17 The Optic Disc
THE NORMAL OPTIC DISC
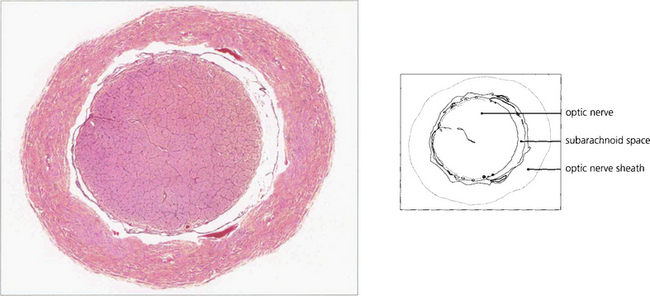
The scleral opening is rigid and nonexpansible. Behind the cribriform plate the axons acquire a myelin sheath and the optic nerve enlarges to a diameter of 3–4 mm. The nerve fibres are arranged roughly topographically in both the retinal nerve fibre layer and the optic nerve (see Ch. 19). The optic nerve sheath is a continuation of the meninges and the axons in the nerve are divided into approximately 1000 bundles by fibrous septa (derived from the pia mater) which also carry centripetal blood vessels. The subarachnoid space communicates intracranially so that the nerves are surrounded by the cerebrospinal fluid (CSF) which transmits the intracranial pressure.
BLOOD SUPPLY
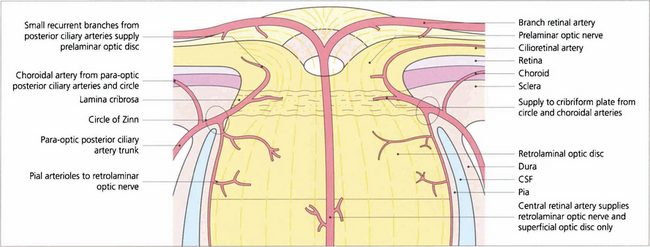
Fig. 17.1 Schematic diagram illustrating the arterial supply of the optic disc and distal optic nerve.
By courtesy of Miss Jane Olver.
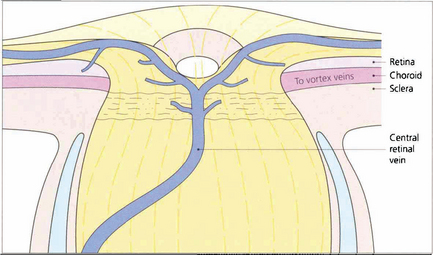
Fig. 17.2 Schematic diagram of the venous drainage of the retina, optic disc and distal optic nerve.
By courtesy of Miss J Olver.
Fig. 17.3 Digest preparations of a human optic disc. (Left) Posterior view showing the circle of Zinn which sends branches to the peripapillary choroid, the retrobulbar nerve and recurrent branches to the prelaminar region. (Right) A lateral view shows the circle of Zinn providing branches to the choroid and retrobulbar nerve.
Reproduced by permission of ED of IOVS.
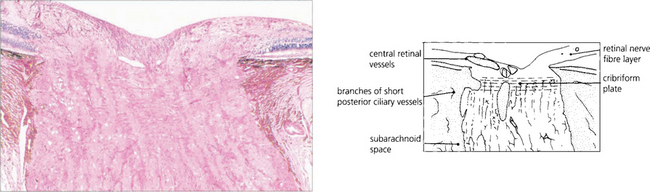
Fig. 17.4 Low-power micrograph showing an anteroposterior section of the distal part of the optic nerve, disc and retina. There is a considerable increase in the transverse diameter of the optic nerve after it passes through the sceral canal due to myelination. This is mostly completed by about the time of birth, although there is possibly some increase in myelination during the first two decades of life.
CONGENITAL ABNORMALITIES OF OPTIC DISC SIZE AND SHAPE
GLIAL REMNANTS
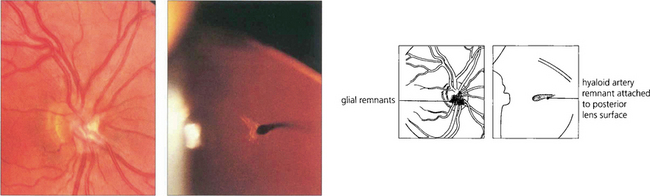
Fig. 17.6 Glial remnants are derived from either hyaloid artery remnants or vitreous condensations and lie in front of the blood vessels (left). Depending on their form and distribution they can simulate swelling or tumours of the disc. Occasionally, fibrous remnants of the hyaloid artery can be seen in the vitreous, sometimes attached to the posterior pole of the lens (right). Remnants of the embryological tunica vasculosa lentis are sometimes seen more peripherally on the lens as a Mittendorf dot (see Ch. 12).
COLOBOMAS OF THE DISC
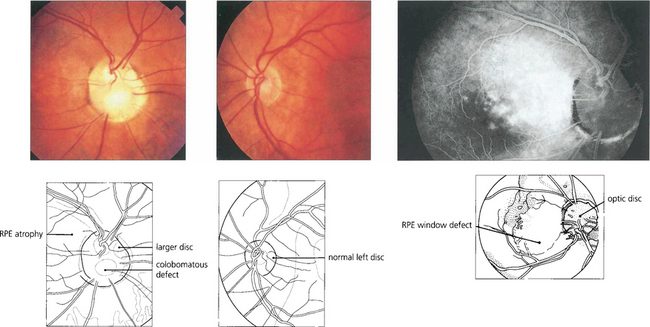
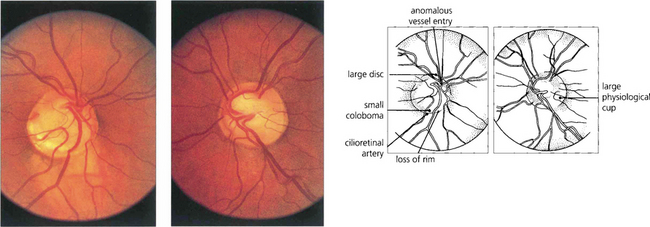
A coloboma is a congenital defect resulting from a malclosure of the fetal cleft. Colobomas vary in size and shape; the disc is usually larger than normal although it may contain fewer nerve fibres. Colobomas usually occur inferiorly with varying involvement of the retina and uveal tract (see Ch. 9). Colobomas are occasionally inherited in an autosomal dominant fashion and may also be a feature of a number of genetic and maldevelopmental syndromes such as the CHARGE syndrome (coloboma, heart defects, anal atresia, retardation of growth, genital and ear defects) which is caused by dysgenesis at 5–6 weeks’ gestation.
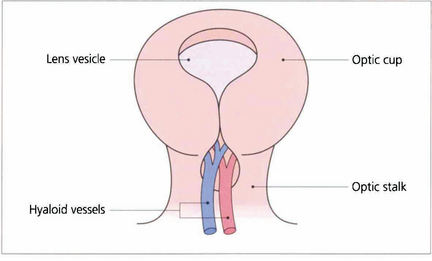
Fig. 17.7 The fetal fissure of the optic cup lies inferiorly and normally closes (starting at the middle and spreading anteriorly and posteriorly) at about 5–7 weeks of gestation. Defects in this process produce a coloboma. These can occur in many shapes and sizes, and typically involve the inferior temporal part of the disc and sometimes the retina and choroid.
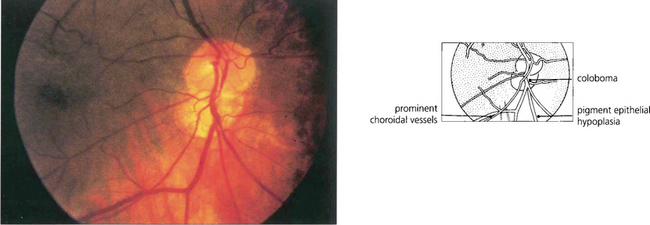
Fig. 17.8 A small coloboma of the disc associated with sectorial hypoplasia of the inferior retinal pigment epithelium in a pigmented eye. The disc appears slightly smaller vertically and is wider horizontally than normal. Choroidal vessels can be seen more easily through the thinned pigment epithelium inferiorly.
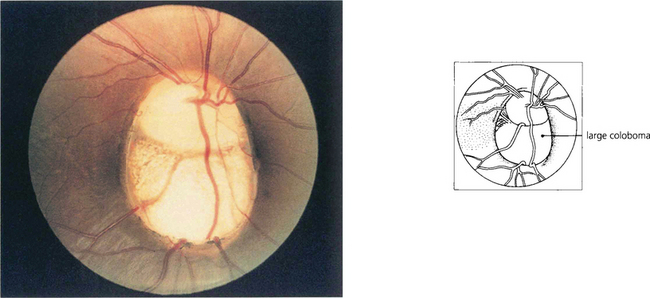
Fig. 17.9 A large coloboma of the disc. There may also be associated colobomas of the retina and choroid, lens or iris (see Ch. 9). A field defect is common and acuity may be poor if macular fibres are affected.
