center, so that it does not block fluoroscopic evaluation and the surgeon does not need to work around a central bar. In addition, by having the traction bar at the side rather than centrally allows the surgeon to simultaneously arthroscope the wrist and stabilize the fracture while obtaining access through a standard volar approach.
The surgeon can fluoroscopically evaluate the position of the plate and screw insertion during stabilization. This new traction tower allows a surgeon to perform arthroscopic–assisted fixation in both the vertical and/or horizontal planes, depending on the surgeon’s preference.(Figure 17.4). If a traction tower is not available, the wrist may be suspended with finger traps attached to a weight over the end of a hand table in the horizontal position, or with a shoulder holder in the vertical position. A small bump is useful to place under the wrist if weights are being utilized over the end of the table to maintain the wrist in slight flexion.
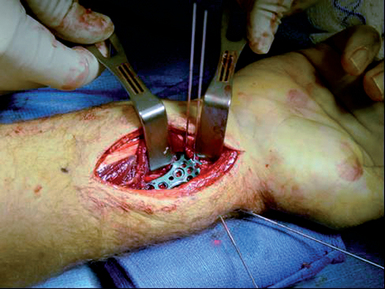
Fractures without extensive metaphysial comminution are most ideal for arthroscopic–assisted management. Radial styloid fractures, die punch fractures, three–part T fractures, and four–part fractures are all amenable to arthroscopic–assisted reduction and internal fixation.17 Some three–part fractures and most four–part fractures are managed through a combination of open reduction and arthroscopic–assisted fixation. In these instances, the fracture is stabilized by a volar plate through a volar approach (but the joint capsule is not incised). Articular reduction may be arthroscopically fine–tuned, and the distal screws inserted to stabilize the fracture. Associated soft–tissue injuries are detected and managed in the same sitting.
Radial Styloid Fractures
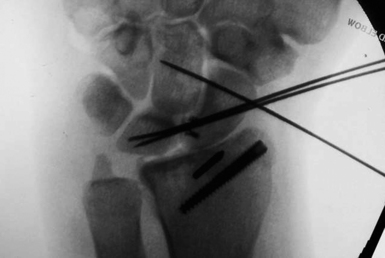
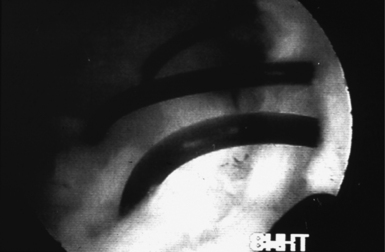
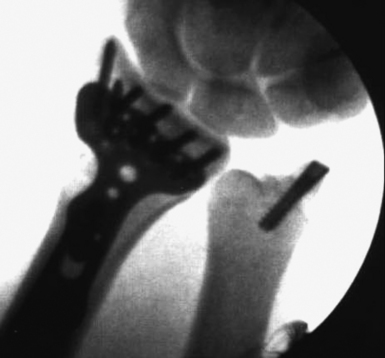
An alternative technique is to advance the guide wire or Kirschner wire under fluoroscopy into the radial styloid fragment alone, and not across the fracture site (Figure 17.5). The position of the guide wire in the radial styloid fragment and its angle in relation to the fracture is viewed directly under fluoroscopy. The wrist is then suspended in the traction tower and the standard wrist arthroscopy portals are made. Similar to before, the best view to judge rotation and reduction of the radial styloid fragment is through the 6–R portal. The previously placed Kirschner wires are then used as joysticks and the fracture is manipulated under direct observation and anatomically reduced to the distal radius (Figures 17.6 and 17.7).

FIGURE 17.5 Lateral view of a fracture dislocation of the distal radius involving the radial styloid.
The guide wires are than advanced across the fracture site once the reduction is judged to be anatomical. It is vital to make a small skin incision over the radial styloid to insert the guide wires through a 14–gauge needle or through a cannula to prevent injury to the dorsal sensory branch of the radial nerve. An alternative technique is utilizing an oscillating drill to insert the guide wires. By use of an oscillating drill, the cutaneous nerves will not wrap around the Kirschner wire as it is being inserted. Once the position of the guide wires is checked under fluoroscopy, a headless cannulated screw may be inserted (Figures 17.8 and 17.9).

FIGURE 17.9 Lateral fluoroscopic view showing the radial styloid fragment and carpus to be anatomically reduced.
