3
The Rhythm of the Heart
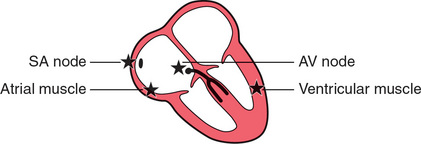
So far we have only considered the spread of depolarization that follows the normal activation of the sinoatrial (SA) node. When depolarization begins in the SA node the heart is said to be in sinus rhythm. Depolarization can, however, begin in other places. Then the rhythm is named after the part of the heart where the depolarization sequence originates, and an ‘arrhythmia’ is said to be present.
When attempting to analyse a cardiac rhythm remember:
• Atrial contraction is associated with the P wave of the ECG.
• Ventricular contraction is associated with the QRS complex.
• Atrial contraction normally precedes ventricular contraction, and there is normally one atrial contraction per ventricular contraction (i.e. there should be as many P waves as there are QRS complexes).
The keys to rhythm abnormalities are:
• The P waves – can you find them? Look for the lead in which they are most obvious.
• The relationship between the P waves and the QRS complexes – there should be one P wave per QRS complex.
• The width of the QRS complexes (should be 120 ms or less).
• Because an arrhythmia should be identified from the lead in which the P waves can be seen most easily, full 12-lead ECGs are better than rhythm strips.
THE INTRINSIC RHYTHMICITY OF THE HEART
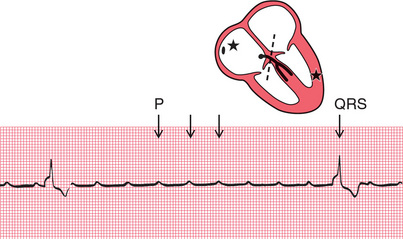
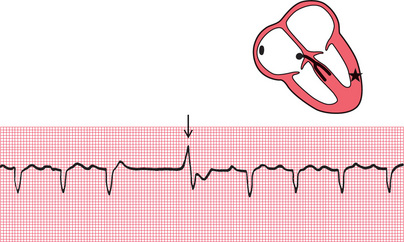
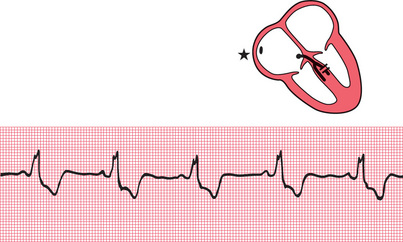
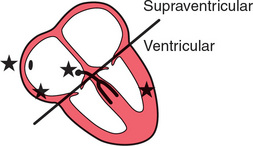
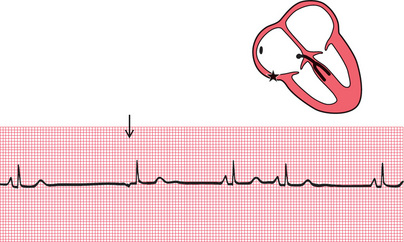
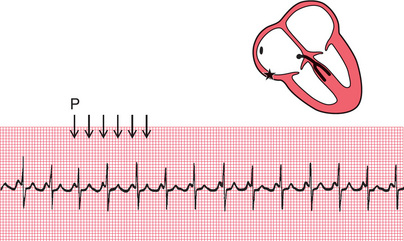
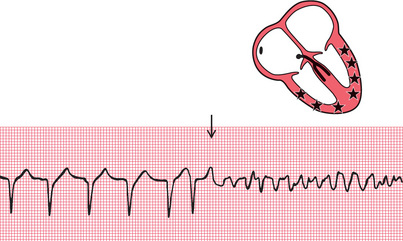
The stars in the figures in this chapter indicate the part of the heart where the activation sequence began. The SA node normally has the highest frequency of discharge. Therefore the rate of contraction of the ventricles will equal the rate of discharge of the SA node. The rate of discharge of the SA node is influenced by the vagus nerves, and also by reflexes originating in the lungs. Changes in heart rate associated with respiration are normally seen in young people, and this is called ‘sinus arrhythmia’ ( Fig. 3.1).

