Chapter contents
2.1 The circulatory system 5
2.2 The pulse 6
2.3 Blood 10
2.4 Summary 13
2.5 The pulse in biomedicine 13
2.6 The pulse in contemporary CM clinical practice 17
This chapter introduces the concepts of blood flow and pressure waves, and looks at the radial artery and its essential features, and its relationship to pulse diagnosis. The chapter is intended as a brief summary of a complex and diverse body of literature that is available on the topic, and is presented here to support further discussions on CM pulse diagnosis presented later in this book. It should not be considered definitive but may be used as a basis for further investigations into understanding the physiological basis of the pulse from other literature sources.
2.1. The circulatory system
The circulatory system functions as a transportation system. It distributes the nutrients and substances required for healthy metabolism to tissue cells and organs while removing metabolic waste from those same cells and organs. According to Berne & Levy (1981: p. 1) the components of the circulatory system can in their simplest form be reduced to a pump moving fluids through a distributing network of tubes. Yet this analogy of the circulatory system is overly simplistic when the circulatory system is considered within the context of health. Rather than the passive distributing network implied in the analogy, it is actually a dynamic regulatory system assisting in the maintaining body temperature; regulate volume flow of blood; and act as a communication network between different body regions. These functions of the circulatory system depend on controlled changes in the width of blood vessels (vasoconstriction and vasodilatation) and the pump-like action of the heart to cause blood flow. These functions are all mediated through an innate biofeedback system which helps maintain homeostasis and organ function. For example, by reducing the blood vessel diameter (vasoconstriction), the surface area of the blood vessel exposed to the environment also decreases and body heat is retained while concurrently reducing blood flow to the superficial and peripheral regions of the body. Increasing blood vessel diameter (vasodilatation) increases the surface area of the blood vessel, thus increasing the rate at which body heat is lost to the environment. The supply of nutrients circulating to the tissue cells is regulated by this same vasodilatation/vasoconstriction mechanism. Chemical transmitters, hormones and other chemical markers produced by the body and required for regulating homeostasis are similarly distributed in this manner.
The body’s organs and tissues have varying nutritional and blood flow requirements for their health and normal functioning. Such requirements also vary depending on the time of day and level of activity. This is reflected in the differing density and type of blood vessels found in different regions of the body. For example, the skin has small requirements for copious blood flow and so the capillary network is fine but densely distributed; useful in times of tissue repair due to trauma or for dispersing body heat during exercise. On the other hand, the brain has a high and constant requirement for blood flow and several large arteries serve this purpose by maintaining a continuous supply of blood flow to the organ, while the lungs are rich in small capillary beds to assist in the transfer of metabolic waste for oxygen. Similarly, other organs vary in both the density of blood vessels present and anatomical structure of the vessels depending on function and purpose. The kidneys in particular have a unique circulation, using specialised arterial structures to increase partial blood pressures to filter toxins from the blood.
These concentrations of blood vessels that serve such a specialised function can be termed a microcirculation. Berne & Levy have noted that some chemicals, whether intrinsic or introduced by therapeutic interventions, may have differing affects on the microcirculation and on arterial smooth muscle:
In studies on this interesting and important type of muscle, great care should be taken in extrapolating results from one tissue to another or from the same tissue under different physiological conditions. For example, some agents elicit vasodilation in some vascular beds and vasoconstriction in others (1981: p. 124).
In the context of health assessment, it is logical to conclude that dysfunction or increased demands on an organ, whether in response to neural, hormonal or chemical stimulus, should mean that the circulatory requirements, and hence the microcirculation of that organ, would be affected.
Extrapolating about Chinese medical ideas then, it is not inconceivable to link such microcirculatory changes posited by Berne and Levy to Chinese medical ideas on pulse diagnosis. In this sense, it can be that such microcirculatory changes when applying CM theory, are detectable elsewhere in the body, and in particular in the radial artery, via signals carried in the haemodynamic pulse wave. Dai et al (1985) hypothesised and demonstrated that disturbances in the arterial blood flow in one region of the body can be detected elsewhere in the body using the arterial pulse wave. They did this through intermittent occlusion of blood flow in the right leg, showing a corresponding reduction in the force level of the pulse in both left and right radial arteries (using pressure transducer measurements). Therefore, it is not illogical to state that changes in an organ’s microcirculation would similarly affect arterial haemodynamics detectable elsewhere in the circulatory system.
At any given point in time, the pulse should reflect the circulatory system’s ability to undertake the distributing and regulatory functions described above. What is described as a ‘pulse’ in the clinical context is foremost, and always, a product of the circulatory system, generated by pressure changes which occur with heart movement. In this context, pulse diagnosis is used to assess heart movement, measuring the rate or frequency of pulse occurrence and whether this is occurring in a rhythmic fashion. From the assessment of pulse movement, it is inferred that the heart is moving and functioning in a particular fashion. Yet these two ‘movement’ characteristics, rate and rhythm, do not adequately explain or describe the range of information that CM literature, or indeed biomedicine, claim as being able to obtain from assessment of the pulse. Thus, in addition to pulse rate and rhythm, there are several other characteristics of the pulse that are assessed. (These are discussed in Chapter 6 and Chapter 7.) In a CM diagnostic framework, each is used to infer the function of a particular aspect of the body via the degree of change occurring in each of the pulse characteristics. The practitioner aims to determine whether the perceived changes in the pulse have arisen due to internal organ function, compromised blood flow, or external conditions such as viruses, bacteria or other environmental factors. It is the body’s response to these factors or attempt to maintain homeostasis or balance which is of interest in the process termed ‘pulse diagnosis’. Investigation and observation of changes in the pulse and their attribution to health is the aim of pulse diagnosis. This leads us to the next question — exactly what is the pulse?
2.2. The pulse
The pulse is a physiological phenomenon propagated throughout the arterial system. It is generally viewed as a travelling pressure wave caused by the rhythmic contraction and relaxation of the heart. Thus the pulse can be described in terms of systole, when the pulse amplitude increases or the heart contracts; and diastole, when the amplitude decreases or the heart relaxes (Box 2.1). A pulse can also be thought of in terms of any regular movement or change in differential pressure that manifests as a rise and fall of fluid in a vessel. In terms of clinical practice, a ‘pulse’ is usually associated with a palpable pressure movement. For example, the radial artery, located at the wrist overlying the radius, is a major site at which to feel the pulse.
Box 2.1
Some definitions
• Systole: The period when the left ventricle of the heart is in contraction forcing blood into the aorta. Systolic pressure is the maximal pressure exerted in the arteries by the heart during systole.
• Diastole: The period when the left ventricle of the heart is in relaxation following systole, when it is refilling with blood. Diastolic pressure is the baseline or resting pressure during diastole, when the heart is at rest. Diastole is the constant pressure that is always present in the artery.
• Blood pressure: The pressure exerted on the walls of the blood vessels. Blood pressure measurements describe the maximal systolic pressure over the resting basal diastolic pressure. Pressure is measured in millimetres of mercury (mmHg). Average blood pressure is 120/80 mmHg.
