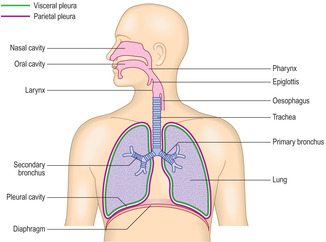
The function of the respiratory system is to transport gases between the atmosphere and sites in the lungs where gaseous exchange between air and blood occurs. Oxygen diffuses into blood in capillaries in the lungs and carbon dioxide is released from the blood. The respiratory system consists of a series of air-filled passages connecting the nose and mouth to the two lungs in the thorax (Fig. 11.1). Two categories of passages are described, the upper and the lower respiratory tracts. The structure of the walls of the passages of the upper respiratory tract ensures that they do not collapse during breathing. The structure of the walls of the lower respiratory tract ensures that efficient gaseous exchange occurs across a barrier which is 0.1–1.5μm thick. It is also essential that the passages in the lower respiratory tract do not collapse during respiration.
The respiratory system
Whilst the respiratory passages conduct gases through the respiratory system, there are other related structures that help propel the gases along the passages. Each lung is enclosed by a pleural sac formed by a serosal membrane (Fig. 11.1). The visceral layer of the pleura is firmly attached to the surface of each lung and the parietal layer to the inner surface of the chest wall. The pleural cavity (the space enclosed by the pleura) contains fluid secreted by the serosal cells and the lungs are thus able to move during respiration in a relatively friction-free environment. The pleural cavity has an important role in breathing as the pressure in the cavity is less than atmospheric pressure. As the thoracic boundaries (the ribs, intercostal muscles and diaphragm) move during breathing the pleural membranes and lungs move with them. Inspiration increases intrathoracic volume (and the negative pressure in the pleural cavities) and draws air into the lungs. Expiration occurs as the thoracic boundaries decrease intrathoracic volume and stretched elastin fibres in the lung (see below) recoil.
The upper respiratory tract comprises passages and tubes of decreasing diameter which connect the nose and mouth to the lower respiratory tract in the lungs. From the exterior inwards, the upper respiratory tract comprises the nasal cavity, nasopharynx, larynx, trachea, bronchi and some bronchioles. These passages are also known collectively as the conducting portion of the respiratory tract as they conduct air to the sites of gaseous exchange in the lungs.
During inspiration the upper respiratory passages are under increasing negative pressure as the intrathoracic volume increases. Air will be drawn into the lungs only if the walls of these passages do not collapse. The larger passages have bone or cartilage in their walls which make them relatively rigid and ensure that they remain patent during inspiration. The smallest passages within the lungs, the bronchioles, do not have bone or cartilage in their walls. Bronchioles are held open during inspiration as elastin connective tissue fibres attached to the outer surface of their walls are stretched as a result of the thoracic volume increasing during inspiration.
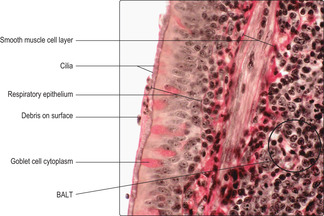
Most of the upper respiratory tract is lined by a mucosa which consists of a respiratory epithelium and a lamina propria which supports numerous blood vessels. In some regions submucosal connective tissue and aggregations of lymphoid cells are also present. The respiratory epithelium is described as pseudostratified with ciliated columnar epithelial cells and goblet cells (Fig. 11.2). The goblet cells secrete mucus onto the surface of the epithelium and this traps particulate matter which may be harmful. Importantly, the beating motion of cilia of columnar epithelial cells moves the mucus so that it is swallowed or discharged from the nose or the mouth. In addition, moisture on the surface of the respiratory epithelium, provided by mucus, humidifies inspired air. This prevents dehydration of the cells lining the lower respiratory tract where gases have to enter an aqueous phase to allow exchange between air and blood. The respiratory epithelium also contains stem cells which can replace damaged goblet and ciliated epithelial cells and replace themselves. Neuroendocrine cells are also present which secrete molecules (paracrine hormones) that regulate the local environment.
Specialised epithelial cells involved in detecting smells, olfactory epithelial cells, lie in the uppermost parts of the nasal cavity. Thus, sniffing odours into the upper part of the nasal cavity is the most efficient way of detecting smells.