ABNORMAL RHYTHMS
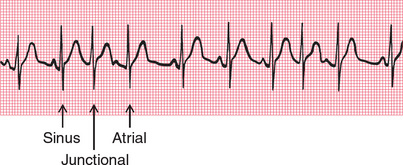
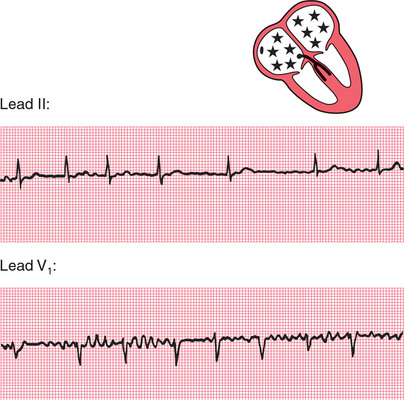
Abnormal cardiac rhythms can begin in one of three places ( Fig. 3.2): the atrial muscle; the region around the atrioventricular (AV) node (this is called ‘nodal’ or, more properly, junctional′); or the ventricular muscle. Although Figure 3.2 suggests that electrical activation might begin at specific points within the atrial and ventricular muscles, abnormal rhythms can begin anywhere within the atria or ventricles.
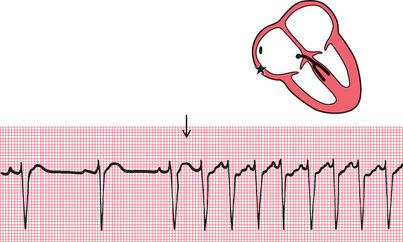
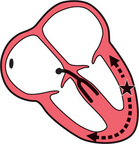
Sinus rhythm, atrial rhythm and junctional rhythm together constitute the ‘supraventricular’ rhythms ( Fig. 3.3). In the supraventricular rhythms, the depolarization wave spreads to the ventricles in the normal way via the His bundle and its branches ( Fig. 3.4). The QRS complex is therefore normal, and is the same whether depolarization was initiated by the SA node, the atrial muscle, or the junctional region.
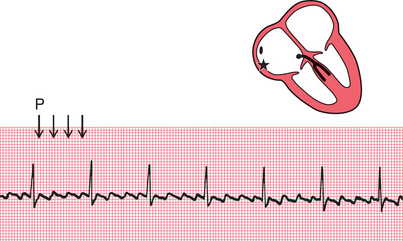
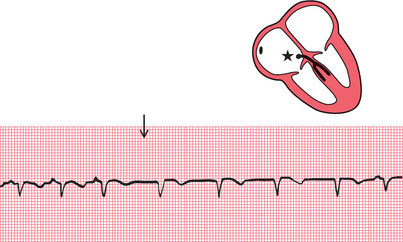
In ventricular rhythms, on the other hand, the depolarization wave spreads through the ventricles by an abnormal and slower pathway, via the Purkinje fibres ( Fig. 3.5). The QRS complex is therefore wide and is abnormally shaped. Repolarization is also abnormal, so the T wave is also of abnormal shape. Remember:
• Supraventricular rhythms have narrow QRS complexes.
• Ventricular rhythms have wide QRS complexes.
• The only exception to this rule occurs when there is a supraventricular rhythm with right or left bundle branch block, or the Wolff-Parkinson-White (WPW) syndrome, when the QRS complex will be wide (see p. 79).
THE BRADYCARDIAS – THE SLOW RHYTHMS
It is clearly advantageous if different parts of the heart are able to initiate the depolarization sequence, because this gives the heart a series of failsafe mechanisms that will keep it going if the SA node fails to depolarize, or if conduction of the depolarization wave is blocked. However, the protective mechanisms must normally be inactive if competition between normal and abnormal sites of spontaneous depolarization is to be avoided. This is achieved by the secondary sites having a lower intrinsic frequency of depolarization than the SA node.