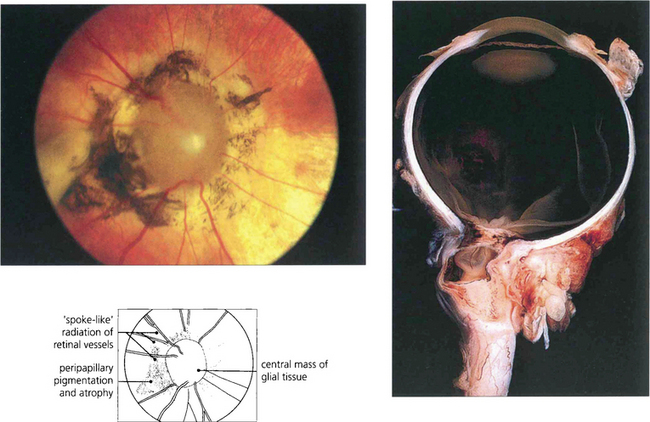
Fig. 17.10 A variant of coloboma is the morning glory disc. This rare congenital deformity of the disc is characterized by a mass of central glial tissue with radiating blood vessels, peripapillary atrophy and pigmentation. It is sometimes called a central coloboma of the disc. In these eyes the optic disc lies posterior to the globe ‘within’ the optic nerve, creating a funnel-shaped defect plugged by a central glial mass.
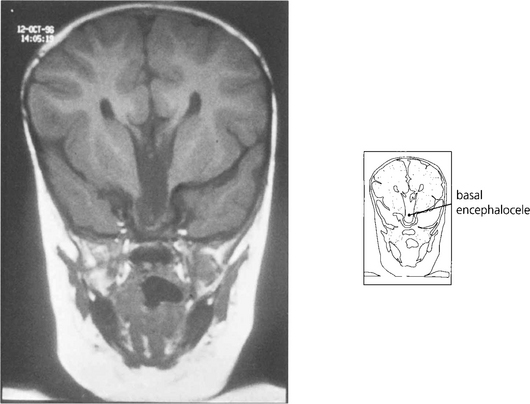
Fig. 17.11 In these patients the vision in the affected eye is poor and there may be associated midline intracranial anomalies such as a basal encephalocele. This is especially true if there are signs of malclosure of the fetal facial clefts, such as palatal deformity or telecanthus.
OPTIC DISC PITS
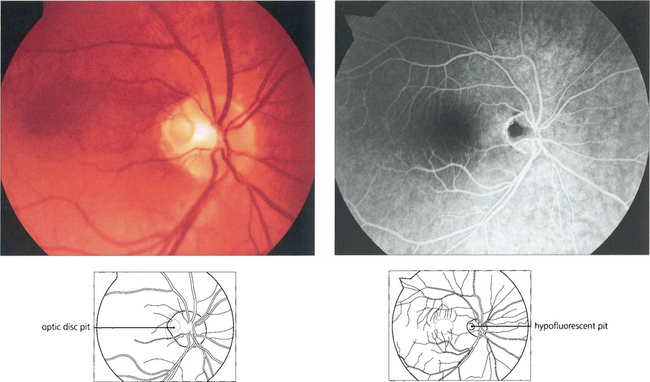
Fig. 17.14 (Left) A pit of the optic disc has a greyish appearance and lies in the temporal or inferior border of the disc (which is of normal or slightly larger diameter), penetrating deeply into its substance. Pits centred on the papillomacular bundle are frequently associated with a centrocaecal field defect; inferior pits produce superior arcuate field defects. Some patients, as in this example, have serous detachment of the macula and usually present with visual loss in early adulthood. (Right) A late-stage fluorescein angiogram shows hypofluorescence of the pit. The aetiology of macular detachment is thought to be transmission of fluid from the vitreous through the pit producing a retinal schisis.
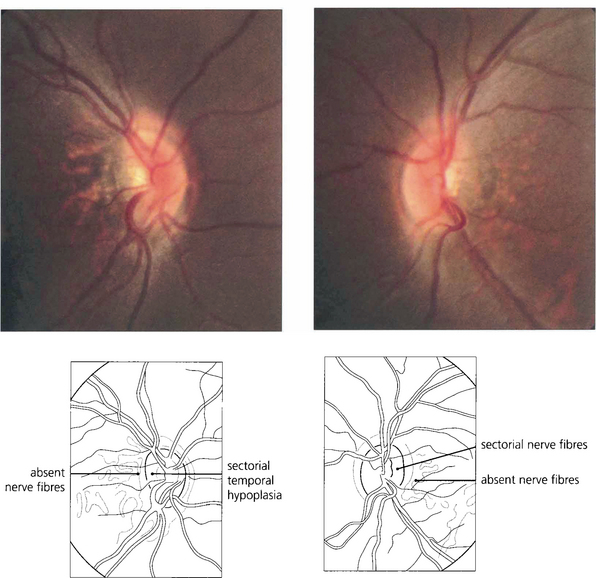
OPTIC DISC HYPOPLASIA
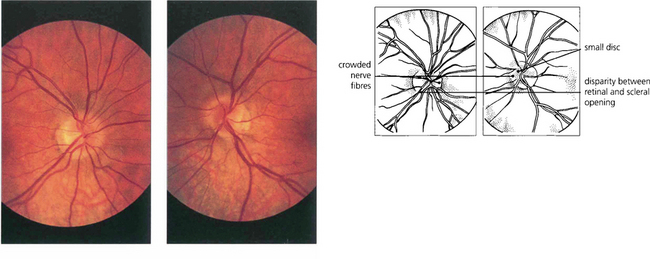
Fig. 17.15 This patient was referred with suspected papilloedema. Both optic discs are small, the left more so and slightly tilted, and the disparity between the retinal and scleral openings can be seen in both eyes. The right disc is small and full. There is crowding of the nerve fibres on the nasal side of each disc, simulating swelling.
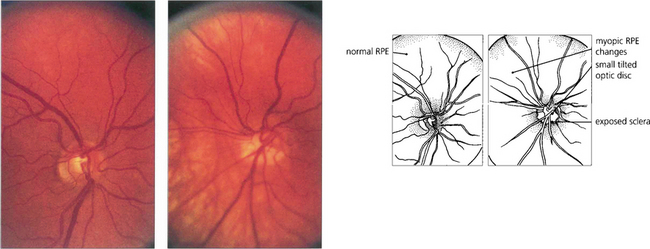
Fig. 17.16 Tilted discs are commonly seen in highly myopic eyes. This patient has a rather small disc in the right eye but the left eye is myopic with a tilted hypoplastic disc.

Fig. 17.17 The same patient had an associated cleft palate defect suggesting that the optic disc anomaly is part of a maldevelopment defect.
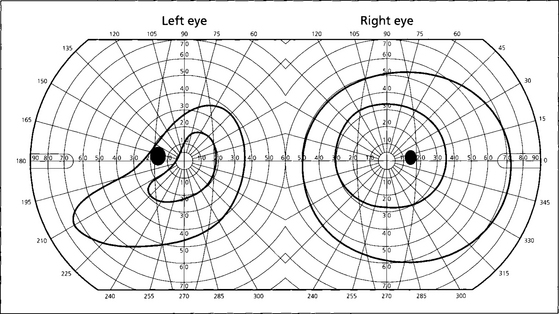
Fig. 17.18 These are the visual fields of the same patient. Fewer axons than normal enter the disc in the defective area and there is corresponding fundus ectasia (as shown by the thin retinal pigment epithelium in Fig. 17.16); together these features result in a visual field defect. As the defect is usually inferonasal this produces a superotemporal field defect simulating chiasmal compression. Such defects, however, cross the vertical meridian, a feature never seen with neurological causes of field loss. Furthermore, the refractive component can be corrected by additional myopic correction and these characteristics allow the correct diagnosis to be made.
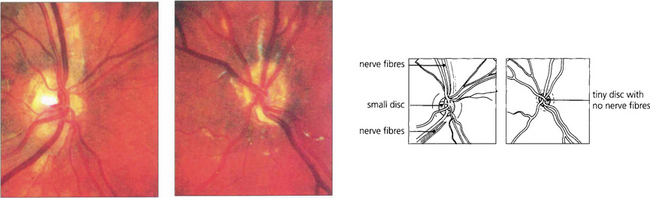
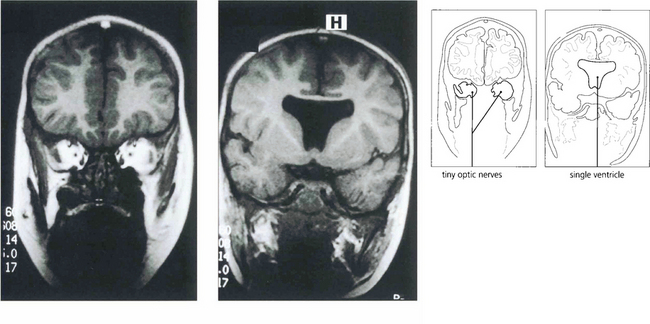
Fig. 17.19 Optic nerve hypoplasia is seen in its most severe form as part of the rare syndrome of septo-optic dysplasia. These children have very poor vision and associated midline intracranial anomalies, of which an absent septum pellucidum is typical. Abnormalities of pituitary hormonal function, especially growth hormone deficiency, are common. The right optic disc is grossly hypoplastic, although some nerve fibres are present; the left contains virtually no nerve fibres at all. This child had short stature as a result of growth hormone deficiency and acuity of 20/40 and PL.
By courtesy of Professor D Taylor.
ANOMALIES ASSOCIATED WITH AXIAL LENGTH
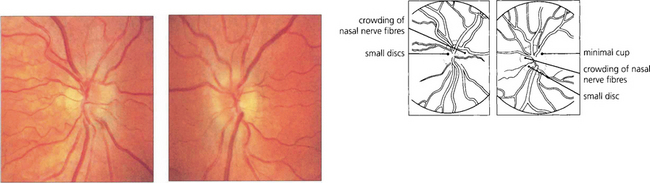
Fig. 17.22 The appearance of the optic discs in a patient with +6D of hypermetropia in each eye and axial lengths of 21 and 20.7 mm. The discs are small and full with a crowded nerve fibre pattern and minimal cupping.