Lying adjacent to the nasal cavity are paranasal sinuses. They are four paired structures (the maxillary, frontal, sphenoid and ethmoid sinuses) which open into the nasal cavity. These sinuses are air-filled spaces in skull bones which are lined by respiratory epithelium. The function of the sinuses is unclear, though it may be related to insulating the brain from the effects of inspiring cold air. Other suggested functions include giving resonance to the voice, lightening the weight of the skull and adding to the ability of the upper respiratory tract to ‘air condition’ (warm and moisten) inhaled air.
In the nasal cavities and the sinuses the mucosa and associated blood vessels are firmly attached to underlying bone or cartilage, and the rigidity conferred by such attachments means that inspiration does not collapse the air passages in these regions.
The nasopharynx and the oropharynx are contiguous parts of the pharynx (a large passage shared by the respiratory and the digestive systems). The nasopharynx, which is traversed by air, is lined by respiratory epithelium, but the oropharynx, which carries food (and drink and air) from the mouth, is lined by a stratified squamous epithelium which is able to resist the ‘wear and tear’ caused by the passage of food.
Aggregations of lymphocytes are a prominent feature deep to the epithelium lining the nasopharynx, particularly on its posterior wall where they form the nasopharyngeal tonsils (adenoids). These aggregations form part of a ring of lymphoid cells (Waldeyer’s ring) around the pharynx. Inhaled and ingested antigenic material (e.g. bacteria and viruses) may be trapped in this region and immune responses mounted, thus protecting the respiratory and gastrointestinal tracts from infection.
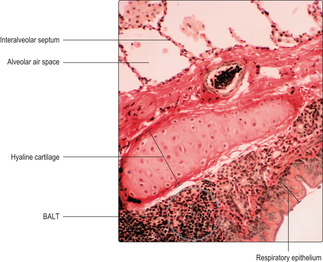
Inspired air passes from the nasopharynx into the larynx and then into the trachea. The larynx has walls containing hyaline cartilage which maintain the patency of the airway, and most of the lumen of the larynx is lined by respiratory epithelium. However, there are flaps (the vocal folds) extending from the walls of the larynx into the lumen which are covered by a stratified squamous epithelium. Vocal cords vibrate and produce sounds and the stratified squamous epithelium resists the wear and tear resulting from the vibrations.
During swallowing, the entry to the larynx from the pharynx is closed temporarily by a large flap-like structure, the epiglottis. This arrangement prevents ingested food and liquid entering the trachea and producing coughing and choking. The stratified squamous epithelium covering the anterior surface of the epiglottis is continuous with the dorsal surface of the tongue and, as it is in contact with food during swallowing is subject to abrasion. In contrast, the posterior surface of the epiglottis is exposed only to air and is covered by respiratory epithelium. The flexibility and recoil movements of the epiglottis during swallowing are aided by its core of elastic cartilage (see Fig. 9.1).
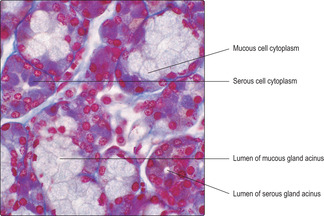
The trachea is a tube attached to the larynx in the neck and it extends about 10cm into the thorax. It is 2–3cm in diameter and is kept patent by 15 to 20 incomplete ‘C’-shaped rings of hyaline cartilage in its wall (Fig. 11.3). Each ring of cartilage is completed on the posterior wall of the trachea by smooth muscle and connective tissue containing elastin fibres. The trachea is lined by respiratory epithelium (Fig. 11.3) and there are serous and mucous glands (Fig. 11.4) in submucosal connective tissue. Secretions from the submucosal glands and goblet cells in the epithelium are propelled by ciliary activity toward the pharynx and are usually swallowed.
The trachea bifurcates into two main (primary) bronchi (Fig. 11.1). These enter the lungs and divide into lobar (secondary) bronchi. Each of these subdivides about 10 times into segmental (tertiary) bronchi which supply specific areas of lung known as bronchopulmonary segments. Each of these segments of lung has its own branch of a pulmonary artery as well as a single tertiary bronchus, and each has clinical significance. For example, knowledge of the architecture of bronchopulmonary segments is vital in bronchoscopy. In addition, a disease may be confined to one segment of lung and surgical resection may be used to remove the diseased segment. Further branching of bronchi in segments reduces their diameter to 5mm and, at this dimension, branching continues but the passages are then known as bronchioles.