ATRIAL ESCAPE
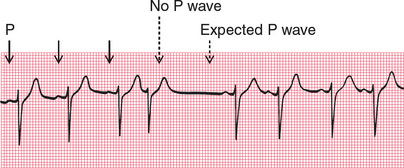
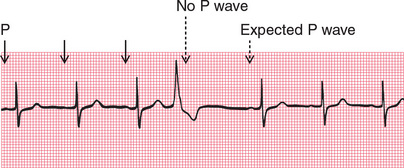
If the rate of depolarization of the SA node slows down and a different focus in the atrium takes over control of the heart, the rhythm is described as ‘atrial escape’ ( Fig. 3.6). Atrial escape beats can occur singly.
NODAL (JUNCTIONAL) ESCAPE
If the region around the AV node takes over as the focus of depolarization, the rhythm is called ‘nodal’, or more properly, ‘junctional’ escape ( Fig. 3.7).
VENTRICULAR ESCAPE
‘Ventricular escape’ is most commonly seen when conduction between the atria and ventricles is interrupted by complete heart block ( Fig. 3.8).
Ventricular escape rhythms can occur without complete heart block, and ventricular escape beats can be single ( Fig. 3.9).
The rhythm of the heart can occasionally be controlled by a ventricular focus with an intrinsic frequency of discharge faster than that seen in complete heart block. This rhythm is called ‘accelerated idioventricular rhythm’ ( Fig. 3.10), and is often associated with acute myocardial infarction. Although the appearance of the ECG is similar to that of ventricular tachycardia (described later), accelerated idioventricular rhythm is benign and should not be treated. Ventricular tachycardia should not be diagnosed unless the heart rate exceeds 120/min.
EXTRASYSTOLES
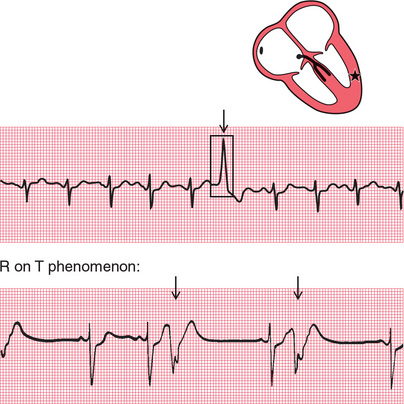
Any part of the heart can depolarize earlier than it should, and the accompanying heartbeat is called an extrasystole. The term ‘ectopic’ is sometimes used to indicate that depolarization originated in an abnormal location, and the term ‘premature contraction’ means the same thing.
Atrial extrasystoles have abnormal P waves ( Fig. 3.11). In a junctional extrasystole there is no P wave at all, or the P wave appears immediately before or immediately after the QRS complex ( Fig. 3.11). The QRS complexes of atrial and junctional extrasystoles are, of course, the same as those of sinus rhythm.
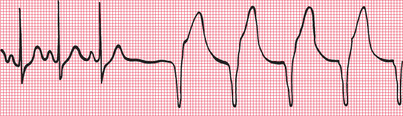
Ventricular extrasystoles, however, have abnormal QRS complexes, which are typically wide and can be of almost any shape ( Fig. 3.12).
It may, however, not be as easy as this, particularly if a beat of supraventricular origin is conducted abnormally to the ventricles (bundle branch block, see Ch. 2). It is advisable to get into the habit of asking five questions every time an ECG is being analysed:
1. Does an early QRS complex follow an early P wave? If so, it must be an atrial extrasystole.
2. Can a P wave be seen anywhere? A junctional extrasystole may cause the appearance of a P wave very close to, and even after, the QRS complex because excitation is conducted both to the atria and to the ventricles.
3. Is the QRS complex the same shape throughout (i.e. has it the same initial direction of deflection as the normal beat, and has it the same duration)? Supraventricular beats look the same as each other; ventricular beats may look different from each other.
4. Is the T wave the same way up as in the normal beat? In supraventricular beats, it is the same way up; in ventricular beats, it is inverted.
5. Does the next P wave after the extrasystole appear at an expected time? In both supraventricular and ventricular extrasystoles there is a (‘compensatory’) pause before the next heartbeat, but a supraventricular extrasystole usually upsets the normal periodicity of the SA node, so that the next SA node discharge (and P wave) comes late.