The pressure wave produced with heart movement is often considered the ‘pulse’, but for purposes of pulse diagnosis using manual palpation the pulse encompasses more than the pressure wave alone. In addition to pressure waves, O’Rourke et al. (1992) note the pulse also encompasses flow waves; the actual movement of blood. They note there is even a third type of wave called diameter waves produced with vessel diameter changes, but these waves are very similar to the pressure wave (O’Rourke et al 1992: p. 17) and, as such, will not be discussed any further in this book. Each of these waves is distinctly different when looking at objective measurements of their contours. Therefore, what is regarded as a single ‘pulse wave’ is in fact a composite of at least two different types of waves. There is the pressure wave, the actual force caused by heart movement, and there is the flow wave, determined by how the pressure wave acts on the actual flow movement of blood. How each contributes to the overall pulse formation probably determines the spectrum of diverse pulse qualities in the CM literature.
In the context of health, it is important to understand that the pulse wave is not a static artefact of heart movement, nor does the pulse remain in constant shape as it moves through the arterial system. It is rather in a constant state of change, acted on by the characteristics of the vessel conduit, the functional state of the organs and tissue and the quality of blood itself, which is in turn determined by the state of health of the individual. It is the cumulative effect of the whole range of these factors that moulds the pulse wave into the pulse that eventually arrives at the radial artery as felt by practitioners. Therefore, the essential characteristics of how the pulse presents to the practitioner when palpating the pulse infer the nature of illness and an individual’s state of health, an intimate ‘record’ of the bodily environment. Pressure waves, flow waves and blood are discussed in further detail below.
2.2.1. Pressure waves
Heart movement produces pressure which causes arterial blood to flow. Pressure waves are generated by the expulsion of blood with heart contraction into the aorta, causing dilatation of that vessel (Guyton and Hall 2006). Thus the greater the blood volume expelled, the greater the pressure wave produced, assuming the aorta’s elastic characteristics remain constant. Blood flows in a closed system of vessels. Any generated pressure therefore affects the entire system. As the pressure wave rises and falls with heart movement, so the blood movement ebbs and flows. In this closed system of pressure and flow, the pressure wave always precedes the actual blood flow, moving considerably faster than its causative affect on the movement of blood (Berne & Levy 1981: p. 105).
The pressure wave has two distinctive components. The first or systolic component has a rise to maximum pressure, followed by a slow decline with a notch or slight increase in pressure from aortic valve closure when the backflow of blood in the aorta overcomes the expulsion force of blood from the heart (Fig. 2.1). According to O’Rourke et al. (1992: p. 40) the second component of pulse formation is due to the phenomenon of wave reflection. Reflective waves are an echo of the initial primary wave that travels from the heart to the periphery. As the arteries narrow in the periphery this results in increased arterial resistance, which causes the pulse wave to rebound, causing a reflective wave to move back towards the heart. Reflective waves occur from the lower and upper body regions. Because the blood vessels of the lower body are larger, the reflective wave affect is also larger than the reflective wave resulting from arterial narrowing in the upper limb. However, both the lower and upper reflective waves have systemic effects and are not confined to the limb in which they were generated. In this way, reflective waves from the lower body interact with the pressure waves in the upper part of the body.
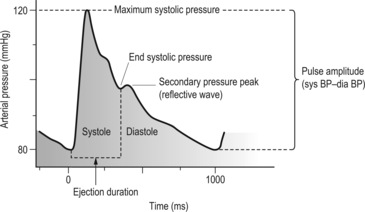 |
| Figure 2.1Features of the radial arterial pulse wave. |
Reflective waves are visualised as a secondary pressure peak in the pulse pressure wave, usually occurring in the diastolic component of the pulse period. Depending on the degree of arterial stiffness, reflective waves can augment the initial primary pressure wave, moving from diastole into the systole component due to arterial hardening (Fig. 2.2). When this occurs the reflective wave merges with the primary pressure wave moving away from the heart, resulting in a greater and longer
Box 2.2. Sphygmography
Diagrammatic representations of pressure waves called sphygmograms or sphygmographs are easy to obtain using pressure sensors. Many CM texts on pulse diagnosis use representation of these graphs to attempt to illustrate different pulse types. Although a useful educative tool, they are limited in their use to represent changes in the pulse wave that occur with different illnesses and caution should be used when looking at these, or mistaking them for the ‘pulse’. This is because many of the CM pulse qualities are not solely dependent for their formation on pressure variations or pressure waves, which are the sole purpose of this form of measurement.
 |
| Figure 2.2The radial arterial pulse wave and augmentation by reflective waves.(After Fig. 3.3.1 in AtCor Medical 2006, A clinical guide: pulse wave analysis, with permission of AtCor Medical Pty.) |
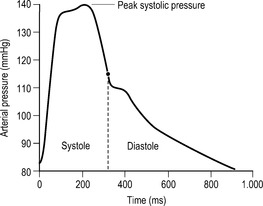
Figure 2.1 illustrates the pressure wave contour typically measured at the radial artery. This is considerably different from the same pressure wave if measured in another part of the circulatory system such as the carotid artery (Fig. 2.3). This is because the anatomy of the arteries varies throughout the circulatory system and this in turn impacts on how the pulse moves through the artery. For example, some arteries are more elastic than others, so their rate of expansion is greater under pressure. This difference is noticeable with palpation when comparing the pulse in the carotid artery in the neck with the pulse in the radial artery in the wrist. The carotid artery has a broader expansive movement because it is more elastic than the radial artery, which has a more distinct arterial wall because it has a large proportion of smooth muscle and thus is not as expansive. The arteries’ capacity to expand with pressure is termed capacitance. The capacitance of a blood vessel is not constant.
 |
| Figure 2.3Features of the carotid arterial pulse wave. Note the rounded contour of the peak pulse pressure due to the carotid elastic properties and relative large diameter. |
Capacitance varies under different conditions, such as differing levels of physical or psychological stress causing a corresponding increase in vessel hardening or vasoconstriction. In this situation capacitance decreases. In addition to capacitance, the pressure wave is also dependent on the stroke volume or amount of blood ejected from the heart with heart contraction. An increased volume of blood gives an increased expansion of the arterial wall, and decreasing blood volume has the reverse effect (assuming the arterial width remains constant).
The major blood vessels are elastic and relatively wide contributing to smooth and unimpeded flow of blood (Stettler et al. 1986). This means the pressure wave remains similar to that at the aorta and throughout all major arteries until the periphery. At the periphery, the arteries begin to narrow. A decreasing arterial width means the force of the pressure and blood flow are compacted together and the pressure exerted from within the artery increases. This is evident in blood pressure measurements between peripheral vessels such as the brachial and radial arteries and the aorta. Maximal pressure in the peripheral arteries such as the radial artery can be 30% greater than maximal pressures in the aorta. However, the force exerted by the pulse pressure wave on the blood vessels falls substantially on entering the smaller capillaries and other vessels beyond the radial and other arteries. Here, Guyton and Hall (2000) note the combined diameter of all these small vessels is greater than that of the arteries and so the force exerted by the pressure wave decreases because of the relative increase in surface area, and the force of the pressure wave is diluted. It should be noted that it is the pressure differential between the aorta and these small capillary networks which causes blood flow; blood flows from an area of high pressure into an area of low pressure (Guyton & Hall 2000).