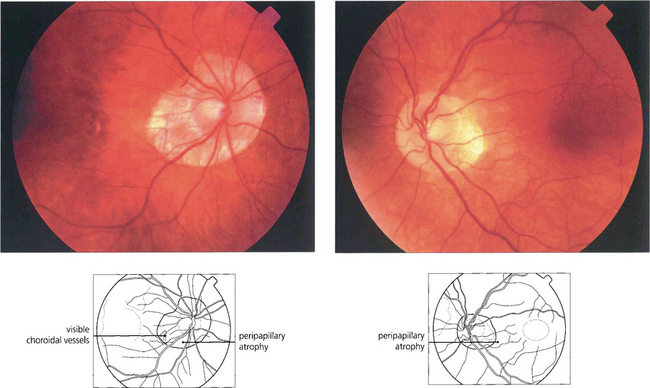
Fig. 17.23 Myopic discs have associated peripapillary atrophy and a temporal crescent. Because of the larger intraocular surface area, the retinal pigment epithelium and choroid appear to be thinned and pale and sometimes the temporal retinal vessels are stretched into a posterior pole staphyloma (see Ch. 15).
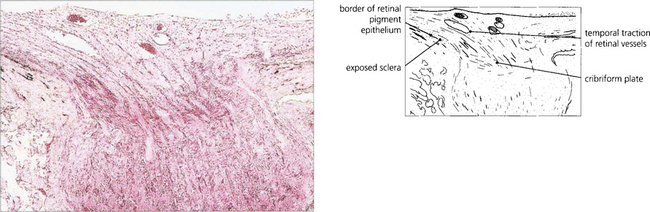
Fig. 17.24 Histological examination of a myopic disc shows that the retinal aperture of the optic disc is larger than the scleral aperture with a deficiency of retina and choroid on the temporal side revealing the bare sclera. There is temporal traction of the blood vessels caused by the stretching or pulling of the retina into the expanded posterior pole of the eye.
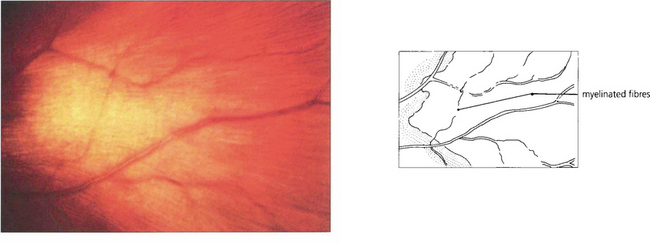
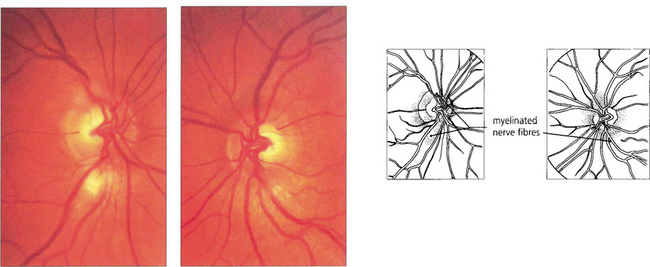
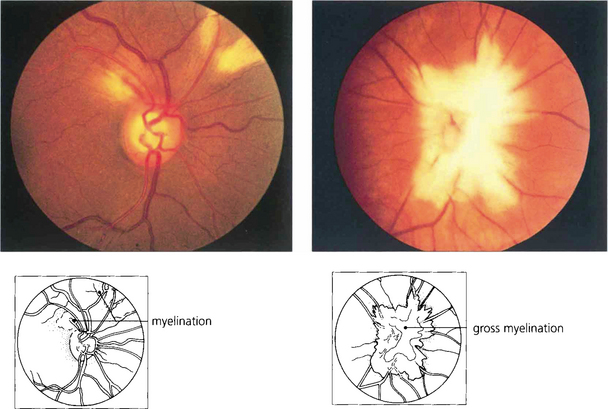
MYELINATED NERVE FIBRES
DRUSEN OF THE DISC
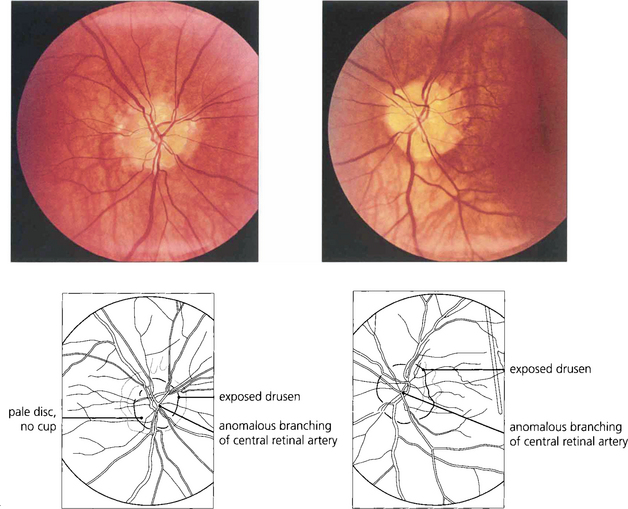
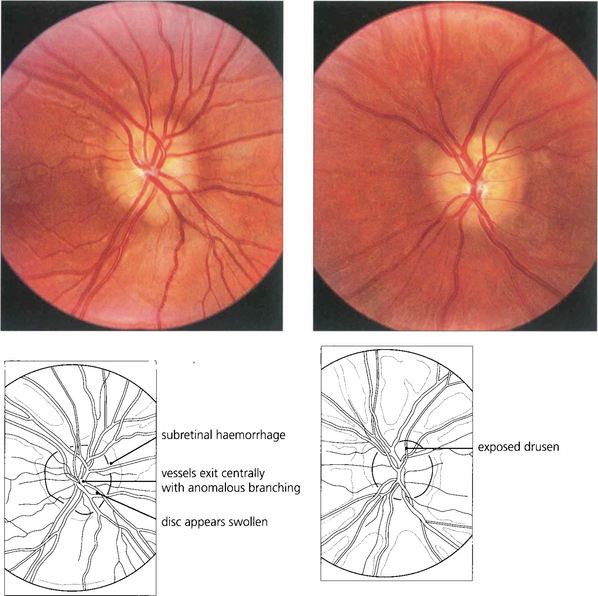
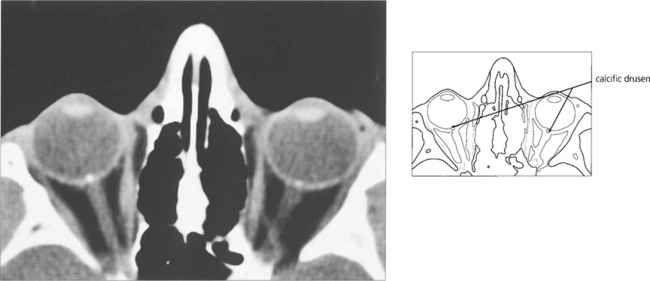
Fig. 17.28 This patient has typical exposed drusen. Note the discs are relatively small, there is no cup and the vascular pattern is anomalous with the vessels exiting centrally. The central retinal artery divides immediately into five branches. The patient had markedly constricted fields.
ANOMALOUS VASCULAR CHANGES
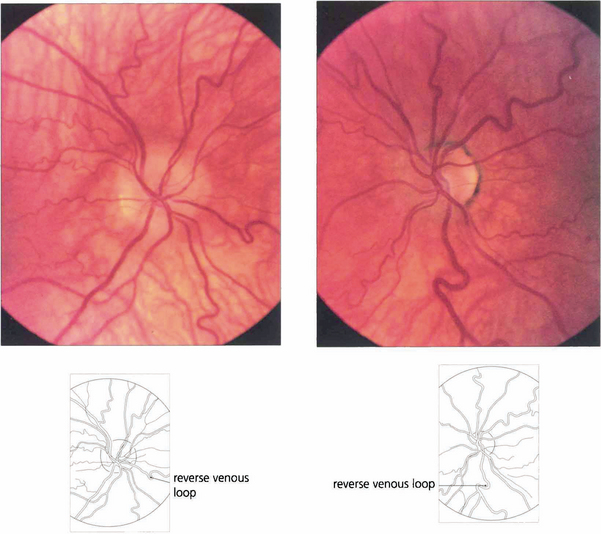
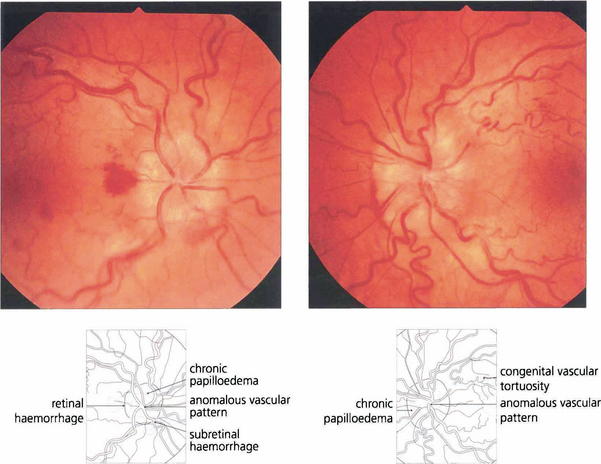
Fig. 17.31 Optic discs with congenitally anomalous blood vessels are often mistakenly thought to be pathologically swollen. These discs are of small size with no physiological cup with vessels that exit centrally in an anomalous pattern. On the retina there is congenital tortuosity, largely affecting retinal veins, with typical reverse loops pointing backwards towards the disc, a sign of congenital vascular tortuosity. The retinal nerve fibres are not swollen and do not cover the vessels; furthermore, the superficial vascular plexus on the disc is not dilated.