THE TACHYCARDIAS – THE FAST RHYTHMS
SUPRAVENTRICULAR TACHYCARDIAS
Atrial tachycardia (abnormal focus in the atrium)
In atrial tachycardia, the atria depolarize faster than 150/min ( Fig. 3.15).
The AV node cannot conduct atrial rates of discharge greater than about 200/min. If the atrial rate is faster than this, ‘atrioventricular block’ occurs, with some P waves not followed by QRS complexes. The difference between this sort of atrioventricular block and second degree heart block is that in atrioventricular block associated with tachycardia the AV node is functioning properly – it is preventing the ventricles from being activated at a fast (and therefore inefficient) rate. In first, second or third degree block associated with sinus rhythm, the AV node and/or the His bundle are not conducting normally.
Atrial flutter
When the atrial rate is greater than 250/min, and there is no flat baseline between the P waves, ‘atrial flutter’ is present ( Fig. 3.16).
When atrial tachycardia or atrial flutter is associated with 2:1 block, you need to look carefully to recognize the extra P waves ( Fig. 3.17). A narrow complex tachycardia with a ventricular rate of about 125-150/min should always alert you to the possibility of atrial flutter with 2:1 block.
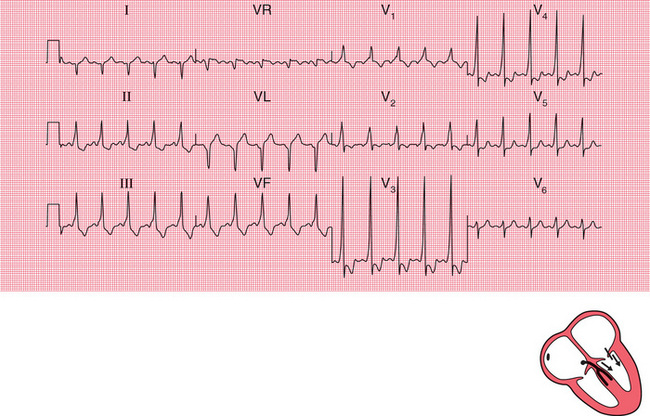
Any arrhythmia should be identified from the lead in which P waves can most easily be seen. In the record in Figure 3.18, atrial flutter is most easily seen in lead II, but it is also obvious in leads VR and VF.
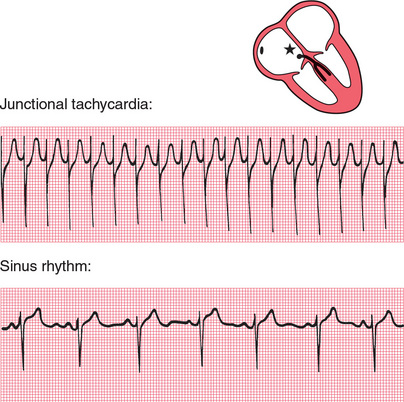
Junctional (nodal) tachycardia
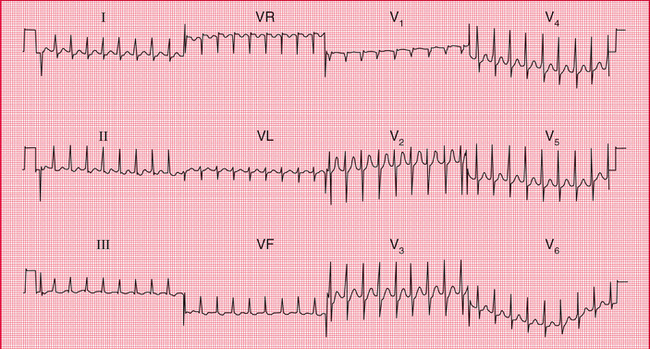
If the area around the AV node depolarizes frequently, the P waves may be seen very close to the QRS complexes, or may not be seen at all ( Fig. 3.19). The QRS complex is of normal shape because, as with the other supraventricular arrhythmias, the ventricles are activated via the His bundle in the normal way.