In CM it is often said that the ‘Qi moves the Blood, and the Blood follows the Qi’. That is, function acts on the blood and the blood responds. In this sense, the pressure wave causes the blood to flow and the blood flow responds accordingly, producing a tidal flow through the vessels. This tidal flow is termed a flow wave and is quite distinctly separate from the pressure wave.
2.2.2. Flow waves
Flow waves refer to the longitudinal movement of blood through the vessel and are the second major component of the pulse wave. Flow waves depend on there being a sufficient volume of blood. It is obvious that if blood volume becomes insufficient then there would be no flow wave. Flow wave formation also depends on the nature of the essential constituents of the fluid. For example, imagine applying a pressure wave to a container of water, and a similar pressure wave to a container of honey. Because of the innate difference in the ‘thickness’ or viscosity of the two fluids, each pressure wave would have a different impact in the creation of the flow wave. The water would transmit the pressure wave into a flow wave easily, with a noticeable surface movement. Because of the thickness of the honey this would not be as noticeable, most likely producing only sluggish movement. In this way, blood can also vary, becoming more viscous or fluid depending on the relative ratio of cells and fluid that make up the blood. However, assuming sufficient blood volume and appropriate viscosity flow waves are determined by two additional factors. These are ventricular contraction and mechanical characteristics of the arterial wall.
Ventricular contraction determines the amount of momentum imparted into the blood forcing it to flow through the vessel. The strength of ventricular contraction also has a relationship to the volume and speed at which blood is expelled from the left ventricle of the heart during systole (Opie 2004). For example, if the heart were to contract strongly, and assuming sufficient time and blood volume for the heart to have refilled during diastole, then the peak systolic pressure would be achieved more rapidly resulting in a sharper incline to the peak if recorded by a sphygmogram. This would cause a greater volume of blood to flow into the aorta at a given point in time. This volume output is referred to as stroke volume (SV) (see Box 2.3). Obviously, if blood volume is diminished or heart contraction slowed then the flow wave would be similarly affected.
Box 2.3
Cardiac output
The total volume of blood flow in 1 minute is termed cardiac output (CO). CO depends on the blood volume expelled by the heart during systole of each heartbeat, termed stroke volume (SV), and the total number of heartbeats per minute or heart rate (HR). Thus:
This relationship is commonly used in biomedical practice for determining the heart’s pump function in maintaining adequate blood flow for tissue perfusion. Blood pressure and resistance to blood flow also have a direct bearing on cardiac output.
The second additional factor in flow wave formation involves mechanical properties of the arterial wall. When the heart contracts, a pressure wave moves into the aorta causing it to expand. When the pressure is removed during heart relaxation (diastole) the aorta returns or recoils to its normal shape. The recoil releases this potential energy stored during expansion back into the blood, causing the blood to flow forward. In conditions in which the elasticity of the arteries is compromised, recoil is diminished and the blood flow becomes retarded, which compromises circulation and the associated functions of the circulatory system. For example, if the arteries were relatively stiff, then a secondary fluctuation or reflective wave would move from diastole into systole, augmenting the initial flow wave, whereas a relaxed or elastic artery would not produce augmentation of the initial wave. Conditions affecting the arterial wall affect the flow wave. This relationship between arterial properties and characteristic of ventricular contraction is described as vascular impedance.
2.3. Blood
Blood is an important component of the formation of the pulse. It is a complex fluid, composed of a plasma liquid base and several formed particles, the most prominent of which are red blood cells, which make up 99% of all particle types found in blood. Other components include:
• White blood cells
• Platelets
• Proteins (albumins, globulins, fibrinogen) dissolved in the plasma.
For these reasons blood is referred to as a liquid tissue. Blood is the medium in which the pulse wave propagates from the heart to the periphery. Therefore, changes in the blood medium — that is, changes in any of the ratio of its components — will affect the propagation of the pulse wave. Changes can occur in a number of ways. They can arise due to illness, from trauma producing blood loss, or from diet where an individual’s inadequate intake of appropriate food groups adversely affects the quality and quantity of the blood. In this way, the ratio of the different cell components of blood can vary between people and can vary within the same individual over time. Blood may consequently ‘thicken’ or ‘thin’. The relative degree of ‘thickness’ is termed viscosity.
Blood viscosity depends on the ratio of cells to plasma in the blood. The higher the proportion of cells, the denser or more viscous is blood. This means that blood becomes more difficult to move through the blood vessels as resistance to its smooth flow increases. For example, polycythemia is a state in which the red blood cell ratio is raised, causing blood to become more viscous. In this state blood flow fluidity is affected, flow velocity slows and blood pressure becomes raised due to increased resistance to its flow in the vessels. Chronic smoking, athletic training and high altitudes can all cause an increase in the ratio of red blood cells. An increased demand for oxygen by the body causes an increased number of red blood cells to assist with oxygen transportation. The concentration of red blood cells can also increase when fluid is lost from the blood plasma through dehydration or burns. Alternatively, dietary intake of iron may fluctuate depending on food sources. Eventually, this also affects blood through changes in the red blood cell ratio and changes in blood viscosity, and changes in the pulse wave will consequently also occur. For example, the decreasing iron levels and haemoglobin associated with anaemia are often accompanied by regulatory changes in blood pressure via vasodilatory mechanisms in an attempt to maintain homeostasis as red blood cell ‘quality’ and ratio decrease. This in turn affects the propagation of the pressure wave and resultant flow wave. Additionally, sudden loss of blood volume due to haemorrhage (cells and fluid) also affects pressure and flow waves. Interestingly, blood volume can also decrease when fluid moves out of the blood plasma, as occurs in dehydration.
2.3.1. Velocity of blood flow
As hinted at in the description of pressure waves, the speed or velocity at which blood moves through the vessels is not constant. There are a number of variables that affect this. The first and most obvious is heart rate. As pressure exerted by the heart increases during systole, blood flow increases under the influence of the pressure wave; as the heart relaxes, so blood flow slows. Any change in pulse rate frequency, or strength at which the heart contracts during systole, will affect blood velocity. Blood flow velocity is measured in centimetres per second (cm/s).
The velocity of blood flow also depends on arterial width. When an artery is wide the blood velocity slows in comparison to blood flow in a narrow artery, in which the velocity hastens. The velocity of blood flow is inversely related to arterial width. Tortora & Grabowski (1996) state:
This means that blood flows slowest where the cross-sectional area is greatest, just as a river flows more slowly as it becomes broader. Each time an artery branches, the total cross-sectional area (diameter) of all its branches is greater than that of the original vessel. On the other hand, when branches combine, for example, as venules merge to form veins, the total cross-sectional area becomes smaller … Thus the velocity of blood flow decreases as it flows from the aorta to arteries to arterioles then capillaries and increases as it leaves capillaries and returns to the heart (p. 620).
For pulse diagnosis purposes the relative degree of arterial wall tension also influences blood flow velocity (arterial wall tension can increase without arterial narrowing). Blood velocity hastens because the artery resists the pressure being exerted by the pulse wave, no longer expanding as it usually would. Consequently, this energy is redirected back into the forward movement of blood. This is likely to be seen in conditions where arterial tension increases via the contraction of the arterial muscle layer (the tunica media), as in cases of psychological or physical stress (‘fright, flight or fight’ response). It is hypothesised that the Stringlike (Wiry) pulse may be attributed partly to this action and the consequent change in blood velocity and resultant diminishing of pulse wave contour. Additionally, pulses which have a distinct amplitude/contour or shape, such as the Slippery pulse, could be associated with a decrease in arterial hardening in which the pressure pulse easily expands the vessel wall, shaping it to the flow wave, assuming there is sufficient blood volume for this to occur.