PAPILLOEDEMA
EARLY PAPILLOEDEMA
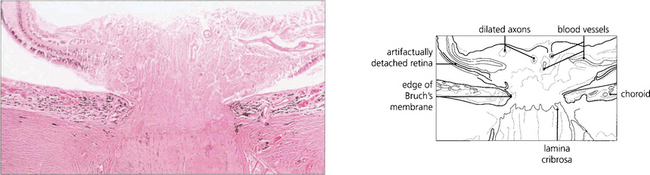
Fig. 17.33 The earliest histological feature seen in any swollen disc is axonal dilatation following hold-up of orthograde axoplasmic transport in the retinal neurones as they pass through the cribriform plate. Axoplasmic transport is a complex traffic of intracellular organelles from the cell nucleus to the synapse (orthograde) or vice versa (retrograde) (see Ch. 13). Vascular engorgement and oedema add to the swelling but the initial changes are found in the nerve fibres. The precise mechanism causing the axoplasmic delay is not well understood but probably consists of a mixture of hypoxic, mechanical and vascular factors.
By courtesy of Professor P Luthert.
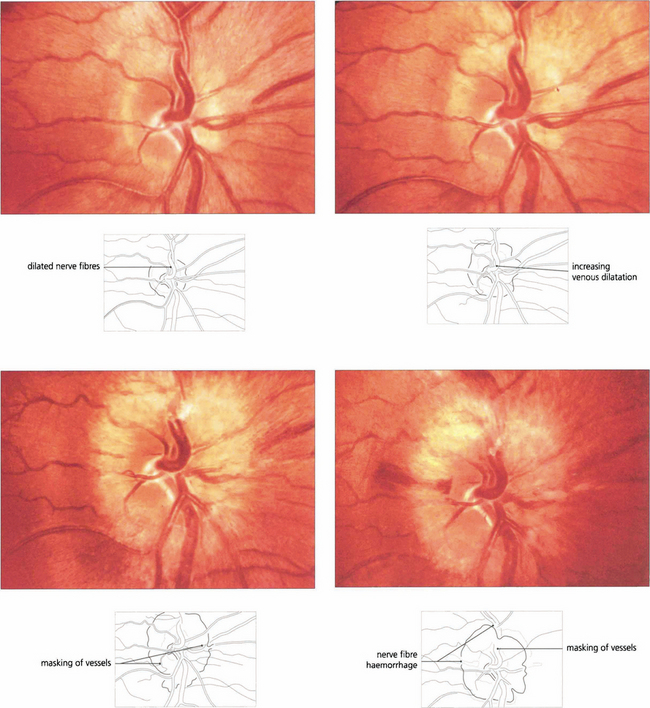
Fig. 17.34 Progressive changes of papilloedema are seen in a patient with an intracranial tumour who declined treatment. (Top left) Early nerve fibre dilatation is seen particularly superiorly, inferiorly and nasally. (Top right) This increases and venous engorgement develops. (Bottom left and right) Temporal nerve fibre dilatation and swelling of the disc increases and haemorrhages and possibly cotton wool spots appear.
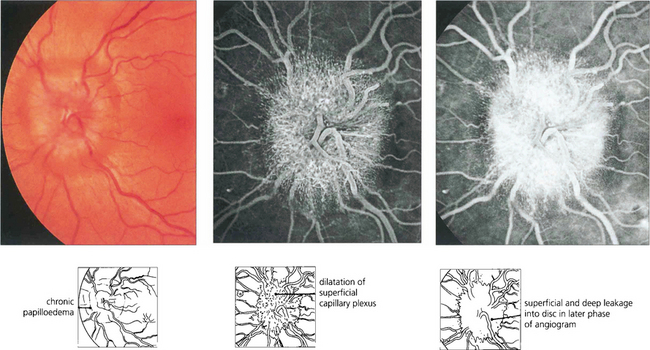
Fig. 17.35 Fundus photography (left) and fluorescein angiography (middle, right) can be extremely useful in establishing the diagnosis of papilloedema and in monitoring its progress. Swollen optic discs show dilatation of the superficial capillary plexus on the disc surface (middle) and deep leakage within the disc in the later stages of the angiogram (right). Although these changes confirm that the disc is swollen, they do not differentiate the cause. Furthermore, caution is required as crowded anomalous discs sometimes stain with fluorescein in the late phases of the angiogram.
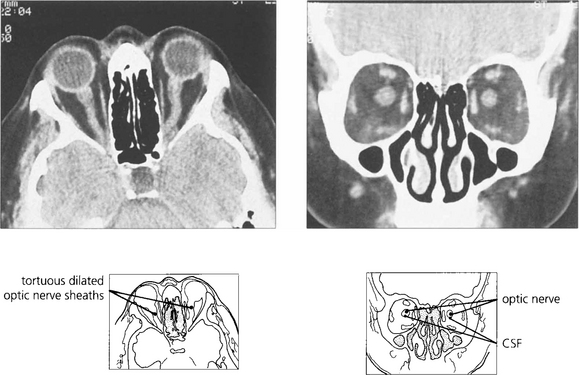
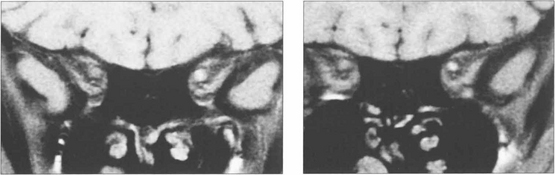
Fig. 17.36 Orbital computed tomograms of patients with raised intracranial pressure show dilatation of the optic nerve sheaths with CSF and provide useful ancillary diagnostic information in difficult cases. Dilatation of the optic nerve sheaths from CSF must be distinguished from thickening due to, for example, inflammation or meningioma.
ACUTE PAPILLOEDEMA
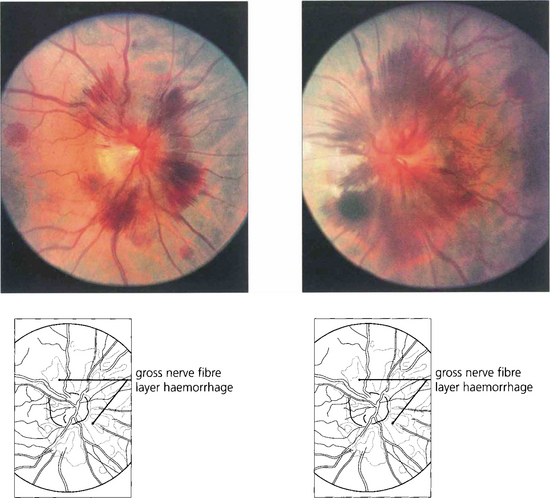
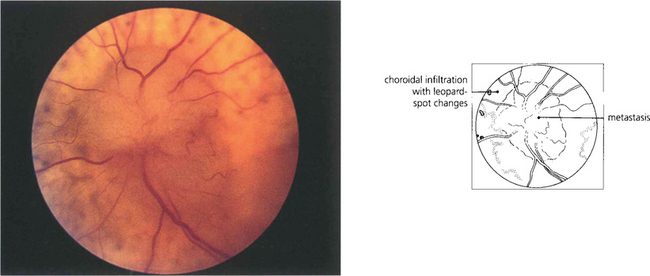
Fig. 17.37 This patient presented with severe headache with metastases from carcinoma of the bronchus. The discs show florid haemorrhages with relatively little swelling, indicating a rapid dramatic increase in CSF pressure.
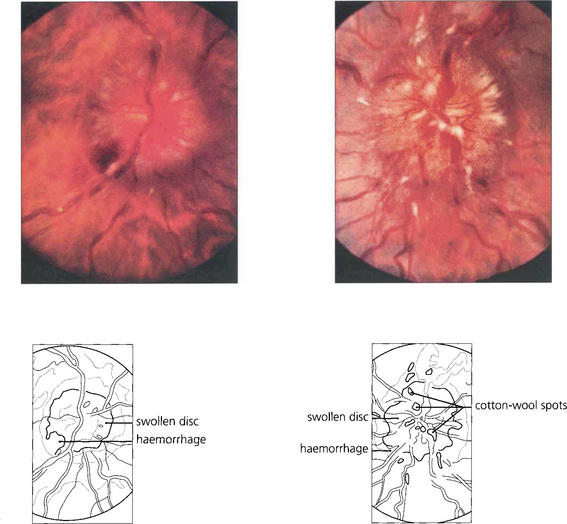
Fig. 17.38 This patient had a posterior fossa tumour. These tumours can readily compress the aqueduct in the midbrain and produce an acute rise in CSF pressure. Both discs are grossly swollen with dilated nerve fibres, masking the blood vessels at the disc borders. There are haemorrhages into the nerve fibre layer around the disc and cotton-wool spots on the disc surface. These are signs that the patient has suffered a rapid rise in intracranial pressure. The optic cup is still preserved.
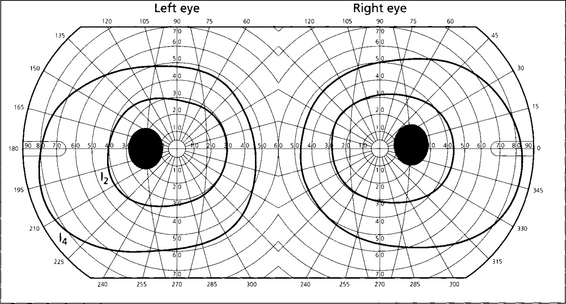
Fig. 17.39 Acute papilloedema is associated with full visual fields, normal visual acuity and colour vision. The blind spots are enlarged as a result of lateral displacement and masking of photoreceptors by swollen nerve fibres, together with accumulated subretinal fluid and hyperopia induced by a more rigid and dilated optic nerve sheath pressing on the globe.
