Chapter 7. The principles of managing trauma
Fractures
Trauma and fractures are not the same thing. When a limb is broken, every tissue in it is damaged. The fact that the bony injury is the only one visible on the radiograph does not make it the most serious. Radiographs do not show severed nerves, crushed muscles, ruptured blood vessels or torn ligaments, any more than they tell whether a wound is contaminated, how the injury occurred or how it should be treated.
The severity of an injury is greatly influenced by the violence of the impact. A leg broken by a car travelling at 95 km/h (60 m.p.h.) will be more seriously injured than one broken by tripping over the cat (Fig. 7.1). In the high speed injury there will be damage to all the soft tissues as well as bone, and possibly damage to the blood vessels. The bone ends will be crushed and devitalized, nerves stretched or severed, and muscles crushed. Although the bone may unite soundly and in good position, so that it is even stronger than before the injury, damaged muscles cannot be restored, and severed nerves will never be the same, however meticulously they are repaired.
 |
| Fig. 7.1
Violence of impact. Cats cause less damage than cars.
|
To understand the damage to the soft tissues, imagine the position of the limb at the moment of impact when the bone ends were widely separated (Fig. 7.2). By the time the patient reaches hospital, the soft tissues will have bounced back almost to their normal position and the radiographs give no indication of the extent to which the soft tissues were stretched. This is not a difficult concept, yet inexperienced casualty officers frequently decide how to treat a patient just by examining the radiograph and this can lead to disaster.
 |
| Fig. 7.2
Displacement of fragments. Soft tissues recoil and pull bone fragments back together after an impact. Try to imagine how the fragments and soft tissues must have been at the time of greatest displacement.
|
Even if the fracture is treated correctly in the accident department, soft tissue injuries can still spoil the result of the finest fracture management. This is easily forgotten when the patient is sitting in the fracture clinic with an injured limb hidden inside a cast. If the radiographs look normal it might be imagined that all that needs to be done for the limb to work normally again is to remove the cast. This is not so.
Fracture management can therefore be divided into three phases. Early management is directed to converting contaminated wounds to clean wounds, and the second stage to joining together those things that have broken, notably bone. The third stage consists of separating those things that have stuck together but should be separate, particularly muscles and joint surfaces.
There is no point in achieving a perfect radiograph with solid bone if the muscles cannot operate the joints. On the other hand, it is equally bad to start early rehabilitation and produce excellent muscles around a malunion. A balance must be struck between these two conflicting aims. The correct approach is to start mobilization and vigorous physiotherapy as soon as it is safe to do so, but to choose the right moment takes experience.
Recognizing a fracture
The physical signs of a fracture
• Abnormal movement in a limb due to movement at the fracture site.
• Crepitus or grating between the bone ends.
• A deformity that can be seen or felt.
• Bruising around the fracture.
• Tenderness over the fracture site.
• Pain on stressing the limb by bending or longitudinal compression.
• Impaired function.
• Swelling at the fracture site.
Although it is usually easy to know when a bone is broken, it is surprisingly easy to miss a fracture and some are notorious for the number of times they escape recognition.
If either of the first two signs on the list above are present, there is a fracture, but these signs are absent if the ends are impacted. Undisplaced fractures cause no deformity, bruising can take hours to appear and unconscious patients cannot report pain or tenderness.
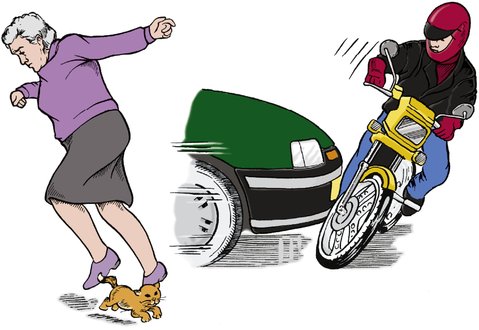
The following fractures are often missed (Fig. 7.3):
 |
| Fig. 7.3
The fractures that most often escape diagnosis.
|
1. Impacted fractures of the femoral neck.
2. Fractures of the ribs.
3. Fractures of the skull, particularly the base of the skull.
4. Facial fractures, particularly the zygoma.
5. Fractures of the radial head.
6. Fatigue fractures before the callus has appeared.
7. Fractures of the scaphoid.
8. Fracture dislocations of the carpus, particularly the lunate.
9. The seventh cervical vertebra.
10. Undisplaced fractures of the pelvis.
11. Fractures of the odontoid.
12. Fracture dislocations of the tarsometatarsal joint.
13. Fracture of the talus.
Natural history of fractures
Grass grows without gardeners and bones unite without orthopaedic surgeons. Like a gardener, the orthopaedic surgeon tries to make nature’s task easier, but nothing will ‘make’ a bone unite if the circumstances are not right.
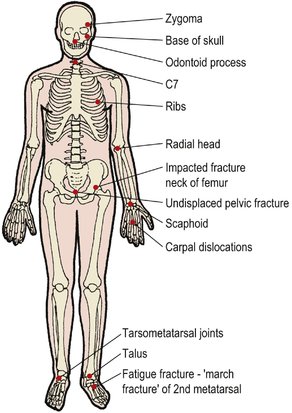
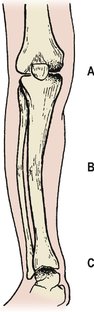
Untreated, fractures can do one of several things. At best, they unite soundly in good position to give a perfect result, but they may be slow to unite ( delayed union), fail to unite at all ( non-union) or unite in the wrong position ( malunion) (Fig. 7.4).
 |
| Fig. 7.4
(a) Malunion; (b) non-union; (c) delayed union.
|
There is no hard and fast rule to say how any one fracture will behave without treatment but, in general, fractures in cancellous bone unite soundly and non-union is seldom a problem, although there may be malunion. In contrast, the long bones are susceptible to non-union, particularly if there is poor blood supply to the bone ends as a result of extensive soft tissue damage.