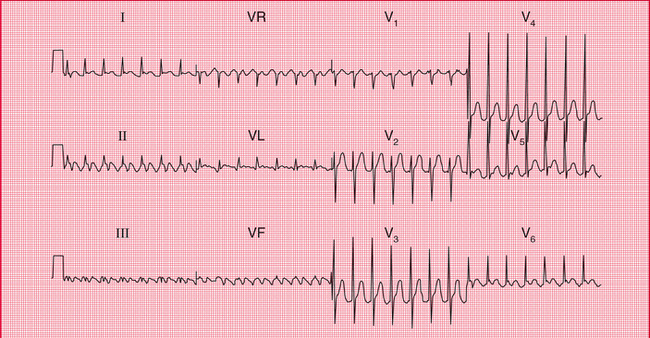
The 12-lead ECG in Figure 3.20 shows that in junctional tachycardia no P waves can be seen in any lead.
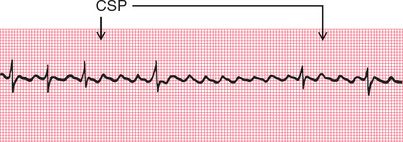
Carotid sinus pressure
Carotid sinus pressure may have a useful therapeutic effect on supraventricular tachycardias, and is always worth trying because it may make the nature of the arrhythmia more obvious ( Fig. 3.21). Carotid sinus pressure activates a reflex that leads to vagal stimulation of the SA and AV nodes. This causes a reduction in the frequency of discharge of the SA node, and an increase in the delay of conduction in the AV node. It is the latter which is important in the diagnosis and treatment of arrhythmias. Carotid sinus pressure completely abolishes some supraventricular arrhythmias, and slows the ventricular rate in others, but it has no effect on ventricular arrhythmias.
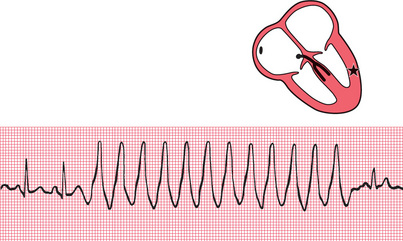
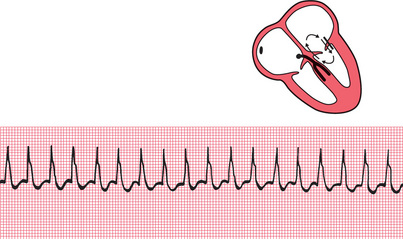
VENTRICULAR TACHYCARDIAS
If a focus in the ventricular muscle depolarizes with a high frequency (causing, in effect, rapidly repeated ventricular extrasystoles), the rhythm is called ‘ventricular tachycardia’ ( Fig. 3.22).
Wide and abnormal complexes are seen in all 12 leads of the standard ECG ( Fig. 3.23).
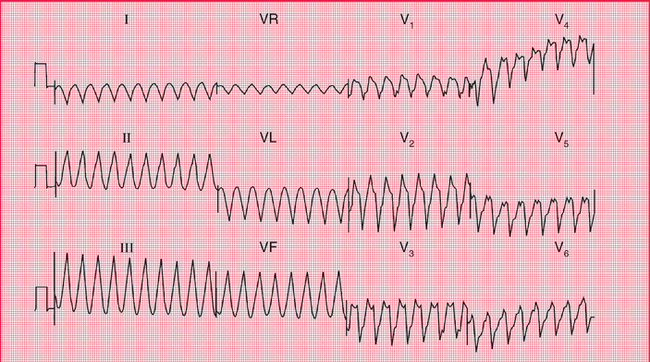
Remember that wide and abnormal complexes are also seen with bundle branch block ( Fig. 3.24).