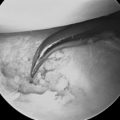
It is important to remember that radial styloid fractures have a high incidence of injury to the scapholunate interosseous ligament18 (Figures 17.10 through 17.12). The zone of injury may pass through the fracture and distally into the scapholunate interosseous ligament. Following arthroscopic reduction to the radial styloid fracture, the arthroscope is placed back in the 3–4 portal to evaluate the integrity of the scapholunate interosseous ligament (Figures 17.13 and 17.14). The arthroscope should also be placed in the radial midcarpal portal to evaluate the scapholunate interval from the midcarpal space. The potential for carpal instability should be thoroughly evaluated from both the radiocarpal and midcarpal spaces. In addition, the occasional loose body may be seen in the midcarpal space, which cannot be detected on plain radiographs. Loose bodies are usually associated with a fracture involving the lunate facet and arise from the hamate.
Three–Part Fractures
Three–part fractures involve a displaced fracture of the radial styloid and lunate facet. The radial styloid fracture may be closed reduced and percutaneously stabilized under fluoroscopic guidance. Again, it is vital to place the guide wires through a small incision to protect the dorsal sensory branch of the radial nerve when stabilizing the radial styloid fragment. The radial styloid fragment is then utilized as a landmark to which the depressed lunate facet fragment is reduced. Following percutaneous reduction and stabilization of the radial styloid fragment under fluoroscopic guidance, the wrist is suspended in the traction tower. The fracture debris and hematoma are then evacuated, and the depressed lunate facet fragment is best observed with the arthroscope in the 3–4 portal. An 18–gauge needle may be placed percutaneously directly over the depressed fragment and viewed arthroscopically as a landmark.
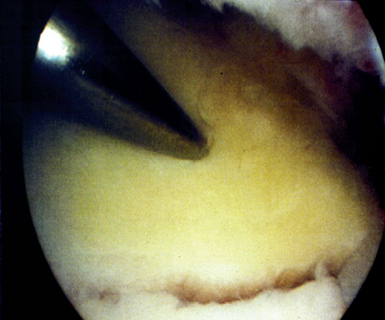
If the articular reduction is not anatomical, the pins may then be removed from the plate and the reduction may be fine–tuned as viewed arthroscopically. Once this reduction is felt to be anatomical, the pins are placed back through the plate to provisionally stabilize the fracture. The most distal screws are then placed through the plate into the distal articular fragment. In die punch fractures, it is particularly helpful to view the reduction while the distal screws are being placed through the plate (Figures 17.15 through 17.17). In this way, the dorsal die punch fragment can be arthroscopically viewed to be anatomical and the can be seen inserting into the fragment for stability (Figures 17.18 and 17.19).
The dorsal die punch fragment is best seen with the scope in the 6–R portal, or through a volar radial portal as promoted by Slutsky. In this instance, a previous volar incision has been made and the arthroscope may be placed between the radioscaphocapitate ligament and the long radiolunate ligament.19 Particularly if any metaphysial comminution is present, plate stabilization is preferred. Volar plate fixation is very stable, and allows for earlier rehabilitation and range of motion.
Four–Part Fractures
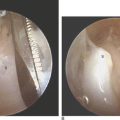
In four–part fractures, the lunate facet is divided into volar and dorsal fragments (Figures 17.20 and 17.21). The volar ulnar fragment is unable to be reduced by closed manipulation. Traction on the volar wrist capsule rotates the volar ulnar fragment, causing it to be unable to be reduced by closed manipulation. The radial styloid fragment is again reduced by closed manipulation and is temporarily stabilized with Kirschner wires. A standard volar approach to the distal radius is performed as described previously. The reduction of the radial styloid fragment may be fine–tuned by direct observation of the fracture fragment and keying it into the shaft of the distal radius.
The volar ulnar fragment is then reduced under direct observation by reducing it back to the shaft and into the radial styloid fragment. It is then pinned provisionally transversely. The position of the reduction of the radial styloid and volar ulnar fragment provisionally stabilized is viewed under fluoroscopy. A volar distal radius plate is then utilized to stabilize the volar bone fragments (Figure 17.22). An initial screw is placed in the proximal portion of the plate to adjust the proximal–distal alignment of the plate in relation to the fracture fragments. The plate is then provisionally pinned to the articular fragments through the holes in the plate.
