6 The Progressive Peel
The Combined Jessner, TCA, Retinoid Peel
Introduction
In our evolution of chemical peeling for all skin types we have developed the progressive peel. This is a multiple coat peel in four steps, allowing the operator to watch the skin and adjust the peel to the skin’s reaction. Some patients will require three or four coats of each progressive peel solution I, II, III and IV. Other patients will develop the end point of the rosy red hue with a white frost with several coats of progressive peel I or II. This gradual progression of the peel allows the operator to stop at a safe end point. The step-by-step process avoids alabaster white, yellow or grey frost that may occur with high concentrations of TCA (45–55%) applied in one or two coats. Historically, the suggestions of other progressive peelers still apply (Box 6.1).
Box 6.1
Suggestions from Eller and Wolff – (1941)
This chapter will be an overview of this progressive peel. We outline the step-by-step skin rejuvenation program (Box 6.2) for the improvement of complexion problems, fine lines and/or blotchy dyspigmentations in 155 patients. This illustrates what types of patients will benefit from the progressive peel. Afterwards, you will be able to conduct your patients through this step-by-step program to a freshened complexion. Previous authors in this textbook have also discussed skin preconditioning before the peel and more penetrating peels are covered in later chapters (see Box 6.3).
Box 6.3
Key features
Method
• Patient selection
Skin Analysis
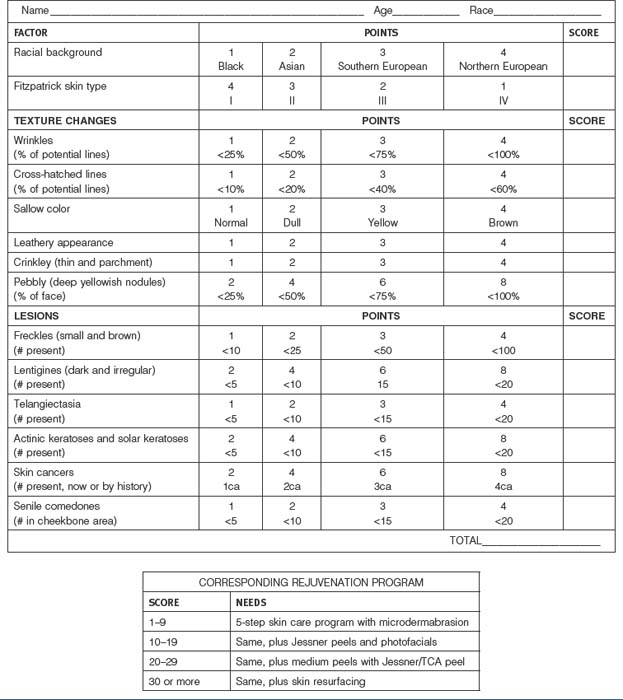
The skin analysis is the starting point for this rejuvenation process. The patient is classified by their Fitzpatrick skin type, plus, the extent of wrinkling, blotchy dyspigmention, sallow color, telangiectasia, pebbly appearance and the presence of skin lesions such as actinic keratoses. The overall score dictates the extent of skin rejuvenation required (Box 6.4). These findings correlate with the Rubin photo aging index. Rubin Level I is characterized by epidermal findings that maybe corrected with an aggressive topical skin care program alone. Rubin Level II is associated with papillary dermal findings which require a daily skin care program plus the progressive peel. Ruben Level III is with reticular dermal level changes which may require deeper rejuvenations such as laser resurfacing, dermabrasions or phenol peels. These will be covered in later chapters.
Informed Consent
The risks and benefits of this step-by-step skin rejuvenation program and the risks and benefits of alternative treatments including no treatment at all are discussed with the patient. All their questions are answered. These peels are contraindicated in some patients (Box 6.5). The degree of skin damage is determined and further documented with digital photography. Each patient signs the informed consent.
• The step-by-step skin rejuvenation program (Box 6.2)
Steps II and III will continue for 4 to 16 weeks depending upon the skin type (Box 6.6) For example, the skin conditioning must be longer in the darker skin types to reduce the possibility of dyschromias.