Patients are, understandably, very eager to know how long their bone will take to join, but fractures unite gradually and the question ‘Has the fracture joined yet?’ is impossible to answer. A bone is only united when it is strong enough to take its normal load; this varies from bone to bone, but a good rule of thumb is to say that most bones join in 8 weeks, lower limb bones take twice as long and fractures in children take half as long.
A very rough guide to fracture healing
Bones join in 8 weeks, but double this in the lower limb and halve it for children.
Fracture healing
The healing of bone explains the clinical behaviour of a uniting fracture. Immediately after the fracture the bone ends rub together and cause crepitus, which is distressing to the patient. After about 14 days, fibrous tissue has replaced the blood clot between the bone ends and the crepitus ceases but the fracture remains mobile.
At about 4 weeks the fracture becomes ‘sticky’ and movement is less obvious. During the next 2 months the bone becomes solid but not always strong enough to do all that is asked of it, particularly if it is a weight-bearing bone in the lower limb.
As healing proceeds, the mass of tissue around the fracture becomes hard and produces a fusiform callus. Patients are often alarmed by the swelling and think they have cancer. They must be reassured that it is a sign of good fracture union. The callus never disappears completely but becomes smaller with time as the soft tissue swelling around it diminishes and remodelling occurs.
Malunion
The term malunion is applied to a bone that has united soundly but in the wrong position (Fig. 7.5). This sounds alarming but does not always matter greatly. Fractures of the clavicle almost always unite with a little shortening and overlap, which is quite acceptable and does not affect the functional result, but in fractures where the fragments are pulled apart by the unopposed action of different muscle groups, the functional result of malunion is poor.
 |
| Fig. 7.5
Non-union, malunion and cross-union. This patient had non-union of the tibia, malunion of the fibula and cross-union between the two.
|
Cross-union. Cross-union, in which two adjacent bones become linked by new bone, is a variety of malunion. Cross-union in the forearm blocks pronation and supination.
Non-union
If the healing process fails, the bone ends do not unite and remain separate. This is a serious problem in a weight-bearing bone but may cause less disability in other situations, such as a fractured metacarpal. Two types of non-union are seen: (1) hypertrophic, and (2) atrophic.
Hypertrophic non-union is characterized by a massive cuff of bone around the ends of the fractures that looks a little like an elephant’s foot (Fig. 7.6a). These fractures are trying desperately to heal and can be helped to do so by realigning the limb and preventing movement between the bone ends. Prevention of movement can be done by rigid internal fixation, or intramedullary or extramedullary stabilization.
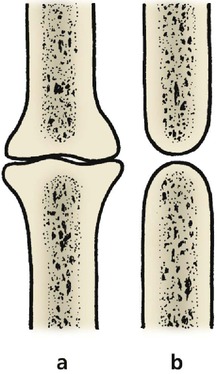 |
| Fig. 7.6
Shape of bones in (a) hypertrophic non-union and (b) atrophic non-union.
|
Atrophic non-union shows rounding of the bone ends (Fig. 7.6b), sometimes so marked that the tips of the bone ends resemble pencils, and the medullary cavity may be closed. This is indicative of a poor blood supply to the bone ends.
A pseudarthrosis forms in some patients (Fig. 7.7). If there is no sign of osteogenesis, treatment must aim to ‘kick start’ this by bone grafting with fresh cancellous bone or marrow.
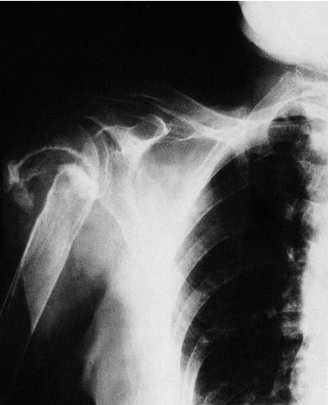 |
| Fig. 7.7
Non-union of a fracture of the surgical neck of the humerus. A pseudarthrosis has formed at the site of the fracture.
|
Delayed union
A fracture with delayed union takes longer to unite than normal but eventually does so. It is important to distinguish delayed union from non-union, as delayed unions will unite with time and attention to correct immobilization of the fracture fragments. Non-unions, however, may need operative intervention in order to allow the bone ends to unite. Separation of the two types can be difficult. Unless there are positive signs of non-union, such as closing of the medullary cavity of the fragments, which makes the diagnosis easy, or an improvement between one radiograph and the next, diagnosis rests on comparing the rate of bone union with the normal rate of healing of a fracture in the same situation.
Classification of fractures
Simple and compound
Fractures can be classified in many ways but the simplest and most practical was the ancient classification of the old military surgeons who regarded all fractures as simple or compound.
Open and closed
Modern treatment of ‘compound’ fractures is so effective that the term is no longer applicable. Apart from this, fractures with intact skin can be far from ‘simple’ to treat and ‘compound’ may be confused with complicated, comminuted or multiple. ‘Simple’ and ‘compound’ have been replaced by ‘ closed’ and ‘ open’ but ‘compound’ is sometimes used to describe how the skin has been damaged (Fig. 7.8). A fracture in which the skin has been penetrated by a bone fragment from inside the leg is sometimes referred to as ‘compound from within’ to distinguish it from a true open fracture and to emphasize the potential danger.