2.3.2. Arteries
The two primary subdivisions of the arteries are the central and peripheral subdivisions. The central subdivision encompasses all arteries in the region of the torso. Circulatory activity in this region is collectively referred to as the central haemodynamics. The arteries located in the central region are wide and relatively elastic, to deal with the high volume flows and the relatively large pressures that are exerted from within. Examples of central arteries are the carotid artery and the aorta. Their elastic properties also assist in the propagation of the pulse signal further along the arterial trunk to the peripheral blood vessels.
The peripheral subdivision encompasses all arteries located in the limbs. Circulatory activity in this region is collectively referred to as the peripheral haemodynamics. Examples of peripheral arteries include the brachial and radial arteries. The arteries in the periphery are described as muscular arteries, having a greater proportion of smooth muscle relative to elastic fibres in the inner layer of the blood vessels. Consequently, Tortora and Grabowski (1996) note the peripheral arteries have a greater vasodilatory and vasoconstricting function than is found with centrally located arteries such as the aorta (see Box 2.4).
Box 2.4
Elastic and muscular properties of arteries
Differences in the elastic qualities versus the muscular properties of the central and peripheral arteries can be felt by comparing the carotid arterial pulse with the radial arterial pulse. The carotid artery is located lateral to the larynx, medial to the sternocleidomastoid muscle. By gently palpating one of the arteries it can be felt that the carotid arterial pulse has a noticeably larger amplitude from the base pressure to the maximum pressure. In comparison, it will be found that the radial artery has noticeably less amplitude difference and is not as expansive across the fingers. Note also that the difference in width between the carotid and radial artery also influences how the pulse feels when palpated.
2.3.3. The radial artery
The radial artery is classified as a peripheral artery. It is a prime area for palpating pulse, and is unique for use in clinical practice as the ‘vascular properties in the upper limbs are less affected by ageing, arterial pressure, or various manoeuvres as compared to vessels in the trunk and lower limbs’ (Chen et al 1997: p. 1834). This means that the radial pulse probably reflects disease-related changes irrespective of an individual’s age. This makes it an ideal area for pulse assessment, and it is the primary site used in both the biomedical and CM systems.
The radial artery commences at the bifurcation of the brachial artery, just distal to the elbow crease, following the lateral portions of the forearm into the hand (Strandring et al 2005). It is the wrist portion of the radial artery, approximately 3–5 cm in length, which is often used for pulse assessment. At this region the radial artery sits superficially, supported by the styloid process of the radius and local tendons such as the brachioradialis. The radial artery is covered by a thin layer of collagen fibres, fat and keratinised cells which form the dermal and epidermal fasciae (Lanir 1986). The radial artery forms two distinct arterial branches. The first is the dorsal carpal branch which meets the ulna dorsal carpal branch and forms the dorsal carpal network that eventually feeds to the middle, ring and little fingers. The second branch is the first dorsal metacarpal artery which supplies blood to the thumb and index finger (Strandring et al 2005) (Fig. 2.4).
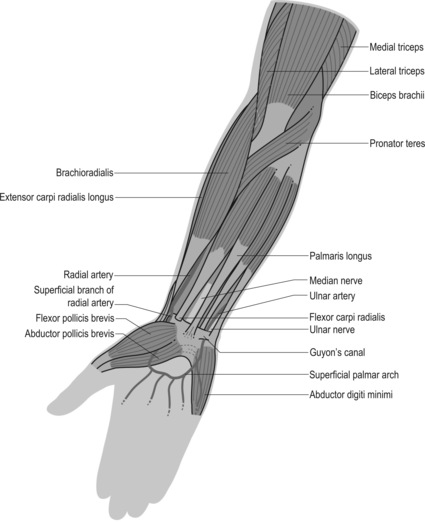 |
| Figure 2.4Position of the radial artery relative to other structures of the forearm. |
All arteries consist of three layers (Fig. 2.5):
• Tunica media: The middle smooth muscle layer that constricts and dilates arterial width
• Tunica intima: The internal elastic layer and thick layer of endothelial cells in contact with the blood. This elastic layer makes the vessel wall smooth for frictionless blood flow and stretches with pulsatile flow during systole and diastole.
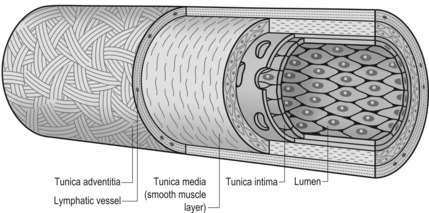 |
| Figure 2.5Structural layers of the radial artery.(After Fig. 7.4 in Gray’s anatomy: the anatomical basis of clinical practice, 39th edn, with permission of Elsevier.) |
The relative proportions of the three wall layers differ depending on the location and associated function that the artery undertakes. For example, the radial artery has a relatively greater proportion of smooth muscle (tunica media layer) than centrally located arteries, such as the aorta, to assist in its distribution and regulation of blood flow.
For the practitioner, it is important to understand that each vessel layer can contribute its own unique ‘signature’ to the presentation of the pulse wave and how it is felt when palpated at an arterial site. The tunica media and tunica intima are particularly important in the practice of pulse diagnosis. These distinct arterial composites of the arterial wall are identifiers of disease and are just as important as the actual pulse movement. A loss of the smooth internal wall through plaque formation in arteriosclerosis will also affect blood flow. This in turn may activate platelet aggregation and formation of clots, or simply affect the smooth flow of blood causing turbulence. In this way, pulse diagnosis is not simply just about the ‘pulse’, it also encompasses the assessment of the blood vessel wall.
2.4. Summary
The pulse is a physiological phenomenon propagated throughout the arterial system and can be viewed as an indication of the circulatory system’s capacity to undertake the distribution of essential substances required for metabolism to body tissue and organs. In the context of health, the pulse is a complex physiological sign and can be described in terms of systole and diastole. It is primarily composed of pressure waves (including reflective waves), and flow waves.
Once produced, a pulse wave undergoes a series of changes as it moves from the heart or central regions of the body into the peripheral blood vessels of the arms and legs. By the time the pulse wave arrives at the radial artery it may have a distinctly different shape and contour than it had when initially produced by the heart. Variables that influence the presentation of the pulse as felt with palpation at the radial artery include:
• Anatomical structure of the blood vessel
– Arterial width
– Arterial tension
– Ratio of elastic versus muscular tissue
• Viscosity or density of blood
• Blood volume
• Stroke volume of blood flow
• Region of the body the pulse is being palpated
• Heart function.
These, in turn, are influenced by the neural, hormonal and chemoregulatory systems for blood pressure and maintaining blood flow for purposes of homeostasis or balance in health and illness. A change in health status affects homeostasis balance, which in turn affects the pulse.