CHRONIC PAPILLOEDEMA
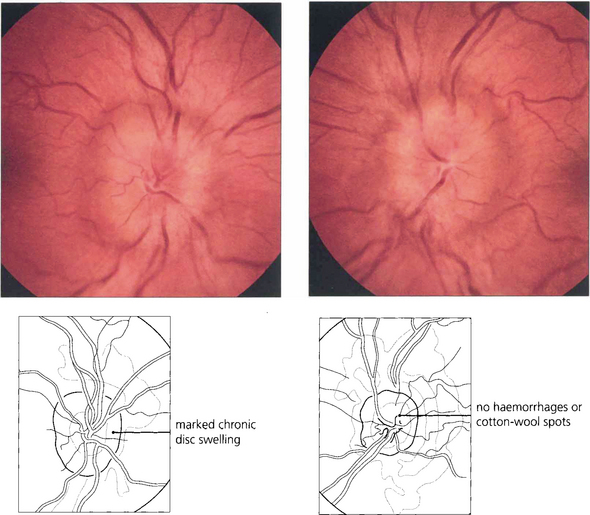
Fig. 17.40 This patient with benign intracranial hypertension has gross disc swelling with no haemorrhages or cotton-wool spots indicating a slow rise in CSF pressure to a severe level.
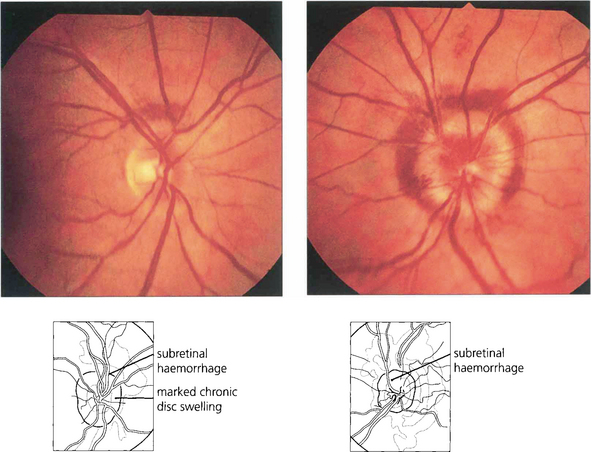
Fig. 17.41 Papilloedema is usually bilateral but can be very asymmetrical. This patient has much more marked disc oedema in the left than in the right eye, indicating that for some reason the increased CSF pressure has not been transmitted to the right optic disc. Subretinal peripapillary haemorrhage is seen in both eyes.
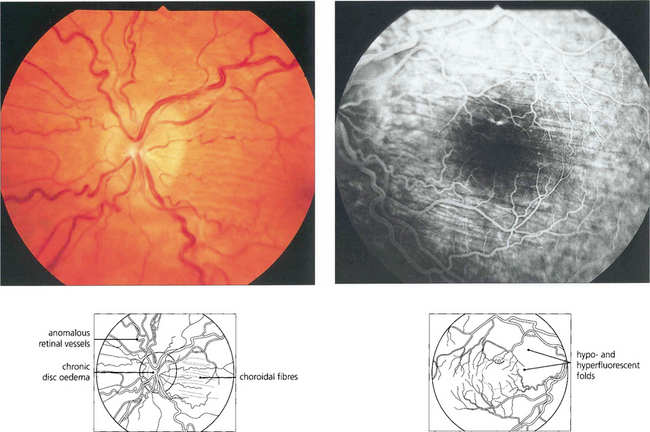
Fig. 17.42 Choroidal folds are produced by the comparatively rigid and distended optic nerve sheath indenting the globe. They are due to folding of the RPE. When associated with papilloedema they normally lie in a horizontal axis. They are much more visible in fluorosein angiography.
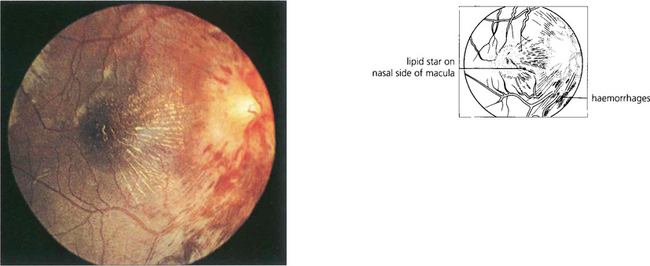
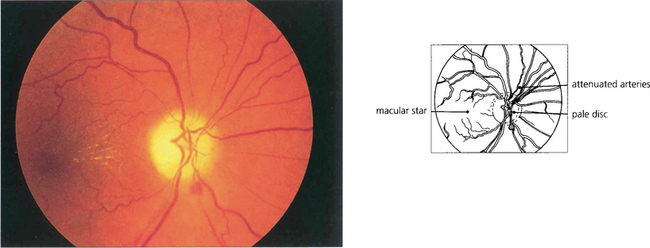
Fig. 17.43 Papilloedema with a macular star. This is one of the few occasions in which papilloedema is accompanied by decreased visual acuity. Macular stars result from plasma lipoproteins leaking from a swollen optic disc and are sometimes seen with either chronic papilloedema or resolving papilloedema following treatment. They are particularly common with ischaemic optic disc swelling, from which papilloedema should be distinguished. The lipoprotein exudate lies within the radiating nerve fibres of Henlé surrounding the macula and is usually more marked on the nasal side.
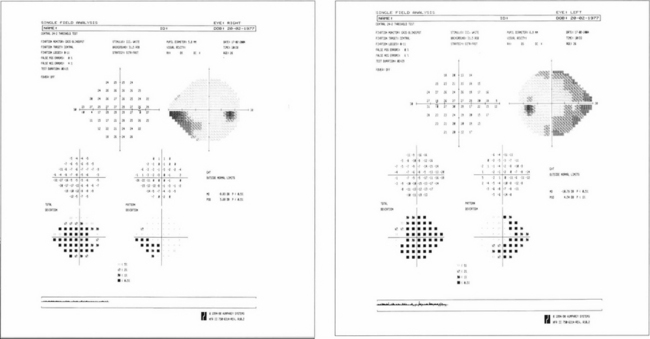
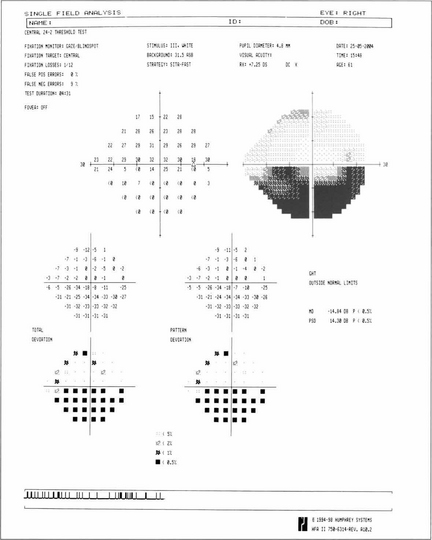
Fig. 17.44 Computerized fields (Humphrey 24–2 protocol) from a patient with bilateral chronic papilloedema. Inferonasal field loss is usually found as the earliest change. As papilloedema becomes chronic there is progressive nerve fibre loss which is usually seen as an inferior arcuate defect; note also the enlarged blind spots. With progression further loss is seen in the superior and inferior arcuate regions. Ultimately the patient is left with preservation of only the central visual field resulting in ‘tunnel’ vision.
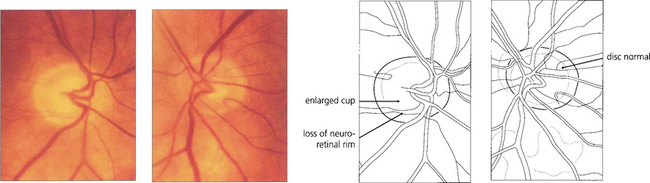
ATROPHIC PAPILLOEDEMA
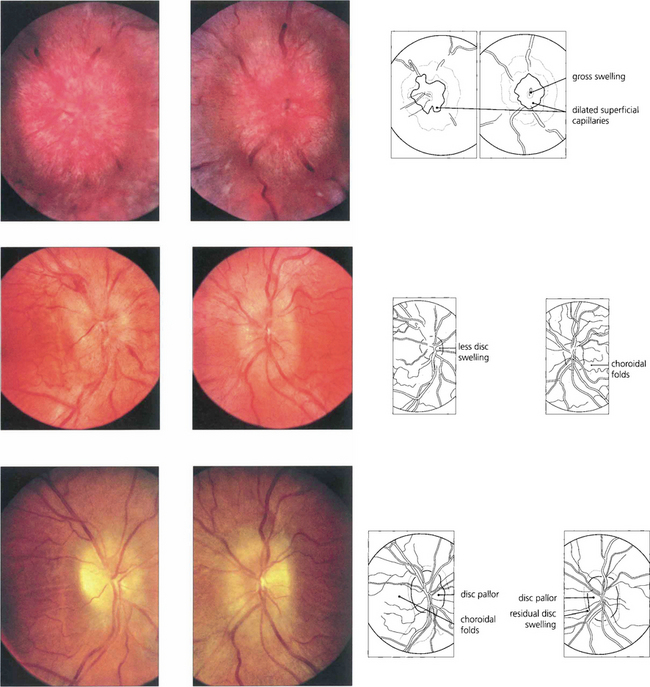
Fig. 17.45 This patient had raised CSF pressure from a glomus tumour. There is gross chronic oedema of both optic discs. He was treated with bilateral optic nerve sheath fenestrations. One month later there is considerable improvement in the disc appearances. Four months after surgery there is residual swelling with pallor more marked in the right than the left eye, signifying axonal loss. Choroidal folds can be seen in the right eye; these frequently persist after resolution of raised CSF pressure due to retinal pigment epithelium damage.