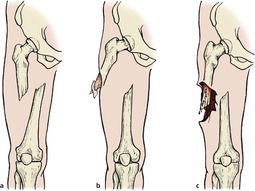 |
| Fig. 7.8
Open and closed fractures: (a) closed fracture; (b) ‘compound from within’; (c) an open fracture with contamination.
|
Shape
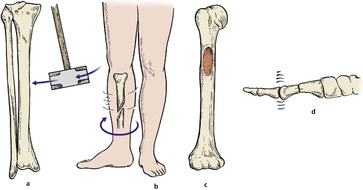
Fractures can also be classified according to the shape of the fragments and this is helpful in deciding management (Fig. 7.9).
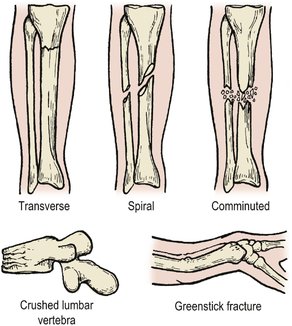 |
| Fig. 7.9
Patterns of fracture.
|
Transverse fractures are the result of a direct blow or a pure angular force applied to the bone. The shape of the bone ends helps transverse fractures to stay aligned more easily than fractures which do not fit together so neatly.
Oblique or spiral fractures. Most long bone fractures are caused by a violent twisting movement about the long axis of the bone rather than the sideways bending which causes a transverse fracture. A sharp twist to the leg while the foot is stuck in a rabbit hole produces a spiral fracture of the tibia, even if radiographs suggest that the fracture line is oblique. In fact, oblique fractures are rare and are almost always a radiological artefact.
The fragments of a spiral fracture are more difficult to balance against each other than the square end of a transverse fracture and are very unstable. The bone spikes damage blood vessels, nerves or skin and the tips of the spikes can themselves break off to produce a triangular fragment known as a ‘butterfly’ fragment.
Crush fractures. A fracture in which cancellous bone is squashed or crushed presents a difficult problem because there are no fragments left to manipulate back into position. If the fracture site is opened up and the cortex of the bone replaced in its normal position, a large cavity remains and the bone can only be restored to its normal shape by packing the space with bone graft or holding the sides of the cavity apart by external fixation.
Crush fractures are typically seen in the lumbar vertebrae, tibial plateaux and calcaneum.
Greenstick fractures. When a green stick breaks, it does not snap cleanly but bends so that one ‘cortex’ buckles while the other remains intact. If the force is very great, one side may snap while the other remains intact – try it. If a green stick fractured in this way is straightened it bounces back slightly but will not hold its correct position.
Fractures of long bones in children behave in the same way. The compressed cortex first buckles to produce a ‘buckle’ fracture. If the force continues, the cortex under tension will fracture (Fig. 7.10). Because of the resilience of the bone, reduction is only possible if the fracture is made complete or if three-point pressure (p. 127) is applied. Fortunately, fractures in children remodel well enough to restore the normal anatomy and the deformity of most greenstick fractures can be accepted.
 |
| Fig. 7.10
A greenstick fracture of the radius with buckling of the dorsal cortex and a crack in the anterior cortex.
|
Mechanism of injury
Fractures can be caused in several ways (Fig. 7.11).
 |
| Fig. 7.11
Mechanism of injury: (a) direct violence; (b) indirect violence; (c) pathological through a tumour; (d) fatigue.
|
Direct violence
Bones can be broken by a direct blow and many patterns are seen. A sharp blow on the front of the knee may shatter the patella into many small fragments held together by soft tissue, like a boiled sweet broken in its wrapper (p. 254), but the fragments of a tibia fractured in a road traffic accident will be widely separated.
Indirect violence
More fractures are caused by indirect violence than direct violence. In this type of trauma, usually a twisting injury, no violence is applied to the site of the fracture itself. Open fractures are therefore uncommon, although the bone fragments can penetrate the skin from inside, making the fracture ‘compound from within’.
Pathological fractures
Pathological fractures occur through abnormally weak bone. Tumours, cysts and osteoporotic bone are common sites of pathological fractures (Fig. 7.12).
 |
| Fig. 7.12
Pathological fracture (a) through a metastasis in the humerus; (b) of the tibia through porotic bone.
|
Fatigue fractures
Repeated small bending stresses will break any material (Fig. 7.13), including bone. The commonest example is a fracture of the second metatarsal in young adults who walk excessive distances. Classically, military recruits suffered this injury after route marches and the fracture is still known in English as a ‘march fracture’ and in French as ‘ pied du jeune soldat’. Fatigue fractures are also seen in the tibiae of long-distance runners and hurdlers, and in the pars interarticularis of fast bowlers and javelin throwers.
 |
| Fig. 7.13
Healed fatigue fracture through the second metatarsal – a ‘march fracture’.
|
Other terms (Fig. 7.14)
Undisplaced fractures
The fragments in an undisplaced fracture are in almost anatomical position and manipulative reduction is not required.
 |
| Fig. 7.14
Terms used to describe fractures: (a) undisplaced; (b) impacted; (c) stable; (d) fracture with complications.
|
Impacted fractures
If cancellous bone is compressed in its long axis the two bone ends are so firmly thrust together that the fracture is stable unless the fragments are pulled apart. On a radiograph, the impacted bone is seen as an area of increased bone density – the opposite of a normal transradiant fracture line, and easily missed. Occasionally, impacted fractures become disimpacted after a few days, producing a troublesome deformity and a difficult clinical problem that requires careful explanation to the patient.
Segmental fractures
Segmental fractures are those in which a long bone is broken in two places, creating a large free segment of bone that is not attached to the rest of the skeleton. The free fragment is difficult to hold without internal fixation.
Stable fractures
A stable fracture is one in which the two bones are lying in a position from which they are unlikely to move. Stable fractures are often undisplaced but some are stable even though the bone is misshapen.
Complicated fractures
A complicated fracture is one that has a complication, such as infection or vascular damage. The term is seldom used but must be distinguished from compound and comminuted.