2.5. The pulse in biomedicine
The procedure of pulse palpation is termed sphygmology, literally meaning ‘the study of the pulse’. The term sphygmos derives from Greek meaning literally a pulse or throb. In contemporary biomedical practice the pulse is used in the assessment of several conditions mainly affecting circulation and reflecting heart function. The pulse is primarily viewed as a product of the heart and compliance of the vascular system, and is highly dependent on the use of sophisticated devices able to record and measure variables quantitatively. Accordingly, the term pulse palpation is largely used with reference to the determinant of pulsatile strength, heart rate and heart rhythm by manual palpation. Yet pulse palpation has not always been used in this manner within biomedicine; it once had an equally broad application for identifying ‘qualitative’ changes in the pulse, as is still claimed in CM.
The principles of sphygmology are derived from the works of ancient Greek physicians, in particular Galen (131–199 ce) (Naqvi & Blaufox 1998), but can be traced back even further to Hippocrates (approximately 450–350 bce). Other important historical figures in the development of pulse in the health assessment process included Aegimius, whose writings founded the concept of pulse as a diagnostic technique; Rufus of Ephesus and his treatise Synopsis on Pulses; and Herophilus of Alexandria, the reputed founder of sphygmology (Bedford 1951, Hsu 2005, Kuriyama 1999, Lloyd 1996). But it was Galen’s prolific discourse on the use of pulse in assessing health, including commentaries on the pulse writings of his predecessors, which meant his thinking on pulse would dominant the practice of pulse by subsequent occidental medical healers.
Galen’s interpretations and descriptions of pulse characteristics have more in common with the CM view of the pulse than with modern biomedical principles. They include differentiating pulse speed, length, width and depth to the body’s homeostasis, and describing them in terms of excess or deficiency depending on the presenting pathology. Variables affecting the pulse presentation were listed as including age, seasons, food, pregnancy and the environment. The pulse was also referred to in terms of organic pulses; authors later interpreted organic pulses as an extension ‘by which each organ imparted its personality to the pulse’ (Bedford 1951: p. 428). That is, specific pulse types were specifically seen as arising from different organs.
Pulse diagnosis in the intervening centuries since Galen’s time remained largely dependent on his books on the pulse, even in times when a more ‘scientific’ or physiologic basis for circulation of the pulse was described by Harvey in the 16th century. For example, Naqvi & Blaufox (1998: p. 24) note Theophile Bordeu (1722–1776) in his 1756 publication Recherches sur le pouls describing the ‘gastric pulse’, ‘renal pulse’ and ‘uterine pulse’ as arising specifically from the organs. Unfortunately, Galen’s extensive writings were plagued with descriptive anomalies which meant clinical interpretation was variably successful with physicians just as often disagreeing on the meaning of a pulse as agreeing (Kuriyama 1999).
As an aside, with reference to Chinese medicine, Hsu notes that the language of pulse remained descriptive, even in later centuries as pulse knowledge accumulated. Pulse qualities continued to be likened to descriptive imagery; practitioners associated pulse sensations to what they saw in the environment around them (Hsu 2005). Such an observation regarding the descriptive use of language in Chinese medicine is equally applicable to pulse terminology in the Western traditions and even into contemporary times. For example, the Steel Hammer pulse is compared to the resounding ring of a hammer blow. This perhaps describes the lack of expansion of the artery on pulsation and the resonance felt by the practitioner’s palpating fingers. These descriptions used by these classical occidental practitioners to describe the various presentations of the radial pulse would have had a resonance for contemporary CM practitioners. For example, terms such as tense, wiry and thready were variously used to describe different qualitative aspects of the pulse (Table 2.1). Some of these pulse terms continue to be used in modern cardiology units and for general health assessment.
| Pulse name | Pulse description | Page number |
|---|---|---|
| Jarring | Jerky and sharp | 139 |
| Steel Hammer | Abrupt and energetic as the rebound of a blacksmith’s hammer; observed in arteries near a joint in rheumatism | 142 |
| Herpes drugs, chemical burn | ||
| Tense | When artery resembles a cord fixed at each extremity, a hard full pulse. When it feels still harder and smaller, it is called wiry | 142 |
| Thready | A scarcely appreciable one as observed in syncope. Rate is rapid; wave appears quickly, is small, and disappears quickly | 142 |
| Trigeminal | Three regular beats followed by a pause | 142 |
From the 16th/17th centuries, the traditional practice of pulse diagnosis, still based on Galen’s work, was radically challenged in two ways. The first was the emerging understanding of blood flow as a single circulatory system, as established by Harvey in the early 17th century. The second was the increasing experimentation of recording pulse waves objectively using mechanical devices. Objective measurements were free from the observer’s personal bias; this meant a recording of the pulse wave could be simultaneously observed and discussed by several practitioners, thereby removing the ambiguity of pulse interpretation that had plagued the technique in past centuries.
By the late 19th century the arterial wave form was being regularly recorded using sphygmograms. For example, Figure 2.6 illustrates such a recording originally published in 1906. Such recordings of the radial arterial waveform were made by mechanisms attached to the wrist region over the radial artery. The pulsations would displace these mechanisms and produce tracings, which were referred to as sphygmographs. In the context of clinical practice, the physician concentrated on deciphering the sphygmograph and its relationship to a patient’s health and any disease present.
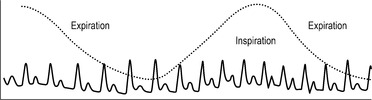 |
| Figure 2.6A sphygmograph trace recorded by Lewis showing the interaction of respiration in a subject with a dicrotic pulse(After Figure 1, p. 415 in Lewis 1906.) |
Yet while objective pulse measurements were obtainable using these mechanical devices, quantitative measurement was not the primary purpose of these recordings. Rather the measurements were obtained to visualise the contour of the pulse waveform being palpated (Fig. 2.6).
However, at the end of the 19th century, the pulse and its use in clinical practice was radically changed when Riva-Rocci introduced into clinical practice the indirect method by which arterial blood pressure was objectively measured. This involved using a mercury manometer, the forerunner of the present-day brachial cuff sphygmomanometer (Naqvi & Blaufox 1998). Eventually, the focus on the sphygmomanometer, as described by O’Rourke et al (1992), saw the descriptive terms diastolic and systolic supplant a range of ‘qualitative’ variables that, until that time, had had high clinical significance placed on them.
This changed perception of the significance and relevance of the pulse wave qualities in clinical diagnosis was not so surprising, according to Kuriyama (1999), since there had always been doubt within the medical fraternity concerning the use of pulse diagnosis to inform diagnosis. The subjective nature of pulse diagnosis, and the inability of the physicians to agree on pulse interpretation, were clearly seen as reasons for this.
2.5.1. Mechanical measurement
In contemporary practice, the benefit of mechanical measurement has been to standardise the system of pulse assessment and to provide a system of accurate record keeping. However, the interpretation of the pulse has largely remained focused on the investigation of the relationship of the heart to systolic pressure, diastolic pressure, heart rate and rhythm. This is evident in the interpretation of sophisticated measurements of the cardiac system back to these basic values. For example, the electrocardiogram (ECG) is primarily interpreted in terms of its presence, rate and pressure values. O’Rourke et al (1992), described this as ‘high-tech recording’ being linked to ‘low-tech interpretation’ (p. 25). Little or no attention is paid to the details of the arterial wave formation, and according to O’Rourke et al (1992)
one would have to concede that basic information presently available on the arterial pulse not only is sparse but also confusing and contradictory. It is surprising that so little is known about the arterial pulse, given the sophisticated knowledge of other bodily functions (p. vii).