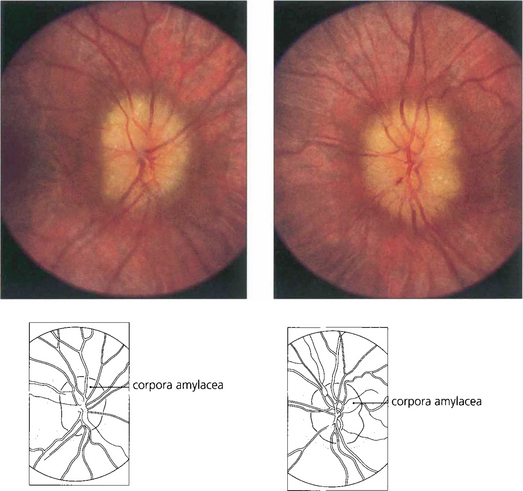
Fig. 17.46 Sustained intracranial pressure over a prolonged period eventually leads to pallid swollen discs with tiny opalescent excrescences on the disc surface, representing debris from axonal damage and sometimes referred to as corpora amylacea. Nerve fibre loss can be seen ophthalmoscopically in the retina. These discs sometimes have an appearance superficially similar to drusen of the disc.
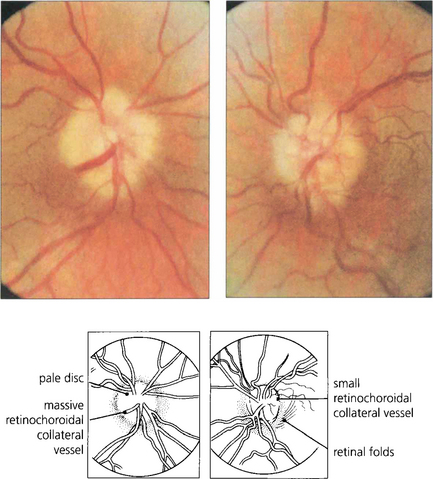
Fig. 17.47 With atrophic papilloedema nerve fibres are eventually destroyed and the optic disc without viable nerve fibres does not swell (if there are no axons left there can be no hold-up of axoplasmic transport). This patient had longstanding benign intracranial hypertension. The discs are pale and slightly swollen, and there is some arterial attenuation. Retinochoroidal venous collaterals are present (a sign that there has been chronic swelling of the disc) shunting blood from high pressure in the central retinal vein to lower pressure in the choroidal circulation to leave the eye by the vortex veins. The visual fields will be grossly and irreversibly constricted with poor visual acuity. At this stage sudden lowering of the CSF pressure can precipitate acute visual loss.
By courtesy of Mr M D Sanders.
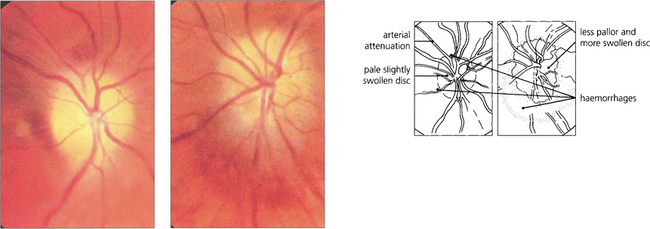
Fig. 17.48 Another patient with cryptococcal meningitis shows terminal papilloedema. The right eye (left) had perception of light; note the pale atrophic disc, minimal swelling and marked arterial attenuation. In the left eye (right), the visual acuity was 20/200 and the disc pallor is less and there is more swelling.
PAPILLITIS
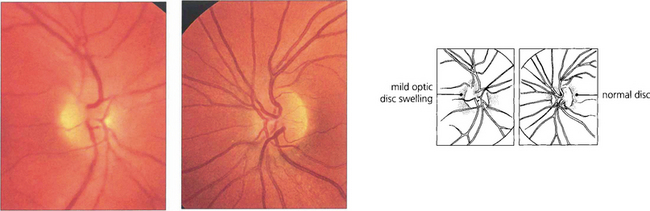
Fig. 17.49 The left eye of this 25-year-old woman is normal but there is mild swelling of the right disc. In this eye the visual acuity was reduced to counting fingers; no Ishihara plates could be recognized and there was some pain on ocular movement and tenderness on retropulsion of the globe.
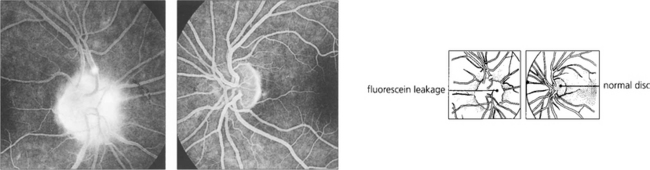
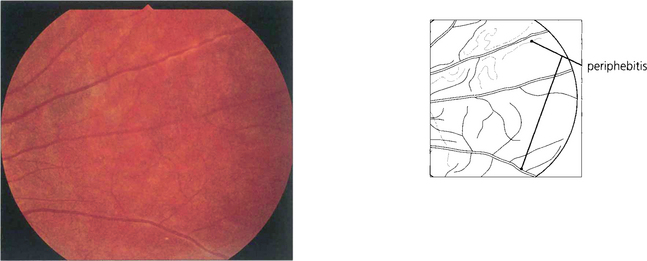
Fig. 17.50 Fluorescein angiography shows deep staining of the disc in the late phases. Although no definite distinction can be made between swelling due to papilloedema or papillitis, the latter is usually less marked with fewer haemorrhages and cotton-wool spots. With papillitis there may sometimes be a low-grade vitreous cellular infiltration. Sheathing of the peripheral retinal veins, similar to that seen with a low-grade retinal vasculitis (see Fig. 10.27 and Fig. 17.53), is seen in about 25 per cent of patients with acute demyelinating retrobulbar neuritis; these are known as Rucker’s lines after the Mayo Clinic neurologist who first described them.
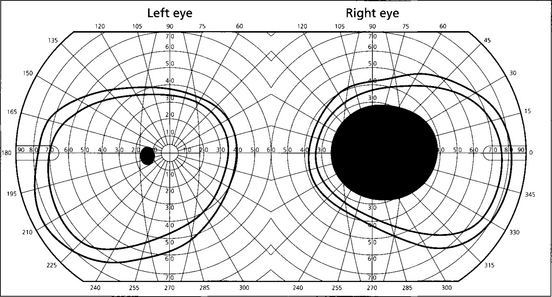
Fig. 17.51 The left visual field is normal; the right has a large central scotoma. This can be easily demonstrated at the bedside by using a red target and a confrontation visual field to show central desaturation. The visual evoked potential (VEP) will show a reduction in amplitude with considerable delay of the waveform; as the vision improves, the amplitude recovers but the delay remains. VEPs are particularly useful for detecting subclinical demyelination in the fellow eye (see Ch. 1).
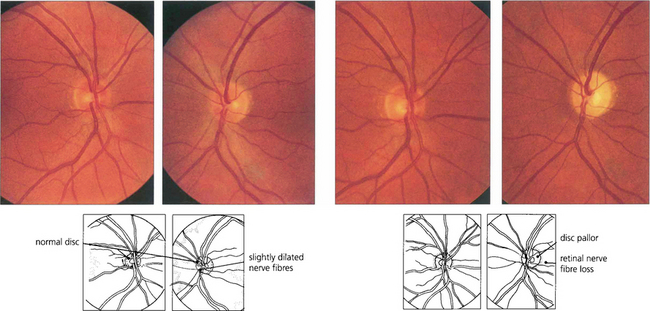
Fig. 17.52 This patient presented with symptoms of left acute optic neuritis with parasthesiae in his right leg. At presentation (left two figures) both optic discs look grossly normal although the nerve fibre outline in the left eye is slightly more blurred. Eight weeks later (right two figures) there is definite pallor of the left optic disc.
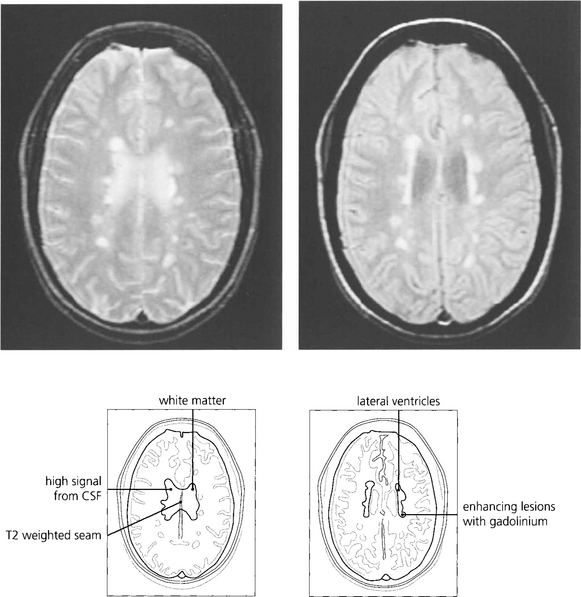
Fig. 17.54 Magnetic resonance imaging shows focal white matter lesions with a prediliction for the periventricular area in about 50 per cent of patients presenting with optic neuritis. Gadolinium enhancement shows the lesions are of recent onset. The presence of typical MRI lesions correlates with a substantially increased risk of developing MS.
