1 The Pediatric Transthoracic Echocardiogram
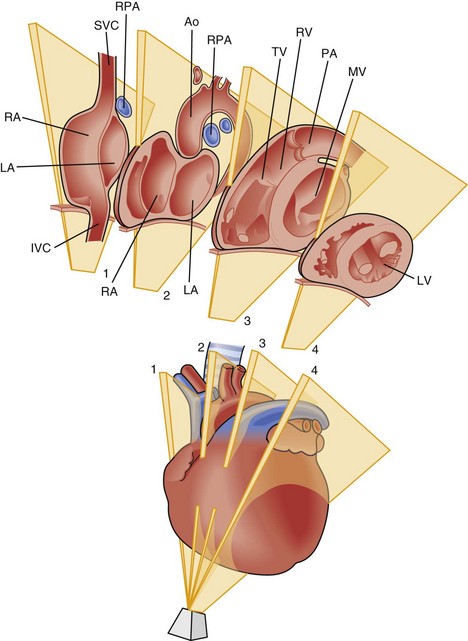
Imaging Planes
Key Points
| Window | View | Basic Anatomy Viewed |
|---|---|---|
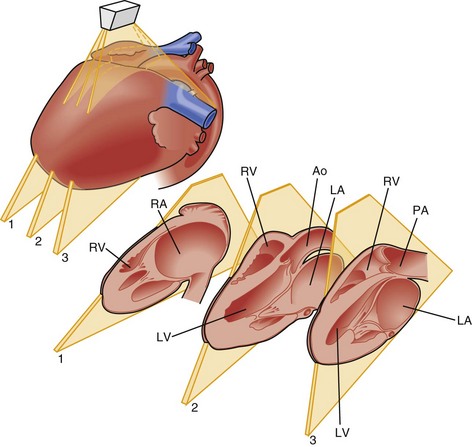
| Left parasternal | LV long axis | LV |
| Slice 2 in Figure 1-3 | Ventricular septum | |
| MV (and supporting structures) | ||
| AV | ||
| LA | ||
| CS | ||
| Proximal aortic root | ||
| RV inflow | RV | |
| Slice 1 in Figure 1-3 | TV (and supporting structures) | |
| RA | ||
| RV outflow | RVOT | |
| Slice 3 in Figure 1-3 | Pulmonary valve | |
| Proximal main PA | ||
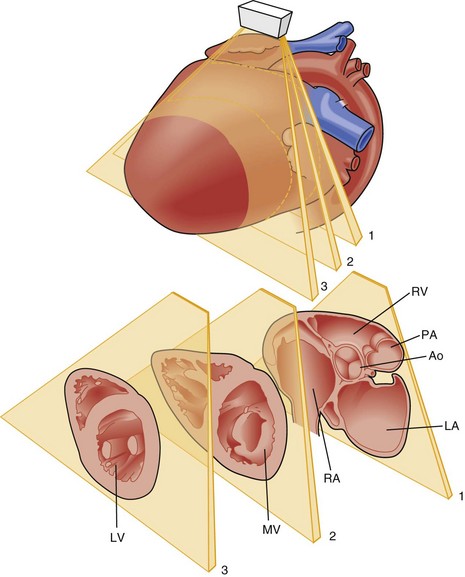
| Short axis | LV | |
| Slices 1, 2, and 3 in Figure 1-4 | MV (and papillary muscles) | |
| AV | ||
| Ventricular septum | ||
| Coronary artery origins | ||
| RVOT | ||
| Pulmonary valve | ||
| Main PA and branches | ||
| TV | ||
| AS | ||
| PVs | ||
| LPA/ductal | ||
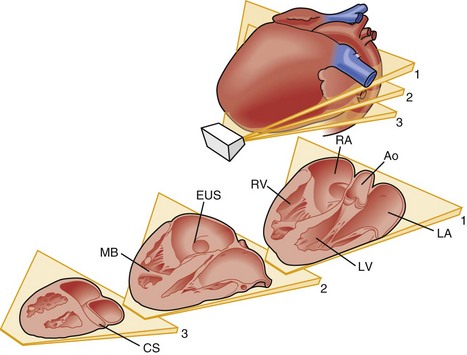
| Apical | 4C | LV, RV |
| Figure 1-5 | VS | |
| AS | ||
| AVVs | ||
| Cardiac crux | ||
| LA, RA | ||
| RV moderator band | ||
| Pulmonary venous flow/connection | ||
| Slice 3 in Figure 1-3 | CS | |
| “Five” chamber Slice 1 in Figure 1-5 |
LVOT | |
| Further anterior angulation | RVOT, pulmonary valve | |
| 3C Figure 1-6 |
All structures noted in parasternal long axis views | |
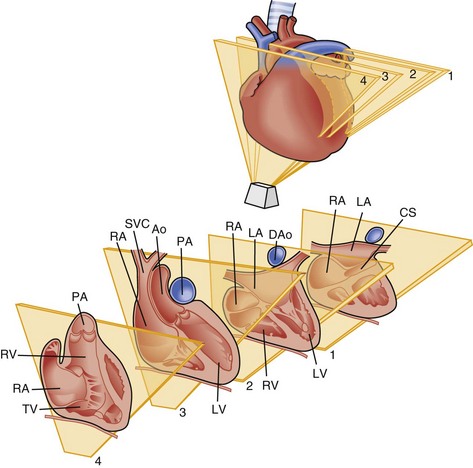
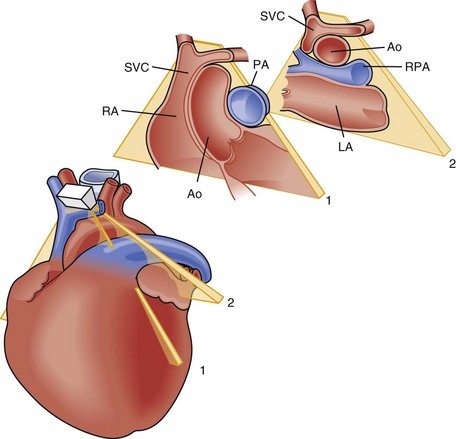
| Subcostal | 4C | LV, RV |
| Figure 1-7 | VS | |
| AS | ||
| Left and right ventricular AVVs | ||
| LVOT, RVOT | ||
| Short axis | VS | |
| Figure 1-8 | RVOT | |
| AS | ||
| IVC | ||
| SVC | ||
| Right parasternal | Long axis | SVC |
| Azygous vein | ||
| Superior aspect of AS | ||
| Ascending aorta | ||
| RPA | ||
| RCA | ||
| Short axis | Ascending aorta | |
| RPA | ||