It is noteworthy that although objective measurements of the pulse do provide quantitatively derived and standardised values, the interpretation of such values is still very much dependent on the diagnostic theory and principles underlying the associated medical system. This is particularly evident in biomedicine, with a number of apparently ‘abnormal’ pulses also having been recorded in people who are, in all respects, apparently ‘healthy’. O’Rourke et al (1992) additionally note that it is not unusual for different authoritative texts to give conflicting explanations and indications for the same pulse type, even when it presents in someone who is apparently healthy.
This discrepancy in pulse classification in the biomedical model may be explained by the focus of biomedicine on cardiac and arterial health as the central variable in the origin of pulse formation. That is, if arterial compliance and cardiac competence are not compromised then the pulse wave is often classified as healthy, irrespective of pathology occurring elsewhere in the body.
2.5.2. The process of pulse palpation in contemporary biomedical practice
2.5.2.1. Arterial pulsations and thrills
Biomedicine makes use of several arterial sites throughout the body, including the dorsalis pedis, femoral, brachial and carotid arteries (Fig. 2.7), but the radial artery remains the primary site of manual palpation for most encounters. The others are used for primary or secondary diagnosis of conditions. For example, carotid arterial pulsations are used for assessing cardiac conditions. The dorsalis pedis pulse, in contrast, is used in addition to other pulse sites for assessing strength of peripheral blood flow to the lower limb.
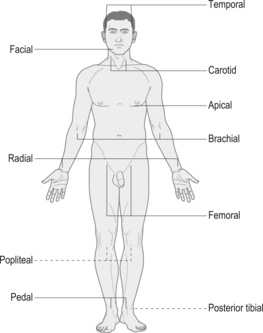 |
| Figure 2.7Location of the pulse sites.(From Funnell et al 2005, Tabner’s nursing care: theory and practice, 4th edn, with permission of Elsevier.) |
In addition to arterial pulsations, the jugular venous pulse is examined. The jugular venous pulse is synchronous with pressure changes in the right atrium (which receives blood from the vena cava). In this way, it is used as an indicator of heart and lung function. Variations in the usual contour and strength of the jugular pulse indicate that the right atrium is contracting against increased resistance associated with tricuspid stenosis, pulmonary hypertension or pulmonary stenosis.
Additionally, the clinician attempts to identify ‘thrills’ or vibrations associated with heart murmurs. O’Rourke & Braunwald (2001) state:
The systolic murmur of mitral regurgitation may be palpated at the cardiac apex. When the palm of the hand is placed over the precordium, the thrill of aortic stenosis crosses the palm toward the right side of the neck, while the thrill of pulmonic stenosis radiates more often to the left side of the neck. The thrill due to a ventricular septal defect is usually located in the third and fourth intercostal spaces near the left sternal border (p. 1257).
2.5.2.2. Finger placement
Using varying increments of pressure, the index and middle fingers are most often used to palpate the pulse at the radial artery. For example, Harvey (1994) asserts that only light pressure is needed to detect pulsus alternans; heavy pressure would occlude it. Some clinicians also suggest the use of the upper palm, where the fingers join, for palpating pulsation through the abdomen and chest as this region of the hand is more sensitive than the finger tips (Harvey 1994). This region of the palm is likely to be used in assessment of thrills at the precordium.
The point at which the pulse is felt most strongly usually dictates the arterial site used for palpation within a given segment of artery. Anatomically, this may very from person to person or within the same person, from day to day. For the radial artery, it is generally the region situated between the wrist crease and medial to the styloid process.
2.5.2.3. Positioning of patient and practitioner
Sometimes, the patient needs to have the arm placed in a certain position to detect specific pulse changes. An example is the detection of the Water Hammer or Collapsing pulse. This is a pulse that occurs in the presence of aortic valve insufficiency in which the aortic valve between the heart and aorta does not close properly. This causes blood to regurgitate or flow back into the left ventricle in the resting or diastole phase rather than continuing forward to the periphery. Therefore, when palpating the pulse during systole the pulse wave increases as usual then suddenly disappears or collapses during diastole. This is particularly noticeable when the patient’s arm is raised above their head. At other times the patient may be reclined at a 45° angle for detection of carotid and jugular pulsations. When examining the carotid pulse, the sternocleidomastoid muscle is placed in a state of rest by slightly turning the patient’s head towards the practitioner. For the brachial artery, the subject’s arm is maintained in a relaxed position, ideally being supported by the practitioner’s arm and using the forefinger to palpate the pulse.
Once the pulse is located, the practitioner uses different increments of pressure to assess the diastolic and systolic components of the pulse pressure wave, assessing variations in pulse contour and pulse strength. This includes assessing the strength of cardiac contraction and consequent pulse pressure rise and amplitude during systole, the duration of the maximum pulse amplitude and the downward diastolic slope. For the radial pulse there is often no strict rule for positioning of the patient and palpation can occur at any time during the examination process. As with the brachial arterial pulse, a similar range of contour variables would probably be assessed in addition to rate and rhythm.
2.5.2.4. The pulse in biomedical clinical practice
Although manual pulse assessment alone is still used to assist in the detection of several conditions, it is often performed in conjunction with auscultation by stethoscope. The stethoscope provides auditory information regarding the heart function and smoothness of blood flow. Uncharacteristic sounds arising from blood flow or heart function are distinctly diagnostic of certain types of dysfunction.
Conditions where pulse assessment alone provides an important diagnostic tool include heart disease, aortic coarctation, hypertrophic cardiomyopathy and aortic regurgitation (Tortora & Grabowski 1996). Funnel et al state that the pulse is assessed primarily on three factors: pulse rate, rhythm and volume (2005: p. 267). These three factors inform about peripheral perfusion and cardiac function. For example, comparative assessment of the strength of the radial and femoral pulses can identify aortic coarctation and is also used as a general assessment of circulatory blood flow to the periphery. Pulse rate identifies conditions involving bradycardia and tachycardia, and the ease of occlusion can identify anaemia. Occasionally, the pulse is examined for blood flow and can be useful in detecting aortic regurgitation as with the Corrigan’s or Water Hammer pulse (see Box 2.5). The arterial structure may also be assessed for plaques, imperfections or abnormalities affecting blood flow.
Box 2.5
Examples of some distinct pulse types recorded in the biomedical literature
• Pulsus tardus: Has a slow rate of climb to the systolic pressure peak, thus a late systolic peak and a similar slow pressure decline. Due to left ventricular ejection obstruction; blood flow is impeded from the left ventricle to the aorta.
• Hyperkinetic pulse: has an increased systolic stroke volume and large pulse amplitude. The peripheral blood vessels are dilated. It is seen during exercise, fever and anxiety.
• Hypokinetic pulse: The opposite of the hyperkinetic pulse, it has a decreased stroke volume with a pressure wave lacking strength.
• Bisferiens pulse: A pulse that has two palpable peaks during systole. It can occur in any condition affecting heart contractility.