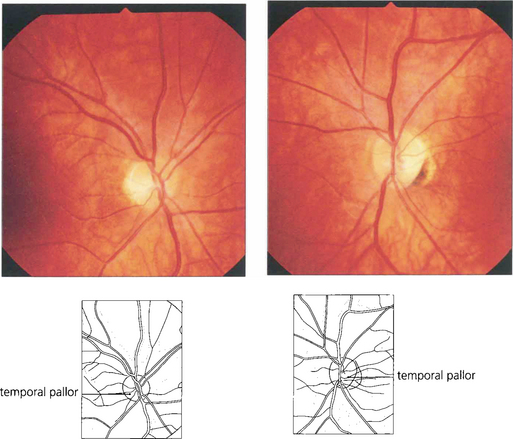
ISCHAEMIC OPTIC NEUROPATHY
NONARTERITIC ANTERIOR ISCHAEMIC OPTIC NEUROPATHY
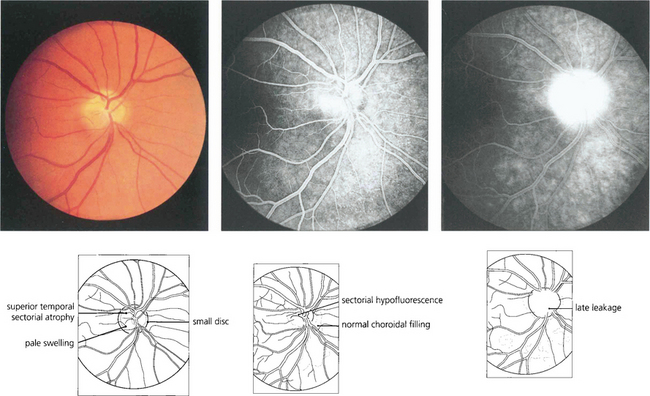
Fig. 17.56 This patient shows the typical features of nonarteritic ischaemic optic neuropathy 3 weeks after the onset of acute visual loss in the right eye. The disc is small, the superior pole is pale and the inferior pole shows pale swelling (left); the angiogram shows hypofluoresence superiorly in the early stages and later leakage (right). Note the peripapillary choroid fills normally.
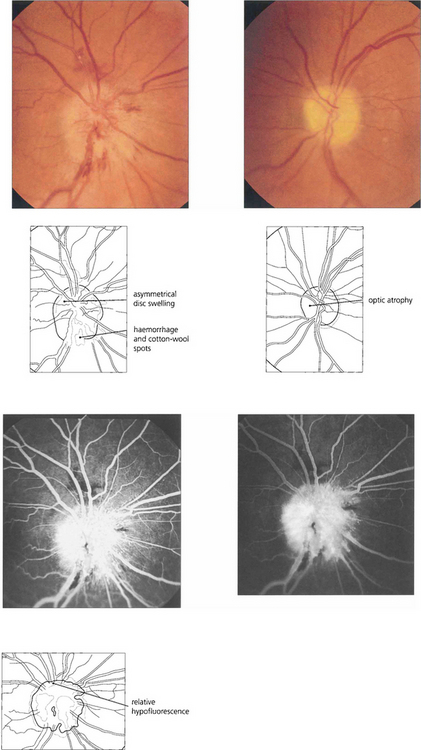
Fig. 17.57 About 30 per cent of patients will have involvement of the second eye within 2 years. This patient has a pale left disc from previous nonarteritic anterior ischaemic optic neuropathy. The right disc shows acute changes, more marked in the inferior pole of the disc, with relative hypofluorescence superiorly.
ISCHAEMIC OPTIC NEUROPATHY DUE TO TEMPORAL ARTERITIS
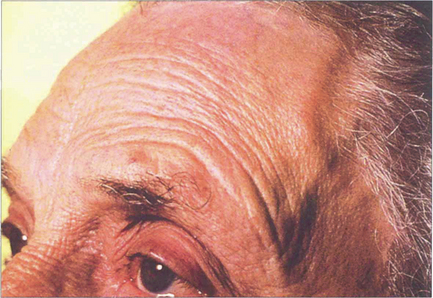
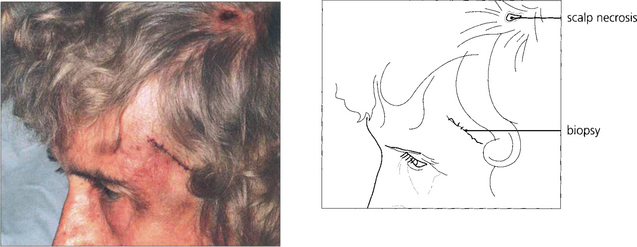
Fig. 17.59 The temporal arteries of this woman were tender, inflamed, thickened and nonpulsatile, although frequently the signs are more subtle. The diagnosis is suggested by finding a high erythrocyte sedimentation rate (ESR) and C-reactive protein level and confirmed by temporal artery biopsy. Prompt treatment with steroids is required as there is a grave risk of fellow eye involvement or stroke.
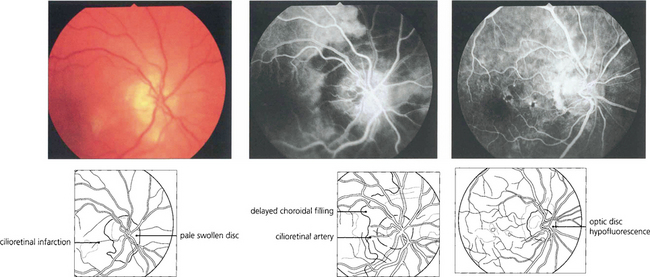
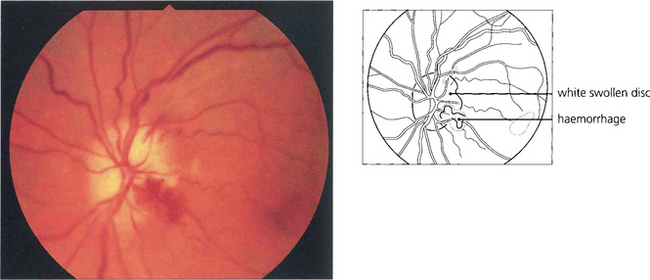
Fig. 17.62 The optic disc of this elderly woman who suddenly lost vision in the right eye is completely infarcted, pale and slightly swollen with a small cilioretinal infarct (left), which is, of course, supplied by the posterior ciliary circulation. The fluorescein angiogram in the early venous phase (middle) shows delayed filling of the optic disc and peripapillary circulations due to involvement of the short posterior ciliary arteries that supply the disc and adjacent peripapillary choroid with some leakage of dye into the optic disc. Such delay in filling of the peripapillary choroid distinguishes arteritic from nonarteritic ischaemic optic neuropathy. The left optic disc shows filling defects indicating subclinical involvement of the posterior ciliary circulation and impending doom. Central retinal artery occlusion can occur in temporal arteritis but is uncommon.
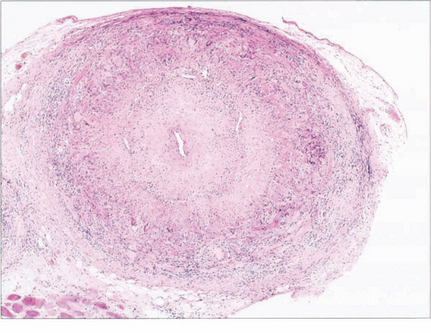
Fig. 17.63 Temporal artery biopsy following presentation is essential to confirm the diagnosis and should be done within the first 48 hours as steroid therapy may affect the histological interpretation. These elderly patients may need prolonged systemic steroid therapy to control the arteritis and commonly suffer treatment side-effects. It is therefore essential to be sure that the diagnosis is well substantiated. The biopsy of this patient shows inflammatory changes throughout the entire arterial wall but these are concentrated mainly in the media with fragmentation of the internal elastic lamina; there are multinucleated giant cells and gross narrowing of the lumen. Skip lesions can occur and it is necessary to examine sections at different levels to exclude this possibility.
INHERITED OPTIC NEUROPATHY
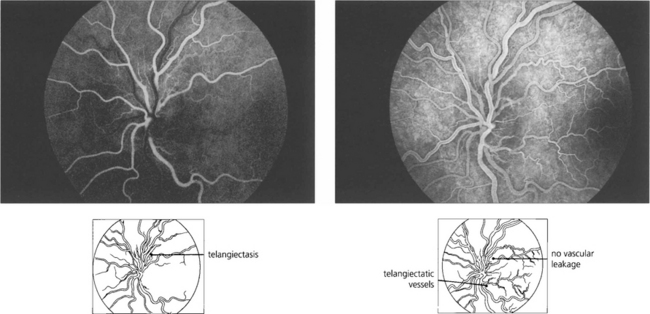
LEBER’S HEREDITARY OPTIC NEUROPATHY
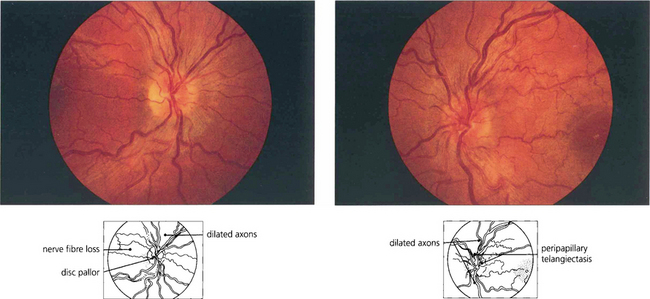
Fig. 17.66 This patient had suffered acute loss of vision in his right eye 6 weeks previously and presented with acute visual loss in the left eye. The right disc (left) is becoming pale but the retinal axons are still dilated and the vascular tortuosity is less marked than in the left eye (right) where telangiectatic vessels can be seen in the dilated and prominent nerve fibre layer surrounding the disc.