HOW TO DISTINGUISH BETWEEN VENTRICULAR TACHYCARDIA AND SUPRAVENTRICULAR TACHYCARDIA WITH BUNDLE BRANCH BLOCK
It is essential to remember that the patient′s clinical state – whether good or bad – does not help to differentiate between the two possible causes of a tachycardia with broad QRS complexes. If a patient with an acute myocardial infarction has broad complex tachycardia it will almost always be ventricular tachycardia. However, a patient with episodes of broad complex tachycardia but without an infarction could have ventricular tachycardia, or supraventricular tachycardia with bundle branch block or the Wolff-Parkinson-White syndrome (see p. 79). Under such circumstances the following points may be helpful:
1. Finding P waves and seeing how they relate to the QRS complexes is always the key to identifying arrhythmias. Always look carefully at a full 12-lead ECG.
2. If possible, compare the QRS complex during the tachycardia with that during sinus rhythm. If the patient has bundle branch block when in sinus rhythm, the QRS complex during the tachycardia will have the same shape as during normal rhythm.
3. If the QRS complex is wider than four small squares (160 ms), the rhythm will probably be ventricular in origin.
4. Left axis deviation during the tachycardia usually indicates a ventricular origin, as does any change of axis compared with a record taken during sinus rhythm.
5. If during the tachycardia the QRS complex is very irregular, the rhythm is probably atrial fibrillation with bundle branch block (see below).
FIBRILLATION
ATRIAL FIBRILLATION
When the atrial muscle fibres contract independently there are no P waves on the ECG, only an irregular line ( Fig. 3.25). At times there may be flutter-like waves for 2–3 s. The AV node is continuously bombarded with depolarization waves of varying strength, and depolarization spreads at irregular intervals down the His bundle. The AV node conducts in an ‘all or none’ fashion, so that the depolarization waves passing into the His bundle are of constant intensity. However, these waves are irregular, and the ventricles therefore contract irregularly. Because conduction into and through the ventricles is by the normal route, each QRS complex is of normal shape.
In a 12-lead record, fibrillation waves can often be seen much better in some leads than in others ( Fig. 3.26).
THE WOLFF-PARKINSON-WHITE (WPW) SYNDROME
The only normal electrical connection between the atria and ventricles is the His bundle. Some people, however, have an extra or ‘accessory’ conducting bundle, a condition known as the Wolff-Parkinson-White syndrome. The accessory bundles form a direct connection between the atrium and the ventricle, usually on the left side of the heart, and in these bundles there is no AV node to delay conduction. A depolarization wave therefore reaches the ventricle early, and ‘pre-excitation’ occurs. The PR interval is short, and the QRS complex shows an early slurred upstroke called a ‘delta wave’ ( Fig. 3.28). The second part of the QRS complex is normal, as conduction through the His bundle catches up with the pre-excitation. The effects of the WPW syndrome on the ECG are considered in more detail in Chapter 7.
The only clinical importance of this anatomical abnormality is that it can cause paroxysmal tachycardia. Depolarization can spread down the His bundle and back up the accessory pathway, and so reactivate the atrium. A ‘re-entry’ circuit is thus set up, and a sustained tachycardia occurs ( Fig. 3.29).
WHATTO DO
Accurate interpretation of the ECG is an essential part of arrhythmia management. Although this book is not intended to discuss therapy in detail, it seems appropriate to outline some simple approaches to patient management that logically follow interpretation of an ECG recording:
1. For fast or slow sinus rhythm, treat the underlying cause, not the rhythm itself.
2. Extrasystoles rarely need treatment.
3. In patients with acute heart failure or low blood pressure due to tachycardia, DC cardioversion should be considered early on.
4. Patients with any bradycardia that is affecting the circulation can be treated with atropine, but if this is ineffective they will need temporary or permanent pacing ( Fig. 3.30).

5. The first treatment for any abnormal tachycardia is carotid sinus pressure. This should be performed with the ECG running, and may help make the diagnosis:
− Sinus tachycardia: carotid sinus pressure causes temporary slowing of the heart rate.
− Atrial and junctional tachycardia: carotid sinus pressure may terminate the arrhythmia or may have no effect.
− Atrial flutter: carotid sinus pressure usually causes a temporary increase in block (e.g. from 2:1 to 3:1).