• The progressive peel
Tray Setup
A standard tray set up is important so nothing will be missed (Figure 6.1). Well-marked containers are used for the four peel solutions. Folded 3″ × 3″ cotton gauze is used to scrub in the chemical solutions. Five or six mL of each solution is poured onto the gauze which is rung out before the application begins sp the solution does not drip, cotton tipped applicators are available for small areas that require touch-ups or for around the eyes or temple areas. An eye wash solution is always on the tray to irrigate the eyes, if necessary. A bottle of water is on the tray to remind the patient to drink 4 or 5 glasses during the day to flush out any penetrating chemicals.
The Progressive Peel: Step I
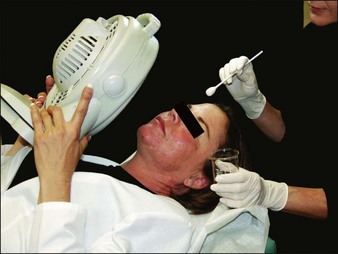
We use the modified Jessner solution both to clean the face and to treat the complexion at the same time. Others will use Septisol® and acetone cleansers before the application of the Jessner solution. We do not use these additional cleansers; yet, the endpoint of the erythematous blanch remains the same. As the moistened gauze of lactic acid, salicylic acid and citric acid is applied on the hair line of the forehead the operator talks the patient through the procedure. The patient controls the fan and is told to hold it close to the face if the burning sensation becomes too intense (Figure 6.2). The application of these peels progresses from the forehead to the cheeks and, then to the center of the face and across the chin, lips, and nose. Three or four coats are applied until moderate erythema develops or the burning sensation becomes intense. The patient continues with the fan for several minutes until the burning sensation fades. To avoid salicylism the patient is well hydrated with fluids and the surface area of the peel is limited to a face, neck and décolleté. The patient drinks a glass of water between steps. (See the video presentation for the actual steps of the procedure.)
The Progressive Peel: Steps II and III
If no significant erythema or blanching has occurred the operator advances to step II. The TCA 7.5% and salicylic acid 2% solution is applied in the same fashion as in step I. After three or four coats the operator observes for erythema and blanching. The patient relates to the operator the extent of the burning on a scale of 1 to 10 and holds the fan accordingly. A significant erythema, blanching or burning sensation indicates the end of step II. If this has not developed, the operator progresses to apply the solution of step III: TCA 15% and salicylic acid 4% in multiple coats. Blanching will usually occur after two or three applications (Figure 6.3).
• Post peel procedures
The patient is told to drink an additional four glasses of water during this initial day and to wash off the retinoid in the shower four to five hours later with a mild cleanser. No occlusive ointments are applied until three days later when the peeling begins. However, the patient can use a light moisturizing cream or sunscreen the next day. The desquamation always begins in the perioral area and progresses across the face to the hairline (Figure 6.4). At that point the peeling edge is kept moist with the application of an aloe vera, petrolatum-based recovery ointment (Recovery Ointment, Vivant Pharmaceuticals, Miami FL). The patient is allowed to cut off excessive scale and moisturize but they are told not to pull or pick off this scale as this manual debridement may damage the new skin and result in reactive hyperpigmentation. A sunscreen-based moisturizer is applied to the new skin for several days until the skin can tolerate the gradual reimplementation of the skin care program. In patients with dyschromias, the application of a bleach cream is started around post peel day 8 or 9 in an attempt to block the dyspigmentation on day 17 to 20.
Results
Several cases studies will illustrate our results.
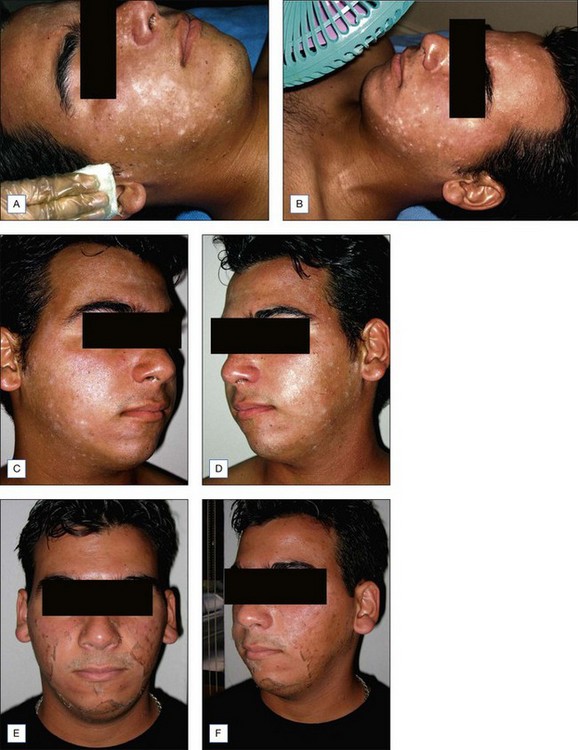
• Case study 1: acne vulgaris
This 17-year-old patient had developed acne at age 12 years on the nose, chin and forehead. As the condition progressed out across the face it became more inflammatory. Even with his daily skin care program he was unable to control the flare-ups. With the addition of two progressive peels his condition was controlled (Figure 6.5).
