CHAPTER 37 The Posterior Petrosal Approach for the Treatment of Petroclival Meningiomas
OPERATIVE TECHNIQUE
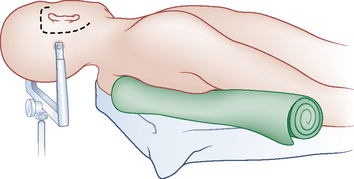
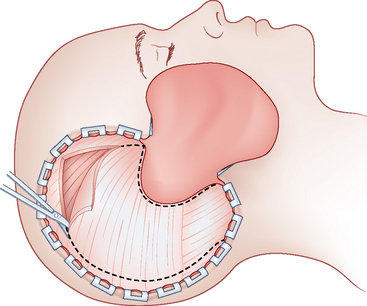
Craniotomy Flap
The skin incision is made extending from the zygoma anterior to the tragus, and extending in a curvilinear fashion behind the ear to below the mastoid process (Fig. 37-1). The skin flap is rotated anteriorly and inferiorly, and the temporal fascia is incised and reflected inferiorly in continuity with the sternocleidomastoid muscle. The temporalis muscle is cut along the superior edge of the incision and retracted inferiorly and anteriorly (Fig. 37-2). This flap will be used at the time of closure to cover the drilled surface of the temporal bone. Once these maneuvers are complete, the bony surfaces of the temporal fossa, mastoid, and lateral posterior fossa are exposed.
Four burr holes are placed straddling the transverse sinus, two in the posterior fossa and two supranteriorly. One hole is made just medial and inferior to the asterion opens into the posterior fossa below the transverse–sigmoid sinus junction. Another hole located at the squamal and mastoid junction of the temporal bond along the projection of the superior temporal line opens into the supratentorial compartment. A single bone flap covering the middle and posterior fossae is made using the foot attachment of a high-speed drill using the burr holes on either side of the sinus for access. The burr holes flanking the sinus are then connected using a rongeur or the drill. Caution should be taken during this step to avoid injury to the venous sinus wall during this step. The transverse–sigmoid sinus junction is exposed with the craniotomy. Care should also be taken when removing the bone flap because in many patients the bone is very adherent to the dura at the junction of the transverse and sigmoid sinus (Fig. 37-3).
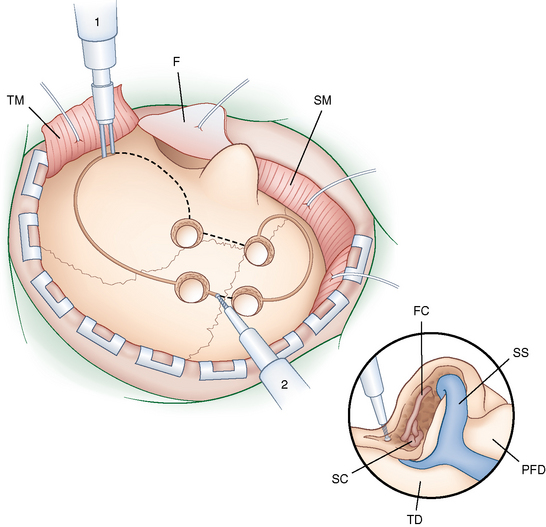
Temporal Bone Drilling
Before drilling the mastoid air cells, the mastoid cortex is scored and cut. This mastoid cortex will be used to reconstruct the calvarium at closure. At this point, the surgeon performs a complete mastoidectomy. This may be started using a round cutting burr; however, we recommend using a diamond bit when drilling near vital anatomic structures. The sigmoid sinus is skeletonized to the jugular bulb. The sinodural angle, Citelli’s angle, which denotes the position of the superior petrosal sinus, is exposed. The superficial mastoid air cells behind the posterior wall of the external ear canal as well as the deep retrofacial air cells are resected to identify the facial canal and the lateral and posterior semicircular canals. Drilling is carried forward along the pyramid to thin the petrous bone toward the apex. Care is taken at this step to leave the facial canal as well as the middle and inner ear structures intact (see Fig. 37-3, inset).