Multiple fractures
This term is applied when there are several separate fractures in the same patient. It is not to be confused with a comminuted or compound fracture.
Epiphyseal injury
Injury to the epiphyses of growing bone can cause severe deformity in later life if a bony bridge forms across the fracture site and prevents growth on one side of the bone.
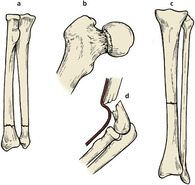
The following five patterns of injury (Fig. 7.15) were described by Harris and Salter:
1. A fracture along the epiphyseal line.
2. Separation of the epiphysis with a triangular fragment of shaft attached to it (Fig. 7.16).
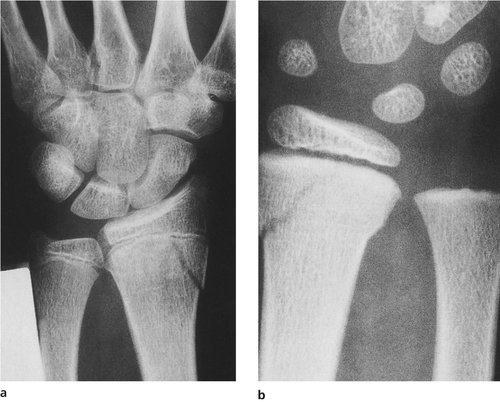 |
| Fig. 7.16
A type 2 Harris and Salter fracture: (a) of the lower radial epiphysis; (b) with the slight variation of a greenstick buckle on the intact cortex.
|
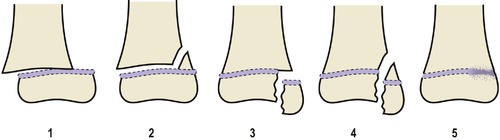 |
| Fig. 7.15
Harris and Salter classification of epiphyseal injuries: (1) epiphyseal slip only; (2) fracture through the epiphyseal plate with a triangular fragment of shaft attached to the epiphysis; (3) fracture through the epiphysis extending to the epiphyseal plate; (4) fracture through the epiphysis and shaft crossing the epiphyseal plate; (5) obliteration of the epiphyseal plate.
|
3. Fracture of the epiphysis, part of it remaining attached to the shaft.
5. A crushing injury (Fig. 7.17). This is difficult to recognize at the time of injury, either clinically or radiologically. This type of injury is more commonly associated with later growth arrest or retardation.
 |
| Fig. 7.17
Growth arrest in the anterior part of the upper tibial epiphysis following trauma.
|
Students often have difficulty in accurately describing fractures seen on a radiograph. As already mentioned, there are a number of terms used and these can be confusing. You might find it useful to imagine that you are describing the radiograph to someone on the other end of a telephone line and they obviously do not have the advantage of looking at the film. You cannot, therefore, point at the fracture or the bone and instead you have to have a method of accurate description.
A useful method is to go through the following steps:
1. This is an X-ray of … (and describe which bone and which patient).
2. There is a … (transverse/oblique/spiral/convoluted/segmental/greenstick, etc. type of fracture).
3. Of the … part of bone (e.g. midshaft of the tibia).
You should then describe the degree of displacement or the angulation of the distal segment.
You will not be able to state with certainty from looking at the film whether the fracture is open or closed, but this will be readily apparent when you examine the injury in detail.
Complications
As elsewhere, the complications of fractures and soft tissue injuries can be classified in two ways:
1. Immediate – within a few hours
Early – within the first few weeks
Late – months and years later.
2. Local
General.
Immediate complications
Haemorrhage
Bones are vascular structures and bleed when they are broken. Apart from blood lost from the bone itself, the sharp ends of the bone can damage the surrounding muscle or the blood vessels, and severe blood loss can occur into the soft tissues (Table 7.1).
| Units (litres) lost | ||
|---|---|---|
| 1–3 (0.5–1.5) | 2–4 (1–2.5) | 3–5 (1.5–3) |
| Tibia | Femur | Pelvis |
| Ankle | Knee | Hip |
| Elbow | Shoulder | |
| Forearm | Humerus | |
The normal blood volume is about 5 litres or 8 units, and serious problems occur if more than one-third of the blood volume is lost from the circulation. From this, it follows that patients with two fractured femora or a fractured pelvis can go into hypovolaemic shock or exsanguinate unless prompt action is taken. It is possible for a patient to bleed to death from a fracture without a drop of blood leaving the body.
Damage to arteries
The arteries most commonly damaged at the moment of injury are:
• The middle meningeal artery in temporoparietal skull fractures.
• The brachial artery in supracondylar fractures of the humerus in children.
• The popliteal artery in fractures and dislocations at the knee.
• The aorta in fractures of the 4th and 5th thoracic vertebrae.
• The femoral artery in fractures of the femur.
Damage to surrounding structures
Serious problems can also arise from damage to neighbouring structures:
• Broken rib – perforated lung – pneumothorax.
• Fractured sternum – ruptured aorta – exsanguination.
• Broken ribs – ruptured liver – exsanguination.
• Broken neck – paraplegia with paralysis of phrenic nerve (C3, 4, 5) – asphyxia.
• Broken skull – brain damage.
• Fractured face or mandible – obstructed airway – suffocation.
Viscera. Complications also arise from damage to the surrounding viscera and a complete list would be endless. Only by awareness can potential complications be anticipated and avoided.
Early complications
• Wound infection.
• Fat embolism.
• Shock lung.
• Chest infection.
• Disseminated intravascular coagulation.
• Exacerbation of generalized illness.
• Compartment syndrome.
Wound infection
Wound infection from open fractures can lead to septicaemia and tetanus or gas gangrene from anaerobic infection.