OPTIC DISC INFILTRATIONS AND TUMOURS
INFLAMMATORY INFILTRATION
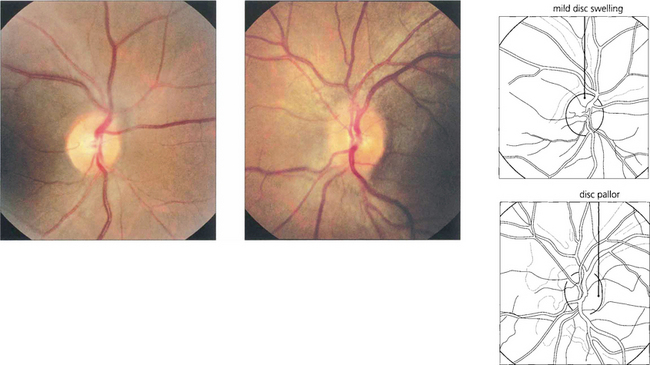
Fig. 17.69 Sarcoid can cause disc swelling secondary to posterior uveitis as a result of optic nerve infiltration or from raised CSF pressure. Patients may also present with primary optic atrophy. This patient presented with mild swelling of the left optic disc with some pallor of the right disc. She had pulmonary sarcoid.
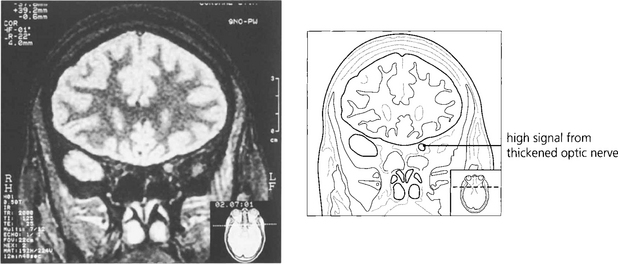
Fig. 17.70 Magnetic resonance imaging of the same patient shows a high signal from the thickened left optic nerve in the posterior orbit.
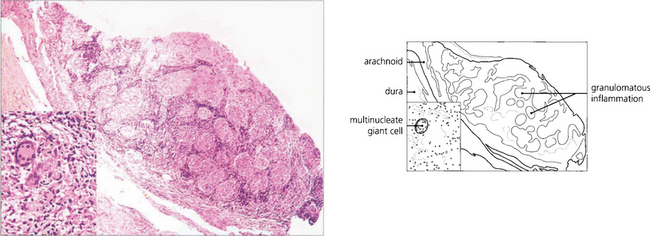
Fig. 17.71 This optic nerve biopsy was taken from a 46-year-old patient with a chronic progressive unilateral optic neuropathy eventually resulting in a blind eye. The patient then started to develop a visual field defect in the fellow eye. MRI showed bilateral optic nerve thickening. Biopsy confirmed the suspected diagnosis of sarcoid optic neuropathy.
TUMOURS
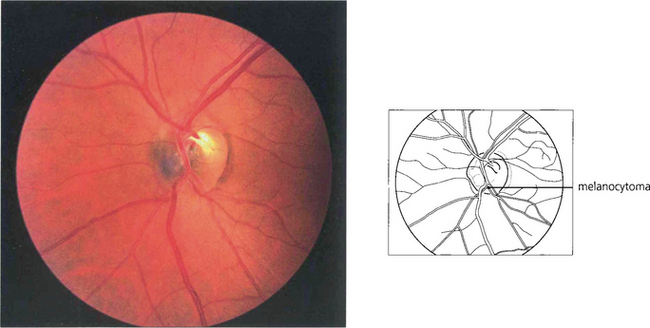
Fig. 17.72 A melanocytoma is a densely pigmented benign tumour that is usually situated in the inferior part of the disc and is more commonly found in dark-skinned people and pigmented eyes. The disc is usually larger than normal. The lesion may increase in size slowly and protrude into the vitreous or spread out on to the retina, in which case differentiation from a malignant melanoma of the choroid can be exceptionally difficult. Field defects can occur although visual acuity is not normally affected. No intratumour circulation is seen on fluorescein angiography. (See also Ch. 9.)
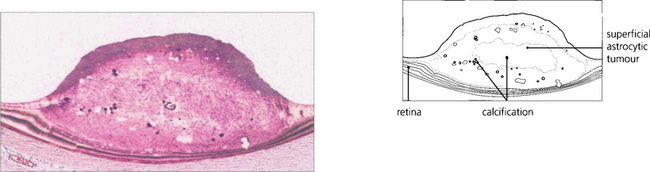
ASTROCYTIC HAMARTOMAS
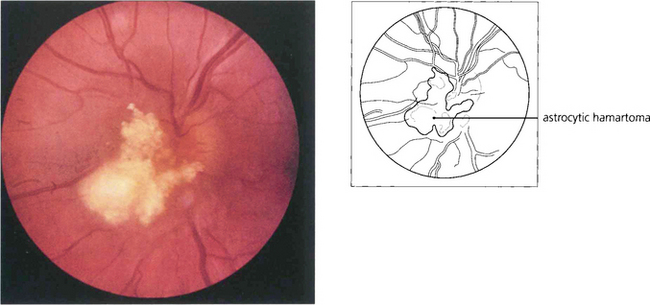
Fig. 17.73 This is a typical nodular white ‘mulberry’ tumour arising from the superficial retina adjacent to the disc. Multiple lesions are not uncommon and can sometimes be mistaken for a retinoblastoma in a child or for drusen of the disc in adults. Intratumour calcification is common. The tumours can be observed to grow slowly over many years.
By courtesy of Mr M D Sanders.
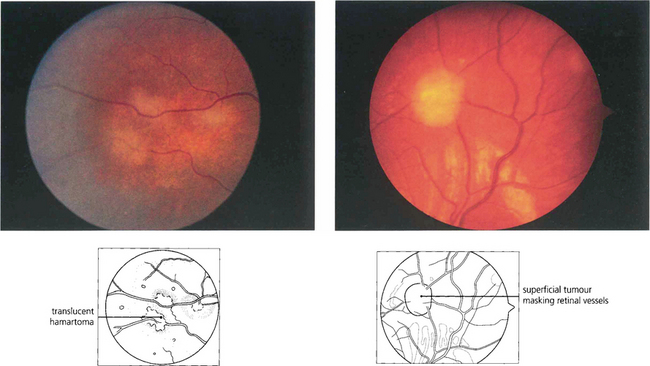
Fig. 17.74 This shows an early hamartomatous lesion in the peripheral retina of a child with tuberous sclerosis. It has a superficial gelatinous appearance, beginning as a greyish opalescent thickening of the nerve fibre layer (left) that later becomes raised and pearly white (right).
By courtesy Professor David Taylor.
NEUROFIBROMATOSIS TYPE II
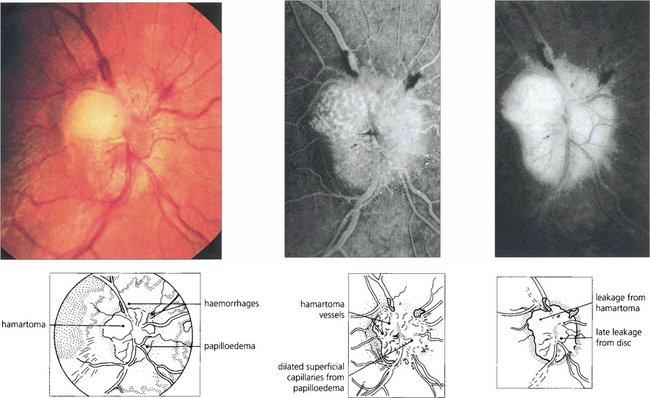
Fig. 17.77 This patient presented with papilloedema and ataxia from a posterior fossa meningioma. He had no cutaneous abnormality and no family history of neurological disease. A ‘hamartomatous’ lesion can be seen on the disc; it remained unchanged over 6 years of observation. The raised intracranial pressure was due to a meningioma in the 4 th ventricle.
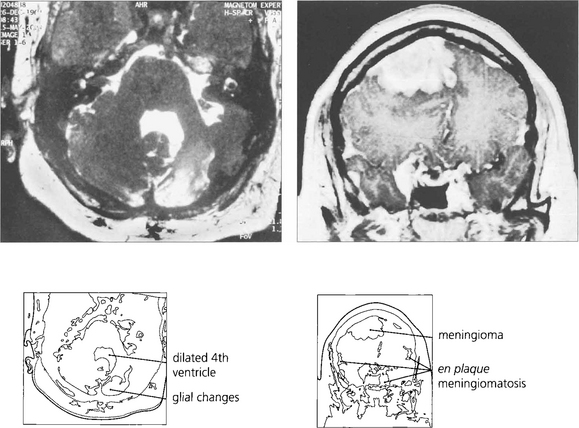
Fig. 17.78 Several years after these photographs of the optic disc were taken, this patient complained of progressive deafness and was found to have bilateral acoustic neuromas, confirming a diagnosis of neurofibromatosis type II. At this stage the patient had developed multiple and en plaque meningioma shown in this gadolinium enhanced MRI.