All bronchi contain hyaline cartilage in their walls which maintains their patency. Primary bronchi have, like the trachea, incomplete rings of cartilage in their walls. Intrapulmonary branches of bronchi have irregularly placed plates of cartilage in their walls (Fig. 11.5). Large bronchi are lined by respiratory epithelium (Fig. 11.5), but as they become smaller in diameter gradual changes occur in the epithelium (see below). The submucosal layer of bronchi contains serous and mucous glands which secrete onto the epithelial surface (Fig. 11.6). Secretions on the epithelial surface are moved up the ‘mucus escalator’ to the pharynx by ciliary activity of the columnar epithelial cells. Smooth muscle (Figs 11.2 and 11.6) is also present in the walls of bronchi and the muscle cells are arranged spirally along the length of the walls. Parasympathetic stimulation of this smooth muscle causes contraction which reduces the diameter of the lumen. Conversely, sympathetic nerve stimulation relaxes the muscle and increases the diameter of the airway. The strength of muscle contraction is not great enough to collapse the bronchi because of the relatively rigid cartilage lying outside the muscle layer. Aggregations of lymphocytes are a common feature in the walls of bronchi (Figs 11.2 and 11.5) and are described as ‘bronchus-associated lymphoid tissue’ (BALT). In these regions, interactions between macrophages and lymphocytes take place which are important in immune defence of the lungs.
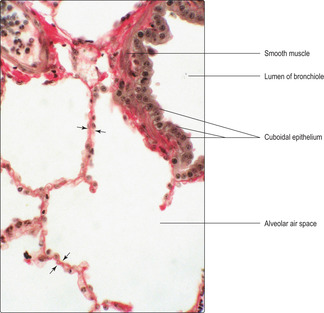
Bronchioles, passages of less than 5mm in diameter, do not have cartilage in their walls but have smooth muscle (Fig. 11.7). The patency of bronchioles during inspiration is assisted not by cartilage in their walls but by elastin fibres in surrounding connective tissue attached to the bronchioles which are stretched as the thoracic volume is increased during inspiration and air is drawn into the respiratory tract.
As the conducting tubes of the respiratory system reduce in calibre, the type of lining epithelium gradually changes. Instead of the typical respiratory epithelium (pseudostratified, ciliated columnar, with goblet cells) as in the larger bronchi (Figs 11.2, 11.5 and 11.6), they become lined by a simple epithelium. Most bronchioles are lined by a simple epithelium consisting of ciliated columnar cells and a few goblet cells. Smaller divisions of bronchioles are lined by ciliated low columnar or cuboidal cells (Fig. 11.7); goblet cells are not present in the smaller bronchioles. In terminal bronchioles the epithelium may become flattened taking on a squamous appearance (Fig. 11.8). There are also specialised cells (Clara cells) in the epithelium lining the smallest bronchioles which may serve a protective function. (Clara cells are prominent in some non-human species.)
There are no submucous glands in bronchioles and very few goblet cells. If such glands and goblet cells were present, it could lead to too much fluid in the bronchioles which may drain into and ‘drown’ the gaseous exchange region of the lower respiratory tract.
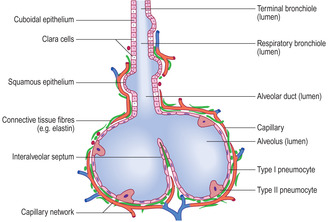
The most distal, lower part of the respiratory tract is also described as the respiratory portion of the tract as it is here that gaseous exchange between air and blood occurs. The walls of the passages are at their thinnest and this facilitates the exchange of gases. Terminal bronchioles continue as respiratory bronchioles. In some parts of respiratory bronchioles the epithelium is simple cuboidal, but in other parts squamous epithelial cells are present and gaseous exchange occurs across the cells in these regions.
Respiratory bronchioles open into alveolar ducts, which in turn lead to several alveoli (Fig. 11.8). Some alveoli are adjacent to each other and share their walls. These walls are known as interalveolar septa (Fig. 11.5, Fig. 11.6, Fig. 11.7 and Fig. 11.8). There are several hundred million alveoli per lung offering an enormous surface area where gaseous exchange occurs.