Fat embolism
Fat embolism is an uncommon complication which leads to hypoxia from pulmonary insufficiency. The likelihood of developing fat embolism syndrome is not proportional to the severity of the injury and death can occur from an apparently straightforward transverse fracture of the tibia with little displacement. At postmortem examination, the alveoli are found to be crammed with small fat globules.
Cause. Two mechanisms have been suggested. The most obvious is direct embolization of fat globules from the fracture site, but this is too simple an explanation. The alternative is that circulating triglycerides split into glycerol and fat, generating many small particles of circulating fat. Whatever the cause, the hypoxia of fat embolism syndrome is a serious problem and there is no effective prophylaxis.
Clinical features. These are as follows:
1. The patient shows signs of hypoxia, including a change of mood, drowsiness and eventually loss of consciousness.
2. There is tachypnoea.
3. Petechiae are seen.
Investigations. These reveal that:
1. The arterial PO 2 is low.
2. Chest radiographs show patchy consolidation (Fig. 7.18).
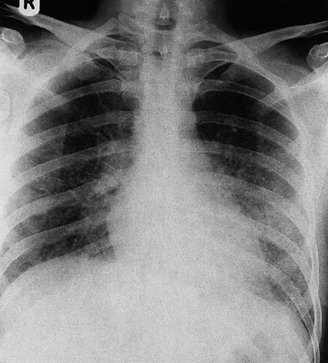 |
| Fig. 7.18
Patchy consolidation of the lungs in fat embolism.
|
3. The platelet count is low.
4. Serum lipase is raised.
5. Fat globules may be present in the urine.
Treatment. Once established, oxygen is the mainstay of treatment, and assisted ventilation may be required. Systemic and intratracheal steroids may be useful.
Shock lung
Shock lung, also known as wet lung or adult respiratory distress syndrome, can follow slight fluid overload and is made worse if there is any damage to the lungs, aspiration into the lung or over-transfusion. Oedema and electrolyte retention secondary to the trauma also contribute to the adult respiratory distress syndrome, described in more detail on page 173.
Treatment is by oxygen and ventilation. Do not over-transfuse with crystalloids!
Chest infection
Chest infection can be fatal in the elderly patient or patients with shock lung. Early mobilization and vigorous chest physiotherapy are the best prophylaxis.
Diffuse intravascular coagulation
Diffuse intravascular coagulation (DIC) can follow any injury and is due to a disturbance of the clotting mechanism. The help of the haematologist is needed in treatment, which may require fresh frozen plasma or platelets, and heparin.
Exacerbation of generalized illness in unfit patients
Diabetes, chest disease, coronary insufficiency and any other pre-existing problem can be exacerbated by a fracture.
Compartment syndrome
See page 112.
Infection
Orthopaedic textbooks of the 19th century describe infections of closed fractures, presumably from a bacteraemia, with the patients dying of septicaemia. This complication is, thankfully, rarely seen in modern times.
Late complications
• Deformity.
• Osteoarthritis of adjacent or distant joints.
• Aseptic necrosis.
• Traumatic chondromalacia.
• Reflex sympathetic dystrophy.
Late complications include malunion, non-union and delayed union, which are dealt with elsewhere (pp. 96–97).
Deformity
Deformity due to malunion may require late correction. Angular deformities greater than 5° can cause degenerative arthritic changes in the joints above and below the fracture. When treating a broken bone it is important, therefore, not to accept an angular deformity unless there is a real possibility that the fracture will remodel. Patients less than 9 years of age with a deformity close to the growth plate and in the axis of joint movement may remodel the fracture over a period of 1–2 years but remodelling in other planes, and in older patients, is much less satisfactory.
Deformities can be corrected by an osteotomy with fixation of the bone or by angular corrections using external fixators and bone lengthening techniques (p. 82). These limb-lengthening techniques can also be used to correct shortening as a result of bone loss, etc.
Where there is a large bony defect or an established non-union, bone can be grown across the defect to unite with the distal bone segment (bone transport). This technique of distraction in healthy bone, transportation of normal bone across the defect and subsequent union to the distal segment has been performed using a ring fixator or a conventional external fixator frame. Slow angular corrections using a circular frame can realign the limb in three planes at the same time. A conventional external fixator applied to the side of the bone alone may only correct the rotational abnormality in two planes at best.
Osteoarthritis of adjacent joints
Joint surfaces broken at the time of the fracture are much more likely to develop osteoarthritis than is an intact joint because of abnormal mechanical wear on the rough joint surfaces.
Osteoarthritis of distant joints
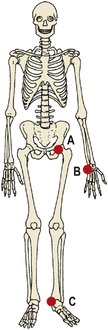
The joint surface does not have to be broken for osteoarthritis to develop (Fig. 7.19). If there is a malunion of the tibia, excessive load will be taken by both the knee and the ankle, and this causes early degenerative change. The same mechanism damages distant joints. If the leg is short after a fracture, the patient will walk with a tilt to one side, compensated for by a curve in the spine. This causes excessive wear on the facet joints on the side opposite the fracture and degenerative osteoarthritis will follow.
 |
| Fig. 7.19
Complications of malunion: ( A) osteoarthritis of the knee; ( B) deformity at the fracture site; ( C) osteoarthritis of the ankle.
|
Aseptic necrosis (avascular necrosis)
If the fracture interrupts the blood supply to bone the affected bone dies, the bone collapses, the joint is destroyed and the patient develops a stiff and painful joint.
Aseptic necrosis often takes 2 years to develop, and it cannot be excluded until then. This is important if the injury is the subject of litigation. If a patient with an excellent result 12 months after injury is reassured that there has been a perfect recovery and settles the claim on this basis, he or she will be very disappointed if aseptic necrosis develops 12 months later.