− Atrial fibrillation and ventricular tachycardia: carotid sinus pressure has no effect.
6. Narrow complex tachycardias should be treated initially with adenosine.
7. Wide complex tachycardias should be treated initially with lidocaine.
 For more on pacemakers, see pp. 187-207
For more on pacemakers, see pp. 187-207
REMINDERS
ABNORMAL CARDIAC RHYTHMS
• Most parts of the heart are capable of spontaneous depolarization.
• Abnormal rhythms can arise in the atrial muscle, the region around the AV node (the junctional region) and in the ventricular muscle.
• Escape rhythms are slow and are protective.
• Occasional early depolarization of any part of the heart causes an extrasystole.
• Frequent depolarization of any part of the heart causes tachycardia.
• Asynchronous contraction of muscle fibres in the atria or ventricles is called fibrillation.
• Apart from the rate, the ECG patterns of an escape rhythm, an extrasystole and a tachycardia arising in any one part of the heart are the same.
• All supraventricular rhythms have normal QRS complexes, provided there is no bundle branch block or pre-excitation (WPW) syndrome.
• Ventricular rhythms cause wide and abnormal QRS complexes, and abnormal T waves.
THE IDENTIFICATION OF RHYTHM ABNORMALITIES
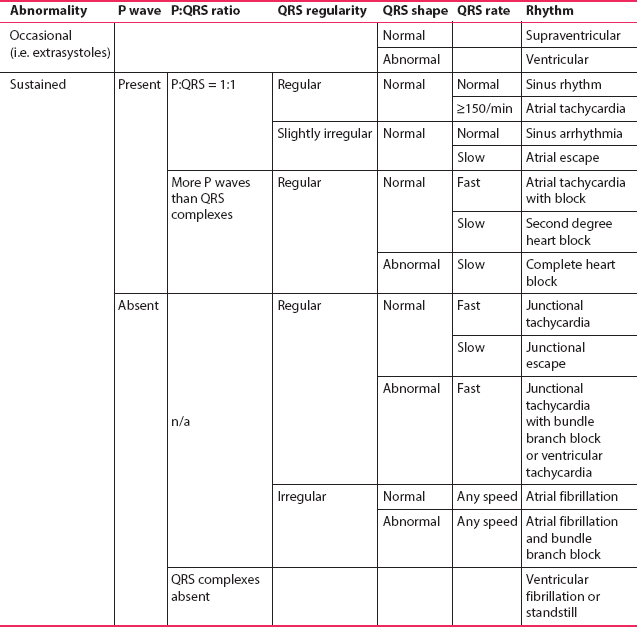
Recognizing ECG abnormalities is to a large extent like recognizing an elephant – once seen, never forgotten. However, in cases of difficulty it is helpful to ask the following questions, referring to Table 3.1:
1. Is the abnormality occasional or sustained?
3. Are there as many QRS complexes as P waves?
4. Are the ventricles contracting regularly or irregularly?
 For more on tachycardias, see pp. 113-147
For more on tachycardias, see pp. 113-147


 For more on broad complex tachycardias, see p. 126
For more on broad complex tachycardias, see p. 126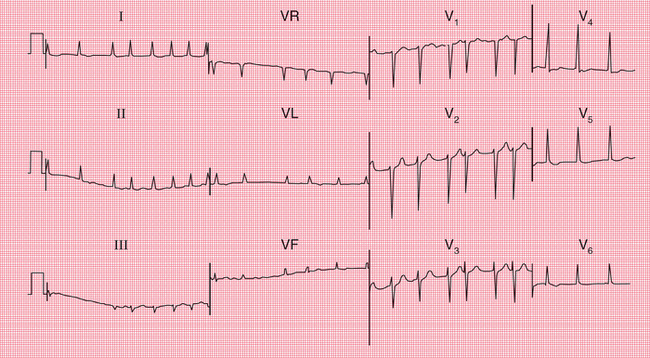
 For more on WPW syndrome, see pp. 69-72
For more on WPW syndrome, see pp. 69-72