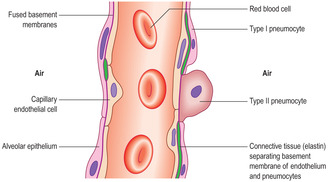
The epithelium lining alveoli lies very close to a capillary network and it is across this air–blood barrier that gases, in the aqueous phase, diffuse. The barrier between air and blood is very thin (Figs 11.6 and 11.7) and consists of (Fig. 11.9):
■ an alveolar epithelium and its basement membrane
■ connective tissue (sparse)
■ a capillary endothelium and its basement membrane.
The alveolar epithelium comprises type I and type II pneumocytes. Type I pneumocytes make up the majority of the surface of alveoli and their cytoplasm forms a very thin layer closely applied to the basement membrane: this aids the diffusion of gases. Type II pneumocytes are roughly spherical cells which synthesise and secrete a surfactant (a lipid material with detergent-like qualities) which reduces surface tension in the alveoli. During inspiration this low surface tension makes it easier to draw air into the alveoli and helps to prevent the alveoli from collapsing.
The connective tissue around alveoli is sparse (Figs 11.6 and 11.7) and consists mainly of elastin fibres, although a little collagen is present. The elastin fibres are stretched on inspiration and this helps to draw air into the alveoli. Importantly, recoil of the elastin during expiration helps to expel air from the alveoli. In some regions there is no connective tissue and the basement membranes of an alveolar epithelium and the adjacent capillary endothelium are fused, thus reducing the distance gases have to travel between air and blood (Fig. 11.9).
Throughout the lungs a variety of immune cells are present. These include cells which phagocytose particulate matter, including bacteria, and others which mount immune responses to foreign molecules. Lying on the alveoli, on the air side or apparently lying free within the air space, are alveolar macrophages. These cells are also present within interalveolar septa. Some macrophages may migrate onto the surface of the epithelium and others may remain in the lungs throughout life. Macrophages are particularly apparent if they have ingested inert particles such as carbon and this can give lungs a black appearance at post-mortem examination.
Smoking Goblet cells increase in number and ciliated cells decrease in number in smokers. One consequence is mucus is not cleared readily from the respiratory passages. Coughing may help clear the passages and prevent mucus from reaching the alveoli and decreasing the efficiency of gaseous exchange. Smoking is associated with an increased risk of heart disease and lung cancer.
Asthma In this condition the airways are abnormally constricted by contraction of the smooth muscle, particularly in the bronchioles. It is often a consequence of immune (allergic) reactions. In asthmatics the airways are inflamed and produce excessive amounts of mucus. Attacks are usually acute episodes of wheezing, coughing and difficulty in breathing. These episodes may be effectively treated with inhalers containing drugs which dilate the airways, and steroid-based drugs which reduce the inflammation.
Cystic fibrosis This is an inherited condition in which excessive amounts of viscous mucus are produced. It is often thought of as a purely respiratory disorder but it is a disorder of exocrine glands. The excess secretions of the exocrine glands cause obstruction in the lungs and a range of other organs such as the pancreas, liver and intestines. The disease pursues a chronic course and sufferers rarely live beyond their third decade.
■ The respiratory system consists of the lungs and a series of passages carrying air to them:
■ the upper respiratory tract passages transport air to and from the lower respiratory tract, where exchange of gases (oxygen and carbon dioxide) between blood and air occurs.
■ The chest wall, diaphragm and pleural membranes around the lungs are involved in moving air in and out of the lungs (during inspiration and expiration).
■ The walls of the trachea and bronchi contain hyaline cartilage which provides rigidity and prevents the passages collapsing during inspiration:
■ all these passage are lined by the typical respiratory epithelium.
■ The walls of bronchioles do not contain cartilage and they are kept open during inspiration as elastin fibres attached to their walls are stretched:
■ the respiratory epithelium is gradually replaced in bronchioles by a simple columnar or cuboidal (non-ciliated) epithelium.
■ Smooth muscle is present in the walls of bronchi and bronchioles and is controlled by autonomic nerves.
■ The walls of the lower respiratory tract are extremely thin and gaseous exchange occurs mostly in alveoli.
■ The blood–air barrier in alveoli comprises:
■ endothelial cells and their basement membrane, sparse elastin fibres, alveolar epithelial cells and their basement membrane
■ alveolar epithelium is formed mostly by very flattened cells (type I pneumocytes), and some type II pneumocytes which are rounded and secrete surfactant.
■ Aggregations of immune cells are present in the walls of the respiratory tract and macrophages are present in alveolar walls and on the surface of the alveolar epithelium.