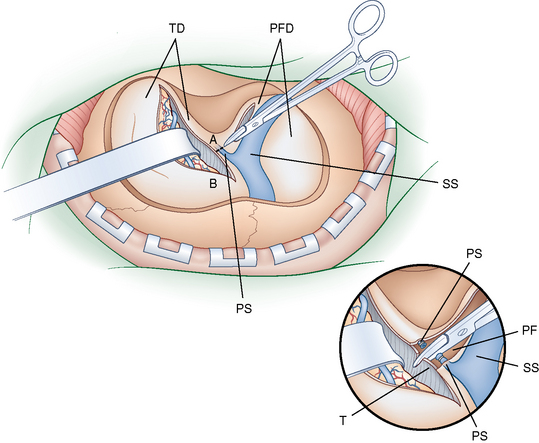
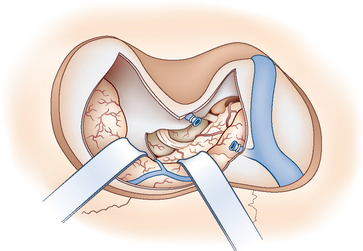
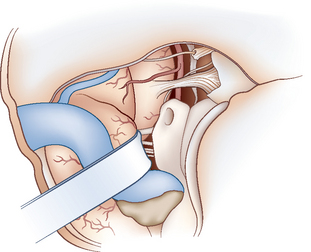
Tumor Exposure
The dura is opened along the floor of the temporal fossa and in the presigmoid region. Care is taken to locate and protect the vein of Labbé at its insertion into the sigmoid sinus (Fig. 37-4). The superior petrosal sinus is coagulated or occluded with a clip, and then it is cut to connect the dural openings (see Fig. 37-4, inset). The tentorium is sectioned in a parallel plane to the petrous ridge and across the incisura after the surgeon locates and preserves the IVth cranial nerve insertion. Opening the tentorium provides excellent exposure of the upper pole of the tumor and the anterior aspect of the brain stem. The posterior temporal lobe is elevated and the sigmoid sinus is retracted posteriorly, allowing access to the supra- and infratentorial spaces. This exposure allows for the safe resection of very large petroclival meningiomas (Fig. 37-5). In cases where the tumor extends to the opposite side, or when it is located anterior to the brain stem or to overcome the visual obstruction by the labyrinth, the pterous apex is drilled to combine the posterior petrosal approach with an anterior petrosal approach (Fig. 37-6).
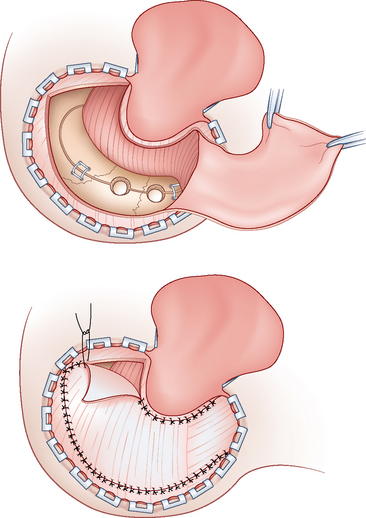
Closure
Before closure, a fat graft is obtained from the abdomen. The dura should be closed in a watertight fashion. In cases where dural shrinkage will not allow direct closure, a suitable dural graft should be obtained and used to ensure a watertight closure. In the past, we have used fascia lata autografts or dura substitute. At this point, open mastoid air cells are obliterated using fat. The bone flap is then replaced and secured with titanium plates and screws. The mastoid cortex is then replaced and secured. Gaps in the bone closure are filled with bone dust saved from the burr holes or with commercially available bone substitutes. The temporal muscle is sewn to the sternomastoid muscle to provide additional support and the soft tissues are closed in layers (Fig. 37-7).
BENEFITS OF THE APPROACH
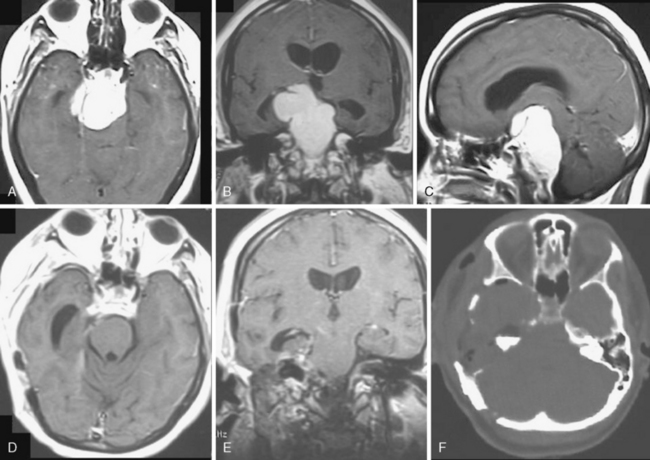
The posterior petrosal approach may be used to provide exposure of tumors deeper within the posterior fossa, lateral to the internal auditory meatus (IAM). Because of this, it is the approach of choice for larger petroclival tumors and for those that extend below the IAM (Fig. 37-8). Removal of part of the petrous temporal bone increases exposure of the petroclival region and allows a more lateral view of the brain stem and petroclival groove. In addition, the petrous resection is retrolabyrinthine, which allows for preservation of hearing. Of patients who underwent a posterior petrosal or combined petrosal approach in a recent series, the hearing preservation rate was 92%.1 This approach also allows for exposure with minimal temporal lobe retraction, and thus reduces the operating distance to the petroclival junction. Resection of the petrous temporal bone increases surgical exposure of the petroclival region by allowing a more lateral view of the brainstem and petroclival groove.