Aseptic necrosis is common in bones that derive most of their blood supply from the medullary cavity rather than the surrounding soft tissues or periosteum. Three bones are particularly susceptible (Fig. 7.20):
 |
| Fig. 7.20
Common sites of aseptic necrosis: ( A) femoral head; ( B) scaphoid; ( C) talus.
|
• The femoral head following a femoral neck fracture.
• The scaphoid – the proximal pole of the scaphoid, because the blood supply of the scaphoid often enters through the distal pole.
• The head of the talus, because the blood supply enters through the sinus tarsi and the neck of the talus. If the neck of the talus is broken, aseptic necrosis of the body will occur.
Radiologically, the affected bone appears denser than the surrounding bone for three reasons:
• Bone collapse, which packs the calcified tissue into a smaller area.
• Disuse osteoporosis – because there is no blood supply the calcium cannot be removed from the dead bone, but the surrounding bone suffers disuse osteoporosis and is decalcified. This makes the living bone appear denser on the radiograph.
• Calcium deposition – calcium salts from the extracellular fluid are deposited on the dead bone, as they are on any dead or foreign material.
Traumatic chondromalacia
Articular cartilage may be damaged by a blow that leaves the bone intact. The articular cartilage softens and eventually disintegrates. The patient is aware of pain and crepitus, which may take as long as 2 years to develop. Once established, traumatic chondromalacia is likely to be followed by osteoarthritis. Injuries to the patella are the commonest cause of traumatic chondromalacia.
Reflex sympathetic dystrophy
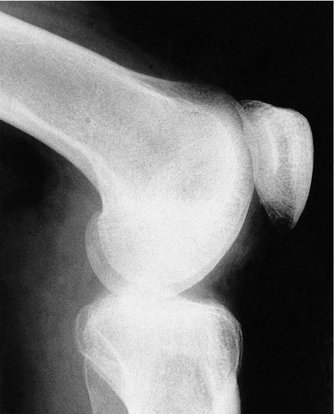
Reflex sympathetic dystrophy is a curious condition similar to causalgia. It affects bone and can follow any injury, particularly a fracture. The clinical features are that the skin feels cold, goes blue or changes colour, and the limb is excruciatingly tender. The patient cannot move the limb normally and in severe cases the skin is thin and shiny. Radiologically, there is patchy osteoporosis (Fig. 7.21).
 |
| Fig. 7.21
Reflex sympathetic dystrophy around the knee. Note the patchy osteoporosis in the patella and femoral condyles.
|
The mechanism of reflex sympathetic dystrophy is unclear but it is probably due to a perversion of the sensory fibres which interpret temperature change as a painful stimulus. This over-activity of the sympathetic nerves at the wrist is called Sudeck’s atrophy or algodystrophy.
Injuries to joints
Three grades of joint injury occur (Fig. 7.22):
1. Subluxation (partial dislocation).
2. Dislocation.
3. Fracture dislocation.
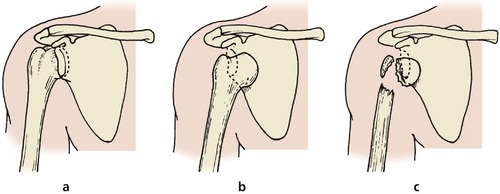 |
| Fig. 7.22
Types of injury to a joint: (a) subluxation; (b) dislocation; (c) fracture dislocation.
|
Subluxation
Joints that are subluxed, or where there is partial contact between joint surfaces, seldom need active treatment, and normal stability usually returns when the periarticular tissues have healed. If symptoms of instability follow, the joint may need to be stabilized.
Dislocation
Joints that have been completely dislocated (no contact between joint surfaces) must be treated more energetically than those that have subluxed. The joint must be reduced and immobilized until the soft tissues have healed, and some joints, such as the knee, may need open repair.
Complications. Dislocations may be followed by recurrent dislocation (recurrent dislocation of the shoulder, p. 365 and patella, p. 426), aseptic necrosis, chronic instability or osteoarthrosis if the joint surfaces are damaged.
Fracture dislocation
Dislocations accompanied by a fracture around the joint often heal more soundly than a simple dislocation because bone unites more soundly than ligament, but early management is more difficult. The bony fragment may become jammed in the joint, or the joint may be very unstable because bony congruity is lost.
Treatment often involves fixation of the bony fragment; management is described in the appropriate sections.
Injuries to ligaments
Three grades of ligament injury are recognized (Fig. 7.23):
1. Sprain, in which stability is maintained.
2. Partial rupture, in which there is some loss of stability but some fibres remain intact.
3. Complete rupture, with loss of both stability and continuity of the ligament.
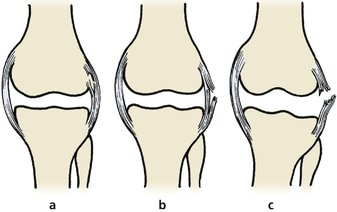 |
| Fig. 7.23
Grades of ligament injury: (a) sprain; (b) partial tear; (c) complete rupture.
|
Sprains
A sprain, or strain, is a partial tear of a ligament or joint capsule which does not make the joint unstable. The site of the tear is tender, there may be bruising, and the physical signs are similar to those of an undisplaced fracture.
Sprains are treated symptomatically but the joint must be protected from stress until healing is complete.
Partial rupture
Partially ruptured ligaments can be treated conservatively if it is certain that the rupture is incomplete. Cast immobilization for 6 weeks may be required but rest and analgesics are usually adequate. Recurrence is common.
Complete rupture
Ruptured ligaments do not heal soundly even if they are accurately repaired because the scar tissue that forms at the site of repair is never as tough as the original. Surgical repair is often attempted but conservative management may be equally effective.