The wrist is suspended in the traction tower and the arthroscope is placed in the 3–4 portal. Usually, the dorsal ulnar fragment is best viewed with the arthroscope in the 6–R portal or through the volar portal as described by Slutsky. The dorsal ulnar fragment is then percutaneously elevated back to the radial styloid and reduced to the volar ulnar fragment, which is utilized as a landmark (Figures 17.23 through 17.25). The distal screws may be inserted into the plate to stabilize the articular surface (once articular reduction of the distal radius is judged to be anatomical as viewed by the arthroscope). It is helpful that the first screw placed is a non–locking screw, which helps reduce the fragments back through the anatomically shaped distal radius plate. Particularly in small dorsal fragments, it is helpful to view the placement of the screws arthroscopically as they are seen inserted into these fragments to provide stability (Figure 17.26).
Ulnar Styloid Fractures
Stabilization of an associated ulnar styloid fragment is usually controversial. Wrist arthroscopy provides some rationale as to when to stabilize an associate ulnar styloid fragment. Following anatomical reduction of the distal radius fracture, the tension of the articular disc is palpated arthroscopically. The arthroscope is placed in the 3–4 portal, and a probe is inserted through the 6–R portal. If there is good tension to the articular disc, the majority of the fibers of the triangular fibrocartilage complex is still attached to the base of the ulna and the ulnar styloid fragment is not stabilized. If the articular disc is lax by palpation, a peripheral tear of the triangular fibrocartilage complex is suspected. This may be covered with hematoma. It is important to debride the hematoma to obtain direct visualization of the periphery of the articular disc. A peripheral tear is then repaired arthroscopically if it is identified (Figure 17.27). The articular disc is repaired utilizing an outside–in technique to the base of the ulna with suture anchors.
Stabilization of a large ulnar styloid fragment is considered when the articular disc is lax when palpated and no peripheral tear is identified (Figure 17.28). In this incidence, the majority of the fibers of the articular disc is attached to the displaced ulnar styloid fragment. A small incision is then made between the interval of the extensor carpi ulnaris and flexor carpi ulnaris. Blunt dissection is carried down to protect the dorsal sensory branch of the ulnar nerve, which is running just volar to the incision. The ulnar styloid fragment is then cleared of fracture debris, and is stabilized by either tension band, Kirschner wire, or preferably by a small headless cannulated screw.
Discussion
The literature is relatively sparse regarding the results of arthroscopic–assisted fixation of displaced intra–articular fractures of the distal radius. Stewart et al. presented a comparison study of 12 open and 12 arthroscopic–assisted reductions of comminuted fractures of the distal radius.20 These fractures were comminuted and were classified as AO type VII and VIII. In the arthroscopic group, they had five excellent, six good, and one fair result. The open group noted no excellent results. The authors concluded that the arthroscopic group had a significantly increased range of motion compared to the group that underwent open stabilization.
Similarly, Doi et al. reported their results in a comparison study of 38 patients who underwent arthroscopic–assisted fixation in comparison to those patients who underwent open reduction.21 The author similarly found that the arthroscopic group had improved range of motion compared to the open group.
Ruch reported his result of a comparison study of 15 patients who underwent arthroscopic–assisted reduction and 15 patients who underwent closed reduction and were stabilized by external fixation under fluoroscopy.22 In the 15 patients who underwent arthroscopic reduction, 10 patients had a tear of the triangular fibrocartilage complex. Seven of those tears were peripheral and underwent arthroscopic repair. No patients in the arthroscopic group had any signs of distal radioulnar joint instability at final follow–up visit. In the 15 patients who underwent closed reduction and external fixation, four patients continued to complain of instability of the distal radioulnar joint. Potentially, these patients had a peripheral tear of the triangular fibrocartilage complex—which could have been acutely repaired at the time of fracture stabilization.
Geissler and Freeland reviewed their results of 33 patients who underwent arthroscopic–assisted reduction of comminuted intra–articular fractures of the distal radius.23 Their criteria were those fractures displaced 2 mm or more following a closed reduction. In their series, at final follow–up visit 25 patients had an anatomical reduction and eight patients had a 1–mm articular step–off. The patients were evaluated utilizing the modified Mayo wrist score and there were 20 excellent, 10 good, and 3 fair results in their series. Simple articular fractures had a better result compared to complex fracture patterns.