| PPV | ||
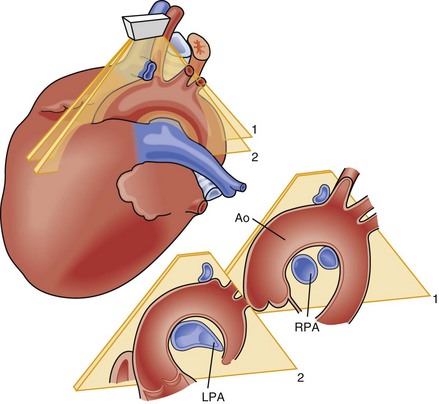
| Suprasternal notch | Long axis | Aortic arch |
| Figure 1-9 | Head and neck vessel branching | |
| Innominate vein | ||
| RPA | ||
| Short axis | Ascending aorta | |
| Figure 1-10 | Arch sidedness | |
| PV crab view | ||
| Additional branch PA views |
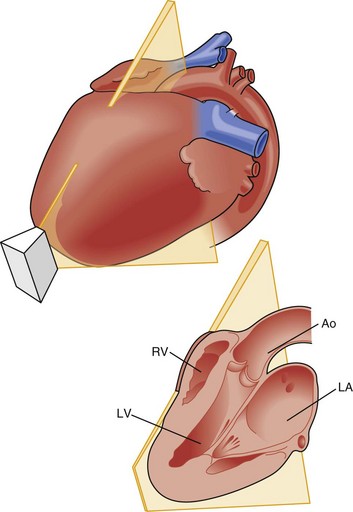
Figure 1-6 Apical three-chamber (3C) view, 90-degree counterclockwise rotation from the apical 4C view.
(Adapted from Snider RA, Serwer GA, Ritter SB. Echocardiography in Pediatric Heart Disease. St. Louis: Mosby; 1980.)
Transducers
Protocols
Sample Pediatric Protocol for a New Patient (Derived from Seattle Children’s Hospital Protocol)
Parasternal Long Axis View
Parasternal Short Axis View
High Left Parasternal View
Four-Chamber Apical View
Apical Three-Chamber or Long Axis View
Subcostal Images
Abdominal Views (Uninverted)
Subcostal Long or Four-Chamber View(Inverted Imaging)
Subcostal Short Axis View
Subcostal Right Ventricular Inflow/Outflow View
Suprasternal Notch View
Right Parasternal
1 Lai WW, Mertens LL, Cohen MS, Geva T, editors. Echocardiography in Pediatric and Congenital Heart Disease: From Fetus to Adult. Oxford, UK: Wiley-Blackwell, 2009.
2 Snider AR, Serwer GA, Ritter SB. Echocardiography in Pediatric Heart Disease, 2nd ed. Philadelphia: Mosby-Year Book; 1997.
3 Silverman NH. Pediatric Echocardiography. Baltimore, MD: Williams & Wilkins; 1993.
4 Seward JB, Tajik AJ, Edwards WD, Hagler DJ. Two-Dimensional Echocardiographic Atlas. Volume I: Congenital Heart Disease. New York: Springer; 1987.
5 Otto C. The Practice of Clinical Echocardiography, 3rd ed. Philadelphia: Saunders Elsevier; 2007.
6 Otto C, Schwaegler RG, editors. Echocardiography Review Guide. Philadelphia: Saunders/Elsevier, 2008.