Injuries to soft tissues
Blood vessels
Blood vessels can be damaged in four ways (Fig. 7.24):
1. Division.
2. Stretching.
3. Spasm.
4. Crushing.
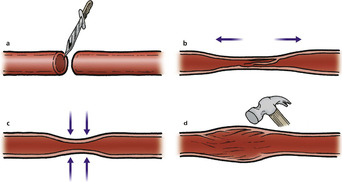 |
| Fig. 7.24
Types of injury to blood vessel: (a) complete division; (b) stretching, with intimal flap; (c) spasm; (d) soft tissue damage to the wall.
|
Complete division
Vessels can be completely divided by penetrating metal objects or the sharp ends of bones. This is a comparatively rare cause of vascular damage.
Stretching
If the deforming force continues after the bone is broken, the blood vessels and other soft tissues will be stretched. This can cause intimal damage, which may be complicated by intravascular clotting, and is common near the elbow and the knee.
Spasm
Spasm of blood vessels can follow intimal damage and is said to be especially common in supracondylar fractures of the humerus in children. Painting the artery with papaverine may relieve the spasm but any intimal damage must also be treated.
Crushing
Direct violence causes intimal damage and sometimes ruptures or severs the vessel completely.
Nerves
Neurapraxia, axonotmesis and neurotmesis are well known. Real-life injuries can seldom be classified so neatly.
Injuries to nerves
• Neurapraxia – transient loss of function caused by outside pressure. Early recovery.
• Axonotmesis – loss of function due to more severe compression but without loss of continuity of the neurone. Recovery in weeks or months.
• Neurotmesis – division of the nerve, no neural continuity. No recovery unless repaired.
Like blood vessels, nerves can be damaged by division, stretching or crushing, but most direct injuries to the nerve involve a combination of all three.
Only if the nerve is cleanly divided on a piece of glass or metal is it reasonable to attempt a precise surgical repair immediately after injury because of the problems of healing (p. 141). The common sites of damage to peripheral nerves are shown in Figure 3.24.
Ischaemia
Ischaemia also impairs nerve function; gradual loss of sensibility involving a whole limb should suggest the possibility of ischaemia. Compartment syndromes or direct pressure are the commonest causes.
Muscle
Muscle can be damaged in four ways:
1. Crushing.
2. Laceration.
3. Ischaemia.
4. Ectopic ossification.
Crushing
Muscle crushed by direct force heals with fibrous tissue, which shortens the muscle and restricts joint movement.
Laceration
Muscles divided transversely will not hold sutures well enough to stop muscular contraction pulling the edges apart. Fascia surrounding a muscle can be repaired, but the risk of a compartment syndrome (p. 112) makes this unwise.
Ischaemia
Muscle is very vascular and its blood supply is critical. If the blood supply is impaired by arterial damage, a compartment syndrome or a tight plaster, the ischaemic muscle is replaced by fibrous tissue which contracts and pulls the associated joints into an unnatural position. This is a real problem in fracture management.
Ectopic ossification
Ossification in the fracture haematoma is usually confined to the area around the bone, where it is most useful. Sometimes, however, ossification can occur in haematomas within the muscle belly, where it limits joint movement (Fig. 7.25). The quadriceps is a common site. The ectopic bone is sometimes gradually absorbed but, if it is not, severe restriction of the joint movement is likely. The bone can form again and excising it from the muscle belly is seldom helpful.
 |
| Fig. 7.25
Ectopic ossification within muscle following fracture.
|
Bone can also form around joints well away from muscle (Fig. 7.26). A large staghorn of bone may develop at the lower end of the humerus, its spikes wrapped tightly around vessels and nerves. The fragment can be removed and some movement restored but the operation is technically difficult.
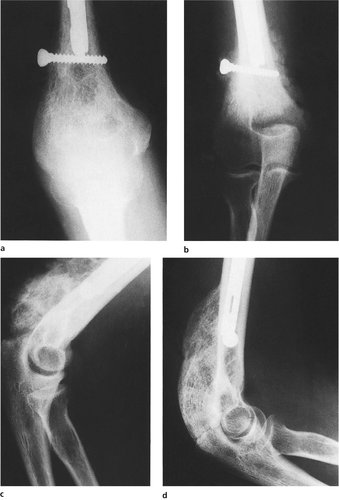 |
| Fig. 7.26
(a) Lower end of humerus immediately after internal fixation of fracture; (b) the same fracture 8 weeks later; (c) 12 weeks after fracture; (d) 12 months after fracture.
|
Both these types of ectopic ossification must be distinguished from myositis ossificans progressiva, a disease of unknown origin in which many muscles undergo ossification, and from the ossification seen around the joints of paralysed limbs.
Skin
Direct trauma
If a limb is hit hard enough to break bone, the skin at the point of impact is bound to be damaged. Fortunately, areas of skin damaged by direct trauma are small but they are always near the fracture site and make wound closure difficult.
Stretching
Like other soft tissues in a broken limb, skin is stretched at the moment of impact. The damaged skin may die but more often the stretching causes a transient ischaemia that leads to ‘fracture blisters’.
Fracture blisters form within 48 h of an injury and complicate internal fixation operations because they are a potential source of infection.
Degloving
If a limb is caught firmly and pulled violently at the moment of impact, the skin may be peeled back over the bones for a considerable distance, perhaps over the whole leg or forearm (Fig. 7.27). These injuries are called ‘degloving’ injuries but the same problems can arise just by the skin being stripped off the underlying tissues without being rolled back like a glove. This type of degloving is common in fractures of the tibia and fibula.