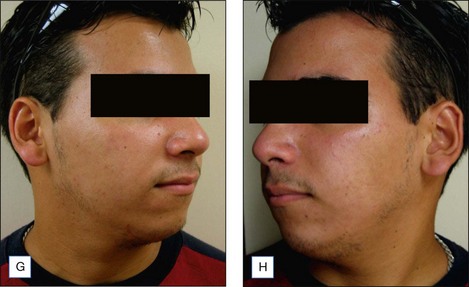
• Case study 2: dyspigmentations
This 28-year-old patient developed melasma after her pregnancies. The condition was only slightly improved with her skin bleaching program. With the addition of progressive peels to her program the melasma improved to the point it could be easily covered up with make-up (Figure 6.6).
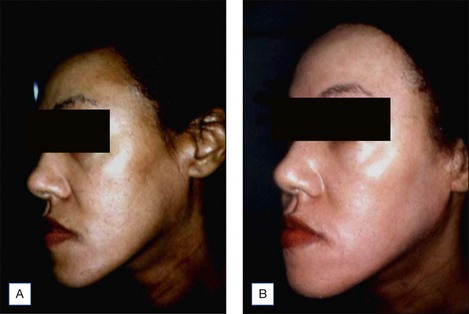
• Case study 3: photoaging
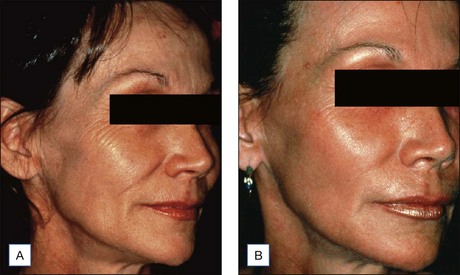
This 42-year-old patient had begun to develop fine lines. Although, there was some improvement with botulinum treatments and a skin care regimen the most dramatic improvement came after three progressive peels (Figure 6.7).
• Case study 4: actinic keratosis
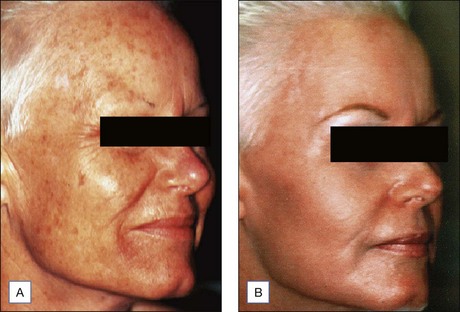
This 53-year-old flight attendant was developing multiple actinic keratosis. She began the conditioning program with buffing grains, toners and vitamin A conditioning lotions. In addition, she underwent three progressive peels. The most prominent elevated keratotic lesions were treated individually with several additional coats of step III solution on a cotton swab (Figure 6.8).
Brubacher JR, Hoffman RS. Salicylism from topical salicylates: Review of the literature. Journal of Toxicology Clinics. 1996;34:431-435.
Cook KK, Cook WR. Chemical peel of nonfacial skin using glycolic acid gel augmented with tca and neutralized based on visual staging. Dermatological Surgery. 2000;26:994-999.
Eller JJ, Wolfe S. Skin peeling and scarification. Journal of the American Medical Association. 1941;116:934-941.
Fulton J, Porumb S. Chemical peels: their place within the range of resurfacing techniques. American Journal of Clinical Dermatology. 2004;5:1-9.
Kligman DE, Draelos ZD. High-strength tretinoin for rapid retinzation of photoaged facial skin. Dermatological Surgery. 2004;30:864-866.
Rubin MG. Manual of Chemical Peels: Superficial and Medium Depth. Philadelphia: Lippincott, William and Wilkins; 1995.