• Bigeminal pulse: A variation of the previous pulse, but occurs regularly and is due to premature ventricular contraction following a regular heartbeat. Manifests as, one strong beat, a weak beat, then a strong beat.
• Dicrotic pulse: Two pulse waves for each heartbeat: a pressure wave from the heart during systole and a reflective pulse wave from the limbs detected during diastole.
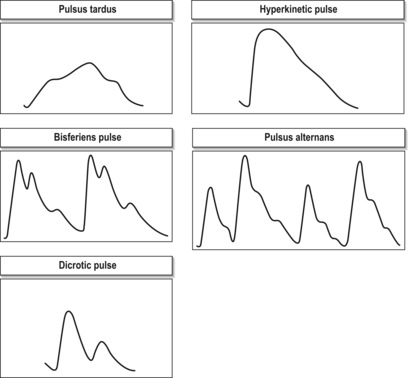 |
(Descriptions derived from Amber & Babey-Brooke 1993, O’Rourke & Baunwald 2001a, O’Rourke et al 1992).
Drzewiecki et al (1986) assert that manual palpation cannot detect diastolic pressure — the constant, baseline pressure in the blood vessels that is always there — but can be used ‘to determine systolic pressure as long as a palpable pulse is present. Thus it finds application where other occlusive cuff methods fail, e.g., in children, with patients in shock, or with hypotensive patients’ (p. 2). In most cases, however, the pulse is viewed as an extension of heart function and used for obtaining measurements of heart rate.
2.6. The pulse in contemporary CM clinical practice
In CM, the process of pulse diagnosis is termed qie mai. Mai derives from a Chinese character meaning a vessel and can equally be applied to blood vessels and acupuncture channels. Qie refers to the process of feeling. Kuriyama (1999) interprets the term qiemai as referring to ‘streams of blood’ (p. 51). In CM, the term pulse diagnosis primarily refers to palpation of the radial arteries at both the left and right arms. It also includes Nine Continent pulses, a seldom—used system that involves palpating several arterial sites situated throughout the body, including the head, torso and legs. In contemporary CM practice, pulse diagnosis is believed to provide both specific and general clinical information (Maciocia 2004):
…apart from giving us indications about prevailing disharmonies, it also reflects the constitution of a person; …pulse diagnosis can give us a very detailed and accurate picture of the state of Qi in all organs and all parts of the body (p. 457).
A wide range of views regarding the importance of pulse in clinical practice is expressed by various authors. Contrary to the emphasis placed on pulse in the diagnostic process by some modern CM authors (Hammer 2001, Maciocia 2004, Porkert 1983), its importance in the modern CM clinic appears to be changing. Some practitioners regularly take the patient’s pulse throughout the treatment session when administering acupuncture in order to gauge the effect of treatment on the patient, and this will influence the duration of needling, the points needled and the degree of needle manipulation. In this case, treatment would continue until the pulse characteristics presented in a desired formation (Birch & Felt 1999). For other practitioners, the pulse is relegated to playing a ‘minor, confirmatory role’ (Flaws 1997: p. 7).
In the experience of two modern CM authors (Flaws 1997, Hammer 1993), the use of pulse as a diagnostic skill has been declining worldwide and particularly in China. In Flaws’ experience as a student in China as long ago as the 1980s, the pulse was examined only briefly, utilising fewer than 10 of the basic CM qualities, such as slow, fast or deep, and rarely discussed in terms of pulse positions. In his opinion, the low importance placed on the pulse in the diagnostic process appeared to stem from the fact that pulse was unable to be validated from a Western physiological perspective, at a time when the focus appeared to be on scientific validation of CM theories.
The changing role of pulse diagnosis was also evident in the results of a questionnaire completed by a selection of Australian university CM students, which evaluated the use of pulse diagnosis by student practitioners (Smith 1996). The study found that while 82% of the students surveyed rated the pulse as ‘important’ or ‘very important’ in formulating a diagnosis, in practice they often used pulse solely as a confirmatory tool and not to establish diagnosis.
In spite of this apparent change in the role of pulse diagnosis observed in students, an Australian survey of CM practitioners found that traditional diagnostic methods are seemingly still being utilised in clinical practice. In 1996 the Victoria State Department of Human Services commissioned a review of the practice of CM in Australia, resulting in a published report called Towards a Safer Choice (Bensoussan & Myers 1996). The authors noted that in a survey of both non-medical and medical practitioners who use CM, 90% of those practitioners who identified CM as their major form of practice said that they relied mainly on CM theory for diagnostic purposes.
Therefore, it can be seen that, amongst the numerous practitioners who utilise CM, there seem to be wide ranging differences in the emphasis placed on the use of traditional theory, such as pulse or tongue diagnosis, in clinical practice. The duration of CM education appears to play some role in determining the importance that allied health practitioners (who incorporated CM practices such as acupuncture into their treatments) give to the traditional theoretical framework. A survey of physiotherapists in the United Kingdom who utilised acupuncture found that:
Respondents who had undertaken long acupuncture courses were more likely (p < 0.001) to use pulse diagnosis, tongue diagnosis and five element theory when compared with those who had not. They placed more importance on traditional diagnosis (p < 0.001) and less on Western diagnosis (p = 0.004).
2.6.1. The process of pulse palpation in contemporary CM practice: a preliminary introduction
2.6.1.1. Finger positioning
Examination of the radial pulse takes place on both arms at the skin region proximal to the wrist crease, directly above the pulsation of the radial artery. This area is divided into three sections referred to as the three pulse positions: Cun(closest to the wrist crease), Guan(medial to the styloid process of the radius) and Chi (furthermost from the wrist crease) in a region approximately 5 cm in length (Fig. 2.8). Each pulse site can be further divided into two levels (superficial and deep) or three levels of depth (superficial, middle and deep). During assessment the wrist is always placed at the level of the heart to avoid pressure variations that may distort the pulse wave. (Pulse assessment techniques and method are discussed in detail in Chapter 5.)
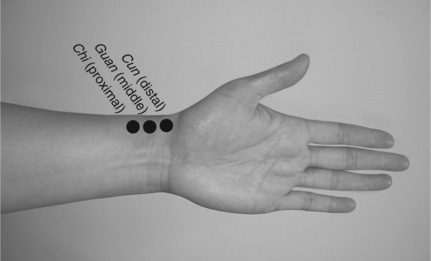 |
| Figure 2.8Finger placement at the three pulse positions. The distal placement corresponds to Cun, the middle to Guan and proximal to Chi. |
Various theoretical systems may be used in the interpretation of the radial pulse information obtained during palpation. (These theoretical systems are termed pulse assumption systems.) For example, each of the positions can be considered as a reflection of the flow of energy through specific pathways in the body (known as channels or meridians), or each position may be associated with a particular internal organ. Alternatively, the Cun, Guan and Chi positions may be seen to reflect the upper, middle and lower regions of the trunk of the body respectively (Maciocia 2004). Birch & Felt (1999) describe a number of other interpretations: for example, Worsley’s traditional acupuncture system in which the relative strength of each pulse position is classified, the Japanese keiraku chiryo system which only uses the 6 deep positions to identify 4 general patterns of weakness and lastly, the use of specific pulse qualities that attempt to classify the pulse in terms of the 27 or so traditional pathological pulse types.