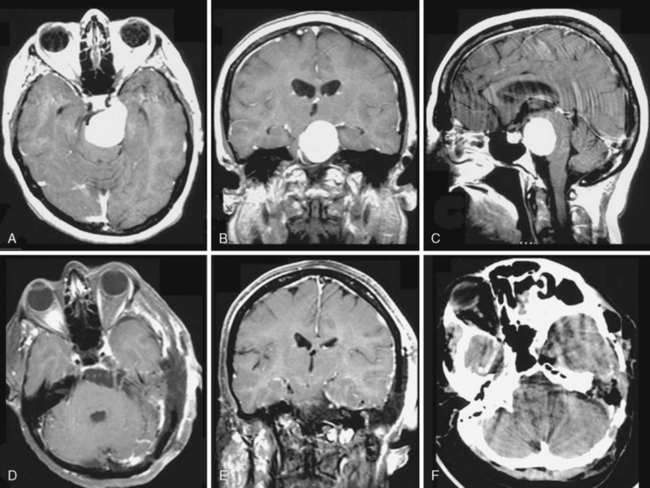
A, Axial preoperative contrast-enhanced MRI.
B, Coronal preoperative contrast-enhanced MRI.
C, Sagittal preoperative contrast-enhanced MRI.
E, Coronal postoperative MRI demonstrating total removal.
F, Postoperative CT demonstrating extent of mastoid drilling.
The retrolabyrinthine posterior petrosal approach requires mobilization of the sigmoid sinus.2 This requires skeletonization and exposure from the transverse sinus to the jugular bulb to provide enough length to be able to retract the sinus. In addition, a posterior fossa craniotomy is required to allow room for displacement of the sinus. Finally, the sigmoid sinus cannot be mobilized until the tentorium is cut to untether the sinus. Once these steps are performed, the sinus can be mobilized posteriorly, allowing adequate exposure.
LIMITATIONS OF THE APPROACH
Many of the complications of this approach are encountered when retracting the mobilized sigmoid sinus or in cutting the tentorium. Although some surgeons advocate transaction of the sigmoid sinus to allow better access,3–7 we believe that this is not necessary for sufficient exposure and carries a risk of insufficient venous outflow. Any injury to the sinus requires meticulous repair. The posterior petrosal approach may present a higher risk to patients who have a dominant or single sigmoid sinus on the side of the tumor, patients with a transverse sinus that do not connect to the torcular herophili, or patients with the venous drainage through the tentorium. In patients with a dominant or single sigmoid sinus ipsilateral to the tumor, retraction of the sinus may lead to venous congestion during the operation and injury to the sinus could lead to more serious complications. In patients whose transverse sinuses do not connect at the torcular herophili, the venous drainage may be completely split, with one hemisphere draining through the superior sagittal sinus and the other through the deep venous system. Thus, retraction of the dominant or single sinus could also lead to venous congestion of the hemisphere that is drained by this structure. In patients with sinus drainage through the tentorium, care must be taken not to transect the tentorium in a way that disrupts this drainage. In these cases, the tentorium should be cut medially and laterally to the tentorial sinus and tumor resection may proceed above and below this structure.
The anatomy of the vein of Labbé is also critical in this approach.8 In cases where the vein of Labbé inserts into the superior petrosal sinus in the tentorium before the transverse–sigmoid sinus junction, care must be taken to keep this drainage from being severed. In these cases, the insertion of the vein should be inspected closely during dural opening to ensure that the incision through the tentorium is made anterior to the insertion of the vein, keeping the venous drainage to the temporal lobe in continuity.
In a number of cases, the posterior petrosal approach may provide inadequate tumor exposure to allow complete resection. In cases of patients with a high jugular bulb, the presigmoid may be inadequate to allow exposure. In patients with tumors that cross the midline of the clivus, this exposure is inadequate and may require a combined petrosal approach. In addition, in cases with a tumor in the anterior corner of the petroclival groove and the posterior cavernous sinus, the labyrinth may obstruct the surgeons view, making complete tumor removal difficult. In cases where hearing is already affected, a translabyrinthine approach or complete petrosectomy should be considered. In cases where hearing is intact, a combined petrosal approach should be considered (Fig. 37-9).
[1] Erkmen K., Pravdenkova S., Al-Mefty O. Surgical management of petroclival meningiomas: factors determining the choice of approach. Neurosurg Focus. 2005;19:E7.
[2] Al-Mefty O. Operative Atlas of Meningiomas. Philadelphia: Lippincott-Raven, 1998.
[3] Cantore G., Delfini R., Ciapetta P. Surgical treatment of petroclival meningiomas: experience with 16 cases. Surg Neurol. 1994;42:105-111.
[4] Hwang S.K., Gwak H.S., Paek S.H., et al. The experience of ligation of transverse or sigmoid sinus in surgery of large petroclival meningiomas. J Korean Med Sci. 2002;17:544-548.
[5] Malis L.I. The petrosal approach. Clin Neurosurg. 1991;37:528-540.
[6] Megerian C.A., Chiocca E.A., McKenna M.J., et al. The subtemporal-transpetrous approach for excision of petroclival tumors. Am J Otol. 1996;17:773-779.
[7] Spetzler R.F., Daspit C.P., Pappas C.T. The combined supra- and infratentorial approach for lesions of the petrous and clival regions: experience with 46 cases. J Neurosurg. 1992;76:588-599.
[8] Sakata K., Al-Mefty O., Yamamoto I. Venous considerations in petrosal approach: microsurgical anatomy of the temporal bridging vein. Neurosurgery. 2000;47:153-160.