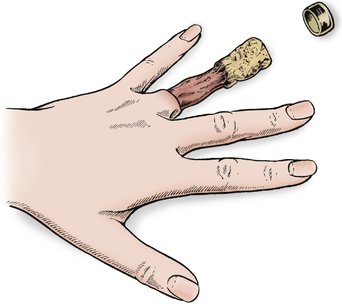 |
| Fig. 7.27
A degloving injury of the finger.
|
Treatment. Degloved skin is dead and should be replaced as if it were a free skin graft. If the replaced skin does not survive, the problem of skin cover is best dealt with by a plastic surgeon.
Operation
Skin that has survived the original injury may be damaged at operation, particularly if it is stripped unnecessarily widely from the underlying tissues or stitched too tightly.
If skin does not come together easily, stitch it loosely and close the wound by delayed primary suture (p. 140).
Viscera
Soft organs, such as liver, spleen, heart, lungs and brain, can all be damaged by direct trauma. This possibility must never be forgotten. The ways in which soft viscera can be damaged are too numerous to classify.
Compartment syndromes
Any injured tissue swells and must have room to expand, because if there is no room for expansion the tissue will become ischaemic. The different compartments are described on page 38.
A similar problem arises if limbs or digits are crushed. Fingers caught between rollers, for example, will be crushed and the skin split (Fig. 7.28). If the skin is stitched meticulously together over the soft tissues, the soft tissues will die. It is much better to leave such wounds open and elevate the limb to encourage the swelling to subside more rapidly.
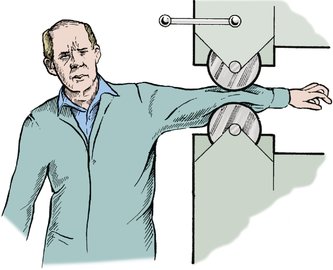 |
| Fig. 7.28
Roller injury. Pressure on the arm between rollers can cause extensive soft tissue damage without fracture.
|
With increase in the pressure in a tight fascial compartment there can be impairment of venous drainage and, ultimately, occlusion of the arterial input. This alteration in the perfusion of the muscles and nerves results in cell death and, in the case of muscle, fibrosis on healing. This fibrosis causes contractions of the muscle.
Clinical features
The symptoms and signs of an ischaemic limb are:
• Pain, greater than expected.
• Pallor of the limb, usually patchy.
• The limb is cool.
• Pulses are absent.
• Movement, particularly passive extension, is exceedingly painful.
Treatment
The fascial compartments and the skin must be divided so that the muscle can swell. The wound is left open until swelling has subsided, when it may be closed or the defect grafted. The management of the different compartment syndromes is described in the chapters on the areas affected.
Case reports
These three cases represent the management of this potentially limb threatening condition.
Patient A
A 23-year-old motorcyclist was involved in a road traffic accident in which he was hit from the side, sustaining a transverse fracture of the left mid-shaft tibia and fibula. He had no other injuries and was taken by ambulance to the accident and emergency department.
When seen there by the casualty officer he was noted to have a swollen leg and the obvious fracture on both clinical examination and radiographs. Because the fracture was relatively undisplaced his leg was immobilized in an above-knee plaster of Paris backslab and he was admitted to the orthopaedic ward, where he remained overnight. No further observations were made and on review the following morning it was noted by the nursing staff that he had required large quantities of opioid analgesics and was writhing around in great pain and discomfort.
On clinical review it was clear that he had pain on passive extension of the ankle plantarflexors and had started to develop an area of dysaesthesia over the web space between the great and second toe. A clinical diagnosis of an acute compartment syndrome was made; he was taken to theatre immediately and a large anterior lateral fasciotomy was performed. This confirmed necrotic muscle in the anterior lateral compartment, which required excision. The tibia was subsequently stabilized but unfortunately for the motorcyclist he had lost the vast majority of the muscles over the front of the shin, resulting in an inability to dorsiflex his foot thereafter.
Patient B
A 55-year-old man sustained relatively minor trauma to the front of the left shin following a fall. He noted increasing pain and discomfort over the shin and, despite analgesics, this failed to settle.
He was referred to the accident and emergency department, where he was subsequently admitted to the hospital with a painful, swollen leg. It was clear on medical review that he was on warfarin for a cardiac abnormality and, when tested, the INR was significantly elevated.
On clinical examination it was noted that the anterior lateral musculature was very swollen and he had marked pain and discomfort with passive flexion of the ankle. He was monitored reasonably closely with circulatory checks and review of the distal neurology. This confirmed a palpable pulse and normal neurology.
The swelling failed to subside and the warfarin anticoagulation was stopped. This took approximately 3 days to settle and during this period of time the patient continued to have significant pain and dysfunction. The decision was then taken to do a fasciotomy and this confirmed necrosis of the muscles as a result of a large bleed. The vast majority of the muscles were excised, leaving a weakness of ankle dorsiflexion and a large scar, which required subsequent correction with plastic surgery.
Patient C
A 30-year-old rugby player sustained a twisting injury to his right lower leg and was admitted to the orthopaedic ward with a spiral fracture of the mid-third of the tibia.
Because of concerns about compartment pressure, a compartment pressure monitor was inserted as soon as he was admitted and this confirmed a raised pressure. At this stage he had normal distal perfusion and sensibility. The decision was taken to operate immediately and the bone was stabilized using an intramedullary unreamed nail, and a wide fasciotomy was performed.
At the time of the procedure the muscle was slightly ‘dusky’ in appearance but viable. This patient went on to make a good recovery, although he had to return to theatre to have the fasciotomy scars closed secondarily.
Moral
Compartment syndromes can be devastating for the patient. There should be a high awareness of this by both nursing and medical staff. These syndromes are not always associated with high energy trauma and in those cases where there could be a reason for an increase in the intracompartmental pressure (for example, bleeding) this can easily happen with a relatively trivial trauma.
Early recognition and appropriate treatment with a fasciotomy to relieve the intracompartmental pressure avoids muscle necrosis and therefore long-term dysfunction.