Summary
Associated intra–articular soft–tissue injuries or loose bodies not detected on plain radiographs may be an explanation why some patients continue to complain of pain (particularly on the ulnar side of the wrist) for several months post–injury despite anatomical restoration of the fracture as seen on plain radiographs.24 Last, wrist arthroscopy provides a rationale of when and when not to stabilize the displaced ulnar styloid fragment when it is associated with a fracture of the distal radius.
1 Lafontaine M, Hardy D, Delince P. Stability assessment of distal radius fractures. Injury. 1989;20:208-210.
2 Short WH, Palmer AK, Werner FW, et al. A biomechanical study of distal radial fractures. J Hand Surg. 1987;12A:529-534.
3 Trumble TE, Schmitt SR, Vedder NB. Fractures affecting functional outcome of displaced intra-articular distal radius fractures. J Hand Surg [Am]. 1994;19A:325-340.
4 Geissler WB, Savoie FH. Arthroscopic techniques of the wrist. Mediguide to Orthopedics. 1992;11:1-8.
5 Geissler WB. Intra-articular distal radius fractures: The role of arthroscopy? Hand Clin. 2005;11:407-416.
6 Geissler WB. Arthroscopically assisted reduction of intra-articular fractures of the distal radius. Hand Clin. 1995;11:19-29.
7 Knirk JL, Jupiter JB. Intra-articular fractures of the distal end of the radius in young adults. J Bone Joint Surg. 1986;68A:647-658.
8 Bradway JK, Amadio PC, Cooney WP. Open reduction and internal fixation of displaced comminuted intra-articular fractures of the distal end of the radius. J Bone Joint Surg. 1989;71A:839-847.
9 Fernandez DL, Geissler WB. Treatment of displaced articular fractures of the radius. J Hand Surg. 1991;16:375-384.
10 Edwards CCIII, Harasztic J, McGillivary GR, Gutow AP. Intra-articular distal radius fractures: Arthroscopic assessment of radiographically assisted reduction. J Hand Surg. 2001;26:A1036. A1A41
11 Hixon ML, Fitzrandolph R, McAndrew M, et al. Acute ligamentous tears of the wrist associated with Colles fractures. Proceedings, American Society for Surgery of the Hand, Baltimore, 1989.
12 Fontes D, Lenoble E, DeSomer B, et al. Lesions ligamentaires associus aux fractures distales du radius. Ann Chir Main. 1992;11:119-125.
13 Mohanti RC, Kar N. Study of triangular fibrocartilage of the wrist joint in Colles fracture. Injury. 1979;11:311-324.
14 Geissler WB, Freeland AE, Savoie FH, et al. Carpal instability associated with intra-articular distal radius fractures. Proceedings, American Academy Orthopedic Surgeons Annual Meeting, San Francisco, 1993.
15 Lindau T. Treatment of injuries to the ulnar side of the wrist occurring with distal radial fractures. Hand Clin. 2005;21:417-425.
16 Hanker GJ. Wrist arthroscopy in distal radius fractures. Proceedings, Arthroscopy Association North America Annual Meeting, Albuquerque, NM, 1993.
17 Melone CP. Articular fractures of the distal radius. Orthop Clin North Am. 1984;15:217-235.
18 Mudgal CS, Jones WA. Scapholunate diastasis: A component of fractures of the distal radius. J Hand Surg. 1990;15B:503-505.
19 Levy HJ, Glickel SZ. Arthroscopic assisted internal fixation of intra-articular wrist fractures. Arthroscopy. 1993;9:122-123.
20 Stewart NJ, Berger RA. Comparison study of arthroscopic as open reduction of comminuted distal radius fractures. Presented at the 53rd Annual Meeting of the American Society for Surgery of the Hand [programs and abstracts]. January 11, 1998, Scottsdale, AZ.
21 Doi K, Hatturi T, Otsuka K, Abe T, Tamamoto H. Intra-articular fractures of the distal aspect of the radius arthroscopically assisted reduction compared with open reduction and internal fixation. J Bone Joint Surg. 1999;81A:1093-1110.
22 Ruch DS, Vallee J, Poehling GG, Smith BP, Kuzma GR. Arthroscopic reduction versus fluoroscopic reduction of intra-articular distal radius fractures. Arthroscopy. 2004;20:225-230.
23 Geissler WB, Freeland AE. Arthroscopically assisted reduction of intra-articular distal radial fractures. Clin Orthop. 1996;327:125-134.
24 Hollingworth R, Morris J. The importance of the ulnar side of the wrist in fractures of the distal end of the radius. Injury. 1976;7:223.