2.6.1.2. The pulse in CM clinical practice
The pulse as a diagnostic technique is incorporated into clinical practice in the four examinations: the basic structure from which a practitioner garners information from patients. The four examinations consist of observation, listening/smelling, asking and palpation. The last category, palpation, usually involves applying pressure to sensitive acupuncture points and tender muscles around the body as well as examination of the pulse.
The three distinct finger positions at the radial pulse have an important diagnostic value. Each position has a theoretical connection to an internal organ structure and therefore each position reflects the relative health or function of that organ. This idea of function permeates all aspects of CM. The concept’s origins can be traced back to the Nei Jing, the earliest extant book on Chinese medical theory. In reference to health, the book emphasises the individual as being in direct influence with their surrounding environment and of that environment being reflected within that individual’s physiology. This micro/macrocosmic dichotomy formed an important foundation for the development of present-day CM diagnostic principles, with disease categorisation based on functional relationships and interactions in addition to actual organic pathology.
Contemporary theories explain this relationship in terms of fluid dynamic principles. The position of each organ in the body is situated at a specific distance from the wrist. Subsequently, this imparts a distinct signature or harmonic to the overall haemodynamic flow wave, which through amplification in the long arteries of the arm can be uniquely palpated distinctly at each of the three positions (Dai et al 1985, Xue & Fung 1989a, Xue & Fung 1989b).
2.6.1.3. Characteristics and qualities
A theoretical assumption of pulse diagnosis is that each position provides different information on body function, which a practitioner uses to arrive at a diagnosis or prognosis. Diagnosis or prognosis is dependent on the variability of each pulse characteristic such as pulse rate. A slow pulse rate (<60 bpm) can indicate hypometabolic activity, as in the case of hypothyroidism, while an increase in pulse rate above that what is normally expected (>90 bpm) can indicate hyperactivity, as in the case of febrile conditions. These characteristics form the foundation of the specific pulse qualities; a distinctive set of pulse characteristics that occur simultaneously with specific disease states. These are discussed extensively in Chapter 6 and Chapter 7.
In addition to disease states, there are several variables that are traditionally assumed to influence the pulse, including age, gender, weight, seasons, circadian cycles, personal traits and environmental conditions. These are explored further in Chapter 5.
References
J Alltree, Physiotherapy and acupuncture: practice in the UK, Complementary Therapies in Medicine 1 (1993) 34–41.
R Amber, A Babey-Brooke, Pulse diagnosis: detailed interpretations for eastern and western holistic treatments. (1993) Aurora Press, Santa Fe, NM .
DE Bedford, The ancient art of feeling the pulse, British Heart Journal 13 (1951) 423–427.
A Bensoussan, S Myers, Towards a safer choice: the practice of traditional Chinese medicine in Australia. (1996) UWS, Sydney .
R Berne, M Levy, Cardiovascular physiology. 4th edn. (1981) Mosby, St Louis .
S Birch, R Felt, Understanding acupuncture. (1999) Harcourt Brace, London .
T Bordeu, 1756 Recherches sur le pouls par rapport aux crises, In: (Editors: NH Naqvi, MD Blaufox) Blood pressure measurement: an illustrated history (1998) Pantheon, New York.
C Chen, E Nevo, B Fetics, et al., Estimation of central aortic pressure waveform by mathematical transformation of radial tonometry pressure: validation of generalized transfer function, Circulation 95 (7) (1997) 1827–1836.
K Dai, H Xue, R Dou, et al., On the detection of messages carried in arterial pulse waves, Journal of Biomechanical Engineering 107 (1985) 268–273.
G Drzewiecki, J Melbin, A Noordergraaf, Noninvasive blood pressure recording and the genesis of korotkof sound, In: (Editors: R Skalak, S Chien) Handbook of Bioengineering (1986) McGraw-Hill, New York; Ch 8.
B Flaws, The secret of Chinese pulse diagnosis. 2nd edn. (1997) Blue Poppy Press, Boulder, CO .
R Funnell, G Koutoukidis, K Larence, Tabner’s nursing care: theory and practice. 4th edn. (2005) Elsevier, Sydney .
A Guyton, J Hall, Textbook of medical physiology. 11th edn. (2006) Elsevier, Philadelphia .
L Hammer, Contemporary pulse diagnosis: introduction to an evolving method for learning an ancient art – part 1, American Journal of Acupuncture 21 (2) (1993) 123–139.
L Hammer, Chinese pulse diagnosis: a contemporary approach. (2001) Eastland Press, Seattle .
WP Harvey, Cardiac pearls, Disease-a-month XL (2) (1994) 43–113.
E Hsu, Tactility and the body in early Chinese medicine, Science in Context 18 (1) (2005) 7–34.
S Kuriyama, The expressiveness of the body and the divergence of Greek and Chinese medicine. (1999) Zone Books, New York .
Y Lanir, Skin mechanics, In: (Editors: R Skalak, S Chien) Handbook of bioengineering (1986) McGraw-Hill, New York; Ch 11.
T Lewis, The factors influencing the prominence of the dicrotic wave, Journal of Physiology 34 (1906) 414–429.
G Lloyd, Aristotelian explorations. (1996) Cambridge University Press, Cambridge .
G Maciocia, Diagnosis in Chinese medicine: a comprehensive guide. (2004) Churchill Livingstone, Edinburgh .
NH Naqvi, MD Blaufox, Blood pressure measurement: an illustrated history. (1998) Pantheon, New York .
L Opie, Heart physiology: from cell to circulation. 4th edn. (2004) Lippincott, Philadelphia .
RA O’Rourke, E Braunwald, Physical examination of the cardiovascular system, In: (Editors: E Braunwald, A Fauci, D Kasper, et al.) 15th edn Harrison’s principles of internal medicine, Volume 1 (2001) McGraw-Hill, New York Ch 225.
M O’Rourke, R Kelly, A Avolio, The arterial pulse. (1992) Lea & Febiger, Pennsylvania .
M Porkert, The essentials of Chinese diagnostics. (1983) Acta Medicinae Sinensis Chinese Medicine Publications, Zurich .
W Smith, Pulse diagnosis at UTS and VUT colleges of acupuncture student clinics [BAppSc]. (1996) University of Technology Sydney, Sydney .
JC Stettler, P Neiderer, M Anliker, Nonlinear mathematical models of the arterial system: effects of bifurcations, wall viscoeleasticity, stenoses, and counterpulsation on pressure and flow waves, In: (Editors: R Skalak, S Chien) Handbook of bioenginnering (1986) McGraw-Hill, New York; Ch 17.
In: (Editor: S Strandring, et al.) Gray’s anatomy: the anatomical basis of clinical practice 38th edn. (2005) Churchill Livingstone, Edinburgh.
G Tortora, S Grabowski, Principles of anatomy and physiology. 8th edn. (1996) Harper Collins, New York .
H Xue, Y Fung, What Nei Jing and Mai Jing say about arterial pulse waves and our attempt to illustrate some of their statements, Journal of Biomechanical Engineering 111 (1989) 88–91.
H Xue, Y Fung, Persistence of asymmetry in nonaxisymmetric entry flow in a circular cylindrical tube and its relevance to arterial pulse wave diagnosis, Journal of Biomedical Engineering 111 (1989) 37–41.